The case
Mrs. D is a 58-year-old woman who presents to the emergency department because of a 2-hour episode of tightness in her chest, which had spontaneously resolved 1 hour before her arrival at the hospital. She has adult-onset diabetes mellitus and hypercholesterolemia, both of which have been controlled with medications. Her blood pressure is normal (120/75 mm Hg), as are the other findings at physical examination. An electrocardiogram (ECG) shows T-wave flattening in the lateral leads and a 1.5-mm T-wave inversion in leads II, III and aVF. The creatine kinase (CK) level and CK MB fraction are normal, but the cardiac troponin I level is 0.9 μg/L (lower limit of detection 0.3 μg/L). The emergency physician assesses Mrs. D's risk status and decides on treatment.
An acute coronary syndrome (ACS) — unstable angina or myocardial infarction — is an important cause of illness and premature death and a common reason for hospital admission. Recent advances in treatment, such as the glycoprotein IIb/IIIa inhibitors eptifibatide and tirofiban, low-molecular-weight heparin, direct thrombin inhibitors, clopidogrel, and the safer and more widespread application of percutaneous coronary intervention, have raised questions about the optimal use of these new management strategies. Tailoring treatment to match risk not only ensures that the patient who will benefit most receives appropriate therapy, it also avoids potentially hazardous treatment in patients with a good prognosis. Patients with an acute coronary syndrome (ACS) and those with similar clinical presentations have a wide spectrum of clinical outcomes. We examine how the physician can use information available in the first few hours after the onset of symptoms to choose appropriate treatment based on diagnosis and risk assessment.
Unstable angina and myocardial infarction are often clinically indistinguishable and usually present with a prolonged episode of chest pain that starts without provocation. Myocardial infarction is diagnosed by detecting evidence of myocardial injury with the presence of abnormal levels of circulating biochemical markers such as creatine kinase (CK) or one of the troponins. However, with the development of increasingly sensitive biochemical markers of cardiac injury, the distinction between unstable angina and myocardial infarction has become less well defined.
Both unstable angina and myocardial infarction usually result from atherosclerotic plaque disruption and thrombotic occlusion of a coronary artery. The outcome depends on the site and magnitude of plaque rupture, the resulting flow disturbance, the extent and duration of the thrombotic occlusion, and the presence or absence of an adequate collateral coronary circulation. Consequent to the interaction of these factors, plaque rupture results in a range of symptoms (from none to prolonged chest pain) and various outcomes (no detectable event, unstable angina, myocardial infarction or sudden death). The subsequent course and outcome will depend on the severity of the initial coronary event and the baseline condition of the patient (his or her age, previous coronary event, left ventricular function and other comorbidity).
An accurate diagnosis and estimation of the risk of an adverse outcome are prerequisites to selecting the most appropriate treatment. Early triage of patients by history and electrocardiogram (ECG) findings initiates a clinical suspicion of ACS and distinguishes ACS patients from those with non-coronary chest pain or stable angina. Diagnosis and risk assessment of the patient presenting with chest pain and suspicion of ACS begins in the emergency department, continues throughout the period of hospital management and is maintained during long-term follow-up.
We have confined our discussion to the early assessment and triage (in the first few hours after symptom onset) of the patient with chest pain. This is a critical period of assessment, when crucially important management decisions are made that determine the patient's short- and long-term outcome. Later decisions and longer-term assessments will be made according to the patient's response to treatment and the results of further investigations such as the exercise stress test and coronary angiography. The importance of the early assessment and triage is clear. Although most patients who present to the emergency department survive the acute event, the 1-year mortality is between 5% and 14%, with about half of these deaths occurring within the first 4 weeks following the acute event.1 With optimal risk stratification and management, some of these events may be preventable. Most important, long-term management of atherosclerosis risk factors with smoking cessation, lipid management, hypertension control and treatment of diabetes will have a major impact on long-term outcomes for survivors of an acute coronary event.
