Abstract
Background
COVID-19 has spread widely among health care workers. Oral health care workers have an increased risk of being infected owing to dental practice characteristics. New, effective vaccines against COVID-19 have been approved for use. The authors aim was to evaluate intentions to be vaccinated against COVID-19 in a population of dentists and identify factors associated with their intentions.
Methods
The authors conducted an anonymous online survey among 761 dentists enrolled at the Board of Physicians and Dentists of the District of Monza Brianza, Monza, Italy. The authors collected data on demographic characteristics, influenza vaccine uptake, COVID-19 history, vaccine attitudes, and specific reasons for their intentions to be vaccinated against COVID-19 or not.
Results
Overall, 421 dentists completed the survey. More than 82% of the participants declared their intention to be vaccinated against COVID-19. The multivariate logistic regression model reported a positive association with receiving the influenza vaccine in the 2020-2021 influenza season (odds ratio, 5.15; 95% CI, 2.14 to 12.39) and a negative association with receiving a diagnosis of COVID-19 previously (odds ratio, 0.32; 95% CI, 0.15 to 0.66). The participants’ main reason for supporting vaccination was to protect their family and friends (87%) and their main reason for opposing vaccination was the lack of information (39%).
Conclusions
It is fundamental to consider vaccine hesitancy in health care workers and address it properly because they must provide recommendations to patients and promote adherence to vaccination programs.
Practical Implications
The vaccination of dental practitioners should be prioritized owing to the high risk related to dental practice.
Key Words: COVID-19, coronavirus, health care professionals, oral health care professionals, dentists, vaccine, vaccine hesitancy
Abbreviation Key: HCW, Health care worker; NA, Not applicable; OHCW, Oral health care worker
COVID-19 has spread widely among health care workers (HCWs).1, 2, 3 Oral HCWs (OHCWs) have an increased risk of being infected owing to dental practice characteristics.4 , 5 The potential risk surrounding dental procedure spray emissions—including aerosols and spatter—has contributed to the transmission of severe acute respiratory syndrome coronavirus 2 in dental practitioners.6 , 7 Although OHCWs can get the disease, they are also potential spreaders to their colleagues, relatives, and cohabitants. Although the systematic use of adequate personal protective equipment and adherence to safety recommendations can prevent infection in dental settings, the risk of being infected and transmitting the infection to households has contributed to psychological distress in OHCWs.5 , 8 Furthermore, the economic crisis and unemployment related to the COVID-19 pandemic have reduced access to oral health care, with relevant repercussions in dental practice.9
New effective vaccines against COVID-19 began to be available to HCWs in the United Kingdom, United States, and Europe in the last weeks of December 2020.10 Researchers have been investigating HCWs’ intentions to be vaccinated against COVID-1911, 12, 13; however, they generally did not consider the opinions of OHCWs. These studies were conducted when vaccines had not yet been developed and their mechanisms of action were unknown.
For the global vaccination campaign to be effective, the reasons for hesitation regarding vaccination must be addressed as soon as possible, especially among HCWs. Aiming to evaluate the intentions to be vaccinated against COVID-19 in a population of dentists and to identify factors associated with their intentions, we focused on dentists living in Lombardy, an Italian region dramatically affected by the disease in its first wave in March and April 2020.
Methods
We conducted an anonymous online survey among 761 dentists enrolled at the Board of Physicians and Dentists of the District of Monza Brianza in Lombardy, Italy, from December 23, 2020, through January 2, 2021. The survey was distributed to OHCWs via email, followed by a second, reminder email after a few days. Data were originally collected to provide information to the public health authority about the demand for vaccines among HCWs. Therefore, data were related to a public health surveillance activity, which does not require institutional review board approval.
The survey items were developed after a detailed analysis of scientific literature on vaccination hesitancy among HCWs and factors that might affect their opinions about vaccine.14, 15, 16 The survey was used for a pilot study among a small group of HCWs.
