Abstract
Clinicians tend to focus on diastolic blood pressure (DBP), rather than systolic blood pressure (SBP), to identify and treat hypertension. The authors used data from the National Health and Nutrition Examination Survey (NHANES III, 1988–1994) Mobile Examination Center to examine the distributions of SBP and DBP in treated and untreated individuals with hypertension. We identified the percentage of the hypertensive population with SBP controlled to <140 mm Hg and the percentage with DBP controlled to <90 mm Hg, stratified by treatment status, gender, race, and ethnicity. Individuals were classified as having hypertension if they had SBP of >140 mm Hg or DBP of >90 mm Hg, or if they were taking medication for hypertension. A weighted analysis was performed to project the results to the entire U.S. population from 1988–1994; these totals were further estimated for the year 2000 by extrapolation. For men, women, whites, African Americans, and Hispanics, SBP control rates were uniformly poorer than DBP control rates. The difference persisted when subgroups were categorized according to treatment status. The disparity in SBP and DBP control rates was especially great for women: only 50% of treated white women with hypertension had SBP control, but 92% had DBP control. The prevalence of isolated systolic hypertension was greater than 50% among all individuals with hypertension in the 55–60‐year age group and increased with age thereafter. A greater emphasis on SBP is needed to improve population blood pressure control.
BACKGROUND
Hypertension is an important health problem in the United States for nearly 50 million Americans. 1 Although hypertension control in North America, Western Europe, Japan, and Australia has improved dramatically since 1950, 2 , 3 , 4 an extremely large proportion of the population is still in need of better care. Despite the availability of effective antihypertensive treatments, many patients diagnosed with hypertension remain uncontrolled and at increased risk for stroke, atherosclerosis, ischemic heart disease, congestive heart failure, and chronic renal failure. 2 , 5 , 6
Recent analyses of the National Health and Nutrition Examination Survey (NHANES III) revealed that the most common type of uncontrolled hypertension was isolated systolic hypertension, 7 , 8 which is consistent with data from other trials. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 In a recent Framingham analysis, 16 systolic blood pressure (SBP) was controlled significantly less well than diastolic blood pressure (DBP) (49% SBP vs. 89.7% DBP). These findings are relevant because of the relationship between blood pressure and cardiovascular disease risk 18 , 19 , 20 , 21 and the growing awareness that SBP may be a better measure of cardiovascular disease risk than DBP. 22 , 23 , 24 , 25
The current analysis expands on the work of our group 8 by further examining the distributions of SBP and DBP in the NHANES III study. SBP and DBP control rates were examined in relation to gender, ethnicity, race, and treatment status. We sought to provide a perspective on the scope of the SBP problem and its likely relevance to a wide range of clinical practices.
METHODS
Study Population
NHANES III, sponsored by the National Center for Health Statistics, was designed to provide estimates of common, chronic conditions and associated risk factors for a representative sample of the civilian, non‐institutionalized population of the United States. 5 , 6 The adult blood pressure component of NHANES III was designed to provide estimates of the prevalence, awareness, treatment, and control of hypertension in the general population. A national sample of 19,661 adults 18 years of age or older agreed to be interviewed in their homes and to have an extensive medical examination at a mobile examination center.
Blood Pressure Measurements
At the end of the interview, the participant's blood pressure was measured three times. A physician obtained a second set of blood pressure measurements during a subsequent medical examination. In both settings, blood pressures were measured with the participant in the sitting position after 5 minutes of rest. A standard mercury sphygmomanometer was used, and one of four cuff sizes was chosen based on the circumference of the participant's arm. All observers were trained to record the DBP at the disappearance of the last sound. The maximum inflation level was determined before the first blood pressure measurement, with at least a 30‐second interval between each cuff inflation. All six blood pressure readings were available for 78.2% of participants; three of six readings were available for an additional 17.6% of participants; and partial data were obtained on one or two occasions for 1.6% of participants. The mean of the available blood pressures 1 , 2 , 3 , 4 , 5 , 6 was used for all analyses presented.
