Abstract
Objective:
This study examined associations of patient, hospital, and service system factors with provision of discharge planning to individuals treated in hospital psychiatric units.
Method:
A retrospective cohort analysis used 2012–2013 New York State Medicaid claims data for 18,185 patients under age 65 who were treated in hospital psychiatric units and discharged to the community. The claims data were linked to data from managed behavioral healthcare organizations regarding whether inpatient staff scheduled a follow-up outpatient appointment with a mental health provider. Additional data regarding hospital and service system characteristics were obtained from the American Hospital Association Annual Survey, the Area Health Resource File, and other state administrative databases. Rates and adjusted odds ratios (AORs) were assessed for the likelihood of inpatient staff scheduling a follow-up appointment.
Results:
Inpatient staff scheduled outpatient appointments for 79.8% of discharges. The adjusted odds of not having an outpatient appointment scheduled as part of the patient’s discharge plan were significantly related to several factors including being homeless on admission, having a co-occurring substance use diagnosis, high medical co-morbidity, and not being engaged in psychiatric outpatient services prior to admission.
Conclusions:
Patient characteristics are more strongly associated with failure to receive discharge planning than are hospital and service system characteristics.
Introduction
Discharge planning practices that promote transition from inpatient psychiatric units to community-based care include communication with outpatient clinicians, scheduling timely appointments for outpatient follow-up care, and forwarding discharge summaries to outpatient clinicians (1–4). Communication with outpatient clinicians and timely scheduling of outpatient follow-up appointments improve rates of attending outpatient psychiatric services (5–9) and continuing care plans convey information that supports continuity of care and lowers the likelihood of relapse and readmission (10–16). These practices are widely accepted as standards of care for inpatient treatment (17–20).
Limited data exist, however, regarding the likelihood of patients receiving such discharge planning practices, and available evidence from varied hospital settings suggests low rates of providers completing these practices. Inpatient medical/surgical clinicians communicate directly with outpatient clinicians for only 37% of discharges (21) and one-third of adults reported being discharged from a hospital without follow-up arrangements made (22). Outpatient appointments are scheduled for 41%–67% of patients discharged from inpatient psychiatric units (7,23), and one study indicated that inpatient psychiatric clinicians communicate with outpatient providers for only 66% of discharges (5). A 2007 review indicated that outpatient primary care clinicians reported receiving a continuing care plan within one week of discharge for only 15% of discharged patients (24), although a recent review found that discharge summaries were available to primary care providers within 48 hours for 55% of discharged patients (25). Most of these studies have significant methodological flaws that limit their generalizability including sample size and selection biases and failure to test for reliability of reporting. To better inform targeting of quality improvement efforts, research is needed to understand the prevalence of psychiatric inpatient discharge planning practices and identify factors associated with low rates of discharge planning in larger and more broadly representative populations.
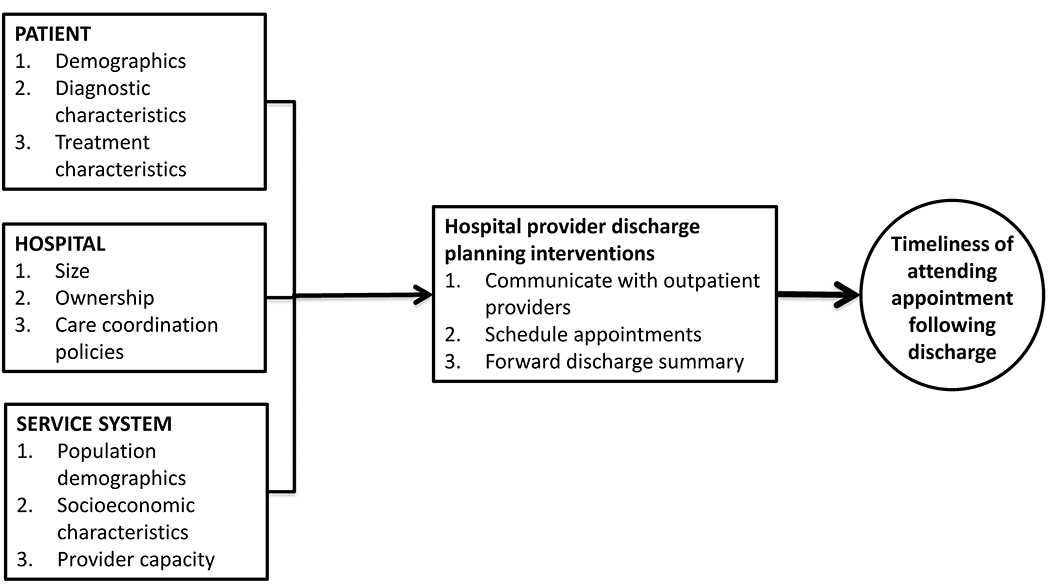
This report examines a key discharge planning practice: inpatient psychiatric providers scheduling outpatient appointments with mental health providers following discharge. We examined a large cohort of inpatient psychiatric admissions and report the proportion of patients who received this practice as well as patient, hospital, and service system characteristics associated with receiving the practice. Based on a conceptual model (Figure 1) we hypothesized that patients who had short inpatient stays or who had diagnoses of less severe psychiatric disorders would be less likely to have an outpatient appointment scheduled as clinicians would assume those patients were more likely to follow through with prior outpatient clinicians. We further anticipated that smaller or non-teaching hospitals would have fewer staff available to schedule outpatient appointments such that their patients would be less likely to receive this discharge planning activity, and that patients who resided in areas with greater economic or mental health resource constraints would also be less likely to have an outpatient appointment scheduled as part of their discharge plan.
Figure 1.
