Abstract
This study assessed the prognostic value of ambulatory vs. clinic blood pressure measurement in 688 hypertensives who had undergone pretreatment 24‐hour intra‐arterial ambulatory blood pressure monitoring. A total of 157 first events were recorded over a follow‐up period of 9.2±4.4 years. Ambulatory systolic or diastolic blood pressure parameters (whether 24‐hour mean, daytime mean, or nighttime mean) or ambulatory pulse pressure provided independent prognostic information in conjunction with clinical variables. The most predictive models contained the ambulatory systolic blood pressure parameters. Age, male gender, South Asian origin, diabetes mellitus, and previous cardiovascular disease were additional independent predictors of events. In a subgroup of 295 uncomplicated patients, 24‐hour ambulatory pulse pressure was an independent predictor of left ventricular mass index and maximal carotid intima‐media thickness. Baseline clinic blood pressure parameters did not provide independent information for the prediction of events or target organ damage. Therefore, in this study, ambulatory blood pressure proved to be superior to clinic measurement for cardiovascular risk stratification. However, the routine use of ambulatory blood pressure monitoring is not currently recommended, mainly because of a lack of outcome trials based on the treatment of ambulatory blood pressure levels.
The management of hypertension is now the leading indication both for visits to physicians and the use of prescription drugs in the United States. 1 However, the optimal method of blood pressure measurement remains unclear. Conventional sphygmomanometry remains, even today, the most widely used technique for measuring blood pressure. Although blood pressure measured in this way is an established risk factor for cardiovascular disease, 2 there is evidence to suggest that isolated clinic blood pressure measurements may not be adequately representative of the daily blood pressure load away from the medical environment. It was shown in 1940 that blood pressure measured at home was lower than in the presence of a doctor, 3 and much interest since then has focused on this so‐called white‐coat effect. The goal of excluding this phenomenon in particular has stimulated a search for alternative strategies of blood pressure measurement with the potential for improving cardiovascular risk stratification.
The technique of ambulatory blood pressure monitoring first became a practical reality more than 30 years ago. 4 , 5 Its attraction lies in its ability to acquire automatic blood pressure measurements throughout the day and night in familiar surroundings. It therefore eliminates the white‐coat effect and potentially offers a more valid assessment of an individual's true blood pressure level by taking multiple readings during routine daily activities. 6 The intra‐arterial method of ambulatory blood pressure monitoring, although impractical and expensive in the practice setting, is a powerful research tool and remains the reference standard by which noninvasive monitors are validated. 7 It provides beat‐to‐beat measurements of blood pressure during a 24‐hour period in truly ambulant patients, and therefore represents the most accurate measure of the daily hemodynamic burden imposed by blood pressure. In contrast, noninvasive auscultatory and oscillometric monitors rely on intermittent recordings at predetermined time intervals, and these may not be accurate during unrestricted physical activity.
Numerous cross‐sectional studies have shown ambulatory blood pressure to be more closely related to target organ damage, than clinic blood pressure measurements. 8 Left ventricular hypertrophy and carotid atherosclerosis are prognostically important forms of target organ damage, as they both confer an increased risk of subsequent cardiovascular events. 9 , 10 , 11 , 12 , 13 In otherwise uncomplicated patients, they may therefore be considered surrogate endpoints of overt cardiovascular disease.
Longitudinal data evaluating the relative abilities of ambulatory and clinic blood pressure to predict the development of cardiovascular complications are limited. Therefore, the main objective of this study was to compare the prognostic value of ambulatory vs. clinic blood pressure measurement for the development of cardiovascular morbid events and, in a subgroup of uncomplicated patients, to predict the long‐term development of left ventricular hypertrophy and carotid atherosclerosis. A secondary objective was to assess the ability of other risk factors to predict these cardiovascular end points.
METHODS
The hypertension database in our institution consists of 723 patients who were subjected to 24‐hour intra‐arterial ambulatory blood pressure monitoring from January 1, 1979 to January 1, 1993. 14 The racial composition of the patient population studied reflects the local population of the London boroughs of Harrow, Brent, and Ealing, which includes mainly white subjects, but also South Asian (Indian subcontinent) and African‐Caribbean subjects. All patients were originally referred for the management of hypertension based on a persistently elevated clinic blood pressure taken during a period of weeks to months in a primary care setting. At each hospital visit, a single blood pressure measurement was taken by a nurse or technician using the conventional auscultatory technique after 5–10 minutes of semisupine rest in a warm environment. The point of disappearance of auscultatory sounds was taken as the diastolic blood pressure. This was followed by a full medical history and physical examination by a physician. Secondary causes of hypertension were excluded, as far as possible, in all patients by measurement of serum urea, creatinine, and electrolytes, urinary catecholamines, chest x‐ray, and more recently, intravenous renal digital subtraction angiography. Baseline clinic blood pressure was taken as the mean of two or more untreated readings at separate clinic visits in the 4 weeks before or after the intra‐arterial study. Those in whom clinic systolic blood pressure was ≥140 mm Hg or diastolic blood presure ≥90 mm Hg were requested to undergo 24‐hour intra‐arterial ambulatory blood pressure monitoring within 2 months. Antihypertensive medication had either not been started or had been withdrawn in the 8 weeks preceding intra‐arterial blood pressure monitoring.