Diagnostic triage (Fig. 1)
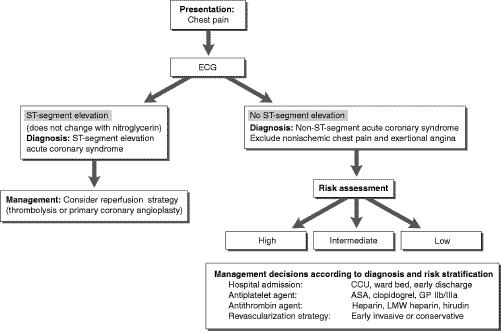
Fig. 1: Diagnostic triage and management of patients presenting to the emergency department with chest pain and a clinical suspicion of an acute coronary syndrome (unstable angina or myocardial infarction). CCU = coronary care unit, GP IIb/IIIa = glycoprotein IIb/IIIa inhibitor, LMW = low-molecular-weight. Photo by: Christine Kenney
The ECG taken at the time of arrival in the emergency department will distinguish between ST-segment elevation ACS and non-ST-segment elevation ACS. Current clinical trials have shown that only patients with ACS and ST-segment elevation benefit from an immediate reperfusion strategy (usually thrombolysis or primary coronary angioplasty if immediately available).2 Thrombolysis should be considered and started within 30 minutes after arrival in every patient with chest pain that began within the 12 hours before presentation and ST-segment elevation or new left bundle-branch block, unless the risk of treatment is considered to be greater than the potential benefits.
However, only 10% of patients with symptoms suggestive of an ACS have ST-segment elevation;3 in addition, many patients have atypical symptoms and a nondiagnostic ECG. Consequently, 25% to 30% of all myocardial infarctions are estimated to be “silent” and unrecognized.4,5,6 Despite our best efforts, about 5% of patients with acute myocardial infarction are unintentionally discharged from emergency departments.7
Risk assessment
The initial diagnosis of an ACS is made on the basis of the patient's history, ECG results and the presence of abnormal levels of biochemical markers. The same information is used to assess the risk of an adverse outcome and tailor management to match the estimated risk. For the majority of patients with an ACS who have no ST-segment elevation, it is important to develop a system to recognize those at higher risk of (re)infarction or death. These patients may benefit from intensive monitoring in a coronary care unit, the use of ASA, antithrombin agents (heparin) and antiplatelet drugs (e.g., glycoprotein IIb/IIIa inhibitor), and a decision to perform early coronary angiography for early revascularization. In contrast, patients who are not at high risk of (re)infarction or death usually remain at low risk, do not require such intensive management and can usually be discharged home following a short period of observation.
The risk assessment should include an evaluation of both the background risk and the severity of the acute coronary event.
Background risk
Age is an important determinant of risk in all cases of ACS, especially for patients over 70 years old. A past history of coronary events or revascularization may indicate a large ischemic burden due to extensive coronary artery disease or impaired left ventricular function, or both: both of these factors determine the patient's outcome should the culprit coronary artery reocclude. People with diabetes mellitus are at an especially high risk of infarction and death, probably because of the extent of their coronary artery disease.
Clinical presentation
The combination of indicators of severity of the acute ischemic event (e.g., prolonged and recurrent pain at rest, and chest pain associated with dyspnea) plus ECG evidence of ST-segment shift correctly identifies 90% of patients with chest pain who will have an adverse outcome in the subsequent 30 days.8 The addition of tests for sensitive biochemical markers of myocardial injury and a period of observation increases the likelihood that almost all high-risk patients can be identified soon after presentation.
Electrocardiogram results
The ECG has been remarkably effective in identifying patients at high risk of (re)infarction or death. ST-segment shift, transient or fixed, is associated with a 30-day mortality of 5% to 7%, as compared with less than 2% when T-wave inversion alone is present9 (Fig. 2). A TRIM substudy showed that T inversion in 5 or more ECG leads had adverse prognostic implications similar to the presence of ST-segment depression.10 At the time of their presentation, patients with unstable angina are indistinguishable from those with non-ST-segment elevation myocardial infarction. Patients with suspected myocardial infarction who present with an ST-segment depression of at least 2 mm have a high 1-year mortality, whether or not an infarction is confirmed.11
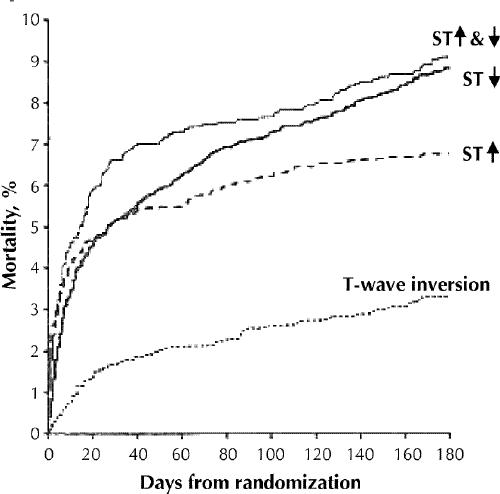
Fig. 2: Six-month mortality among patients with an acute coronary syndrome, by electrocardiogram result at time of presentation. Although patients with ST-segment depression (ST↓) have a better early (5-day) survival than those with ST-segment elevation (ST↑), their long-term outlook is as bad, if not worse. In this study patients at lowest risk were those with T-wave inversion alone. [Adapted, with permission, from Savonitto et al, JAMA 1999;281:707-13.9 Copyrighted 1999, American Medical Assocation.]