Conceptual model for factors impacting attendance at initial outpatient service following psychiatric hospitalization
Methods
Data Sources
Data were obtained from four primary sources: 1) 2012–2013 New York State (NYS) Medicaid claims records; 2) the 2012–2013 American Hospital Association Annual Survey (26); 3) the 2012–2013 Health Resources and Human Services Administration Area Resource File (27); and 4) a 2012–2013 NYS Managed Behavioral Healthcare Organization (MBHO) Discharge File created during a quality assurance program in which NYS contracted with five MBHOs in geographically distinct regions to review discharge planning practices for fee-for-service inpatient psychiatric admissions. NYS hospital providers were required to notify the regional MBHO of every Medicaid psychiatric inpatient admission and provide specific information regarding the patient’s treatment and discharge plan to the MBHO. The MBHOs, which were not applying medical necessity criteria and not paying providers for the hospital care during this period, were required to offer hospital providers the option to submit the information by telephone, fax, or secure web-based portal.
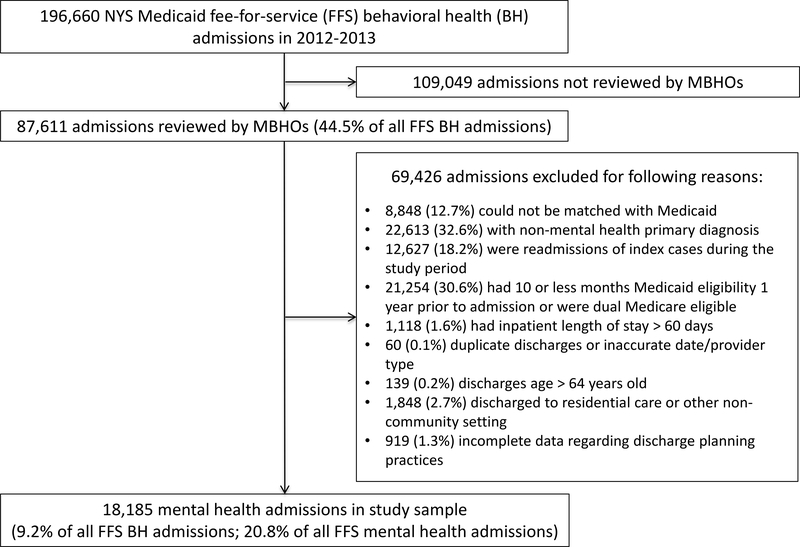
Patient eligibility criteria included: 1) age <65 years; 2) admitted to an inpatient psychiatric unit during 2012–2013 with a principal diagnosis of a mental disorder; 3) discharged to the community; 4) Medicaid eligibility for at least 11 of the 12 months prior to admission; 5) no Medicare eligibility; and 6) inpatient length of stay of ≤60 days. For patients with more than one inpatient psychiatric admission during 2012–2013, only the initial admission was included. Figure 2 is a consort diagram describing the creation of the study sample. After matching the MBHO Discharge File with NYS Medicaid claims records and applying all eligibility criteria, the final sample included 18,185 inpatient psychiatric discharges. The local institutional review board approved the study and granted a waiver of individual consent.
Figure 2.
Consort diagram depicting creation of study sample.
Dependent Variables
Outcome variables were created from the MBHO data file. The MBHOs were required to report whether, for each discharge, the inpatient psychiatric team: 1) scheduled a mental health outpatient appointment; 2) communicated with a current or prior outpatient clinician; and 3) forwarded a discharge summary to an outpatient clinician. We also created a composite dichotomous variable defined by provision of all three discharge planning practices. To assess the reliability of the reported data and operationalize definitions of the discharge planning practices, we completed a reliability study in which MBHO reports were compared to data extracted from inpatient medical records (n=214) from two hospitals (28). Only one of the three discharge planning practice variables met a level of moderate reliability (kappa ≥.4) for inclusion in regression models reported below: scheduling an outpatient appointment with a specified date following discharge. Descriptive data related to the other discharge planning practices (communication with an outpatient clinician and forwarding a discharge summary), along with descriptive data and regression models for the composite variable describing whether the patient received all three discharge planning practices (which did meet our reliability threshold) are reported in an on-line supplement.
Independent Variables
Independent variables included patient, hospital, and regional service system characteristics that prior research suggested could impact discharge planning and post-discharge continuity of care for patients with psychiatric disorders (29,30). Patient level variables from Medicaid claims included demographics, primary inpatient discharge diagnosis, and co-occurring substance use diagnosis at discharge. Prior engagement in psychiatric outpatient services was assessed based upon claims data indicating receipt of outpatient services listing a primary mental disorder diagnosis or mental health service code with each patient categorized as Active (at least one service in 30 days prior to admission), Recent (received at least one service in the 12 months prior to admission but no services in the 30 days prior to admission), or None (no services in the 12 months prior to admission). Additional patient characteristics included homeless at admission and burden of co-occurring medical conditions using an Elixhauser Comorbidity Index (ECI). We used established algorithms to create an ECI index score for each discharge based on clinical diagnoses reported in inpatient and outpatient claims for all Medicaid services during the 12 months prior to admission (31,32).
Hospitals were characterized based upon size, provision of outpatient psychiatric services, hospital ownership, percentage of total annual discharges enrolled in Medicaid, and medical resident teaching status. Information from NYS administrative databases including the NYS Medicaid Program, the New York State Department of Health Statewide Planning and Research Cooperative System-SPARCS, and the NYS Office of Mental Health’s Mental Health Automated Record System were used to create additional variables characterizing the hospitals. These “case mix” variables included the percentage of psychiatric discharges with a substance use disorder diagnosis and percentage of psychiatric patients with two or more psychiatric hospitalizations during the period. Area Health Resource File data characterized counties in which patients resided with respect to regional mental health resources, poverty, and urban/rural classification. An MBHO variable was added to distinguish among the five different MBHOs.
Analytic Plan
The proportion of inpatients not having an appointment scheduled was determined overall and stratified by each patient, hospital and service system characteristic. Unadjusted odds ratios with 99% confidence intervals (CIs) were calculated for each characteristic and adjusted odds ratios calculated using logistic regression analyses describe the effect of each variable on the probability of not having an outpatient appointment scheduled, controlling for all other covariates. Average marginal effects (AMEs) are also provided as a measure of effect on the probability scale. Because of the nesting of patients within different hospitals, the observations are non-independent. Accordingly, generalized estimating equations were used to account for the clustering of observations within hospitals. We consider AORs with 99% CIs that do not include 1.0 and AMEs with 99% CIs that do not include 0, to be statistically significant, while also noting AORs and AMEs with p-values >.01 and < .05. In this large, exploratory study, no adjustments were made to the many CIs and p-values which should therefore be interpreted with caution.