The method of 24‐hour intra‐arterial ambulatory blood pressure monitoring was approved by the hospital ethics committee and patients gave written informed consent prior to the procedure. General practitioners were informed of the results of the test and antihypertensive therapy was generally recommended if 24‐hour ambulatory systolic blood pressure was ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg. The treatment of lower ambulatory blood pressure readings was more conservative and discretionary. Subsequent assessment of blood pressure control and treatment was largely left to the individual family practitioners or hospital physicians and was based on clinic blood pressure measurements in keeping with standard clinical practice.
Intra‐arterial Blood Pressure Monitoring
The technique of intra‐arterial blood pressure recording used in this laboratory has been well documented, 15 as has the method of analysis. 16 Blood pressure was recorded from a fine brachial artery cannula with a specially designed transducer/perfusion unit and an Oxford Medilog Mark I™ tape recorder. The equipment was designed so that patients were fully ambulant and able to carry out their normal daily activities away from the hospital environment. The 24‐hour tape recordings were analyzed on a custom‐built hybrid computer, using a program that calculated mean hourly blood pressure and heart rate. Twenty‐four‐hour mean systolic, diastolic, and pulse pressures were calculated by averaging the 24 hourly mean readings of these parameters. Blood pressure and heart rate variability were expressed as the standard deviation of mean hourly systolic and diastolic blood pressures and heart rate, respectively. Daytime mean systolic and diastolic blood pressures were defined as the average of the hourly blood pressure readings from 6 a.m. to 10 p.m. and the nighttime mean blood pressures as those between 10 p.m. and 6 a.m. 17 The nocturnal falls in systolic and diastolic blood pressure were calculated by subtracting respective nighttime mean from daytime mean blood pressure readings.
Nondippers were defined as those who did not exhibit a reduction in mean systolic and diastolic blood pressure by at least 10% from day to night, and the remaining subjects were classified as dippers. 17 The white‐coat effect of systolic and diastolic blood pressure was defined as initial clinic blood pressure measurements minus respective daytime mean ambulatory readings.
Follow‐up Evaluation
The study patients have been intermittently reviewed over the years to record clinic blood pressure, drug therapy, and the occurrence of interim cardiovascular events. The most recent follow‐up was performed during an 18‐month period from 1994 to 1996 (Figure). To obtain complete mortality data, the dates and certified causes of interim deaths were obtained from the National Health Service Central Register (Southport, U.K.). The hospital records of all patients were also scrutinized.
Figure.
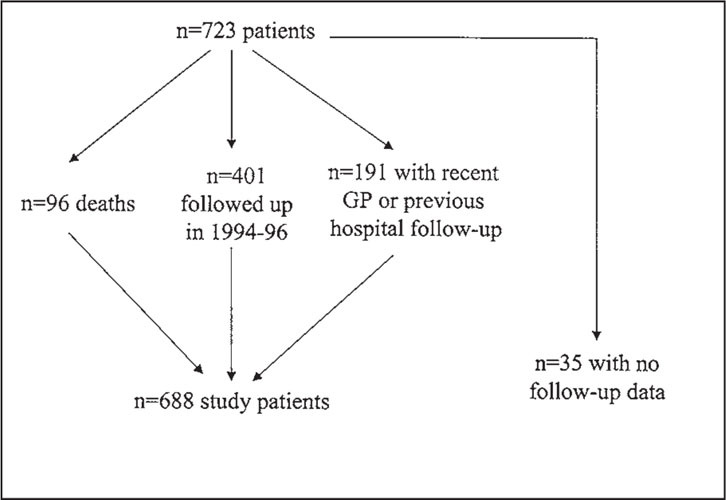
Follow‐up scheme for the 723 study patients.
Survivors were invited to attend a follow‐up evaluation for documentation of events, clinic blood pressure measurement on current treatment, serum creatinine estimation, and fasting cholesterol level. Echocardiography and carotid ultrasonography were also performed in those without a history of cardiovascular disease. Family practitioners of the nonattenders were sent a questionnaire for details of these patients. Documented events consisted of noncardiovascular death, coronary death (myocardial infarction or ischemia, ventricular fibrillation, or cardiac failure), cerebrovascular death, peripheral vascular death, nonfatal myocardial infarction, nonfatal stroke, and coronary revascularization.