Biochemical markers
Patients with biochemical evidence of myocardial injury (presence of serum myoglobin, CK [and MB fraction] and cardiac troponin I and T) have a 5-fold higher risk of early and later reinfarction and death than possible ACS patients without biochemical evidence of myocardial injury.12
Cardiac troponin I and T have recently been introduced as markers of myocardial injury. Neither is detectable in plasma from healthy control subjects, and consequently they are sensitive and specific indicators of myocyte necrosis. About 33% of patients with unstable angina (no ECG findings of acute infarction, and normal CK levels and CK MB fractions) are found to have detectable cardiac troponin levels.12 These patients are 4.3 times more likely than those with a negative troponin level to have a myocardial infarction or die within 30 days after presentation.12 The presence of troponin in patients with an ACS appears to be a marker of complex atherosclerotic lesions and visible thrombus on angiography and is an indicator of increased risk of reocclusion of the coronary artery.13
The risk of death within 30 to 42 days after presentation has been shown to be related to the initial cardiac troponin I or T level (Fig. 3).14,15 Blood should be sampled at the time of presentation; if negative for troponin, the test should be repeated after 6 hours, and again as needed. Analysis of results from the GUSTO-IIa trial16 and the TIMI IIIB trial14 showed that the baseline sample alone is inadequate for both diagnosis and risk stratification.
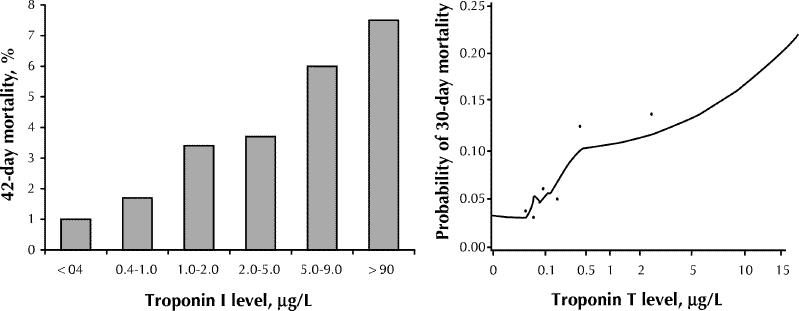
Fig. 3: Mortality in relation to cardiac troponin levels at time of randomization. Left: Troponin I, in TIMI IIIB study [adapted, with permission, from Antman et al,14 N Engl J Med 1996;335:1342-9]. Right: Troponin T, in GUSTO-IIa study [adapted, with permission, from Ohman et al,15 N Engl J Med 1996;335:1333-41].
The presence of cardiac troponin I or T indicates an increased risk of fatal and nonfatal (re)infarction above that implied by ECG findings, whether ST-segment shift, T-wave inversion or a normal tracing is present.14,15 However, the independence and relative predictive value of cardiac troponin and ECG observations remain controversial. A multivariate analysis in the TRIM substudy10 showed that only T-wave inversion in 5 or more leads and ST-segment depression, and not cardiac troponin T, was predictive of outcome at 30 days. In the TIMI IIIB study,14 ST-segment depression predicted outcome with a relative risk of 4.71, whereas the predictive value of troponin T was dependent upon the magnitude of the level of the biochemical marker (relative risk 1.03 per 1-μg/L increase). Ravkilde and associates17 showed that the CK MB fraction and the troponin T level provided independent prognostic information but added no additional information for risk stratification once ECG abnormalities were considered. The study of Hamm and collaborators18 supported the independent prognostic value of both troponin I and T. However, the strict ECG criterion in their study (ST-segment depression greater than 0.15 mV) was more conservative than that used by other investigators (ST-segment depression greater than 0.5–1 mV).9
Many patients with a clinical suspicion of ACS have troponin levels that are marginally elevated. How should we approach risk stratification and management for these patients? Would they benefit from intensive medical treatment and early intervention? A recent analysis of the PRISM study19 showed that a cardiac troponin I level greater than 1.0 μg /L (measured using the Abbott assay) during the first 12 hours after presentation predicted benefit from treatment with tirofiban. In contrast, the presence of a low level of troponin I (between 0.3 and 1.0 μg/L) was not predictive of treatment benefit. A troponin level that is low or borderline at presentation could also be clearly elevated several hours later. It is recommended that patients with a clinical suspicion of ACS who have a low troponin level (the level individualized for the assay and institution) be observed and the measurement repeated.
