Graphical abstract
Keywords: Endoscopy, Coronavirus infections, Prevention and mitigation
Abstract
Background and study aims
The COVID-19 outbreak has reorganized surgical team conditions regarding endoscopy. The number of interventions has been reduced, the number of healthcare professionals must be limited, and both the patients and physicians are more protected than ever.
Patients and Methods
In the highest peak of contagion in Colombia, endoscopy, colonoscopy, and esophagogastroduodenoscopy were performed using a low-cost disposable device. A total of 1388 procedures were performed. Every patient was assessed for symptoms via a telephone call, at the health center, and after the procedure, following specific attention routes.
Results
After procedure follow-up, no positive cases of COVID-19 were noted.
Conclusion
The methodology reduced the risk of infection during the COVID-19 pandemic.
Introduction
At the end of 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged for the first time in the Chinese region of Hubei and spread worldwide in a few months; this infection causes mainly respiratory conditions ranging from mild symptoms such as rhinitis, fever, cough, anosmia, and dysgeusia, to pneumonia and acute respiratory distress syndrome [1].
The SARS-CoV-2 virus is mainly transmitted by droplets of saliva when speaking or coughing. However, the fecal–oral transmission is not excluded. Thus, gastrointestinal endoscopic procedures have a high risk of contagion because they require airway manipulation and direct contact with respiratory droplets or gastrointestinal secretions. They are also considered aerosol-generating procedures [1], [2]. Previous reports on other outbreaks showed that gastrointestinal endoscopy can also be a vector of transmission for some viruses, such as hepatitis B and C [3].
Currently, approximately 160 million cases and 3 million 3 million deaths have been reported worldwide. In Colombia, over 3 million cases and over 8 80 80.000 deaths have been recorded. Hence, this study aimed to describe our clinical experience, the results of using a low-cost device for endoscopy, and the methodology used in our hospital for patient admission and discharge to reduce infection risk when performing an endoscopy.
Patients and methods
Study population, setting, and data collection
We retrospectively investigated patients who required an endoscopic procedure during the peak of the COVID-19 pandemic at our center in Bogotá, Colombia, between May and July of 2020.
Patient data and characteristics collected from the center’s database were analyzed. These data included the number of answered calls, the symptoms, and the procedure type. The IRB number was 353130.
Approach strategy for covid-19 prevention
According to epidemiological reports, establishing a strategy for preventing COVID-19 contagion is crucial.
Two days before the intervention, patients were called via a telephone call to inquire about respiratory or systemic symptoms using a questionnaire. If the patient was asymptomatic and isolated, the attention routes were explained. We sent an email with instructions wherein the patient and his/her partner should be assigned as A and B, respectively.
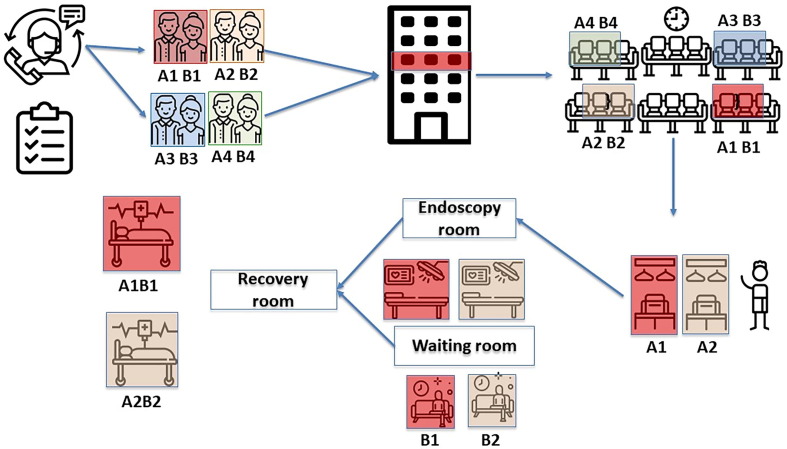
At procedure day, patients were grouped into four, namely, the first groups (A1B1) and (A2B2) in the first time slot for procedures and the second groups (A3B3) and (A4B4), all according to our proposed organizational scheme.
All patients followed the required biosecurity and hygiene elements, maintaining the 2 m physical distance in the waiting room. They were divided into four groups to access by turns to the endoscopy room. At the end of the procedure, the patient and his/her companion were reunited and discharged through an alternative exit route (Fig. 1, Fig. 2 ).