Ultrasound Studies
The echocardiographic examination was performed by the same investigator using a commercially available machine. Both carotid arteries were imaged with a high‐resolution ultrasound system equipped with a mechanical sector probe. The middle and distal common carotid artery, carotid bulb, and proximal portions of the internal and external carotid arteries were systematically interrogated in short‐axis and long‐axis views for the detection of atherosclerotic plaque. A plaque was defined as a distinct area with an intima‐media thickness at least 50% greater than that of the adjacent wall and the maximal intima‐media thickness measurement (IMTmax) was used as a semiquantitative score for carotid atherosclerosis severity. In the absence of atheroma, the intima‐media thickness of the far wall of the distal common carotid artery was taken as IMTmax.
Analysis
The clinical variables analyzed included age, gender, race, body mass index, diabetes mellitus, smoking, fasting cholesterol level, and previous cardiovascular disease, along with clinic blood pressure and ambulatory blood pressure parameters. The follow‐up period was defined as the time interval between 24‐hour intra‐arterial ambulatory blood pressure monitoring and the development of a first morbid event, or last follow‐up in uncomplicated patients. Univariate and multivariate analyses were performed to determine the predictors of time to a first event. In the subgroup of uncomplicated patients, continuous clinical variables and blood pressure parameters were correlated with left ventricular mass index (LVMI) and IMTmax, and stepwise multiple regression analysis was then performed to determine the independent predictors of LVMI and IMTmax. A p value of <0.05 was considered significant.
RESULTS
The study population consisted of 688 patients (440 male, 248 female) with follow‐up data: 528 white, 106 South Asian, and 54 African‐Caribbean. A total of 157 first events were recorded during a mean follow‐up period of 9.2±4.1 years, including 32 noncardiovascular deaths, 27 coronary deaths, 10 cerebrovascular deaths, four peripheral vascular deaths, 46 nonfatal myocardial infarctions, 20 nonfatal strokes, and 18 coronary revascularization procedures.
Comparison of Demographic Data
Table I gives a comparison of the baseline demographic data in those with and without events. As expected, those with events were significantly older and had higher fasting cholesterol levels than those without events. A significantly greater proportion of males than females, smokers than nonsmokers, diabetics than nondiabetics, and those with a previous history of cardiovascular disease than those without such a history experienced a subsequent event. In addition, proportionately fewer African‐Caribbean subjects (9%) developed an end point compared to whites (23%; p<0.001) and South Asians (28%; p<0.001).
Table I.
COMPARISON OF BASELINE DEMOGRAPHIC DATA BETWEEN PATIENTS WITH AND WITHOUT EVENTS
| No Events (n=531) | Events (n=157) | p Value | |
| Age (yr) | 49±11 | 56±8 | <0.001 |
| Gender: males | 71% | 29% | <0.001 |
| females | 89% | 11% | |
| Smoking: yes | 70% | 30% | 0.002 |
| no | 82% | 18% | |
| Diabetes: yes | 34 (65%) | 18 (35%) | 0.04 |
| no | 497 (78%) | 139 (22%) | |
| Previous CVD: yes | 40% | 60% | <0.001 |
| no | 80% | 20% | |
| Body mass index (kg/m2 | 26.8±4.4 | 26.4±3.9 | NS |
| Fasting cholesterol (mmol/l) | 5.8±1.3 | 6.3±1.1 | <0.001 |
| CVD=cardiovascular disease; NS=not significant | |||
Comparison of Blood Pressure Parameters
Table II shows a comparison of the baseline blood pressure data in those with and without events. As expected, all components of systolic blood pressure and pulse pressure (initial clinic, 24‐hour mean, daytime mean, and nighttime mean) were significantly greater in those who experienced a morbid event. The most discriminatory diastolic blood pressure parameter between the two groups was nighttime mean diastolic blood pressure. Those with events had a significantly greater proportion of nondippers and lesser nocturnal falls in both systolic and diastolic blood pressure compared to those without events. Heart rate variability was also significantly lower in those who developed a morbid end point.
Table II.