Definition of Variables
Hypertension was defined as mean SBP of ≥140 mm Hg, mean DBP of ≥90 mm Hg, or current treatment for hypertension with prescription medication. Hypertension treatment was defined as use of prescription medication for high blood pressure at the time of the interview. SBP control was defined as SBP of <140 mm Hg (irrespective of DBP), and DBP control was defined as DBP of <90 mm Hg (irrespective of SBP). Overall hypertension control was defined as the simultaneous presence of SBP of <140 mm Hg and DBP of <90 mm Hg, consistent with targets from the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). 2 Isolated systolic hypertension (ISH) was defined as SBP of ≥140 mm Hg and DBP of <90 mm Hg. Awareness of hypertension was determined by interviews with untreated hypertensive participants only.
Study Design
The NHANES III data were analyzed for means, medians, and standard deviations of SBP and DBP in the overall population of individuals with hypertension. The prevalence of ISH (among individuals with hypertension) was examined for age groups in 5‐year strata. Awareness, treatment, and control were examined for age groups in 10‐year strata. Differences in SBP and DBP control rates were obtained for treated and untreated individuals grouped according to gender and race or ethnicity.
Statistical Analysis
A weighted analysis was performed to assess hypertension parameters among the entire adult civilian, non‐institutionalized, 1988–1994 population of the United States. These totals were further extrapolated for the year 2000 population. Estimates were weighted and adjusted to reduce bias from nonresponse at the interview stage. Since the design of NHANES III was a multistage probability sample, conventional statistical analyses with underlying distributional assumptions were inappropriate for variance estimation. The SUDAAN software (Research Triangle Institute, Cary, NC) 26 PROC DESCRIPT® was used to compute Taylor series standard deviations for survey data. All other analyses were performed with SAS© statistical software (SAS Corp., Cary, NC). 27
RESULTS
Based on NHANES III data, 42.7 million adult Americans, or 24% of the adjusted adult U.S. population, were projected to have hypertension in the period 1988–1994. For the year 2000 U.S. adult population of 205.4 million, 28 there were a projected 49.3 million individuals with hypertension, approximately one half being men and one half being women. The systolic and diastolic blood pressures of the hypertensive individuals from the NHANES interviews are presented in Figure 1.
Figure 1.
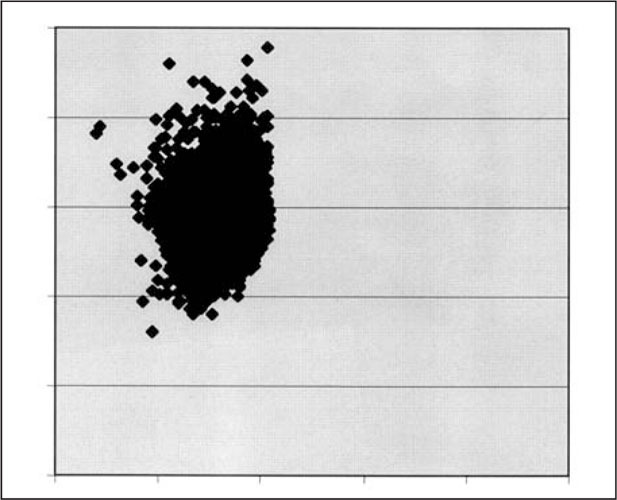
Systolic and diastolic blood pressure levels in the U.S. hypertensive population 30
The majority of individuals with hypertension have SBP of >140 mm Hg and DBP of <90 mm Hg. In 1988–1994, over 28 million people had a SBP of >140 mm Hg, whereas only 11.4 million had a DBP of >90 mm Hg. This extrapolates to 32.3 million with uncontrolled SBP and 13.2 million with uncontrolled DBP in the year 2000. The 1988–1994 numbers are the basis for the overall SBP and DBP control rates previously published by our group: SBP was controlled in only 34%, whereas DBP was controlled in 73%. 8
The distribution of SBP in the population with hypertension is presented in Figure 2. The median SBP was 146 mm Hg, the mean SBP was 147.7 mm Hg, and the standard deviation was 8.4 mm Hg. Thus, the mean SBP was almost one standard deviation above the target SBP goal of 140 mm Hg.
Figure 2.
