Abstract
Background
Recent guidelines have acknowledged that thrombolysis decreases mortality from acute myocardial infarction (AMI) independently of age. The purpose of this study was to determine the age-related rates of thrombolytic administration and in-hospital mortality and the variables related to the use of thrombolytic therapy for patients with AMI.
Methods
A prospective cohort analysis involved a registry of 44 acute care Quebec hospitals that enrolled 3741 patients with AMI between January 1995 and May 1996. The main outcomes of interest were crude and adjusted age-related in-hospital mortality rates and rates of use of thrombolytic therapy.
Results
In-hospital mortality rates increased dramatically with age from 2.1% in patients with AMI who were less than 55 years of age to 26.3% in those who were 85 years of age or older. Overall, 35.8% of the patients received thrombolysis. There was a pronounced inverse gradient in the use of thrombolysis with age, ranging from 46.2% in the youngest age group (< 55 years) to 9.5% in the oldest group (≥ 85 years). After adjustment for potential confounders, the older patients remained significantly less likely to receive thrombolytic therapy. Compared with patients who were less than 55 years of age, the odds ratio of receiving thrombolytic therapy was 0.68 (95% confidence interval [CI] 0.52–0.89) for patients aged 65–74 years, 0.48 (95% CI 0.35–0.65) for patients aged 75–84 years and 0.13 (95% CI 0.06–0.26) for patients aged 85 years or more. Other variables related to thrombolytic therapy were diabetes (odds ratio [OR] 0.77, 95% CI 0.59–1.00), cerebrovascular disease (OR 0.46, 95% CI 0.30–0.72), angina (OR 0.73, 95% CI 0.56–0.95), typical chest pain (OR 2.56, 95% CI 1.88–3.47), ST elevation (OR 8.93, 95% CI 7.24–11.00), Q wave MI (OR 5.26, 95% CI 4.20–6.60) and increased length of time between onset of symptoms and arrival at hospital.
Interpretation
Age is an important independent predictor of in-hospital mortality and lower thrombolytic use following AMI. Other studies are required to further evaluate the appropriateness of thrombolytic therapy for elderly patients.
Despite a significant reduction in the overall age-adjusted mortality rates due to cardiovascular disease in the last 25 years, acute myocardial infarction (AMI) continues to be a leading cause of mortality, especially in elderly patients.1,2 The in-hospital case-fatality rate among elderly patients has been reported to be up to 9 times higher than that for patients aged less than 65 years.3
Several large randomized trials have confirmed the efficiency of thrombolytic therapy in reducing short- and long-term mortality from AMI.4,5,6,7 The ISIS-2 trial first demonstrated this benefit for those over the age of 70 years.4 However, an overview of mortality at 5 weeks in the 9 largest trials by the Fibrinolytic Therapy Trialists' Collaborative Group did not confirm a survival advantage for thrombolysis in patients over the age of 75 years.8 In this overview, the small sample of elderly patients may have limited its power to detect any meaningful differences. Faced with these limited data, it is, therefore, not surprising that clinicians and even practice guidelines are not uniform in their recommendations concerning thrombolytic therapy for elderly patients.9,10,11,12 Earlier studies have shown a marked difference among age groups in the likelihood of their receiving thrombolytic therapy but have not adequately considered potential confounders.13,14,15,16 There appear to be few Canadian data concerning this question.
The purpose of this study was, first, to examine the recent age-related in-hospital AMI mortality rate and its determinants in a large cohort of consecutive patients and, second, to examine age-related differences in the use of thrombolytic therapy for patients with AMI and the variables responsible for these variations.
Methods
Forty-four (52%) of the 85 Quebec acute care hospitals agreed to participate in this prospective registry. The participating hospitals represented the general distribution of the province's hospitals in that they included urban, rural, tertiary and community institutions. Other characteristics of the registry have been described elsewhere.17 The population studied consisted of 8917 consecutive patients admitted to the emergency department of each participating hospital with a suspected acute coronary syndrome. The data were prospectively collected from January 1995 to May 1996. Local approval was obtained to collect these anonymous data in compliance with local ethics guidelines.