COMPARISON OF BASELINE HEMODYNAMIC DATA BETWEEN PATIENTS WITH AND WITHOUT EVENTS
| No Events (n=531) | Events (n=157) | p Value | |
| Systolic BP 24‐Hour | 154±21 | 166±23 | <0.0001 |
| Daytime | 161±21 | 173±23 | <0.0001 |
| Nighttime | 138±23 | 152±25 | <0.0001 |
| Clinic | 169±22 | 180±26 | <0.0001 |
| Nocturnal fall | 23±12 | 21±13 | 0.05 |
| SD | 18±6 | 18±6 | NS |
| White‐coat | 15±20 | 14±24 | NS |
| Diastolic BP 24‐Hour | 90±13 | 93±15 | 0.02 |
| Daytime | 95±13 | 98±15 | NS |
| Nighttime | 79±14 | 83±16 | 0.001 |
| Clinic | 102±12 | 106±14 | 0.03 |
| Nocturnal fall | 17±8 | 15±9 | 0.007 |
| SD | 12±4 | 12±4 | NS |
| White‐coat | 12±14 | 13±17 | NS |
| Pulse Pressure 24‐Hour | 64±13 | 73±17 | <0.0001 |
| Daytime | 66±13 | 75±18 | <0.0001 |
| Nighttime | 59±13 | 69±18 | <0.0001 |
| Clinic | 67±18 | 74±21 | <0.0001 |
| Nondippers | 116 (21%) | 41 (26%) | 0.002 |
| Heart rate variability | 13±4 | 12±4 | 0.001 |
| BP=blood pressure; SD=standard deviation; NS=not significant | |||
Independent Predictors of Morbid Events
Certain blood pressure parameters significantly improved the prediction of events when added individually to a baseline regression model containing clinical variables. Ambulatory systolic and diastolic blood pressure parameters (whether 24‐hour mean, daytime mean, or nighttime mean) and ambulatory pulse pressure provided independent information and significantly improved the fit of the model for the prediction of events. The addition of clinic blood pressure measurements that were univariate predictors, but in multivariate analysis failed to provide independent prognostic value, did not enhance the prediction of events. Neither the measures of blood pressure and heart rate variability (including hourly standard deviations of blood pressure and heart rate, degree of nocturnal fall in blood pressure, and nondipper status) nor the white‐coat effect of systolic and diastolic blood pressure were able to provide any incremental prognostic information for the prediction of future events.
Statement A
In the regression model containing 24‐hour ambulatory systolic blood pressure, age (p<0.001), gender (p<0.001), race (South Asians vs. whites: p=0.008), diabetes (p=0.05), history of cardiovascular disease (p<0.001), and 24‐hour ambulatory systolic blood pressure (p=0.001) were independent predictors of time to a first morbid event.
Subgroup Analysis of Target Organ Damage in Uncomplicated Patients
Of the 401 patients who underwent echocardiography and carotid ultrasonography, 106 patients were excluded from the analysis for the following reasons: 70 gave a history of overt cardiovascular disease, 23 had inadequate echocardiographic or carotid ultrasound images, two had significant valvular disease, and 11 had regional wall motion abnormality indicative of underlying coronary artery disease. Therefore, an assessment of target organ damage was made in the remaining 295 patients (161 male, 134 female). At a mean follow‐up period of 10.2±3.5 years, the mean age of the group was 58.2±11.1 years, with a body mass index of 26.5±4.6 kg/m2 and serum cholesterol of 5.6±1.0 mmol/l. A positive smoking history was given by 129 patients and the mean pack‐years of smoking for the group as a whole was 7.3±13.7 years. Antihypertensive medication was being taken by 90% of the patients, of whom 54% were on monotherapy and 46% on multiple therapy. As an indication of blood pressure control, clinic systolic and diastolic blood pressures were reduced from baseline values of 166±19 mm Hg and 101±10 mm Hg, respectively, to 152±22 mm Hg and 92±11 mm Hg, respectively, at follow‐up. Correlations of continuous clinical variables and blood pressure parameters to LVMI and IMTmax are given in Table III. There was a nonsignificant trend toward higher LVMI and IMTmax in men compared to women (110±32 vs. 103±31 g/m2 [p=0.06] and 0.16±0.10 vs. 0.14±0.09 cm [p=ns], respectively).
Table III.
CORRELATION COEFFICIENTS RELATING CLINICAL VARIABLES AND BP PARAMETERS TO LEFT VENTRICULAR MASS INDEX AND CAROTID ATHEROSCLEROSIS SEVERITY
| LVMI | IMTmax | |
| (r value) | (r value) | |
| Clinical Variables | ||
| Age | 0.39 | 0.47 |
| Cholesterol | ‐ | 0.12 |
| Body mass index | 0.17 | ‐ |
| Follow‐up years | 0.30 | 0.15 |
| Pack‐years of smoking | ‐ | 0.29 |
| Systolic BP | ||
| Baseline clinic | 0.27 | 0.24 |
| 24‐hour | 0.33 | 0.32 |
| Daytime | 0.33 | 0.31 |
| Nighttime | 0.27 | 0.34 |
| Diastolic BP | ||
| Baseline clinic | 0.23 | ‐ |
| 24‐hour | 0.17 | ‐ |
| Daytime | 0.16 | ‐ |
| Nighttime | 0.14 | ‐ |
| Miscellaneous | ||
| 24‐hour pulse pressure | 0.38 | 0.48 |
| BP=blood pressure | ||
Multivariate analysis revealed age (p<0.001), gender (p<0.001), body mass index (p=0.002), follow‐up years (p=0.004), and 24‐hour systolic blood pressure (p<0.001) to be independent predictors of LVMI (R2=31%), whereas age (p<0.001), gender (p=0.04), pack‐years of smoking (p=0.004), and 24‐hour pulse pressure (p<0.001) were independent predictors of IMTmax (R2=35%). The next best blood pressure parameter to predict IMTmax was 24‐hour systolic blood pressure. Clinic systolic and diastolic blood pressure were univariate but not multivariate predictors of LVMI and IMTmax.