The survey consisted of the following 4 parts: demographic characteristics (age, sex), influenza vaccine uptake (influenza vaccine uptake in past influenza seasons and the 2020-2021 influenza season), COVID-19 and new vaccines (previous diagnosis of COVID-19, diagnosis of COVID-19 among family members or friends, intention to be vaccinated against COVID-19), and specific reasons for intending to be vaccinated against COVID-19 or not. Two separate lists of reasons (for and against vaccination) were formulated, and only 1 list was presented, according to the participant’s intention to be vaccinated or not.
The first 3 parts included closed-ended questions and single answers, and the last part regarding reasons for intending to be vaccinated against COVID-19 or not included closed-ended questions and multiple-choice answers. When participants selected “other reason,” they could clarify their answer.
Data were analyzed using SAS Statistical Software, Version 9.4 (SAS Institute). Categorical variables were reported as absolute and relative frequencies. Logistic regression was used in univariable and multivariable models to test the association between the potential adherence to the COVID-19 vaccination program and variables collected (that is, demographic characteristics, influenza vaccine uptake, previous diagnosis of COVID-19, and a diagnosis of COVID-19 among family members or friends). The variables included in the multivariable model were age (as a dichotomous variable of 55 years or younger or older than 55 years), sex, adherence to influenza vaccination programs (past and 2020-2021), and a previous diagnosis of COVID-19 (personal and among family members or friends). Odds ratio (OR) and 95% CI were reported.
Results
In all, 421 dentists completed the survey (421 of 761; 55% response rate). The main characteristics of our study population are presented in Table 1 . The most representative age group was 56 through 65 years (32.5%), followed by 46 through 55 years (24.7%), and 36 through 45 years (17.6%). Age groups at the ends were the least numerous: 14.3% and 10.9% in age groups 25 through 35 years and older than 65 years, respectively. When age groups were combined in a dichotomous variable, approximately 56.6% of the participants were 55 years and younger and approximately 43.4% were older than 55 years. Most of the dentists in our study were men (71.5%). Concerning COVID-19, 10.9% of the respondents had received a diagnosis of COVID-19 and 55.3% had at least 1 family member or friend with COVID-19.
Table 1.
Characteristics of the study population (n = 421).
| CHARACTERISTIC | NO. (%) |
|---|---|
| Age, y | |
| 25-35 | 60 (14.3) |
| 36-45 | 74 (17.6) |
| 46-55 | 104 (24.7) |
| 56-65 | 137 (32.5) |
| > 65 | 46 (10.9) |
| Age > 55 y | |
| No | 238 (56.6) |
| Yes | 183 (43.4) |
| Sex | |
| Male | 301 (71.5) |
| Female | 120 (28.5) |
| Influenza Vaccination in 2020-2021 Influenza Season | |
| No | 250 (59.4) |
| Yes | 171 (40.6) |
| Influenza Vaccination in Previous Influenza Seasons | |
| Never | 304 (72.2) |
| At least 1 time | 117 (27.8) |
| COVID-19 Diagnosis (Personal) | |
| No | 375 (89.1) |
| Yes | 46 (10.9) |
| COVID-19 Diagnosis (Family or Friends) | |
| No | 188 (44.7) |
| Yes | 233 (55.3) |
| Potential COVID-19 Vaccine | |
| No | 16 (3.8) |
| Probably no | 59 (14.0) |
| Probably yes | 95 (22.6) |
| Yes | 251 (59.6) |
We also collected data on the adherence to influenza vaccination programs with 2 questions about previous and 2020-2021 vaccination programs. Approximately 40.6% of dentists were vaccinated in the 2020-2021 influenza season and 27.8% were vaccinated at least once in the past 3 influenza seasons.
Table 1 also presents the intentions of OHCWs to adhere to the COVID-19 vaccination program. More than 82% of participants declared their intent to be vaccinated against COVID-19. Specifically, 59.6% answered “yes” and 22.6% answered “probably yes.” Conversely, 3.8% and 14.0% of dentists answered “no” and “probably no,” respectively.