Results
Hospital psychiatric staff scheduled a follow-up outpatient appointment with a mental health provider for 14,503 out of 18,185 discharges (79.8%) with complete information. Data regarding the other two discharge planning practices as well as the composite variable of receiving all three discharge planning practices are available in an on-line supplement.
Table 1 reports percentages of patients not having an outpatient mental health appointment scheduled stratified by patient, hospital, and service system characteristics. In the adjusted logistic regression model, patient characteristics associated with not having an appointment scheduled included being older (relative to the 4–12 years old group) and having short (≤4 days) or long (31–60 days) inpatient lengths of stay (Table 1). Non-Hispanic Black and Puerto Rican-Hispanic ethnic groups had a higher probability of not having an appointment scheduled in unadjusted models, although these associations were largely eliminated in the adjusted models. Other variables associated with not having an outpatient appointment scheduled included being homeless on admission, having a co-occurring substance use diagnosis, high medical comorbidity (Elixhauser score ≥4), and not being engaged in psychiatric outpatient services prior to admission. Patients with bipolar disorder tended to have a higher probability of not having an outpatient appointment scheduled (p=.02).
Table 1.
Patient, hospital, and system characteristics associated with likelihood of not having an outpatient appointment scheduled as part of discharge planning.
| Total sample (N=18,185) | Did not receive (N=3,682) | Unadjusted models of no appointment scheduled | Adjusted models of no appointment scheduled (n=17,831) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient Characteristics | N | N | % | Odds Ratio | 99% CI | Average Marginal Effect, % | 99% CI | Odds Ratio | 99% CI | p-value | Average Marginal Effect, % | 99% CI | p-value |
| Age | |||||||||||||
| 4–12 | 1,798 | 192 | 10.7 | ref | ref | ref | ref | ||||||
| 13–17 | 2,537 | 499 | 19.7 | 2.05 | 1.33, 3.16 | 8.99 | 2.25, 15.73 | 2.08 | 1.37, 3.16 | <.001 | 8.67 | 3.5, 13.85 | <.001 |
| 18–35 | 5,488 | 1,075 | 19.6 | 2.04 | 1.21, 3.44 | 8.91 | 3.18, 14.64 | 1.80 | 1.23, 2.63 | <.001 | 6.55 | 2.74, 10.36 | <.001 |
| 36–64 | 8,362 | 1,916 | 22.9 | 2.49 | 1.47, 4.20 | 12.23 | 6.22, 18.25 | 1.99 | 1.37, 2.88 | <.001 | 7.99 | 4.25, 11.73 | <.001 |
| Gender | |||||||||||||
| Female | 8,395 | 1,562 | 18.6 | ref | ref | ref | ref | ||||||
| Male | 9,790 | 2,120 | 21.7 | 1.21 | 1.06, 1.38 | 3.05 | .94, 5.16 | 1.10 | .97, 1.26 | .05 | 1.36 | −0.42, 3.15 | .05 |
| Race/ethnicity | |||||||||||||
| Non-Hispanic White | 7449 | 1239 | 16.3 | ref | ref | ref | ref | ||||||
| Non-Hispanic Black | 6056 | 1435 | 23.7 | 1.56 | 1.24, 1.96 | 7.06 | 3.40, 10.73 | .98 | .84, 1.14 | .77 | −.25 | −2.37, 1.88 | .77 |
| Puerto Rican - Hispanic | 1987 | 417 | 20.9 | 1.33 | 1.08, 1.65 | 4.35 | 1.20, 7.51 | .84 | .72, .97 | .00 | −2.35 | −4.35, −.34 | .00 |
| Other | 1409 | 361 | 25.6 | 1.73 | 1.32, 2.25 | 8.99 | 4.38, 13.60 | 1.02 | .85, 1.23 | .73 | .34 | −2.25, 2.93 | .74 |
| Unknown | 1284 | 230 | 17.9 | 1.09 | .71, 1.69 | 1.28 | −5.09, 7.65 | 1.04 | .76, 1.43 | .73 | .61 | −3.94, 5.16 | .73 |
| Length of stay | |||||||||||||
| 5–14 days | 9,309 | 1,784 | 19.2 | ref | ref | ref | ref | ||||||
| 0–4 days | 2,690 | 576 | 21.4 | 1.15 | .88, 1.50 | 2.25 | −2.22, 6.72 | 1.60 | 1.33, 1.92 | <.001 | 6.96 | 3.67, 10.24 | <.001 |
| 15–30 days | 4,740 | 975 | 20.6 | 1.09 | .89, 1.34 | 1.41 | −1.84, 4.65 | 1.07 | .94, 1.21 | .18 | .86 | −.82, 2.53 | .19 |
| 31–60 days | 1,446 | 347 | 24.0 | 1.33 | 1.03, 1.72 | 4.83 | .39, 9.27 | 1.45 | 1.17, 1.8 | <.001 | 5.36 | 1.88, 8.85 | <.0001 |
| Homeless at admission | |||||||||||||
| No | 16,046 | 2,914 | 18.2 | ref | ref | ref | ref | ||||||
| Yes | 1,283 | 399 | 31.1 | 2.03 | 1.52, 2.72 | 12.94 | 7.01, 18.87 | 1.32 | 1.06, 1.65 | .01 | 4.06 | .67, 7.44 | .01 |
| Primary diagnosis at discharge | |||||||||||||