DISCUSSION
In general terms, the relationship of established cardiovascular risk factors to target organ damage and subsequent morbid events is imprecise. 18 Exposure to risk factors often, but not always, leads to the gradual development of target organ damage to the vasculature and myocardium, which in turn predisposes to myocardial infarction, stroke, and sudden death. Alternatively, risk factor exposure may progress to the development of a morbid event in the absence of target organ damage, and indeed target organ damage may be present in the absence of well‐defined risk factors.
In the present study, we evaluated the independent influences of a variety of demographic variables and blood pressure parameters on the development of both target organ damage and overt cardiovascular disease. Although the events data have been described elsewhere, the left ventricular mass and carotid artery data have not previously been published. Age, gender, and 24‐hour systolic or pulse pressure were independently associated with LVMI and IMTmax in the subgroup of hypertensive patients without complications and were independent predictors of subsequent morbid events in the study population as a whole. Although clinic blood pressure measurements were predictive of cardiovascular events when evaluated in isolation, they failed to provide independent prognostic information after adjustment for other clinical variables.
An important limitation of this study was the lack of a formalized protocol for the assessment of blood pressure control and for the administration of antihypertensive drug therapy. Both of these aspects of hypertension management were left entirely to the discretion of the attending physician of the hypertension clinic or to the family practitioner. Blood pressure control was based on clinic blood pressure measurements as part of standard clinical practice, as it was not considered justifiable on ethical grounds to repeat intra‐arterial blood pressure monitoring, particularly in the face of developing noninvasive technologies for ambulatory blood pressure measurement in subsequent years. In spite of the importance of the effects of antihypertensive drug therapy on events, highly significant relationships between baseline ambulatory blood pressure and subsequent risk remained, indicating only partial modification of risk by treatment in these patients. The fact that mean blood pressures were reduced to only 152/92 mm Hg suggests that the maximum benefit of the therapy was not achieved.
Although limited longitudinal data evaluating the prognostic value of ambulatory blood pressure monitoring in hypertension are available, the patient populations and methods of analysis have varied considerably, and details of drug treatment have often been inadequate or absent. Perloff et al. 19 showed that daytime ambulatory blood pressures that were higher than predicted from a regression line between ambulatory blood pressure and office blood pressure were associated with an adverse outcome. However, the use of a patient‐activated, semiautomatic, indirect blood pressure recorder did not allow the measurement of nocturnal blood pressure. In this study, adequate data on drug therapy and achieved blood pressure were lacking. It is therefore difficult to draw conclusions about these results. Two studies of 24‐hour ambulatory blood pressure monitoring, one using the noninvasive oscillometric method and the other using the intra‐arterial technique, used different cut‐off points of ambulatory blood pressure to define white‐coat and sustained hypertensives. 20 , 21 Both studies showed white‐coat hypertensives to have a relatively benign outcome, with significantly lower event rates than sustained hypertensives. The presence of white‐coat hypertension was an independent negative predictor of subsequent morbidity and mortality. A study of 86 patients with refractory hypertension showed that patients in the lowest tertile of daytime ambulatory diastolic blood pressure (<88 mm Hg) had a significantly lower rate of morbidity and less target organ damage, despite similar clinic pressures to the other two groups. 22 Data from the Systolic Hypertension in Europe trial showed that ambulatory systolic blood pressure, particularly the nighttime component, was a significant predictor of cardiovascular risk over and above conventional clinic blood pressure in untreated, older patients. 23 The only study of a general population, based in Japan, showed ambulatory blood pressure monitoring to be superior to clinic measurement for the prediction of all‐cause mortality. 24 However, the latter study is not directly applicable to western populations, given that only 13% of deaths were attributable to heart disease.
The present study provides the longest follow‐up data and evaluates ambulatory blood pressure as a continuous variable, allowing assessment of linear and nonlinear relationships with subsequent cardiovascular disease. Our findings indicate that ambulatory blood pressure monitoring yields greater prognostic information than clinic blood pressure measurements. The addition of any one of the 24‐hour mean, daytime mean, or nighttime mean ambulatory systolic or diastolic blood pressure parameters or ambulatory pulse pressure provided independent information for the prediction of all‐cause events. This partly reflects the high degree of collinearity between systolic and diastolic blood pressure making it difficult to determine the relative contribution of each of these components of blood pressure with disease risk. However, accumulating epidemiologic data suggest that systolic blood pressure may confer greater prognostic information than that conferred by diastolic blood pressure, particularly in the elderly. 25 , 26 Our results lean toward this view, with the most predictive regression models containing the ambulatory systolic blood pressure parameters. Previous studies have shown a blunted fall in nocturnal blood pressure to be associated with left ventricular hypertrophy, 27 , 28 coronary heart disease, and cerebrovascular manifestations. 20 , 29 In the present study, however, neither the levels of nocturnal fall in systolic and diastolic blood pressure nor nondipper status was able to provide independent information for the prediction of morbid events or target organ damage. Measures of blood pressure variability and heart rate variability also failed to provide additional prognostic information.