Table 2 reports the associations between demographic characteristics, influenza vaccine uptake, having received a diagnosis of COVID-19 previously, and a diagnosis of COVID-19 among family members or friends and potential adherence to the COVID-19 vaccination program. In the univariate analysis, the intention to adhere to the COVID-19 vaccination program was associated with being older than 55 years (OR, 2.26; 95% CI, 1.31 to 3.91), receiving an influenza vaccine in the 2020-2021 influenza season (OR, 7.46; 95% CI, 3.48 to 15.99), and receiving at least 1 influenza vaccination in the past 3 influenza seasons (OR, 4.53; 95% CI, 2.01 to 10.20). Furthermore, having received a diagnosis of COVID-19 previously was associated with low inclination to receive the COVID-19 vaccine (OR, 0.31; 95% CI, 0.16 to 0.60). No associations between sex and COVID-19 diagnosis among family members or friends and opinions on the novel vaccine were found. The multivariate model, reported in Table 2, confirmed the positive association with influenza vaccine uptake in the 2020-2021 influenza season (OR, 5.15; 95% CI, 2.14 to 12.39) and the negative association with receiving a previous COVID-19 diagnosis (OR, 0.32; 95% CI, 0.15 to 0.66).
Table 2.
Univariate logistic regression results indicating the odds ratios for the association between the potential adherence to the COVID-19 vaccination program and variables collected (demographics, influenza vaccine uptake, and a previous COVID-19 diagnosis).
| UNIVARIATE MODEL |
MULTIVARIATE MODEL∗ |
|||||
|---|---|---|---|---|---|---|
| VARIABLE | Odds Ratio | 95% CI | P Value | Odds Ratio | 95% CI | P Value |
| Age> 55 y | .003 | .115 | ||||
| No | [Reference] | NA† | NA | [Reference] | NA | NA |
| Yes | 2.26 | 1.31 to 3.91 | NA | 1.62 | 0.89 to 2.95 | NA |
| Sex | .460 | .387 | ||||
| Male | [Reference] | NA | NA | [Reference] | NA | NA |
| Female | 0.82 | 0.48 to 1.40 | NA | 0.77 | 0.43 to 1.39 | NA |
| Influenza Vaccination in 2020-2021 Influenza Season | < .001 | < .001 | ||||
| No | [Reference] | NA | NA | [Reference] | NA | NA |
| Yes | 7.46 | 3.48 to 15.99 | NA | 5.15 | 2.14 to 12.39 | NA |
| Influenza Vaccination in Previous Influenza Seasons | < .001 | .319 | ||||
| Never | [Reference] | NA | NA | [Reference] | NA | NA |
| At least 1 time | 4.53 | 2.01 to 10.2 | NA | 1.62 | 0.63 to 4.21 | NA |
| COVID-19 Diagnosis (Personal) | < .001 | .002 | ||||
| No | [Reference] | NA | NA | [Reference] | NA | NA |
| Yes | 0.31 | 0.16 to 0.60 | NA | 0.32 | 0.15 to 0.66 | NA |
| COVID-19 Diagnosis (Family or Friends) | .702 | .615 | ||||
| No | [Reference] | NA | NA | [Reference] | NA | NA |
| Yes | 0.91 | 0.55 to 1.5 | NA | 1.16 | 0.66 to 2.04 | NA |
The multivariate model includes all variables listed.
NA: Not applicable.