| Schizophrenia | 4,998 | 1,068 | 21.4 | ref | ref | ref | ref | ||||||
| Schizoaffective | 1,844 | 379 | 20.6 | .95 | .75, 1.22 | −.82 | −4.86, 3.23 | 1.01 | .82, 1.25 | .88 | .16 | −2.60, 2.93 | .88 |
| Bipolar disorders | 5,968 | 1,274 | 21.4 | 1.00 | .77, 1.30 | −.02 | −4.41,4.37 | 1.19 | .99, 1.42 | .02 | 2.36 | −.17, 4.91 | .02 |
| Depressive disorders | 3,424 | 641 | 18.7 | .85 | .64, 1.12 | −2.65 | −7.03, 1.74 | 1.02 | .82, 1.26 | .84 | .22 | −2.62, 3.07 | .84 |
| Other disorders | 1,951 | 320 | 16.4 | .72 | .51, 1.05 | −4.97 | −10.45, .52 | 1.19 | .90, 1.53 | .08 | 2.37 | −1.20, 6.03 | .09 |
| Co-occurring substance use diagnosis at discharge | |||||||||||||
| No | 11,479 | 1,822 | 15.9 | ref | ref | ref | ref | ||||||
| Yes | 6,706 | 1,860 | 27.7 | 2.03 | 1.63, 2.54 | 11.86 | 7.67, 16.06 | 1.76 | 1.52, 2.05 | <.001 | 8.19 | 5.79, 10.6 | <.001 |
| Medical comorbidity in previous 12 months (non-behavioral health) | |||||||||||||
| 0 | 5,972 | 1,094 | 18.3 | ref | ref | ref | ref | ||||||
| 1–3 | 8,645 | 1,722 | 19.9 | 1.11 | .93, 1.32 | 1.60 | −1.04, 4.24 | 1.05 | .93, 1.18 | .33 | .63 | −1.02, 2.27 | .33 |
| 4 or higher | 3,383 | 832 | 24.6 | 1.45 | 1.17, 1.81 | 6.27 | 2.56, 9.99 | 1.26 | 1.09, 1.45 | <.001 | 3.28 | 1.13, 5.44 | <.001 |
| Prior engagement in psychiatric outpatient services | |||||||||||||
| Active (past month) | 9,108 | 1,430 | 15.7 | ref | ref | ref | ref | ||||||
| Recent (past 12 months but not past month) | 3,800 | 823 | 21.7 | 1.48 | 1.18, 1.87 | 5.96 | 2.39, 9.53 | 1.35 | 1.06, 1.71 | .001 | 3.86 | .72, .71 | .01 |
| None in past 12 months | 5,277 | 1,429 | 27.1 | 1.99 | 1.56, 2.54 | 11.38 | 7.08, 15.68 | 1.90 | 1.54, 2.35 | <.001 | 9.35 | 6.27, 12.44 | <.001 |
| Hospital Charcteristics | |||||||||||||
| Number of hospital beds | |||||||||||||
| Small: less than 100 | 768 | 96 | 12.5 | ref | ref | ref | ref | ||||||
| Medium: 100–499 | 9680 | 1756 | 18.1 | 1.55 | .61, 3.94 | 5.64 | −4.96, 16.24 | 1.24 | .59, 2.61 | .46 | 2.71 | −6.01, 11.43 | .42 |
| Large: 500 or more | 7737 | 1830 | 23.7 | 2.17 | .84, 5.61 | 11.15 | −.31, 22.61 | 1.35 | .52, 3.49 | .42 | 3.88 | −7.90, 15.66 | .39 |
| Hospital ownership | |||||||||||||
| Public | 5035 | 1137 | 22.58 | ref | ref | ref | ref | ||||||
| Private not-for-profit | 11334 | 2198 | 19.39 | .82 | .48, 1.43 | −3.19 | −12.51, 6.13 | 1.03 | .57, 1.83 | .91 | .34 | −7.47. 8.15 | .91 |
| Private for-profit | 1816 | 347 | 19.11 | .81 | .39, 1.69 | −3.47 | −15.45, 8.50 | 1.28 | .52, 3.14 | .48 | 3.63 | −10.24, 17.50 | .50 |
| Psychiatric discharges that were Medicaid, % | |||||||||||||
| Low: less than 49% | 3537 | 654 | 18.5 | ref | ref | ref | ref | ||||||
| Medium: 49–71% | 9231 | 1507 | 16.3 | .86 | .49, 1.51 | −2.16 | −10.37, 6.04 | 1.11 | .78, 1.57 | .46 | 1.3 | −3.11, 5.70 | .45 |
| High: over 71% | 5417 | 1521 | 28.1 | 1.72 | .97, 3.06 | 9.59 | −.42, 19.60 | 1.38 | .79, 2.42 | .14 | 4.51 | −3.33, 12.36 | .14 |
| Hospital provides outpatient psychiatric services | |||||||||||||
| No | 2459 | 331 | 13.5 | ref | ref | ref | ref | ||||||
| Yes | 15726 | 3351 | 21.3 | 1.74 | .86, 3.51 | 7.85 | −.79, 16.49 | 1.03 | .66, 1.61 | .85 | .45 | −5.55, 6.44 | .85 |
| Teaching hospital | |||||||||||||
| No | 3394 | 440 | 13.0 | ref | ref | ref | ref | ||||||
| Yes | 14791 | 3242 | 21.9 | 1.88 | .85, 4.16 | 8.95 | −.46, 18.37 | 1.14 | .62, 2.10 | .58 | 1.75 | −6.26, 9.76 | .57 |
| Psychiatric discharges with substance use disorder diagnosis | |||||||||||||
| Low: less than 34% | 4260 | 789 | 18.52 | ref | ref | ref | ref | ||||||
| Medium: 34–60% | 10154 | 2243 | 22.09 | 1.25 | .67, 2.31 | 3.57 | −6.04, 13.17 | .93 | .57, 1.50 | .69 | −1.03 | −7.75, 5.70 | .69 |
| High: over 60% | 3771 | 650 | 17.24 | .92 | .44, 1.92 | −1.28 | −12.20, 9.63 | .99 | .55, 1.78 | .96 | −.13 | −8.46, 8.19 | .96 |
| Psychiatric population with 2 or more psychiatric discharges | |||||||||||||
| Low: less than 24.5% | 4050 | 511 | 12.62 | ref | ref | ref | ref | ||||||
| Medium: 24.5–35% | 8905 | 1778 | 19.97 | 1.73 | .84, 3.57 | 7.35 | −1.44, 16.14 | .94 | .48, 1.82 | .79 | −.92 | −10.37. 8.52 | .80 |