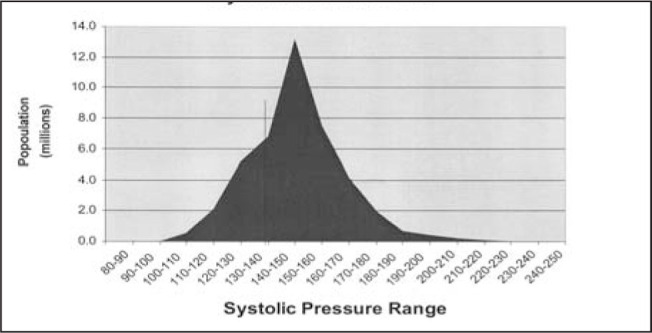
Systolic blood pressure of individuals with hypertension. 30 Reprinted with permission from J Hypertens. 1999;17(suppl 3):S188.
The distribution of DBP in the population with hypertension is presented in Figure 3. The median DBP was 81 mm Hg, the mean DBP was 80.8 mm Hg, and the standard deviation was 12.1 mm Hg. Thus, the mean DBP was nearly one standard deviation below the target DBP of 90 mm Hg.
Figure 3.
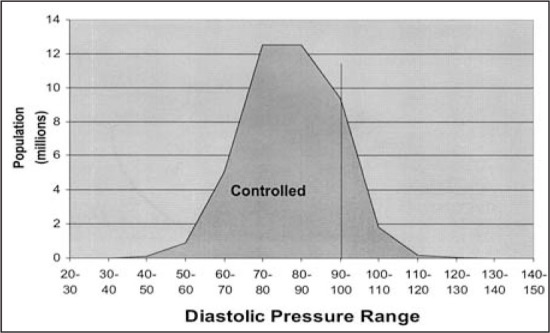
Diastolic blood pressure of individuals with hypertension 30
Figure 4 shows the prevalence of ISH among individuals with hypertension in 5‐year age strata. ISH prevalence increased from 25% in 45–50‐year‐old hypertensive patients to over 90% in those aged 70 and above. It reached more than 50% by age 55–60.
Figure 4.
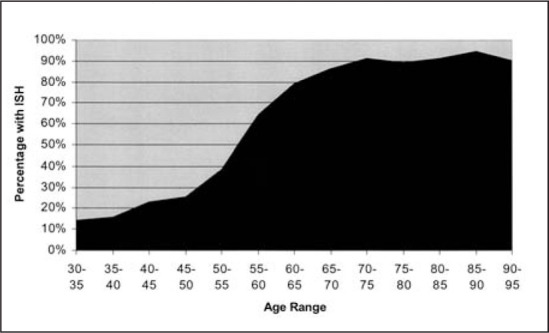
Prevalence of isolated systolic hypertension (ISH) by age in the U.S., 1988–1994. 30 Reprinted with permission from J Hypertens. 1999;17(suppl 3):S188.
In the Table, SBP and DBP control rates are presented for individuals with hypertension grouped according to gender and race or ethnicity. The results are further divided according to treatment status. SBP control rates were uniformly lower than DBP control rates for all participant groups and were consistently lower in untreated women than untreated men. Only 50% of treated white women with hypertension had SBP control, whereas 90% had DBP control. Treated white men and women had higher control rates for both SBP and DBP than either African Americans or Hispanics.
Table TABLE.
Percent of SBP and DBP Controlled by Race/Ethnicity, Gender, and Treatment Status
| Percent with SBP Controlled | Percent with DBP Controlled | |||
| Treated | Untreated | Treated | Untreated | |
| Females | ||||
| White | 50 | 6 | 92 | 80 |
| African American | 48 | 17 | 82 | 51 |
| Hispanic | 40 | 10 | 85 | 73 |
| Males | ||||
| White | 49 | 25 | 80 | 51 |
| African American | 47 | 31 | 71 | 35 |
| Hispanic | 45 | 32 | 70 | 42 |
| SBP=systolic blood pressure; DBP=diastolic blood pressure | ||||
Awareness, treatment, and control are presented according to age in Figure 5. All three measures reached a plateau at approximately age 60–69 and fell thereafter in this elderly population, and there was a predominance of ISH (Fig. 4). The elderly hypertensive population was also predominantly female.
Figure 5.