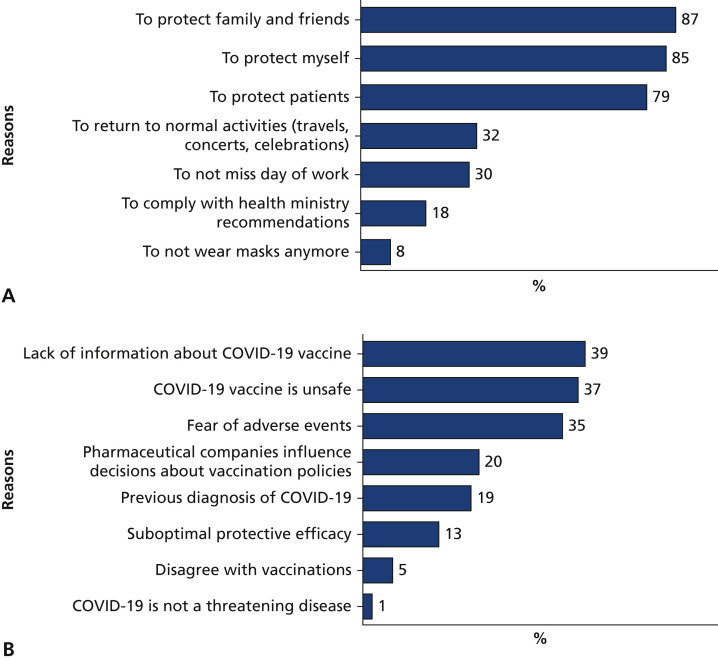
We also assessed the reasons behind the decision whether to receive the novel vaccine. Data are provided in Figures 1A and 1B. Among the 346 dentists who supported receiving the vaccination, the main reasons were to protect family and friends (87%), to protect oneself (85%), and to protect patients (79%). Furthermore, 32% of OHCWs agreed to receive the vaccination to return to normal activities (such as travel, concerts, and celebrations), 30% to not miss days of work, and 18% to comply with health ministry recommendations. Finally, approximately 8% of dentists reported wanting to be vaccinated to avoid having to wear masks (Figure 1A).
Figure 1.
A. Reasons for adhering to the COVID-19 vaccination program (n = 346). B. Reasons for not adhering to the COVID-19 vaccination program (n = 75).
Conversely, among the 75 participants who were opposed to receiving the COVID-19 vaccine, the main reasons were the lack of information about the vaccination (39%), the opinion that the vaccine is unsafe (37%), and fear of adverse events (35%). In addition, 20% stated that pharmaceutical companies influence decisions on vaccination policies, 19% had received a previous COVID-19 diagnosis, and 13% believed that the vaccine has suboptimal protective efficacy. As shown in Figure 1B, few participants provided other reasons, such as disagreement with vaccinations in general (5%) and the opinion that COVID-19 is not a threatening disease (1%). Some dentists reported immune disorders and severe allergies as additional reasons to avoid receiving the COVID-19 vaccination (4%).
Discussion
Our aim was to evaluate the intention to be vaccinated against COVID-19 in a population of dentists and to identify associated factors. To our knowledge, no similar studies have been conducted among dental practitioners, despite their increased risk of being infected owing to the nature of their practices.5 Earlier studies on these topics were conducted among general HCWs, but only when vaccines were not yet available and their mechanisms of action were still unknown.
At the time of our study, COVID-19 vaccines were already available, and in several countries including Italy the coronavirus vaccination campaign had already begun. A survey of the general Italian population conducted in September 2020 reported that only 1 in every 2 Italians wanted to be vaccinated.17 Lazarus and colleagues18 conducted a global survey of the potential acceptance of a COVID-19 vaccine among general populations worldwide; approximately 70% of participants were very or somewhat likely to take a COVID-19 vaccine. Other studies have reported similar results.19 , 20
We reported that a high percentage of dentists were favorable to vaccination (82%). This rate of COVID-19 vaccine acceptance was also higher than rates reported in several worldwide studies that focused on vaccine hesitancy among HCWs.11, 12, 13 , 21
We found that the intention to be vaccinated was associated with adherence to the 2020-2021 influenza vaccination program. This finding is not surprising because attitudes toward vaccines in general influence attitudes toward COVID-19 vaccines.11 However, we did not find an association between being favorable to COVID-19 vaccines and having been vaccinated in a influenza vaccination campaign in the past.