When a patient was admitted to the emergency department, data were collected by the attending physician on a 1-page questionnaire that included questions about age, sex, medical history, risk factors and comorbidities, duration of time between the onset of acute coronary symptoms and arrival at the emergency department, electrocardiographic data and symptoms on arrival. Information concerning the administration of thrombolytic therapy, final diagnosis and in-hospital mortality was ascertained at hospital discharge through a systematic chart review by trained and designated nurse coordinators at each centre.
Patients with missing demographic data (age or sex, or both) were excluded from the analysis. Other missing data (5%–8% for all variables, except for time from onset of symptoms to arrival at the emergency department [33.3%]) were not excluded from the logistic regression analyses: instead, for every variable that had missing values, “missing” was considered to be another response category. Thus, we assessed the potential confounding influence of missing values on the estimated effects of the other variables.18
The simultaneous effect of several potentially confounding variables that might influence the use of thrombolytic agents was adjusted for by means of multivariate logistic regression analysis. Age was divided into 5 groups: younger than 55 years of age, 55–64 years, 65–74 years, 75–84 years and 85 years or older. The independent variables controlled for in the regression analyses were age group, sex, diabetes, hypertension, history of cerebrovascular disease, coronary artery disease and relevant interventions (angina, AMI, percutaneous transluminal coronary angioplasty and coronary artery bypass grafting), symptoms on admission (typical versus atypical chest pain, cardiogenic shock), electrocardiographic data (anterior versus inferior or posterior, ST elevation of 1 mm or more, left bundle branch block), time between onset of symptoms and arrival at hospital (< 3 hours, 3 to < 6 hours, 6 to < 9 hours, 9 to < 12 hours and ≥ 12 hours), type of AMI (Q wave versus non-Q wave) and tertiary (with on-site catheterization laboratory) versus non–tertiary care hospital. The χ2 test was used to compare discrete variables.
As a first step, we determined the univariate relationship between candidate variables and the use of thrombolytic therapy. All variables associated with thrombolytic therapy in which the p value was less than 0.20 were included in the initial multivariate model. Clinically relevant variables with a p value greater than 0.20 were also included.19 A nonautomated backward selection among the candidate variables was performed and those with a p value that was less than 0.10 were retained. Variables associated with in-hospital mortality were also determined by multiple logistic regression using the same methodology. Smoking status (current versus not current smoker), peripheral vascular disease and the type of treatment (thrombolytic versus no thrombolytic therapy) were added to the candidates' variables for the in-hospital mortality analyses. The results are expressed as odds ratios with 95% confidence intervals unless otherwise specified.
Results
Sample description
During the study period, data were collected from 8917 patients admitted with suspected acute coronary syndromes. A final diagnosis of AMI was made in 3741 patients. Patients treated with primary coronary angioplasty (47 patients, 1.3%) and those with missing data on sex or age (82 patients, 2.2%) were excluded from the analysis, leaving a sample of 3612 patients.