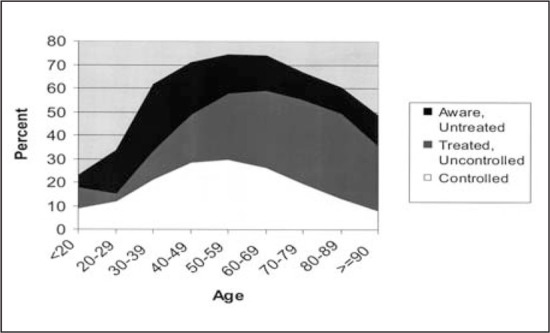
Awareness, treatment, and control of hypertension in U.S. patients, by age. 30 Reprinted with permission from J Hypertens. 1999;17(suppl 3):S188.
DISCUSSION
SBP control rates were lower than DBP control rates in a variety of patient groups. Clinical practices differ broadly from one geographic region to another, but the low control rate of systolic hypertension is relevant to both genders and all racial and ethnic groups examined in this study. These results suggest that the majority of physicians who treat middle‐aged or elderly patients with hypertension face the same problem: control of systolic hypertension, with ISH as a major challenge.
Reviews of previous clinical studies confirm poor SBP as compared to DBP control rates. This appears evident in the Hypertension Optimal Treatment (HOT), Antihypertensive and Lipid Lowering treatment to prevent Heart Attack Trial (ALLHAT), and Controlled Onset Verapamil Investigation of Cardiovascular Endpoints (CONVINCE) trials. 22 , 23 , 24 In the HOT study, DBP was below the 90 mm Hg goal in 91.7% of all participants and the mean DBPs were 85.2, 83.2, and 81.1 mm Hg in the three target groups, or 5–9 mm Hg below the JNC VI guidelines. In contrast, the mean SBPs were 143.7, 141.4, and 139.7 mm Hg, respectively, in the three target groups. Assuming that SBP is normally distributed, this suggests that fewer than one half of HOT patients achieved SBP control, whereas the vast majority had DBP control. Similarly, in the ALLHAT 24 and CONVINCE 23 studies, DBP control rates were close to 90%, while SBP control rates were only about 60%.
Studies of clinical practice have also yielded data consistent with the NHANES III findings. Berlowitz et al. 10 found mean SBP and DBP levels similar to those in NHANES III in their Veterans Administration population. 10 In their model of physician practice patterns, DBP was a stronger predictor than SBP of physician action to intensify treatment.
Alexander et al. 11 studied patients within a large health maintenance organization and found that approximately 70% of patients with hypertension had good DBP control but fewer than 40% had an SBP of <140 mm Hg. SBP control rates were lower than DBP control rates in both younger (under 65) and older age groups. The DBP control rate was 63.4% for those under 65 and 82.8% for those 65 years or older, whereas SBP control was 40% for those under 65 and only 26.4% for those aged 65 or older.
Paramore et al. 12 also found SBP to be less well controlled than DBP in a large managed care group. In 54% of visits, patients had SBP above the JNC VI target of 140 mm Hg, while DBP was above the target level of 90 mm Hg in only 26% of visits. Over a 1‐year time horizon, 41.5% of patients had at least one visit at which SBP was above 160 mm Hg.
Hyman et al. 13 surveyed 1200 primary care physicians on their blood pressure treatment thresholds and found that thresholds for treating SBP were not as strict as those for treating DBP. For middle‐aged patients with uncomplicated hypertension, 33% of physicians would not start drug therapy until DBP was greater than 95 mm Hg, whereas 43% would not initiate drug therapy unless SBP was greater than 160 mm Hg. For patients on drug therapy, 25% of physicians would not increase drug therapy with a DBP of 94 mm Hg, and 33% would not increase drug therapy for an SBP of 158 mm Hg.
Oliveria et al. 14 surveyed physicians on their practices and examined medical records of patients who had uncontrolled hypertension for 6 months. SBP control rates (7%) were lower than DBP control rates (77.9%). Pharmacologic therapy was initiated or changed at only 38% of visits. The most frequently cited reason for inaction was related to the physicians being satisfied with the blood pressure level. Physicians reported that they had less aggressive treatment thresholds for SBP than for DBP.