In summary, the presence of cardiac troponin I or T in a patient with a non-ST-elevation ACS is an indicator of increased risk of an adverse outcome, with the risk related to the peak troponin level in the first 8 to 12 hours after presentation. Cardiac troponin is an indicator of high risk for recurrent thrombotic episodes and suggests the need for aggressive antithrombotic management. However, troponin may not be detectable despite the presence of other high-risk features (e.g., ST-segment depression or recurrent myocardial ischemia associated with ST-segment shift). Until evidence is available to the contrary, these patients should receive the same aggressive antithrombotic treatment as those with elevated troponin levels.
Recurrent myocardial ischemia
Recurrent chest pain, especially when associated with ST-segment depression on an ECG and occurring despite medical treatment, is a powerful indicator of both fatal and nonfatal infarction (Fig. 4).20,21 Silent ischemia detected by continuous ECG monitoring is also predictive of an adverse outcome and increases risk above that indicated by the presence of troponin.22 Current technology present in many cardiac care units and emergency departments permits continuous real-time ST-segment analysis of 12-lead cardiograms and early recognition of these high-risk patients.22
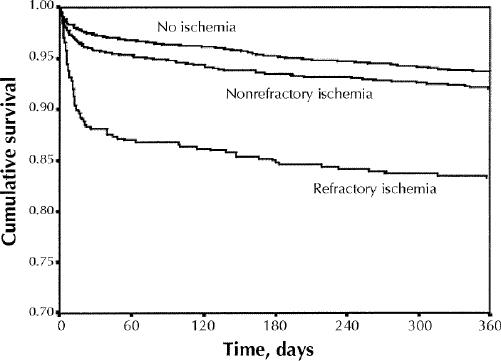
Fig. 4: Cumulative survival during the 360 days following acute coronary syndrome (ACS) with non-ST-segment elevation ACS in patients with refractory myocardial ischemia. [Adapted, with permission, from Armstrong et al,21 Circulation 1998;98:1860-8.]
Risk scores
Recent analyses of clinical trials9,23,24 have examined the independent determinants of outcome in patients presenting with symptoms compatible with an ACS. Antman and associates23 developed the TIMI risk score as a means of predicting death, myocardial infarction and recurrent ischemia prompting revascularization on the basis of the following 7 risk factors, which were found to be significant in a multivariate analysis of factors of patients in the unfractionated heparin arm of the TIMI 11B trial: age of 65 years or more, at least 3 risk factors for coronary artery disease, prior coronary stenosis of 50% or more, ST-segment shift, at least 2 anginal events in the 24 hours before presentation, use of ASA in the 7 days before presentation and elevated levels of cardiac markers. Using 3 patient cohorts to validate the TIMI risk score, the authors assigned a value of 1 for each risk factor present and then categorized patients by the number of risk factors present. They found a modest predictive value for the composite end point, although the predictive value for death was higher.
In the analysis of the PURSUIT study,24 age, severe symptoms and ST-segment shift were also found to be independent predictors of risk. In this group of higher risk patients, hypotension, tachycardia and heart failure were predictive of an adverse outcome.
Although the TIMI and PURSUIT risk score models provide insight into the relative contributions of the independent risk factors, the patients analyzed had entry criteria that, on their own, predict a higher event rate. Patients at low and very low risk were not included in either of these trials. Furthermore, neither study included troponin or recurrent ischemia as risk factors.