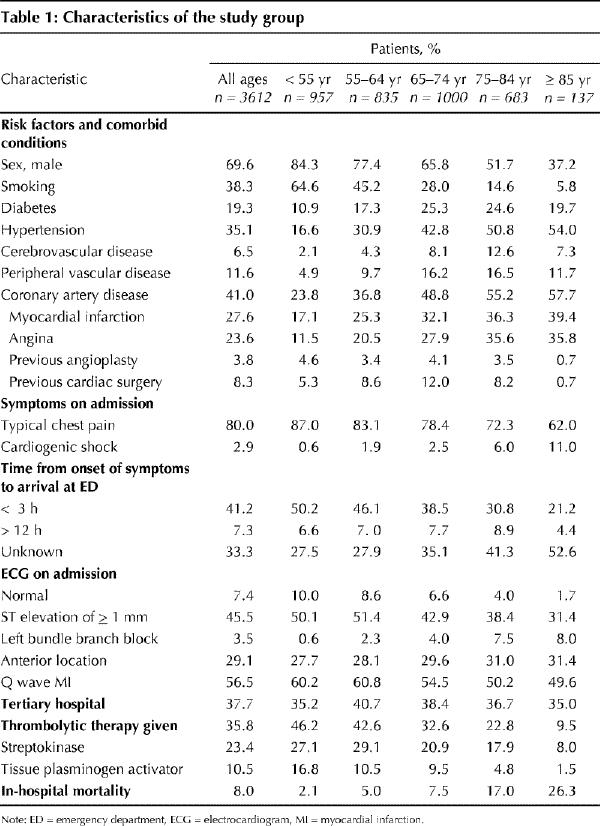
Patient characteristics according to age group are presented in Table 1. The age distribution was as follows: patients aged less than 55 years, 26.5%; 55–64 years, 23.1%; 65–74 years, 27.7%; 75–84 years, 18.9%; 85 years or more, 3.8%. Older patients were less likely to be male and smokers and were more likely to have had a diagnosis of hypertension or coronary artery disease before their admission to hospital. The highest incidence of diabetes (25.3%) was observed in the group aged 65–74 years. The incidence of cerebrovascular disease (12.6%) and peripheral vascular disease (16.5%) reached a maximum in the group aged 75–84 years. Older patients were less likely to present with typical chest pain and were more likely to be in cardiogenic shock on admission. Only 21.2% of patients aged 85 years or more presented at the emergency department less than 3 hours after the onset of symptoms compared with 50.2% of patients less than 55 years of age. Furthermore, the time between the onset of symptoms and arrival at the emergency department was not reported in 52.6% of patients aged 85 years or more compared with 27.5% of patients less than 55 years of age. The initial electrocardiograms of the oldest patients were less likely to be normal (1.7% v. 10.0%), to present ST elevation (31.4% v. 50.1%) or a Q wave (49.6% v. 60.2%) and were more likely to present left bundle branch block (8.0% v. 0.6%) compared with those of the youngest group.
Table 1
In-hospital mortality
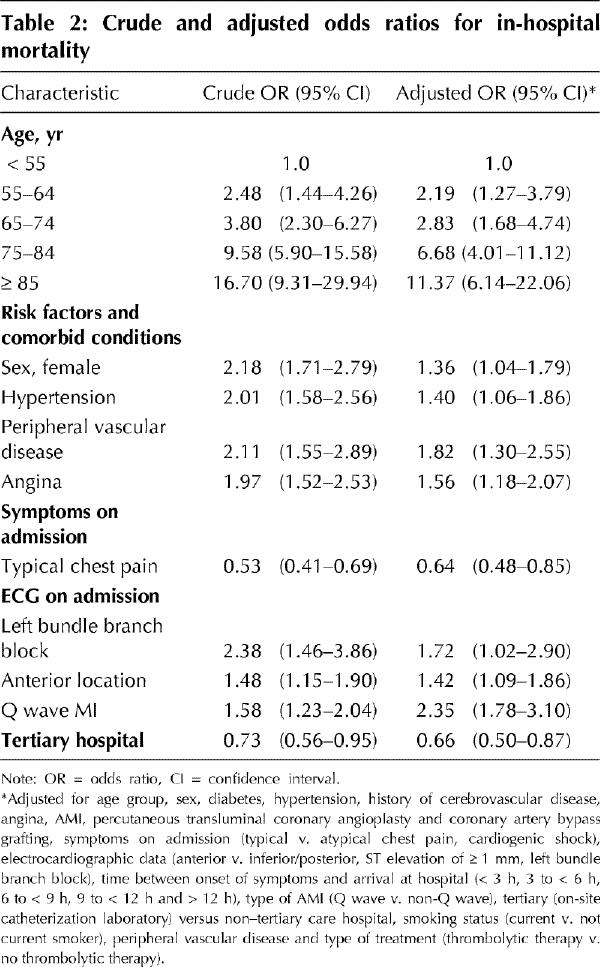
The in-hospital mortality rate increased dramatically with age, from 2.1% in patients less than 55 years of age to 26.3% for patients aged 85 years or more (Table 1). In a multivariate analysis, age remained a strong predictor of in-hospital mortality. Compared with patients aged less than than 55 years, the adjusted odds ratio for in-hospital mortality was 6.68 (95% CI 4.01–11.12) for patients aged 75–84 years and 11.37 (95% CI 6.14–22.06) for patients aged 85 years or more (Table 2). Other variables associated with an increased in-hospital mortality rate were being female, hypertension, peripheral vascular disease, pre-existing angina, left bundle branch block, anterior MI and a Q wave MI. Patients presenting with typical chest pain and those initially admitted to a tertiary center had a lower in-hospital mortality rate.