Notably, 24‐hour ambulatory diastolic blood pressure demonstrated a curvilinear relationship with morbid events, indicating no reduction in risk below a threshold level of diastolic blood pressure. Much controversy surrounds the notion that loweres diastolic blood pressure too far in certain patients with hypertension may provoke a coronary event. Proponents of this J‐curve phenomenon have emphasized the consistency of this finding across a variety of populations with hypertension 30 , 31 and formed the hypothesis that an inappropriately lowered diastolic blood pressure may lead to myocardial ischemia in predisposed subjects because of a failure of autoregulation in the coronary circulation. 30 Others argue that the effect occurs as a result of an irregularity of small sets of data compounded by biased methods of analysis 2 and suggest that the association between low blood pressure and mortality merely reflects a deterioration in general health rather than a treatment‐induced causal relationship. 32 Our findings of a nonlinear relationship between baseline pretreatment 24‐hour ambulatory intra‐arterial diastolic blood pressure and subsequent events adds to the body of evidence in favor of a curved relationship, which has been observed in untreated populations. 32 However, recent hypertension treatment trials, such as the Systolic Hypertension in the Elderly Program 33 and Hypertension Optimal Treatment trial, 34 have failed to support the J‐curve hypothesis, showing no increase in coronary events despite marked reductions in diastolic blood pressure.
In the subgroup of uncomplicated patients, ambulatory but not clinic blood pressure parameters were independently related to LVMI and IMTmax. The most predictive models contained either 24‐hour mean systolic or pulse pressure. The prominent role of systolic pressure in the development of both morbid events and target organ damage reaffirms its importance in the pathogenesis of cardiovascular complications and counters the traditionally held assumption that diastolic blood pressure is the main determinant of cardiovascular disease. It is thought that the path from hypertension to vascular disease likely involves three interrelated processes: pulsatile flow, endothelial cell dysfunction, and smooth muscle cell hypertrophy. 35 Higher systolic pressures are probably more responsible for these changes than are diastolic levels, and this may provide an explanation for the closer approximation of cardiovascular risk to systolic pressure. The vast majority of previous cross‐sectional studies have shown systolic blood pressure to be the predominant hemodynamic correlate of left ventricular mass, 8 but in most instances the effect of pulse pressure has not been addressed. More recent studies using clinic and ambulatory blood pressure measurements have highlighted the importance of pulse pressure as a major determinant of cardiovascular structure and function. Although it is not clear whether elevated pulse pressure is a causative factor or merely a manifestation of atherosclerotic disease, other studies have also shown a wide pulse pressure to be associated with left ventricular hypertrophy, 36 carotid artery stenosis, 37 and an increased incidence of cardiovascular events, particularly myocardial infarction. 38 , 39
Smoking was independently related to carotid atherosclerosis severity, but was not a predictor of left ventricular mass or morbid events. The lack of association with morbid events is somewhat surprising and may be attributed to methodologic shortcomings. Although binary information on smoking was available on all study patients at baseline, the number of cigarettes smoked and the time period of active tobacco exposure were not ascertained. However, in the subgroup of uncomplicated hypertensive patients who underwent echocardiography and carotid ultrasonography, detailed information regarding smoking history, expressed as pack‐years of smoking, was obtained at the time of these investigations. This may partly explain the discordant relationships of smoking with carotid artery structure and subsequent morbid events.
The increased risk of subsequent morbidity and mortality in South Asians compared to whites is consistent with epidemiologic data from the United Kingdom and elsewhere showing that South Asians are particularly prone to coronary heart disease and also have a higher mortality from cerebrovascular disease than white subjects. 40 , 41 As expected, diabetes mellitus was also an independent predictor of morbid events. However, in view of the relatively small sample population, the effects of racial origin and diabetes mellitus on target organ damage were not evaluable in the subgroup of uncomplicated hypertensives.
CONCLUSIONS
The findings of the present study showed that age, gender, and 24‐hour ambulatory systolic or pulse pressure were strong and consistent independent predictors of target organ damage and cardiovascular outcome in essential hypertension. Ambulatory blood pressure was a better predictor of cardiovascular risk than clinic blood pressure measurement, and this finding has been confirmed by other longitudinal studies. However, the routine use of ambulatory blood pressure monitoring is not currently recommended because of a lack of outcome trials based on the treatment of ambulatory blood pressure levels, along with the absence of a universally accepted definition for the normal range of ambulatory blood pressure and cost.