Although a diagnosis among family members and friends did not influence opinions on COVID-19 vaccines, having personally received a diagnosis of COVID-19 seemed to be associated with a low inclination to be vaccinated. Dentists who had COVID-19 considered themselves immune. On the one hand, this response is comprehensible; on the other hand, there is little information on immunity from natural disease and the need for vaccination.
Despite the high risk of being infected in a dental practice, it is essential to note that only 1 in 9 dentists reported receiving a diagnosis of COVID-19, fewer than other practitioners from the same highest-hit Italian region.22 This result is probably due to proper use of personal protective equipment, adherence to safety recommendations, and, in part, government restrictions that closed dental offices in the first phase of the pandemic.
Overall, 17.8% of the participants reported vaccine hesitancy. The main reasons given were the lack of information about the new vaccines, potential adverse events, and general vaccination safety. These reasons were typical arguments associated with vaccine hesitancy.16 , 23 , 24 There is a lively debate about making vaccination mandatory among some professional categories, such as HCWs, and even the general population. Although we do not want to take a firm position on this complex and sensitive issue, in our opinion, it is desirable to provide information about vaccines, to manage misinformation and fake news, and raise awareness concerning the importance of widespread vaccination, for example, with educational initiatives.25 This is a focal point for a successful vaccination campaign to reduce vaccine hesitancy and attain high vaccination coverage. The only path toward a rapid return to “normal activities” is to encourage the vaccination of HCWs and the general population. Furthermore, vaccination against COVID-19 among dentists should be prioritized owing to the particular risks inherent to practicing dentistry.
The main limitation of our study was that all of the participants were selected from the same territory, the district of Monza Brianza, in the most affected Italian region. The findings might not be representative of other dental practitioners in Italy. Furthermore, the response rate was suboptimal, and the possibility of distortion should be considered. Despite these limitations, we are the first researchers, to our knowledge, to examine attitudes about COVID-19 vaccines among dentists in Italy and worldwide. Our study is also the first, to our knowledge, conducted on Italian HCWs when vaccines were available.
Conclusions
The percentage of dentists who wanted to adhere to the COVID-19 vaccination program was high, which indicates their awareness about the importance of prevention and the high occupational risk related to their practice. However, it is crucial to consider vaccine hesitancy in HCWs and address it because they must provide recommendations to patients and promote adherence to vaccination programs. We also investigated the reasons for nonadherence to the COVID-19 vaccination program, and knowledge of specific reasons is important in implementing strategies to address COVID-19 vaccine hesitancy properly. Finally, because dentists are at high risk of contracting COVID-19, vaccination of dental practitioners should be prioritized.
Biographies
Dr. Belingheri is an assistant professor, School of Medicine and Surgery, University of Milano-Bicocca, Monza, Italy; and a councilor, Board of Physicians and Dentists of the District of Monza Brianza, Monza, Italy.
Dr. Roncalli is the president, Dentists’ Register Committee, Board of Physicians and Dentists of the District of Monza Brianza, Monza, Italy.
Dr. Riva is an associate professor, School of Medicine and Surgery, University of Milano-Bicocca, Monza, Italy; and a councilor, Board of Physicians and Dentists of the District of Monza Brianza, Monza, Italy.
Dr. Paladino is an adjunct professor, School of Medicine and Surgery, University of Milano-Bicocca, Monza, Italy.
Dr. Teruzzi is the president, Board of Physicians and Dentists of the District of Monza Brianza, Monza, Italy.
This article has an accompanying online continuing education activity available at: http://jada.ada.org/ce/home.
Footnotes
Disclosure. None of the authors reported any disclosures.