| High: over 35% | 5230 | 1393 | 26.63 | 2.51 | 1.20, 5.27 | 14.02 | 4.14, 23.89 | .93 | .37, 2.35 | .84 | −1.02 | −13.96, 11.92 | .84 |
| System Characteristics | |||||||||||||
| Behavioral Health Organization | |||||||||||||
| Western | 2577 | 224 | 8.7 | ref | ref | ref | ref | ||||||
| Central | 2534 | 171 | 6.6 | .76 | .34, 1.71 | −1.94 | −7.31, 3.42 | 1.30 | .54, 3.12 | .44 | 1.89 | −4.70, 8.48 | .46 |
| Hudson River | 4594 | 1151 | 25.1 | 3.51 | 2.19, 5.64 | 16.36 | 9.59, 23.14 | 5.01 | 2.43, 10.32 | <.001 | 20.24 | 12.27, 28.21 | <.001 |
| NYC | 6736 | 1894 | 28.1 | 4.11 | 2.65, 6.37 | 19.43 | 13.15, 25.7 | 3.80 | 1.86, 7.77 | <.001 | 15.14 | 7.52, 22.77 | <.001 |
| Long Island | 1744 | 242 | 13.9 | 1.69 | 1.07, 2.67 | 5.18 | .63, 9.73 | 1.85 | .89, 3.87 | .03 | 5.19 | −1.38, 11.75 | .04 |
| County population in poverty | |||||||||||||
| Low: less than 15% | 5887 | 1102 | 18.72 | ref | ref | ref | ref | ||||||
| Medium: 15–19% | 6867 | 1305 | 19.00 | 1.02 | .68, 1.52 | .28 | −5.89, 6.46 | .97 | .62, 1.53 | .87 | −0.42 | −7.15, 6.31 | .87 |
| High: 20% or higher | 5262 | 1222 | 23.22 | 1.31 | .90 – 1.92 | 4.50 | −1.71, 10.71 | .69 | .36, 1.31 | .13 | −4.92 | −13.41, 3.56 | .14 |
| Mental health workers per 100k | |||||||||||||
| Low: less than 67 | 1391 | 132 | 9.49 | ref | ref | ref | ref | ||||||
| Medium: 67 to 166 | 10219 | 2078 | 20.33 | 2.43 | 1.45, 4.08 | 10.85 | 5.05, 16.64 | .89 | .54, 1.47 | .54 | −1.74 | −9.26, 5.78 | .55 |
| High: 167 or more | 6406 | 1419 | 22.15 | 2.71 | 1.69, 4.35 | 12.66 | 7.75, 17.58 | .81 | .46, 1.43 | .33 | −3.03 | −11.38, 5.32 | .35 |
| Urban/rural classification | |||||||||||||
| Medium metro | 2129 | 257 | 12.1 | ref | ref | ref | ref | ||||||
| Large central metro | 9797 | 2427 | 24.8 | 2.4 | 1.30, 4.44 | 12.7 | 5.11, 20.29 | 2.05 | .92, 4.56 | .02 | 8.89 | .45, 17.33 | .01 |
| Large fringe metro | 3188 | 646 | 20.3 | 1.85 | .99, 3.46 | 8.19 | .74, 15.65 | 1.74 | .89, 3.41 | .03 | 6.43 | −.60, 13.46 | .02 |
| Small metro | 1052 | 142 | 13.5 | 1.14 | .45, 2.84 | 1.43 | −8.96, 11.82 | 1.36 | .71, 2.62 | .23 | 3.27 | −3.53, 10.07 | .23 |
| Micropolitan | 1438 | 108 | 7.5 | .59 | .30, 1.15 | −4.56 | −11.01, 1.88 | 1.19 | .59, 2.38 | .52 | 1.76 | −5.13, 8.65 | .51 |
| Noncore | 412 | 49 | 11.9 | .98 | .45, 2.14 | −.18 | −8.38, 8.02 | 1.16 | .53, 2.53 | .63 | 1.44 | −6.35, 9.24 | .63 |
None of the hospital characteristics were significant. The MBHO variable was significant with patients treated in hospitals reviewed by the NYC and Hudson River MBHOs having a higher probability of having aftercare appointments scheduled with a similar tendency for the Long Island MBHO (p=.03) when compared to the Western Region MBHO. Patients treated in hospitals located in large metropolitan regions also showed a tendency to not have an outpatient appointment scheduled (p=.03).
Discussion
Over 20% of hospitalized patients did not have an appointment with an outpatient mental health provider scheduled at the time of discharge. This quality of care gap is concerning given the known clinical risks associated with the period immediately following discharge from inpatient psychiatric units including relapse and hospital readmission (7,13,33–37), homelessness (38,39), violent behavior (40,41), criminal justice involvement (42,43), and all-cause mortality including suicide (44–46).
We hypothesized that several patient, hospital, and service system characteristics would be associated with the probability of patients having an outpatient appointment scheduled. Our findings revealed that patient characteristics were much more likely to predict whether appointments were scheduled: seven patient-level variables were significant in the adjusted models, none of the hospital level variables were significant, and only one of the service system variables was significant. Patient characteristics appear to be more critical determinants of whether patients receive adequate discharge planning and should be primary areas of focus for hospital quality improvement activities.