Matching treatment to baseline risk
On the basis of clinical information available during the first few hours after presentation, patients can be classified as being at high risk (30-day risk of fatal or nonfatal myocardial infarction greater than 10%), intermediate risk (3%–9%) or low risk (less than 3%), and the risk stratum can then be used to choose an appropriate management strategy. However, risk algorithms directing management have not been tested in prospective clinical trials, and currently they can provide only guidelines for the management of individual patients. The American Heart Association and American College of Cardiology guidelines for the management of unstable angina and non-ST-segment elevation myocardial infarction provide an algorithm that uses both ECG findings and cardiac biomarkers to direct patients into an acute ischemia pathway.25 Although the majority of the ACS patients will be at high risk, those who have no high-risk features yet have provokable ischemia are also included in the acute ischemia pathway. Furthermore, the algorithm appears to recommend the same antithrombotic regimen of ASA, heparin and glycoprotein IIb/IIIa inhibitors for all patients entering the pathway, independent of presentation. Another algorithm is suggested in Fig. 5. Developed at a conference attended by cardiologists and other health care professionals in Toronto, it was designed to apply current knowledge and be applicable in Canada.26
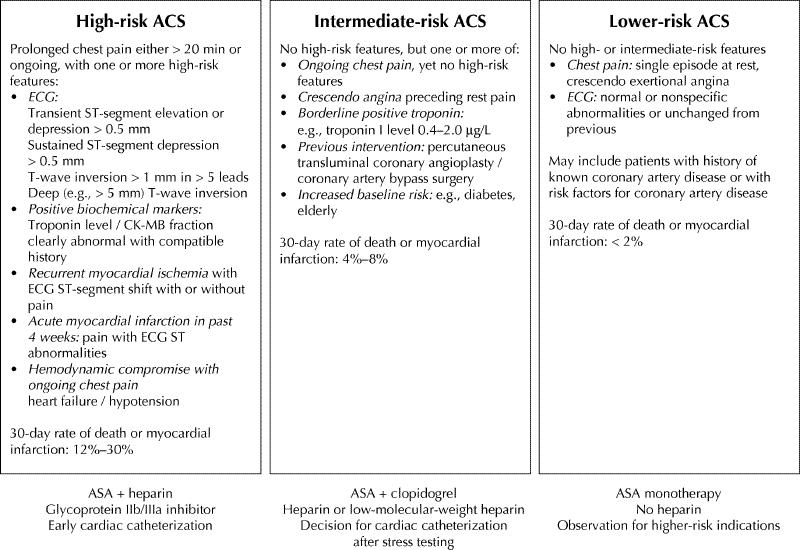
Fig. 5: Risk stratification of patients presenting with a non-ST-segment elevation acute coronary syndrome (ACS). Identification of high-, intermediate- and low-risk categories allows appropriate management choices. [Adapted, with permission, from Fitchett,30 Can J Cardiol 2000;16:1423-32.]
Patients at high risk of fatal or non fatal myocardial infarction include those with prolonged chest pain that is associated with ECG evidence of ST-segment depression and extensive T-wave inversion, significant elevation of biochemical markers of myocardial injury, recurrent myocardial ischemia, or the presence of heart failure or hypotension, or chest pain that occurs following a recent myocardial infarction. Clinical trials of heparin27 and low-molecular-weight heparin,28,29,30,31 of platelet glycoprotein IIb/IIIa inhibitors32,33,34 and of early revascularization35,36 all have shown benefit in the management of patients with these high-risk features. Despite these guidelines, the use of low-molecular-weight heparin and glycoprotein IIb/IIIa inhibitors remains low in such patients. Preliminary observations from the Canadian Heart Research Centre ACS registry shows that, in 48 hospitals across Canada, low-molecular-weight heparin is used in about 30% of patients with high-risk features such as ECG evidence of ST-segment depression, and glycoprotein IIb/IIIa inhibitors are used in only about 5% of the same population. The recently reported CURE trial37 showed the platelet activation inhibitor clopidogrel, when added to ASA for the management of patients with non-ST-segment elevation ACS, reduced rates of death, myocardial infarction and stroke by 20% over the mean 9-month follow-up. Benefit from the clopidogrel treatment was observed within hours after administration of the loading dose of clopidogrel, and the rate of refractory ischemia during hospital stay was reduced by 24%. A similar reduction (20%) in the rate of adverse outcomes was seen during both the early (first 30 days) and late (30 days to 9 months) follow-up. These benefits were achieved with a small (1%) increase in the rate of major bleeding. In future, the majority of patients at intermediate risk with non-ST-segment ACS will probably receive clopidogrel. However, the role of clopidogrel in the current management of high-risk patients with glycoprotein IIb/IIIa inhibitors and an early invasive strategy remains undefined. Until safety data are available, the combined use of clopidogrel with ASA, heparin and an intravenous glycoprotein IIb/IIIa inhibitor should not be used except at the time of percutaneous coronary intervention.