Fig. 1.
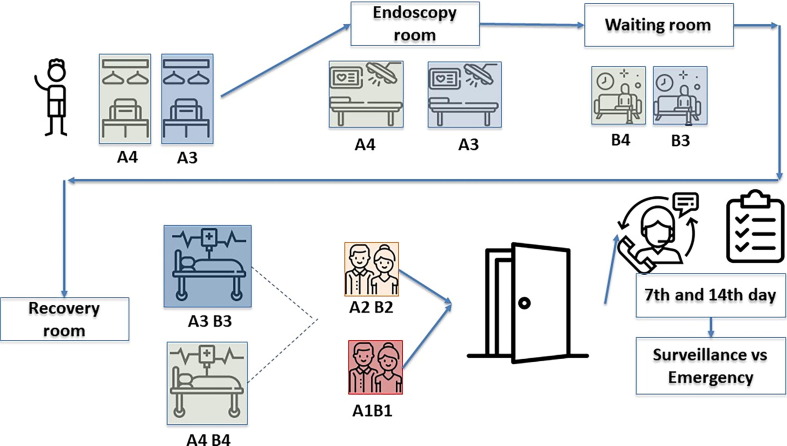
Fig. 2.
Patient protection
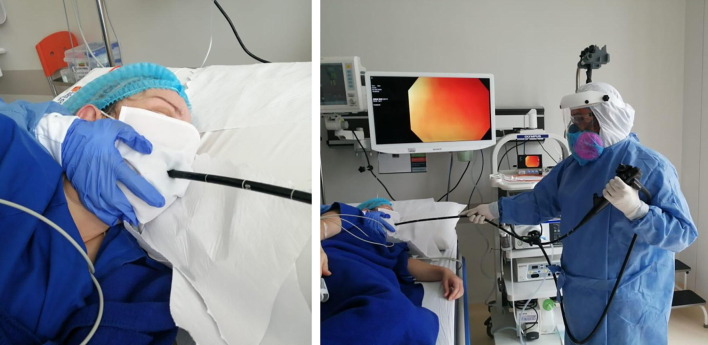
Endoscopies were performed using a low-cost method, that is, disposable mask wearing with a modified incision of 1–1.5 cm (Fig. 3 A), to reduce the risk of contagion for both the patient and the healthcare professionals in the operating room. The use of this device did not alter the development of any of the endoscopic procedures, and the protective benefits provided by this device were clearly explained to the patient. Meanwhile, colonoscopies had a lesser risk of contagion, but the physician and the patient still used the PPE recommended for each case.
Fig. 3.
Staff protection
The staff consisted of 4 gastroenterologists, 5 nurses, 2 receptionists, and 1 counselor. The gastroenterologists and assistants used all the protection elements to limit the droplet transmission and always maintained the appropriate distance. Such protection consisted of gloves, medical masks, goggles or a face shield, gowns, and aprons (Fig. 3B) [4]. All staff members were tested periodically for COVID-19. If a staff member exhibited possible COVID-19 symptoms or was exposed to a positive case, local safety protocols must be followed while staying off work.
After the procedure, all patients were followed up via a telephone call on three separate occasions (7, 14, and 21 days) to assess for new symptoms according to the recommendations of the New York Society of Gastrointestinal Endoscopy and the American Society of Gastrointestinal Endoscopy [3].
Our institution’s ethics committee approved our study protocol. The protocol conformed to the principles of the Declaration of Helsinki and Good Clinical Practice guidelines.
Results
During the study duration (May 2020–July 2020), 1388 procedures were performed in which 80 (5.76%) were inpatients and 1308 (94.24%) were outpatients. Among the procedures, three were diagnostic (endoscopy, colonoscopy, and esophagogastroduodenoscopy), and 16 were therapeutic (resection of large intestine injury, endoscopic extraction of foreign bodies, dilation of anastomosis, ERCP, and insertion of stent for the esophagus). Subsequent follow-up was achieved at least once in 93.4% of the patients. Table 1
Table 1.