Table 2
In a univariate analysis, the use of thrombolytic therapy showed a reduction in the mortality rate (crude odds ratio 0.70, 95% CI 0.54–0.92) that did not persist in the multivariate analysis.
Thrombolytic therapy according to age group
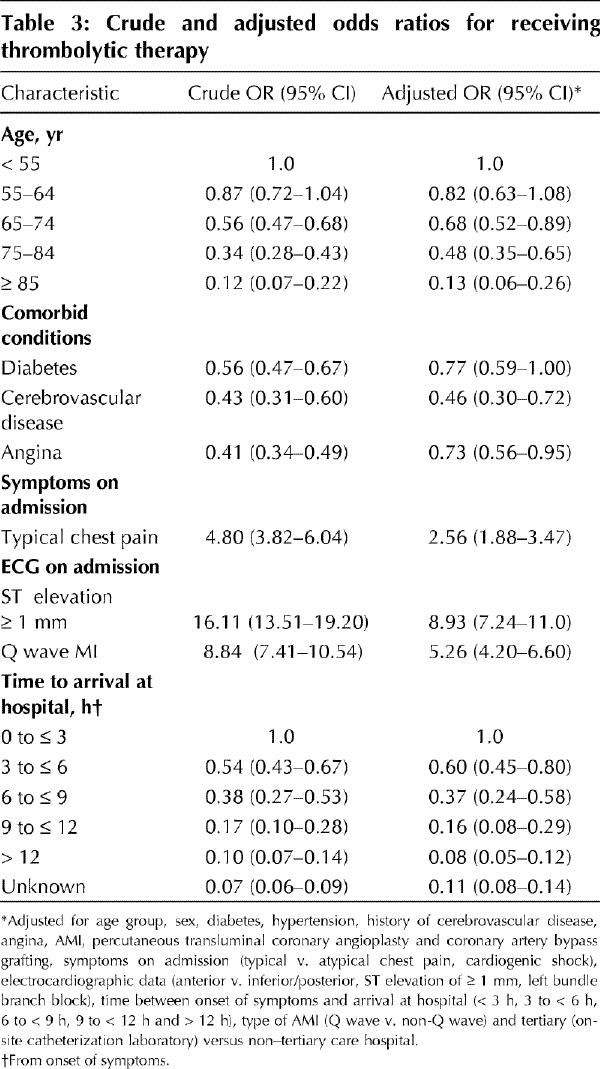
Overall, 1293 (35.8%) patients received a thrombolytic agent (Table 1). There was a marked decrease in the use of thrombolytic agents with increasing age: they were administered to 46.2% of patients aged less than 55 years, 42.6% aged 55–64 years, 32.6% aged 65–74 years, 22.8% aged 75–84 years and 9.5% aged 85 years or more (p < 0.001). After adjustment for other potentially confounding variables, older patient groups were found to be significantly less likely to receive thrombolytic therapy (Table 3). Compared with patients less than 55 years of age, the adjusted odds ratio of receiving thrombolytic therapy decreased to 0.68 (95% CI 0.52–0.89) for patients aged 65–74 years, to 0.48 (95% CI 0.35–0.65) for patients aged 75–84 years and to 0.13 (95% CI 0.06–0.26) for patients aged 85 years or more. There was no statistically significant difference in the use of thrombolytic therapy between patients aged less than 55 years and those aged 55–64 years. Diabetes, cerebrovascular disease, pre-existing angina and increased or unknown time between onset of symptoms and arrival at hospital were the other variables associated with a lower rate of use of thrombolytic therapy. Typical chest pain, ST elevation and Q wave MI were the variables associated with increased use of thrombolytic therapy.