The majority of patients presenting to an emergency department with chest pain, and about one-third of those admitted to hospital, have no high-risk features at the time of presentation and have a relatively low 30-day risk of either death or myocardial infarction. Such patients include those with persistent or recurrent chest pain and no ECG change with pain; crescendo angina preceding an episode of pain at rest; a low cardiac troponin level (e.g., troponin I level less than 2.0 μg/L); a history of recent coronary angioplasty or coronary artery bypass surgery; or a high background risk (e.g., high age, diabetes, poor left ventricular function). These patients need to be observed for the development of high-risk markers (recurrent myocardial ischemia or clear biochemical evidence of myocardial injury). In the absence of high-risk markers, treatment should be continued with heparin, clopidogrel and ASA. In these lower risk patients, glycoprotein IIb/IIIa inhibitors have not been shown to be of value above that of treatment with heparin alone. Either unfractionated heparin or low-molecular-weight heparin can be used; however, based on the results of the ESSENCE30 and TIMI 11B31 studies, which included patients at intermediate risk, low-molecular-weight heparin is likely to be better. A decision to pursue coronary revascularization in these patients can be made after noninvasive evaluation for provocable myocardial ischemia by either exercise electrocardiography, stress perfusion imaging or stress echocardiography.
In the absence of either high or intermediate risk indicators, recent studies have suggested that patients at low risk can be identified after a short period of observation. In these patients the absence of recurrent symptoms or silent myocardial ischemia, abnormal ECG findings, biochemical evidence of myocardial injury and readily provokable ischemia during stress testing permits early discharge of an important number of patients directly from the emergency department. The CHEER study38 examined the validity of early discharge in the management of patients with ACS and no high-risk features: 16% of the patients had previous myocardial infarction, 15% had prior revascularization, and 50% had abnormal, but not high-risk, ECG findings. The patients were randomly assigned either to a 6-hour observation period in an emergency department chest pain monitoring unit (CPU) or to routine hospital admission to either a cardiac care unit or ward. Following an uneventful observation period and an exercise ECG without ischemia at a low level of exertion, 46% of the patients in the CPU group were discharged home; none of these patients had events in the next 30 days. In contrast, myocardial infarction or recurrent myocardial ischemia occurred in 7% of the remaining CPU patients who required admission. The authors concluded that a 6-hour observation period of patients who have no high-risk features but who have a past history of coronary artery disease and have abnormal, yet not high-risk, ECG findings is a safe and cost-effective means of identifying patients who are adequately stable to return home. Measurement of cardiac troponin I or T would probably have provided further security for the early discharge of this low-risk group. For patients presenting with symptoms compatible with an ACS and no high-risk features, a negative troponin I level after 8 hours of observation is associated with a 0.3% incidence of death or myocardial infarction at 30 days, compared with an incidence of 18% among patients with detectable troponin I levels.18
For the patient discharged early with a diagnosis of possible low-risk ACS, an early follow-up evaluation is essential. Although the short-term risk is low, the long-term outcome may be improved with appropriate managment of risk factors.
In summary, many therapeutic strategies are available to reduce the risk of further early acute coronary events. Therefore, it is important to consider the magnitude of the baseline risk, the absolute therapeutic benefit and potential hazards. Treatment choices that require special selection are thrombolysis, anticoagulation with heparin (low-molecular-weight or unfractionated), antiplatelet therapy with glycoprotein IIb/IIIa inhibitors, and coronary angiography and revascularization. A better understanding of indicators of risk and the benefits of the various treatments available will permit optimal matching of therapeutic strategy to baseline risk.
Treatment for Mrs. D
The emergency physician assesses Mrs. D's history, clinical features and risk factors and concludes that she is at intermediate risk of ACS because of her diabetes, nonspecific ECG abnormalities and borderline cardiac troponin I level. Treatment is started with ASA (325 mg) and heparin, and she is admitted for monitoring. After 6 hours the ECG shows a 3-mm T-wave inversion in the lateral leads and a new T-wave inversion in leads II, III and aVF. The CK level and the CK MB fraction remain normal; however, the troponin I level is now 4.9 μg/L. Her status is upgraded to high-risk non-ST-segment ACS. A glycoprotein IIb/IIIa inhibitor is indicated but is not prescribed at this time. Twelve hours after admission Mrs. D has a further transient episode of chest pain. An ECG recorded during the pain shows a 3-mm ST-segment elevation in leads II, III and aVF, which resolves after administration of nitroglycerin sublingually. Her risk status is raised to an even higher level, and intravenous therapy with a glycoprotein IIb/IIIa inhibitor is started. The following day a coronary angiogram reveals a stenosis of 80% associated with an ulcerated plaque in the proximal right coronary artery. The stenosis is successfully dilated and a stent deployed. The glycoprotein IIb/IIIa inhibitor therapy is continued for a further 24 hours after the procedure. Mrs. D has no symptoms 6 months later.