The RAND Corporation 15 developed a quality of care measurement system and evaluated it in medical records of women with hypertension in a west coast health plan. Only 37% of hypertensive patients with persistent elevations of >160/90 mm Hg had documentation of any changes in therapy or any recommendation for lifestyle modifications in the medical record. In this study, lower compliance with quality indicators was associated with worse blood pressure control.
Although part of the problem with low SBP control rates may be lack of access to care or lack of treatment, these studies point to a significant problem in physician practices, with failure to step up therapy and a tendency to treat DBP instead of SBP. This is consistent with the data in the Table, which show low SBP control rates even among treated patients.
In terms of improving SBP control, target populations may include women and the elderly. The disparity of SBP and DBP control rates is greatest for women. Older patients have a much greater prevalence of ISH. Among elderly individuals, women outnumber men. National guidelines recommend aggressive treatment of SBP, but studies like those of Oliveria et al. 14 suggest that national guidelines have not yet sufficiently changed physician practice. O'Connor et al. 9 also suggest that implementing hypertension guidelines, with identification, tracking, and active outreach to patients can lead to significantly improved hypertension control.
Both the elderly and the middle‐aged are important target populations for treating ISH. In NHANES III, more than one half of hypertensive individuals between ages 55 and 60 have ISH. Lower prevalence figures may have been reported in the past, as prior definitions of ISH were limited to SBP of >160 mm Hg and DBP of <90 mm Hg. However, even borderline ISH is associated with an approximate doubling of cardiovascular risk in women, 29 and guidelines recommend that it be treated.
CONCLUSIONS
In NHANES III, SBP control rates were uniformly worse than DBP control rates. This was true irrespective of gender, race, ethnicity, or treatment status. The prevalence of ISH was greater than 50% among all individuals with hypertension in the 55–60‐year age group and increased with age thereafter. A greater emphasis on SBP is clearly needed to improve population blood pressure control.
References
- 1. 2000 AHA Heart and Stroke Statistical Update. American Heart Association Web site. Available at: http://www.americanheart.org/statistics/hb.html. Accessed November 1,2000. [Google Scholar]
- 2. JNC VI. The sixth report of the Joint National Committee on the Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). Arch Intern Med. 1997;157:2413–2446. [DOI] [PubMed] [Google Scholar]
- 3. Guidelines Subcommittee 1999 World Health Organization‐International Society of Hypertension Guidelines for the Management of Hypertension . J Hypertens. 1999;17:151–183. [PubMed] [Google Scholar]
- 4. Ramsay LE, Williams B, MacGregor GA, et al. Guidelines for the management of hypertension: report of the third working party of the British Hypertension Society. J Hum Hypertens. 1999:569–592. [DOI] [PubMed] [Google Scholar]
- 5. Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the U.S. adult population: results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25:305–313. [DOI] [PubMed] [Google Scholar]
- 6. National Center for Health Statistics. NHANES III data. Hyattsville, MD: U.S. Public Health Service; 1997. [Google Scholar]
- 7. National High Blood Pressure Educational Program working group . National High Blood Pressure Education Program report on hypertension in the elderly. Hypertension. 1994;23:275–285. [PubMed] [Google Scholar]
- 8. Franklin SS, Jacobs MJ, Wong ND, et al. The predominance of isolated systolic hypertension among middle‐aged and elderly U.S. hypertensives—an analysis based on NHAHES III. Hypertension. In press. [DOI] [PubMed] [Google Scholar]
- 9. O'Conner PJ, Quiter ES, Rush WA, et al. Impact of hypertension guidelines implementation on blood pressure control and drug use in primary care clinics. J Quality Improvement. 1999;2:268–277. [DOI] [PubMed] [Google Scholar]