Table 3
In order to identify patients who were ideal candidates for thrombolytic therapy, we selected the subgroup of 1143 patients who had ST elevation, no history of cerebrovascular disease or absolute contraindication to thrombolytic therapy and had a time of less than 12 hours between onset of symptoms and arrival at hospital. According to these criteria, 39.5% of patients aged less than 55 years were ideal candidates for thrombolytic therapy; this percentage decreased significantly to 28.8% in the group of patients aged 65–74 years, to 20.2% in those aged 75–84 years and to 16.1% in patients aged 85 years or more (Fig. 1). Among these 1143 ideal candidates, 927 (81.1%) received thrombolytic therapy. Compared with the youngest group of patients, the odds ratio of receiving thrombolytic therapy was 0.68 (95% CI 0.45–1.02) for patients aged 65–74 years, 0.38 (95% CI 0.24–0.61) for those aged 75–84 years and 0.10 (95% CI 0.04–0.24) for patients aged 85 years or more.
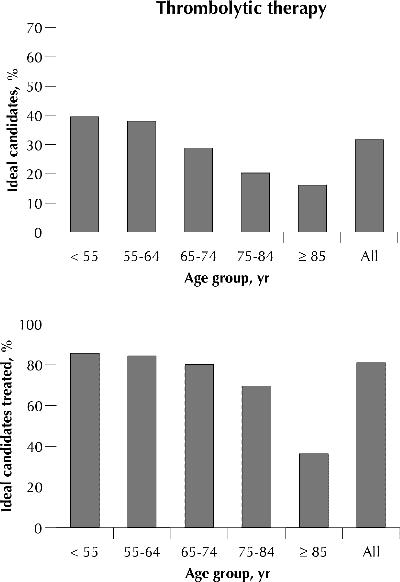
Fig. 1: Patients who were ideal candidates for thrombolytic therapy (ST elevation, no history of cerebrovascular disease and no contraindication to thrombolytic therapy, and time between onset of symptoms and arrival at hospital was less than 12 hours) (top). Patients among those ideal candidates who received thrombolytic therapy (bottom).
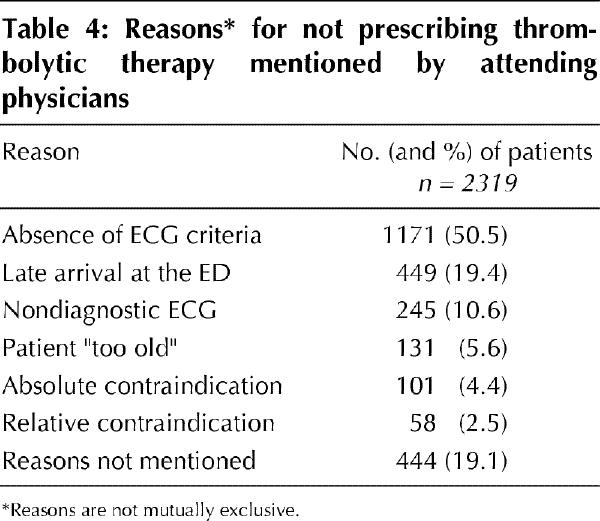
When thrombolytic therapy was not administered, the treating physician was asked to select the reason(s) from a list (Table 4). As expected, absence of electrocardiographic criteria (50.5%) was the most common reason, followed by late arrival (median 12.3 hours, 25th–75th quartile 6.4–18.6 hours) at the emergency department (19.4%). In 5.6% of cases, the patient was judged to be “too old” to receive thrombolytic therapy (mean age 80.9 years, standard deviation 7.6 years). Absolute and relative contraindications to receiving thrombolytic therapy were the reasons in 4.4% and 2.5% of cases respectively, and in 19.1% of cases other reason(s) not otherwise mentioned justified not using thrombolytic therapy.