Follow-up (May patients).
| First Call | Second Call | Third Call | |
|---|---|---|---|
| No change | 89.62% | 86.16% | 71.28% |
| No answer | 6.57% | 12.8% | 28.72% |
| Present symptoms | 3.81% | 1.04% | 0% |
Patients who manifested symptoms after the procedure underwent an RT-PCR test for SARS-Cov-2 and were suggested to undergo preventive isolation. However, of all the symptomatic patients, none were positive in the following test. All the staff members in charge of the procedure were also screened by the same RT-PCR test and were found to be negative as of the date of the study.
Discussion
COVID-19 is a disease caused by the pathogen officially called as SARS-CoV-2, which is an RNA betacoronavirus that is quite similar to the known coronavirus SARS discovered in 2003. These coronaviruses utilize the angiotensin-converting enzyme 2 to access the cell and begin its replication [4], [5], [6].
Respiratory symptoms are the most common manifestation related to COVID-19. However, a recent meta-analysis of 60 studies with 4243 patients from Asia, Europe, and the United States showed a prevalence of gastrointestinal symptoms of 17.6%. The most commonly reported symptom was anorexia (26.8%), followed by diarrhea (12.5%), nausea and vomiting (10.2%), and abdominal pain or discomfort (9.2%). Nonetheless, in most cases, these symptoms decrease or disappear over the course of the disease [5], [6].
Gastrointestinal manifestations of the virus seem to be more involved every time. In a multicenter retrospective study conducted in China, almost half of the patients with COVID-19 mainly complained of at least one gastrointestinal symptom. The variety in the symptomatology leads to confusion in some patients because of the characteristic mildness [7].
An aerosol-generating procedure is any medical procedure that can induce the production of aerosols of any size, including droplet nuclei [8]. Endoscopy services worldwide, being an aerosol-generating procedure, need to modify their protocols to deal with this pandemic. Filho et al. reported that various international gastroenterology societies reviewed endoscopy recommendations and practices. These societies all agreed to recommend the mandatory use of PPE during examinations and to postpone non-urgent procedures, but only 86% recommended stratifying the patients’ risk for COVID-19 [9].
By conducting a systematic review, the Canadian Agency for Drugs and Technologies in Health identified procedures that showed a significant increase in SARS infection during the SARS outbreak in 2002–2003. These procedures included endotracheal intubation, noninvasive intubation (CPAP and BiPAP), tracheostomy intubation, and manual ventilation before intubation [2].
A general recommendation is to reduce the number of endoscopy personnel, who should be highly trained to reduce the duration of the procedure and the risk of exposure, as well as the use of suitable PPE for both the personnel and the patient. Staff members who are in close contact with a patient with COVID-19 have an increased risk of infection because of the potential for transmission during upper digestive endoscopy and the increasing evidence of fecal–oral transmission by inhalation or contact of conjunctival spatter or direct contact with feces during colonoscopy [6].
Zhang et al. created a flowchart to explain the conditions on who should receive endoscopies and who should be postponed. Those who were in need of the procedure were prescreened, and only those with negative test results were appointed for endoscopy. The temperature was also checked, and every patient was followed up for 14 days. The patients signed an additional informed consent form, approving a digestive endoscopy during the coronavirus outbreak [10], [11].
The endoscopic intervention’s priority is to improve patient’s survival in an emergency situation, such as critical oncological events, life-threatening gastrointestinal bleeding, or foreign body ingestion. Otherwise, the procedure can be postponed after the resolution of the COVID-19 pandemic. However, the decision is mainly based on the criteria of the physician, taking into account possible contagion risks depending on the patient’s clinical status [7].
Most of the individuals with COVID-19 are asymptomatic or have mild symptoms, making them go unnoticed; hence, increased vigilance and careful screening of individuals who are at risk are needed, and elective, non-urgent procedures should be deferred until this pandemic is over [3].
Another important recommendation in confirmed COVID-19 cases or high-risk patients is mandatory double disinfection of the equipment used for the procedure. The incidence of infection associated with endoscope use is one case per 1.8 million procedures. Estimating the causal relationship between the endoscope use and the pathogen is challenging. Nevertheless, the disinfection process of the endoscope should be the following: precleaning, cleaning, rinsing, high-level disinfection, rinsing, drying (air/alcohol), and storage [6], [7], [8], [9], [10], [11], [12], [13], [14].