Acknowledgments: This study was supported by an educational grant from the Northwick Park Hospital Cardiac Research Fund. The late Dr. E.B. Raftery provided invaluable guidance and support. We thank Christopher Kinsey, Ann Banfield, and the staff at the NHS Central Register, Southport, U.K., for their assistance with data collection.
References
- 1. Schappert SM. National ambulatory medical survey : 1991. Summary. NCHS Advance Data, no. 230, Vital and Health Statistics of the National Center for Health Statistics. Hyattsville, MD: U.S. Department of Health and Human Services Publication (PHS) 93–1250; March 29, 1993. [Google Scholar]
- 2. McMahon S, Peto R, Cutler J, et al. Blood pressure, stroke and coronary heart disease: Part 1, prolonged differences in blood pressure: Prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. [DOI] [PubMed] [Google Scholar]
- 3. Ayman D, Goldshine AD. Blood pressure determinations by patients with essential hypertension: I. The difference between clinic and home readings before treatment. Am J Med Sci. 1940;200:465–474. [Google Scholar]
- 4. Hinman AT, Engel BT, Bickford AF. Portable blood pressure recorder: Accuracy and preliminary use in the evaluation of intra‐daily variations in pressure. Am Heart J. 1962;63:663–668. [DOI] [PubMed] [Google Scholar]
- 5. Bevan AT, Honour AJ, Stott FH. Direct arterial pressure recording in unrestricted man. Clin Sci. 1969;36:329–344. [PubMed] [Google Scholar]
- 6. Pickering TG. Blood pressure measurement and detection of hypertension. Lancet. 1994;344:31–35. [DOI] [PubMed] [Google Scholar]
- 7. White WB, Lund‐Johansen P, Omvik P. Assessment of four ambulatory blood pressure monitors and measurements by clinicians versus intra‐arterial blood pressure at rest and during exercise. Am J Cardiol. 1989;65:60–66. [DOI] [PubMed] [Google Scholar]
- 8. Clement DL, De Buyzere M, Duprez D. Prognostic value of ambulatory blood pressure monitoring. J Hypertens. 1994;12:857–864. [PubMed] [Google Scholar]
- 9. Casale PN, Devereux RB, Milner M, et al. Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. Ann Intern Med. 1986;105:173–178. [DOI] [PubMed] [Google Scholar]
- 10. Koren MJ, Devereux RB, Casale PN, et al. Relation of left ventricular mass and geometry to morbidity and mortality in men and women with uncomplicated essential hypertension. Ann Intern Med. 1991;114:345–352. [DOI] [PubMed] [Google Scholar]
- 11. Salonen JT, Salonen R. Ultrasound B‐mode imaging in observational studies of atherosclerotic progession. Circulation. 1993;87(suppl 3):56–65. [PubMed] [Google Scholar]
- 12. Bots ML, Hoes AW, Koudstall PJ, et al. Common carotid intima‐media thickness and risk of stroke and myocardial infarction: The Rotterdam Study. Circulation. 1997;96:1432–1437. [DOI] [PubMed] [Google Scholar]
- 13. O'Leary DH, Polak JF, Kronmal RA, et al., for the Cardiovascular Health Study Collaborative Research Group . Carotid artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14–22. [DOI] [PubMed] [Google Scholar]
- 14. Acharya DU, Heber ME, Dore CJ, et al. Ambulatory intra‐arterial blood pressure in essential hypertension: Effects of age, sex, race and body mass—The Northwick Park Hospital Database Study. Am J Hypertens. 1996;9:943–952. [DOI] [PubMed] [Google Scholar]
- 15. Millar‐Craig MW, Bishop CN, Raftery EB, et al. Circadian variation of blood pressure. Lancet. 1978;1:795–797. [DOI] [PubMed] [Google Scholar]
- 16. Cashman PM, Stott FD, Millar‐Craig MW. Hybrid system for fast data reduction of long‐term blood pressure recordings. Med Biol Eng Comput. 1979;17:629–635. [DOI] [PubMed] [Google Scholar]
- 17. Verdecchia P, Schillaci G, Guerrieri M, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81:528–536. [DOI] [PubMed] [Google Scholar]
- 18. Devereux RB, Alderman MH. Role of preclinical cardiovascular disease in the evolution from risk factor exposure to development of morbid events. Circulation. 1993;88(part 1): 1444–1455. [DOI] [PubMed] [Google Scholar]
- 19. Perloff D, Sokolow M, Cowan R. The prognostic value of ambulatory blood pressures. JAMA. 1983;249:2792–2798. [PubMed] [Google Scholar]
- 20. Verdecchia P, Porcellati C, Schillaci C, et al. Ambulatory blood pressure: An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801. [DOI] [PubMed] [Google Scholar]