Table 4
Interpretation
Our study shows a progressive age-related increase in in-hospital mortality after AMI in the thrombolytic era that persists even after multivariate analysis. Age was the most important independent predictor of in-hospital mortality, and the other predictors were consistent with the results of previous studies.2,3,14,15,16
Some of these predictors do deserve further comment. First, the adjusted lower in-hospital mortality rate in the tertiary care hospitals, despite the exclusion of patients treated with primary angioplasty, is intriguing. However, given the nonrandomized nature of the study and the numerous variables examined, this may not represent a true association and needs to be confirmed through future studies.
The lack of association between thrombolytic therapy and improved survival, which contrasted with the findings of randomized thrombolytic trials, was most interesting.2,4,5,6,20,21,22 Our study was an observational registry study and, despite adjustment for potential confounders, it is highly likely that a selection bias (indication bias) is at play, or that the lack of association could be a result of chance. Nevertheless, it should be noted that another recent observational study found not only a lack of benefit as we did, but also a higher 30-day mortality rate among elderly patients receiving thrombolysis (15.4% v. 18.0%, p = 0.003).23
The proportion of patients with AMI eligible for thrombolytic therapy in previous studies has ranged from less than 10% to nearly 50%.24 Our study showed that the overall use of thrombolytic therapy was 35.8%. Among those deemed ideal candidates for treatment, 81.1% received thrombolytic therapy (Fig. 1). Differences in health care and socioeconomic factors in the use of invasive cardiac procedures in Canada compared with the United States may influence the approach to AMI.25,26 For example, primary angioplasty, which is an alternative to thrombolysis, was used infrequently (1.3%) in our Canadian study and may contribute to our greater use of thrombolytic therapy.
We also observed a progressive age-related reduction in the use of thrombolytic therapy despite adjustment for potential eligibility. Physicians may have been influenced by other pathophysiological factors and comorbidities, which were not assessed in our study, that they might have suspected would negatively alter the delicate risk–benefit ratio of thrombolytic therapy for elderly patients. The decision to administer thrombolytic therapy to elderly patients is especially difficult because both benefits and risks are age dependent27 and are perhaps complicated by marginally conflicting Canadian and US guidelines.10,12
Other major variables associated with a reduction in the administration of thrombolytic therapy independent of age included late presentation for medical therapy, atypical chest pain, a nondiagnostic electrocardiogram, diabetes, cerebrovascular disease, pre-existing angina and non-Q wave myocardial infarction. These findings are generally concordant with practice guidelines, with the exception of those for diabetes and pre-existing angina.10,12 Patients with diabetes and ischemic heart disease are at exceedingly high risk of a poor outcome and, consequently, should have a large absolute gain from thrombolysis, but unfortunately in our cohort these patients had a reduced probability of receiving such therapy.
An advantage of our study is that it considered a cohort of prospective and consecutive patients who were admitted for AMI to 44 acute care hospitals that covered the spectrum of urban, rural, tertiary and community institutions. Consequently, the results are probably representative of current Canadian practice patterns. Furthermore, more detailed and validated information on clinical variables was available than with a databank analysis.