Footnotes
This article has been peer reviewed.
Acknowledgement: Financial support for this article was from the Canadian Heart Research Centre.
Competing interests: The authors have received speaker fees and support for clinical research from Merck Frosst, Key Schering, Aventis, Pharmacia Upjohn and Eli Lilly.
Reprint requests to: Dr. David Fitchett, Rm. 7-037, St. Michael's Hospital, 30 Bond St., Toronto ON M5B 1W8; fitchettd@smh.toronto.on.ca
References
- 1.Rahimtoola SH. Coronary bypass surgery for unstable angina. Circulation 1984; 69:842-8. [DOI] [PubMed]
- 2.Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Lancet 1994;343:311-22. [PubMed]
- 3.Rude RE, Poole WK, Muller JE, Turi Z, Rutherford J, Parker C, et al. Electrocardiographic and clinical criteria for the recognition of acute myocardial infarction based on analysis of 3,697 patients. Am J Cardiol 1983;52:936-42. [DOI] [PubMed]
- 4.Margolis JR, Kannel WS, Feinleib M, Dawber TR, McNamara PM. Clinical features of unrecognized myocardial infarction — silent and symptomatic. Eighteen year follow-up: the Framingham study. Am J Cardiol 1973;32:1-7. [DOI] [PubMed]
- 5.Kannel WB, Abbott RD. Incidence and prognosis of unrecognized myocardial infarction: an update on the Framingham study. N Engl J Med 1984;311:1144-7. [DOI] [PubMed]
- 6.Rosenman RH, Friedman M, Jenkins CD, Straus R, Wurm M, Kositchek R. Clinically unrecognized myocardial infarction in the Western Collaborative Group Study. Am J Cardiol 1967;19:776-82. [DOI] [PubMed]
- 7.McCarthy BD, Beshansky JR, D'Agostino RB, Selker HP. Missed diagnoses of acute myocardial infarction in the emergency department: results from a multi-center study. Ann Emerg Med 1993;22:579-85. [DOI] [PubMed]
- 8.Green G, Bessman E, Dehlinger E, Chan DW, Beaudreau RW, McGreivy TS, et al. A combined approach using multiple myocardial markers predicts adverse events among ED patients [abstract]. Circulation 1996;94:I-134.
- 9.Savonitto S, Ardissino D, Granger CB, Morando G, Prando MD, Mafrici A, et al. Prognostic value of the admission electrocardiogram in acute coronary syndromes. JAMA 1999;281:707-13. [DOI] [PubMed]
- 10.Holmvang L, Luscher MS, Clemmensen P, Thygesen K, Grande P. Very early risk stratification using combined ECG and biochemical assessment in patients with unstable coronary artery disease (A Thrombin Inhibition in Myocardial Ischemia [TRIM] substudy). The TRIM Study Group. Circulation 1998;98:2004-9. [DOI] [PubMed]
- 11.Lee HS, Cross SJ, Rawles JM, Jennings KP. Patients with suspected myocardial infarction who present with ST depression. Lancet 1993;342:1204-7. [DOI] [PubMed]
- 12.Wu AHB, Lane PL. Metaanalysis in clinical chemistry: validation of cardiac troponin T as a marker for ischemic heart diseases. Clin Chem 1995;41:1228-33. [PubMed]
- 13.Heeschen C, van Den Brand MJ, Hamm CW, Simoons ML. Angiographic findings in patients with refractory unstable angina according to troponin T status. Circulation 1999;100:1509-14. [DOI] [PubMed]
- 14.Antman EM, Tanasijevic MJ, Thompson B, Schactman M, McCabe CH, Cannon CP, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996;335:1342-9. [DOI] [PubMed]
- 15.Ohman EM, Armstrong PW, Christenson RH, Granger CB, Katus HA, Hamm CW, et al. Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med 1996;335:1333-41. [DOI] [PubMed]
- 16.Newby LK, Christenson RH, Ohman EM, Armstrong PW, Thompson TD, Lee KL, et al. Value of serial troponin T measures for early and late risk stratification in patients with acute coronary syndromes. The GUSTO-IIa Investigators. Circulation 1998;98:1853-9. [DOI] [PubMed]
- 17.Ravkilde J, Nissen H, Horder M, Thygesen K. Independent prognostic value of serum creatine kinase isoenzyme MB mass, cardiac troponin T and myosin light chain levels in suspected acute myocardial infarction. J Am Coll Cardiol 1995;25: 574-81. [DOI] [PubMed]