References
- 1.Belingheri M., Paladino M.E., Riva M.A. Working schedule, sleep quality and susceptibility to COVID-19 in healthcare workers. Clin Infect Dis. 2021;72(9):1676. doi: 10.1093/cid/ciaa499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nguyen L.H., Drew D.A., Graham M.S. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Belingheri M., Paladino M.E., Riva M.A. Risk exposure to coronavirus disease 2019 in pregnant healthcare workers. J Occup Environ Med. 2020;62(7) doi: 10.1097/JOM.0000000000001881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harrel S.K., Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. JADA. 2004;135(4):429–437. doi: 10.14219/jada.archive.2004.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meng L., Ma B., Cheng Y., Bian Z. Epidemiological investigation of OHCWs with COVID-19. J Dent Res. 2020;99(13):1444–1452. doi: 10.1177/0022034520962087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sergis A., Wade W.G., Gallagher J.E. Mechanisms of atomization from rotary dental instruments and its mitigation. J Dent Res. 2021;100(3):261–267. doi: 10.1177/0022034520979644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Izzetti R., Nisi M., Gabriele M., Graziani F. COVID-19 transmission in dental practice: brief review of preventive measures in Italy. J Dent Res. 2020;99(9):1030–1038. doi: 10.1177/0022034520920580. [DOI] [PubMed] [Google Scholar]
- 8.Bakaeen L.G., Masri R., AlTarawneh S. Dentists’ knowledge, attitudes, and professional behavior toward the COVID-19 pandemic. JADA. 2021;152(1):16–24. doi: 10.1016/j.adaj.2020.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi S.E., Simon L., Riedy C.A., Barrow J.R. Modeling the impact of COVID-19 on dental insurance coverage and utilization. J Dent Res. 2021;100(1):50–57. doi: 10.1177/0022034520954126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oliver S.E., Gargano J.W., Marin M. The Advisory Committee on Immunization Practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 vaccine: United States, December 2020. Morb Mortal Wkly Rep. 2020;69(50):1922. doi: 10.15585/mmwr.mm6950e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gagneux-Brunon A., Detoc M., Bruel S. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross sectional survey. J Hosp Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwok K.O., Li K.K., Wei W.I., Tang A., Wong S.Y.S., Lee S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021;114:103854. doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang K., Wong E.L.Y., Ho K.F. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38(45):7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herzog R., Álvarez-Pasquin M.J., Díaz C., Del Barrio J.L., Estrada J.M., Gil Á. Are healthcare workers’ intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13(1):1–17. doi: 10.1186/1471-2458-13-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Durando P., Alicino C., Dini G. Determinants of adherence to seasonal influenza vaccination among healthcare workers from an Italian region: results from a cross-sectional study. BMJ Open. 2016;6(5) doi: 10.1136/bmjopen-2015-010779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lane S., MacDonald N.E., Marti M., Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF joint reporting form data—2015-2017. Vaccine. 2018;36(26):3861–3867. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.La Vecchia C., Negri E., Alicandro G., Scarpino V. Attitudes towards influenza vaccine and a potential COVID-19 vaccine in Italy and differences across occupational groups, September 2020. Med Lav. 2020;17 doi: 10.23749/mdl.v111i6.10813. 111(6):445-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazarus J.V., Ratzan S.C., Palayew A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sherman S.M., Smith L.E., Sim J. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021;17(6):1612–1621. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dror A.A., Eisenbach N., Taiber S. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Missaglia R., Belingheri M., Antolini L. SARS-CoV-2 pandemia in Lombardy: the impact on family paediatricians. Ital J Pediatr. 2020;46(1):184. doi: 10.1186/s13052-020-00950-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical students. J Public Health (Oxf). Published online December 26, 2020. https://doi.org/10.1093/pubmed/fdaa230 [DOI] [PMC free article] [PubMed]
- 24.Giambi C., Fabiani M., D’Ancona F. Parental vaccine hesitancy in Italy: results from a national survey. Vaccine. 2018;36(6):779–787. doi: 10.1016/j.vaccine.2017.12.074. [DOI] [PubMed] [Google Scholar]
- 25.Jarrett C., Wilson R., O'Leary M., Eckersberger E., Larson H.J., the SAGE Working Group on Vaccine Hesitancy Strategies for addressing vaccine hesitancy: a systematic review. Vaccine. 2015;33(34):4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]