The main limitation of our study is that some potentially important variables in the process of deciding whether to administer thrombolytic therapy to elderly patients were not collected. For instance, poor functional autonomy, low quality of life prior to hospital admission, risk of cerebral hemorrhage and major cognitive impairment were not measured. In a substantial number of patients not receiving thrombolysis (19.1%), the reasons were not specified (Table 4) and may reflect the presence of residual confounders.
Our study has demonstrated the crucial role of age in determining in-hospital mortality and the selection of thrombolytic therapy. We have established the decreasing probability that elderly patients will receive thrombolysis, but whether this represents an appropriate clinical judgement or an inappropriate care gap is an important question that deserves to be clarified in future studies.
Footnotes
This article has been peer reviewed.
Acknowledgements: We thank Leah DenBesten for technical assistance in the preparation of the manuscript.
Members of the Executive of the Quebec Acute Coronary Care Working Group are listed at the end of the article.
This study was supported by grants from the Fonds de recherche en santé du Québec and by Genentech Canada.
Competing interests: This study was supported in part by a grant from Genentech Canada.
Reprint requests to: Dr. Normand Racine, Institut de Cardiologie de Montréal, 5000 rue Bélanger E, Montréal QC H1T 1C8; fax 514 593-2575; racin@videotron.ca
References
- 1.Udvarhelyi IS, Gatsonis C, Epstein AM, Pashos CL, Newhouse JP, McNeil BJ. Acute myocardial infarction in the Medicare population. Process of care and clinical outcomes. JAMA 1992;268(18):2530-6. [PubMed]
- 2.Maggioni AP, Maseri A, Fresco C, Franzosi MG, Mauri F, Santoro E, et al. Age-related increase in mortality among patients with first myocardial infarctions treated with thrombolysis. The Investigators of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI-2). N Engl J Med 1993;329:1442-8. [DOI] [PubMed]
- 3.Gurwitz JH, Goldberg RJ, Chen Z, Gore JM, Alpert JS. Recent trends in hospital mortality of acute myocardial infarction — the Worcester Heart Attack Study. Have improvements been realized for all age groups? Arch Intern Med 1994;154:2202-8. [PubMed]
- 4.Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet 1988;ii:349-60. [PubMed]
- 5.GISSI-2: a factorial randomised trial of alteplase versus streptokinase and heparin versus no heparin among 12,490 patients with acute myocardial infarction. Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico. Lancet 1990;336:65-71 [PubMed]
- 6.ISIS-3: a randomised comparison of streptokinase vs tissue plasminogen activator vs anistreplase and of aspirin plus heparin vs aspirin alone among 41,299 cases of suspected acute myocardial infarction. ISIS-3 (Third International Study of Infarct Survival) Collaborative Group. Lancet 1992;339(8796):753-70. [PubMed]
- 7.Collins R, Peto R, Baigent C, Sleight P. Aspirin, heparin, and fibrinolytic therapy in suspected acute myocardial infarction. N Engl J Med 1997;336:847-60. [DOI] [PubMed]
- 8.Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Lancet 1994;343:311-22. [PubMed]
- 9.Ryan TJ, Anderson JL, Antman EM, Braniff BA, Brooks NH, Califf RM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol 1996;28(5):1328-428. [DOI] [PubMed]
- 10.Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, et al. 1999 update: ACC/AHA Guidelines for the management of patients with acute myocardial infarction: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). Circulation 1999;100(9):1016-30. [DOI] [PubMed]