We hypothesized that patients who had shorter inpatient stays and primary diagnoses of less severe psychiatric disorders would be less likely to have an outpatient appointment scheduled. These hypotheses were partially supported: there were no differences in discharge planning practices among patients with different primary diagnoses, but patients with both short (≤ 4 days) and long (31–60 days) lengths of stay had a higher probability of not having an appointment scheduled. Patients with short lengths of stay may be less likely to receive discharge planning because this group includes patients who sign out against medical advice or otherwise do not wish to pursue treatment. Patients with longer lengths of stay, however, are more likely to have persistent symptoms or complex psychosocial circumstances that require extended inpatient care. These characteristics may also make discharge planning more complicated and increase the likelihood that patients may not have timely follow-up appointments scheduled. This finding suggests another important focus are for hospital quality improvement activities to ensure high-need patients receive adequate discharge planning.
Patients who had co-occurring substance use, were homeless, or were not engaged in care prior to the admission had higher probabilities of not having an outpatient appointment scheduled. In prior research, these characteristics are also strong predictors of failed care transitions and poor outcomes in the period immediately following discharge (29,30,47). Individuals with co-occurring substance use are more likely to be discharged without adequate access to community-based treatment for co-occurring disorders, making them vulnerable to relapse, substance use, and further disengagement from care (48). Homeless individuals are similarly at risk due to their lack of stable supports in the community (49), and individuals who previously did not engage in community-based care are more likely to continue to be disengaged without more intensive follow-up (29,30). Inpatient clinicians should aim to ensure these patients receive adequate discharge planning, and many will require more intensive care transition interventions shown to improve continuity of care for high-risk patients (50–57).
Inpatient clinicians were less likely to schedule appointments for patients with high medical comorbidity. Because this study only included patients who were discharged to the community, this finding cannot be explained by transfers to other hospital units or residential treatment facilities. Inpatient clinicians may believe that patients with high medical co-morbidity have established networks of community-based medical providers who will manage post-discharge care without the need for timely aftercare from psychiatric providers. This should still be considered inadequate discharge planning given the importance of integrating care for these vulnerable patients.
We also hypothesized that patients treated in smaller or non-teaching hospitals, or who resided in areas with greater economic or mental health resource constraints would also be less likely to have an outpatient appointment scheduled. Although none of the hospital variables were associated with scheduling an appointment in the adjusted logistic models, hospitals that served higher proportions of patients with Medicaid had lower rates of scheduling outpatient appointments. Counter to what we anticipated, patients treated in teaching hospitals had a higher probability of not receiving complete discharge planning (also see Supplemental Table 1). This is counterintuitive given the important educational role and availability of trainees to support care and treatment planning. However, many teaching hospitals are located in urban areas and treat patients with higher rates of poverty and other factors that may complicate clinicians’ discharge planning practices.
Despite known shortages of mental health providers in rural and underserved communities, the service system variables related to poverty and density of mental health workers were not associated with having an outpatient appointment scheduled. The variable denoting the MBHO reviewing admissions for each defined region of the state was associated with discharge planning practices, with the New York City MBHO reporting lower rates of scheduling appointments. This may reflect greater numbers of patients not receiving discharge planning in New York City hospitals that also provided outpatient psychiatric services. Anecdotal reports indicate that many New York City hospitals operated walk-in clinics for outpatient follow-up appointments; it may be that hospitals with such clinics had lower rates of appointments scheduled because those clinics were seen as obviating the need for discharge planning.
The main limitation of this study involves the reliability of the discharge planning practice variables; we did not model two of the discharge planning practices due to low correlations between MBHO reports and documentation of the specific practices in patients’ medical records from two hospitals in our reliability study (descriptive data regarding these practices are available in on-line supplement). Another limitation involves the naturalistic design of this study that limits inferences regarding causality because of the potential threat posed by unmeasured confounding factors.
We also did not have discharge planning data for the entire population of Medicaid patients admitted to inpatient psychiatric units during the 2012–2013 study period. The sample comprised 20.8% of NYS Medicaid fee-for-service hospital psychiatric admissions with a mental health primary diagnosis and included representation from 105 out of 106 statewide hospitals that admitted Medicaid fee-for-service patients in 2012–2013. The greatest numbers of excluded cases included patients with non-mental health diagnoses, readmissions, cases not reviewed by MBHOs, and cases not meeting the pre-admission Medicaid eligibility criteria. Patients with non-mental health primary diagnoses represented admissions to substance use disorder treatment programs, which were not the population of interest for this study. Readmissions were excluded to avoid bias associated with duplicate patients. Admissions not reviewed by MBHOs, which included admissions for both mental and substance use treatment, were more likely to have been younger, male, and have had shorter lengths of stay, which may represent a group less likely to receive discharge planning. Patients were also excluded due to not meeting our requirement of Medicaid eligibility for 11 of the 12 months prior to the index admission. During the study planning period a preliminary analysis indicated that this Medicaid eligibility threshold allowed for 76% of all Medicaid admissions in 2012–2013 to be considered. We considered lowering the requirement to eight months; this would have yielded 86% of the original cohort but would have included a significant number of cases with no available data for up to one-third of the period of interest prior to admission. For this reason, we kept the selection criterion of eligibility for 11 out of 12 months. It is not clear whether cases excluded because of this criterion may be more or less likely to receive discharge planning.
Conclusions
This study used a unique, large administrative database to examine whether inpatient psychiatric clinicians met an important standard of care for discharge planning and to identify factors that may have been limiting providers’ ability to deliver these practices. The findings identify important opportunities for continuous quality improvement: over 20% of discharged patients failed to receive a discharge planning practice identified as the standard of care. This important quality gap should be addressed by hospitals via continuous quality improvement efforts focusing on identified sub-groups of patients at high risk for failed care transitions.
Supplementary Material
Highlights.
Among a cohort of 18,185 Medicaid recipients under age 65 who were treated in hospital psychiatric units and discharged to the community, only 46.4% received comprehensive discharge planning practices recommended to decrease risk for discontinuing mental health treatment following discharge;
Inpatient staff scheduled outpatient appointments for 79.8% of discharges; and
Patient characteristics including being homeless on admission, having a co-occurring substance use diagnosis, high medical co-morbidity, and not being engaged in psychiatric outpatient services prior to admission are more strongly associated with failure to receive discharge planning than are hospital and service system characteristics.