- 10. Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–1963. [DOI] [PubMed] [Google Scholar]
- 11. Alexander M, Tekawa I, Hunkeler E, et al. Evaluating hypertension control in a managed care setting. Arch Intern Med. 1999;159:2673–2677. [DOI] [PubMed] [Google Scholar]
- 12. Paramore LC, Halpern MT, Lapuerta P, et al. The impact of poorly controlled hypertension on healthcare resource utilization and cost. Am J Managed Care. 2001;7:389–398. [PubMed] [Google Scholar]
- 13. Hyman DJ, Pavlick VN. Self‐reported hypertension treatment practices among primary care physicians. Arch Intern Med. 2000;160:2281–2286. [DOI] [PubMed] [Google Scholar]
- 14. Oliveria S, Lapuerta P, McCarthy B, et al. Physician knowledge and barriers to the effective management of uncontrolled Hypertension. Circulation. 2000;102:4108. [DOI] [PubMed] [Google Scholar]
- 15. Asch SM, Kerr EA, Lapuerta P, et al. A new approach for measuring quality of care for women with hypertension. Arch Intern Med. In press. [DOI] [PubMed] [Google Scholar]
- 16. Lloyd‐Jones DM, Evans JC, Larson MG, et al. Differential control of systolic and diastolic blood pressure: factors associated with lack of blood pressure control in the community. Hypertension. 2000;36:594–599. [DOI] [PubMed] [Google Scholar]
- 17. Burt VL, Cutler JA, Higgins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult U.S. population. Hypertension. 1995;26:60–69. [DOI] [PubMed] [Google Scholar]
- 18. Cushman WC. The clinical significance of systolic hypertension. Am J Hypertens. 1998;11;182S–185S. [DOI] [PubMed] [Google Scholar]
- 19. O'Donnell CJ, Kannel WB. Cardiovascular risks of hypertension: Lessons from observational studies. J Hypertens. 1998;16(suppl 6):S3–S7. [PubMed] [Google Scholar]
- 20. Ogden LG, Jiang H, Lydick E, et al. Long‐term absolute benefit of lowering blood pressure in hypertensive patients according to the JNC‐VI risk stratification. Hypertension. 2000;35:539–543. [DOI] [PubMed] [Google Scholar]
- 21. Izzo JI, Levy D, Black HR. Clinical advisory statement: importance of systolic blood pressure in older Americans. Hypertension. 2000;35:1021–1024. [DOI] [PubMed] [Google Scholar]
- 22. Hansson L, Zsancheth A, Caruthers SG, et al., on behalf of the HOT Study Group . Effects of intensive blood pressure lowering and low‐dose aspirin in patients with hypertension: principle results of the Hypertension Optimal Treatment (HOT) trial. Lancet. 1998;351:1755–1762. [DOI] [PubMed] [Google Scholar]
- 23. Black HR, Elliot WG, Neaton JD, et al. Baseline characteristics of the 16,605 patients in the CONVINCE study. J Hypertens. 1999;17:S201. [Google Scholar]
- 24. Cushman WC, Black HR, Probstfield, JL ; et al., for the ALLHAT Research Group . Blood pressure control in the Antihypertensive and Lipid Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) [abstract]. Am J Hypertens. 1998;11:17A. [Google Scholar]
- 25. Swales JD. Current clinical practice in hypertension: the EISBERG (Evaluation and Intervention for Systolic Blood Pressure Elevation—Regional and Global) project. Am Heart J. 1999;138:S231–S237. [DOI] [PubMed] [Google Scholar]
- 26. Shah BV, Barnwell BG, Bieler GS. SUDAAN Users' Manual. Release 7.5, Research Triangle Park. Cary, NC: Research Triangle Institute; 1997. [Google Scholar]
- 27. SAS Institute . SAS Procedures Guide, version 6.12. 3rd ed, Cary, NC: SAS Institute; 1995. [Google Scholar]
- 28. Population Estimates Program, Population Division, U.S. Census Bureau . Internet release date: April 11, 2000 Revised date: June 28, 2000. Available at: http://www.census.gov/population/www/estimates/uspop.html. Accessed December 1, 2000.
- 29. Jackson EA, Buring JE, Ridker PM, et al. Borderline isolated systolic hypertension and risk of cardiovascular disease in women [abstract]. Paper presented at: 40th Annual Conference on Cardiovascular Disease Epidemiology and Prevention; March 2, 2000; San Diego, CA. [Google Scholar]
- 30. Lapuerta P, L'Italien GJ. Awareness, treatment and control of blood pressure in the United States. J Hypertens. 1999;17(suppl3):S188. [Google Scholar]