- 21. Khattar RS, Senior R, Lahiri A. Cardiovascular outcome in white‐coat versus sustained mild hypertension: A 10‐year follow‐up study. Circulation. 1998;98:1892–1897. [DOI] [PubMed] [Google Scholar]
- 22. Redon J, Campos C, Narciso ML, et al. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: A prospective study. Hypertension. 1998;31:712–718. [DOI] [PubMed] [Google Scholar]
- 23. Staessen JA, Thijs L, Fagard R, et al., for the Systolic Hypertension in Europe Trial Investigators . Predicting cardiovascular risk using conventional versus ambulatory blood pressure in older patients with systolic hypertension. JAMA. 1999;282:539–546. [DOI] [PubMed] [Google Scholar]
- 24. Ohkubo T, Imai Y, Tsuji I, et al. Prediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: A pilot study in Ohasama. J. Hypertens. 1997;15:357–364. [DOI] [PubMed] [Google Scholar]
- 25. Kannel WB, Gordon T, Schwartz MJ. Systolic versus diastolic blood pressure and the risk of coronary heart disease. Am J Cardiol. 1971;27:335–364. [DOI] [PubMed] [Google Scholar]
- 26. Silagy CA, McNeil JJ. Epidemiological aspects of isolated systolic hypertension and implications for future research. Am J Cardiol. 1992;69:213–218. [DOI] [PubMed] [Google Scholar]
- 27. Verdecchia P, Schillaci G, Guerrieri M, et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation. 1990;81:528–536. [DOI] [PubMed] [Google Scholar]
- 28. Palatini P, Penzo M, Racioppa A, et al. Clinical relevance of nighttime blood pressure and of daytime blood pressure variability. Arch Intern Med. 1992;152:1855–1860. [PubMed] [Google Scholar]
- 29. Shimada K, Kawamoto A, Matsubayashi K, et al. Diurnal blood pressure variations and silent cerebrovascular damage in elderly patients with hypertension. J Hypertens. 1992;10:875–878. [PubMed] [Google Scholar]
- 30. Cruickshank JM. Coronary flow reserve and the J curve relation between diastolic blood pressure and myocardial infarction. BMJ. 1988;297:1227–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Farnett L, Mulrow C, Linn WD, et al. The J‐curve phenomenon and the treatment of hypertension: Is there a point beyond which pressure reduction is dangerous? JAMA. 1991;265:489–495. [PubMed] [Google Scholar]
- 32. Fletcher AE, Bulpitt CJ. How far should blood pressure be lowered? N Engl J Med. 1992;326:251–254. [DOI] [PubMed] [Google Scholar]
- 33. Hansson L, Zanchetti A, Carruthers SG, et al., for the HOT Study Group . Effects of intensive blood pressure lowering and low‐dose aspirin in patients with hypertension: Principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351:1755–1762. [DOI] [PubMed] [Google Scholar]
- 34. Systolic Hypertension in the Elderly Program Co‐operative Research Group . Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: Final results of the Systolic Hypertension in the Elderly Program. JAMA. 1991;255:3255–3264. [PubMed] [Google Scholar]
- 35. Kaplan NM. Systemic hypertension: Mechanisms and diagnosis. In: Braunwald E, ed. Heart Disease: A Textbook of Cardiovascular Medicine. Philadelphia, PA: WB Saunders; 1997:807–839. [Google Scholar]
- 36. Pannier B, Brunel P, Aroussy W, et al. Pulse pressure and echocardiographic findings in essential hypertension. J Hypertens. 1989;7:127–129. [PubMed] [Google Scholar]
- 37. Sutton‐Tyrell K, Alcorn HG, Wolfson SK Jr, et al. Predictors of carotid stenosis in older adults with and without isolated systolic hypertension. Stroke. 1993;24:355–361. [DOI] [PubMed] [Google Scholar]
- 38. Benetos A, Rudnichi A, Safar M, et al. Pulse pressure and cardiovascular mortality in normotensive and hypertensive subjects. Hypertension. 1998;32:560–564. [DOI] [PubMed] [Google Scholar]
- 39. Franklin SS, Khan SA, Wong ND, et al. Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham Heart Study. Circulation. 1999;100:354–360. [DOI] [PubMed] [Google Scholar]
- 40. Balarajan R. Ethnic differences in mortality from ischaemic heart disease and cerebrovascular disease in England and Wales. BMJ. 1991;302:560–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. McKeigue PM, Miller GJ, Marmot MG. Coronary heart disease in South Asians overseas: A review. J Clin Epidemiol. 1989;42:597–609. [DOI] [PubMed] [Google Scholar]