Disclosures and acknowledgments
The authors have no conflicts of interest to disclose. Editor Emeritus Howard H. Goldman, M.D., Ph.D., served as decision editor on the manuscript.
Research supported by grant from the National Institute of Mental Health (R01MH106558)
References
- 1.Vigod SN, Kurdyak PA, Dennis CL, et al. Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. Br J Psychiatry 2013;202(3):187–94. [DOI] [PubMed] [Google Scholar]
- 2.Hansen LO, Young RS, Hinami K, et al. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med 2011;155(8):520–8. [DOI] [PubMed] [Google Scholar]
- 3.Shepperd S, Lannin NA, Clemson LM, et al. Discharge planning from hospital to home. Cochrane Database Syst Rev 2013;1:CD000313. [DOI] [PubMed] [Google Scholar]
- 4.Cherlin EJ, Curry LA, Thompson JW, et al. Features of high quality discharge planning for patients following acute myocardial infarction. J Gen Intern Med 2013;28(3):436–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyer CA, McAlpine DD, Pottick KJ, et al. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry 2000;157(10):1592–8. [DOI] [PubMed] [Google Scholar]
- 6.Pfeiffer PN, Ganoczy D, Zivin K, et al. Outpatient follow-up after psychiatric hospitalization for depression and later readmission and treatment adequacy. Psychiatr Serv 2012;63(12):1239–42. [DOI] [PubMed] [Google Scholar]
- 7.Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv 2000;51(7):885–9. [DOI] [PubMed] [Google Scholar]
- 8.Steffen S, Kösters M, Becker T, et al. Discharge planning in mental health care: a systematic review of the recent literature. Acta Psychiatr Scand 2009;120(1):1–9. [DOI] [PubMed] [Google Scholar]
- 9.Shaw H, Mackie CA, Sharkie I. Evaluation of effect of pharmacy discharge planning on medication problems experienced by discharged acute admission mental health patients. Int J Pharm Pract 2000;8:144–53. [Google Scholar]
- 10.Zivin K, Pfeiffer PN, McCammon RJ, et al. "No-Shows": Who Fails to Follow Up With Initial Behavioral Health Treatment? Am J Manag Care 2009;15(2):105–12. [PubMed] [Google Scholar]
- 11.Kreyenbuhl J, Nossel IR, Dixon LB. Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: a review of the literature. Schizophr Bull 2009;35(4):696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith TE, Burgos J, Dexter V, et al. Best practices for improving engagement of clients in clinic care. Psychiatr Serv 2010;61(4):343–5. [DOI] [PubMed] [Google Scholar]
- 13.Bodén R, Brandt L, Kieler H, et al. Early non-adherence to medication and other risk factors for rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Res 2011;133(1–3):36–41. [DOI] [PubMed] [Google Scholar]
- 14.Laan W, van der Does Y, Sezgi B, et al. Low treatment adherence with antipsychotics is associated with relapse in psychotic disorders within six months after discharge. Pharmacopsychiatry 2010;43(6):221–4. [DOI] [PubMed] [Google Scholar]
- 15.Morken G, Widen JH, Grawe RW. Non-adherence to antipsychotic medication, relapse and rehospitalisation in recent-onset schizophrenia. BMC Psychiatry 2008;8:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schennach R, Obermeier M, Meyer S, et al. Predictors of relapse in the year after hospital discharge among patients with schizophrenia. Psychiatr Serv 2012;63(1):87–90. [DOI] [PubMed] [Google Scholar]
- 17.Bodenheimer T. Coordinating care--a perilous journey through the health care system. N Engl J Med 2008;358(10):1064–71. [DOI] [PubMed] [Google Scholar]
- 18.To Err is Human: Building a Safer Health System. Washington, D.C.: Institute of Medicine, National Academies Press; 1999. [PubMed] [Google Scholar]
- 19.NCQA. National Committee for Quality Assurance, Healthcare Effectiveness Data and Information Set (HEDIS). http://www.ncqa.org/tabid/59/default.aspx. Accessed July 18, 2012.
- 20.Commission J. Hospital-Based Inpatient Psychiatric Services measures.
- 21.Oduyebo I, Lehmann CU, Pollack CE, et al. Association of self-reported hospital discharge handoffs with 30-day readmissions. JAMA Inter Med 2013;173(8):624–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schoen C, Osborn R, Huynh PT, et al. Taking the pulse of health care systems: experiences of patients with health problems in six countries. Health Aff 2005;Suppl Web Exclusives:W5:509–25. [DOI] [PubMed] [Google Scholar]
- 23.Nakanishi M, Niimura J, Tanoue M, et al. Association between length of hospital stay and implementation of discharge planning in acute psychiatric inpatients in Japan. Int J Ment Health Syst 2015;9:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297(8):831–41. [DOI] [PubMed] [Google Scholar]
- 25.Kattel S, Manning DM, Erwin PJ, et al. Information Transfer at Hospital Discharge: A Systematic Review. J Patient Saf 2016. [DOI] [PubMed]
- 26.AHA Annual Survey Database™ Fiscal Year 2012. Chicago, IL: American Hospital Association; 2013. http://www.ahadataviewer.com/book-cd-products/aha-survey/. Accessed cited July 7, 2019. [Google Scholar]
- 27.Area Health Resources Files [database on the Internet]. US Department of Health and Human Services, Health Resources and Human Services Administration, Bureau of Health Professions 2012–2013. https://data.hrsa.gov/topics/health-workforce/ahrf. Accesed cited July 7, 2019.