To conclude, the COVID-19 pandemic and the real risk for healthcare personnel need further elucidation. Other viral epidemics have shown practically no risk of transmission in endoscopic and laparoscopic procedures, and we can extrapolate the results [15]. Though no studies have expressed recommendation on using a similar low-cost device for endoscopy, the use of this device contributed to the safety of both the staff and patients during the study period.
Declaration of competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Sinonquel P., Aerts M., Badaoui A., Bisschops R., Blero D., Demedts I. BSGIE survey on COVID-19 and gastrointestinal endoscopy in Belgium: results and recommendations. Acta gastro-enterologica Belgica. 2020;83(2):344–354. [PubMed] [Google Scholar]
- 2.Asociación Colombiana de Infectología. Consenso Colombiano de atención, diagnóstico y manejo de la infección por SARS-CoV-2/COVID-19 en establecimientos de la atención de la salud;24(3). Mayo de 2020.
- 3.Perisetti A., Gajendran M., Boregowda U., Bansal P., Goyal H. COVID-19 and gastrointestinal endoscopies: current insights and emergent strategies. Dig Endosc. 2020;32(5):715–722. doi: 10.1111/den.13693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villareal R., Cabrera L.F., Pedraza M., Cuervo J.E., Santos J.H., Jurado J.R. Dispositivo de bajo costo para disminuir el efecto de aerosol durante la endoscopia de vías digestivas altas en COVID-19. Revista Colombiana de Gastroenterología. 2020;35(Supl. 1):17–20. [Google Scholar]
- 5.Cheung K.S., Hung I.F.N., Chan P.P.Y. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology. 2020;S0016-5085(20):30448–130440. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aguila E.J.T., Cua I.H.Y., Dumagpi J.E.L., Francisco C.P.D., Raymundo N.T.V., Sy-Janairo M.L.L. COVID −19 and its effects on the digestive system and endoscopy practice. JGH Open. 2020;4(3):324–331. doi: 10.1002/jgh3.12358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elli L., Rimondi A., Scaramella L., Topa M., Vecchi M., Mangioni D. Endoscopy during the Covid-19 outbreak: experience and recommendations from a single center in a high-incidence scenario. Digest Liver Dis. 2020;52(6):606–612. doi: 10.1016/j.dld.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Repici A, Maselli R, Colombo M, Gabbiadini R, Spadaccini M, Anderloni A, et al. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020;92(1):192-197. pii: S0016-5107(20)30245-5. [DOI] [PMC free article] [PubMed]
- 9.Castro Filho E.C., Castro R., Fernandes F.F., Pereira G., Perazzo H. Gastrointestinal endoscopy during the COVID-19 pandemic: an updated review of guidelines and statements from international and national societies. Gastrointest Endosc. 2020;92(2):440–445.e6. doi: 10.1016/j.gie.2020.03.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yafei Z et al. Suggestions for infection prevention and control in digestive endoscopy during current 2019-nCoV pneumonia outbreak in Wuhan, Hubei Province, China. 2020;52:312-314. [DOI] [PMC free article] [PubMed]
- 11.Bonato G., Dioscoridi L., Mutignani M. Faecal-oral transmission of SARS-COV-2: practical implications. Gastroenterology. 2020;159(4):1621–1622. doi: 10.1053/j.gastro.2020.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xiao F., Tang M., Zheng X., Liu Y.e., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831–1833.e3. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiu P.W.Y., Ng S.C., Inoue H., Reddy D.N., Ling Hu E., Cho J.Y. Practice of endoscopy during COVID-19 pandemic: position statements of the Asian Pacific Society for Digestive Endoscopy (APSDE-COVID statements) Gut. 2020;69(6):991–996. doi: 10.1136/gutjnl-2020-321185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryu J.K., Kim K.K.A., Choi I.J., Hahm K.B. Role of the clinical endoscopy in emphasizing endoscope disinfection. Clin Endosc. 2015;48:351–355. doi: 10.5946/ce.2015.48.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston E.R., Habib-Bein N., Dueker J.M., Quiroz B., Corsaro E., Ambrogio M. Risk of bacterial exposure to the endoscopist’s face during endoscopy. Gastrointest Endosc. 2019;89(4):818–824. doi: 10.1016/j.gie.2018.10.034. [DOI] [PubMed] [Google Scholar]