- 11.Cairns J, Armstrong P, Belenkie I, Hirsh J, Johnstone D, Knudtson M, et al. Canadian Consensus Conference on Coronary Thrombolysis — 1994 update. Can J Cardiol 1994;10(5):517-21. [PubMed]
- 12.Canadian Consensus Conference on Coronary Thrombolysis — 1994 recommendations. National Health Research and Development Program. Can J Cardiol 1994;10(5):522-9. [PubMed]
- 13.Pfeffer MA, Moye LA, Braunwald E, Basta L, Brown EJ, Cuddy TE, et al. Selection bias in the use of thrombolytic therapy in acute myocardial infarction. The SAVE Investigators. JAMA 1991;266:528-32. [PubMed]
- 14.Gurwitz JH, Gore JM, Goldberg RJ, Rubison M, Chandra N, Rogers WJ. Recent age-related trends in the use of thrombolytic therapy in patients who have had acute myocardial infarction. National Registry of Myocardial Infarction. Ann Intern Med 1996;124:283-91. [DOI] [PubMed]
- 15.Chandra H, Yarzebski J, Goldberg RJ, Savageau J, Singleton C, Gurwitz JH, et al. Age-related trends (1986–1993) in the use of thrombolytic agents in patients with acute myocardial infarction. The Worcester Heart Attack Study. Arch Intern Med 1997;157:741-6. [PubMed]
- 16.Krumholz HM, Murillo JE, Chen J, Vaccarino V, Radford MJ, Ellerbeck EF, et al. Thrombolytic therapy for eligible elderly patients with acute myocardial infarction. JAMA 1997;277(21):1683-8. [PubMed]
- 17.Brophy JM, Diodati JG, Bogaty P, Theroux P. The delay to thrombolysis: an analysis of hospital and patient characteristics. CMAJ 1998;158(4);475-80. Abstract available: www.cma.ca/cmaj/vol-158/issue-4/0475.htm [PMC free article] [PubMed]
- 18.Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med 1993;118:201-10. [DOI] [PubMed]
- 19.Hosmer DW, Lemeshow S. Applied logistic regression. New York (NY): John Wiley and Sons; 1989. p. 82-134.
- 20.ISAM (Intravenous Streptokinase in Acute Myocardial Infarction) Study Group. A prospective trial of intravenous streptokinase in acute myocardial infarction ISAM): mortality, morbidity, and infarct size at 21 days. N Engl J Med 1986;314:1465-71. [DOI] [PubMed]
- 21.AIMS (APSAC Intervention Mortality Study) Trial Study Group. Effects of intravenous APSAC on mortality after acute myocardial infarction: preliminary report of a placebo-controlled clinical trial. Lancet 1988;i:545-9. [PubMed]
- 22.Wilcox RG, von der Lippe G, Olsson CG, Jensen G, Skene AM, Hampton FR for the ASSET (Anglo-Scandinavian Study of Early Thrombolysis) Study Group. Trial of tissue plasminogen activator for mortality reduction in acute myocardial infarction (ASSET). Lancet 1988:ii:525-30. [DOI] [PubMed]
- 23.Thiemann DR, Coresh J, Schulman SP, Gerstenblith G, Oetgen WJ, Powe NR. Lack of benefit for intravenous thrombolysis in patients with myocardial infarction who are older than 75 years. Circulation 2000;101:2239-46. [DOI] [PubMed]
- 24.Muller DW, Topol EJ. Selection of patients with acute myocardial infarction for thrombolytic therapy. Ann Intern Med 1990;113:949-60. [DOI] [PubMed]
- 25.Pilote L, Racine N, Hlatky MA. Differences in the treatment of myocardial infarction in the United States and Canada. A comparison of two university hospitals. Arch Intern Med 1994;154:1090-6. [PubMed]
- 26.Rouleau JL, Moye LA, Pfeffer MA, Arnold JM, Bernstein V, Cuddy TE, et al. A comparison of management patterns after acute myocardial infarction in Canada and the United States. The SAVE investigators. N Engl J Med 1993;328(11):779-84. [DOI] [PubMed]
- 27.Selker HP, Griffith JL, Beshansky JR, Schmid CH, Califf RM, D'Agostino RB, et al. Patient-specific predictions of outcomes in myocardial infarction for real-time emergency use: a thrombolytic predictive instrument. Ann Intern Med 1997;127(7):538-66. [DOI] [PubMed]