- 28.Haselden M, Corbeil T, Tang F, et al. Family Involvement in Psychiatric Hospitalizations: Associations With Discharge Planning and Prompt Follow-Up Care. Psychiatr Serv 2019. doi: appips201900028. [DOI] [PMC free article] [PubMed]
- 29.Olfson M, Marcus SC, Doshi JA. Continuity of care after inpatient discharge of patients with schizophrenia in the Medicaid program: a retrospective longitudinal cohort analysis. J Clin Psychiatry 2010;71(7):831–8. [DOI] [PubMed] [Google Scholar]
- 30.Stein BD, Kogan JN, Sorbero MJ, et al. Predictors of Timely Follow-Up Care Among Medicaid-Enrolled Adults After Psychiatric Hospitalization. Psychiatr Serv 2007;58(12):1563–9. [DOI] [PubMed] [Google Scholar]
- 31.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43(11):1130–9. [DOI] [PubMed] [Google Scholar]
- 32.van Walraven C, Austin PC, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 2009;47(6):626–33. [DOI] [PubMed] [Google Scholar]
- 33.Cuffel BJ, Held M, Goldman W. Predictive models and the effectiveness of strategies for improving outpatient follow-up under managed care. Psychiatr Serv 2002;53(11):1438–43. [DOI] [PubMed] [Google Scholar]
- 34.Carlisle CE, Mamdani M, Schachar R, et al. Aftercare, emergency department visits, and readmission in adolescents. J Am Acad Child Adolesc Psychiatry 2012;51(3):283–93. [DOI] [PubMed] [Google Scholar]
- 35.Mark T, Tomic KS, Kowlessar N, et al. Hospital readmission among medicaid patients with an index hospitalization for mental and/or substance use disorder. J Behav Health Serv Res 2013;40(2):207–21. [DOI] [PubMed] [Google Scholar]
- 36.Lin HC, Lee HC. The association between timely outpatient visits and the likelihood of rehospitalization for schizophrenia patients. Am J Orthopsychiatry 2008;78(4):494–7. [DOI] [PubMed] [Google Scholar]
- 37.Valenstein M, Copeland LA, Blow FC, et al. Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Med Care 2002;40(8):630–9. [DOI] [PubMed] [Google Scholar]
- 38.Olfson M, Mechanic D, Hansell S, et al. Prediction of homelessness within three months of discharge among inpatients with schizophrenia. Psychiatr Serv 1999;50(5):667–73. [DOI] [PubMed] [Google Scholar]
- 39.Herman DB, Susser ES, Jandorf L, et al. Homelessness among individuals with psychotic disorders hospitalized for the first time: findings from the Suffolk County Mental Health Project. Am J Psychiatry 1998;155(1):109–13. [DOI] [PubMed] [Google Scholar]
- 40.Elbogen EB, Van Dorn RA, Swanson JW, et al. Treatment engagement and violence risk in mental disorders. Br J Psychiatry 2006;189:354–60. [DOI] [PubMed] [Google Scholar]
- 41.Monahan J. The MacArthur studies of violence risk. Crim Behav Ment Health 2002;12:S67–S72. [Google Scholar]
- 42.Van Dorn RA, Desmarais SL, Petrila J, et al. Effects of outpatient treatment on risk of arrest of adults with serious mental illness and associated costs. Psychiatr Serv 2013;64(9):856–62. [DOI] [PubMed] [Google Scholar]
- 43.Oliver P, Keen J, Rowse G, et al. The effect of time spent in treatment and dropout status on rates of convictions, cautions and imprisonment over 5 years in a primary care-led methadone maintenance service. Addiction 2010;105(4):732–9. [DOI] [PubMed] [Google Scholar]
- 44.Katz IR, Peltzman T, Jedele JM, et al. Critical periods for increased mortality after discharge from inpatient mental health units: Opportunities for prevention. Psychiatr Serv 2019;70(6):450–6. [DOI] [PubMed] [Google Scholar]
- 45.Valenstein M, Kim HM, Ganoczy D, et al. Higher-risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. J Affect Disord 2009;112(1–3):50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vasiliadis HM, Ngamini-Ngui A, Lesage A. Factors associated with suicide in the month following contact with different types of health services in Quebec. Psychiatr Serv 2015;66(2):121–6. [DOI] [PubMed] [Google Scholar]
- 47.Smith TE, Haselden M, Corbeil T, et al. Relationship between continuity of care and discharge planning after hospital psychiatric admission. Psychiatr Serv 2019. In press. [DOI] [PMC free article] [PubMed]
- 48.Manuel JI, Gandy ME, Rieker D. Trends in hospital discharges and dispositions for episodes of co-occurring severe mental illness and substance use disorders. Adm Policy Ment Health 2015;42(2):168–75. [DOI] [PubMed] [Google Scholar]
- 49.Lamanna D, Stergiopoulos V, Durbin J, et al. Promoting continuity of care for homeless adults with unmet health needs: The role of brief interventions. Health Soc Care Community 2018;26(1):56–64. [DOI] [PubMed] [Google Scholar]
- 50.Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 2006;166(17):1822–8. [DOI] [PubMed] [Google Scholar]
- 51.Naylor MD, Aiken LH, Kurtzman ET, et al. The care span: The importance of transitional care in achieving health reform. Health Aff 2011;30(4):746–54. [DOI] [PubMed] [Google Scholar]
- 52.Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine. J Gen Intern Med 2009;24(8):971–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Voss R, Gardner R, Baier R, et al. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med 2011;171(14):1232–7. [DOI] [PubMed] [Google Scholar]
- 54.Dixon L, Goldberg R, Iannone V, et al. Use of a critical time intervention to promote continuity of care after psychiatric inpatient hospitalization. Psychiatr Serv 2009;60(4):451–8. [DOI] [PubMed] [Google Scholar]
- 55.Orlosky MJ, Caiati D, Hadad J, et al. Improvement of psychiatric ambulatory follow-up care by use of care coordinators. Am J Med Qual 2007;22(2):95–7. [DOI] [PubMed] [Google Scholar]
- 56.Reynolds W, Lauder W, Sharkey S, et al. The effects of a transitional discharge model for psychiatric patients. J Psychiatr Ment Health Nurs 2004;11(1):82–8. [DOI] [PubMed] [Google Scholar]
- 57.Kasprow WJ, Rosenheck RA. Outcomes of critical time intervention case management of homeless veterans after psychiatric hospitalization. Psychiatr Serv 2007;58(7):929–35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.