- 18.Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T. Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med 1997;337:1648-53. [DOI] [PubMed]
- 19.Heeschen C, Hamm CW, Goldmann B, Deu A, Langenbrink L, White H. Troponin concentrations for stratification of patients with acute coronary syndromes in relation to therapeutic efficacy of tirofiban. Lancet 1999;354:1757-62. [DOI] [PubMed]
- 20.Murphy JJ, Connell PA, Hampton JR. Predictors of risk in patients with unstable angina admitted to a district general hospital. Br Heart J 1992;67:395-401. [DOI] [PMC free article] [PubMed]
- 21.Armstrong PW, Fu Y, Chang WC, Topol EJ, Granger CB, Betriu A, et al. Acute coronary syndromes in the GUSTO-IIb trial: prognostic insights and impact of recurrent ischemia. The GUSTO-IIb Investigators. Circulation 1998;98:1860-8. [DOI] [PubMed]
- 22.Jernberg T, Lindahl B, Wallentin L. ST-segment monitoring with continuous 12-lead ECG improves early risk stratification in patients with chest pain and ECG nondiagnostic of acute myocardial infarction. J Am Coll Cardiol 1999;34: 1413-9. [DOI] [PubMed]
- 23.Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 2000;284:835-42. [DOI] [PubMed]
- 24.Boersma E, Pieper KS, Steyerberg EW, Wilcox RG, Chang WC, Lee KL, et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation 2000;101:2557-67. [DOI] [PubMed]
- 25.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on the Management of Patients with Unstable Angina). J Am Coll Cardiol 2000;36:970-1062. [DOI] [PubMed]
- 26.Fitchett D. Guidelines for the early management of acute coronary syndromes: focus on antithrombotic and antiplatelet therapy. Can J Cardiol 2000;16:1423-32. [PubMed]
- 27.Theroux P, Ouimet H, McCans J, Latour JG, Joly P, Levy G, et al. Aspirin, heparin, or both to treat acute unstable angina. N Engl J Med 1988;319:1105-11. [DOI] [PubMed]
- 28.Gurfinkel EP, Manos EJ, Mejail RI, Cerda MA, Duronto EA, Garcia CN, et al. Low molecular weight heparin versus regular heparin or aspirin in the treatment of unstable angina and silent ischemia. J Am Coll Cardiol 1995;26:313-8. [DOI] [PubMed]
- 29.Low-molecular-weight heparin during instability in coronary artery disease. Fragmin during Instability in Coronary Artery Disease (FRISC) Study Group. Lancet 1996;347:561-8. [PubMed]
- 30.Cohen M, Demers C, Gurfinkel EP, Turpie AG, Fromell GJ, Goodman S, et al. A comparison of low-molecular-weight heparin with unfractionated heparin for unstable coronary artery disease. Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events (ESSENCE) Study Group. N Engl J Med 1997;337:447-52. [DOI] [PubMed]
- 31.Antman EM, McCabe CH, Gurfinkel EP, Turpie AG, Bernink PJ, Salein D, et al. Enoxaparin prevents death and cardiac ischemic events in unstable angina/ non-Q-wave myocardial infarction. Results of the thrombolysis in myocardial infarction (TIMI) 11B trial. Circulation 1999;100:1593-601. [DOI] [PubMed]
- 32.Inhibition of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non-Q-wave myocardial infarction. Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) Study Investigators. N Engl J Med 1998;338:1488-97. [DOI] [PubMed]
- 33.A comparison of aspirin plus tirofiban with aspirin plus heparin for unstable angina. Platelet Receptor Inhibition in Ischemic Syndrome Management (PRISM) Study Investigators. N Engl J Med 1998;338:1498-505. [DOI] [PubMed]
- 34.Inhibition of platelet glycoprotein IIb/IIIa with eptifibatide in patients with acute coronary syndromes. The PURSUIT Trial Investigators. N Engl J Med 1998;339:436-43. [DOI] [PubMed]
- 35.Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Lancet 1999;354:708-15. [PubMed]
- 36.Cannon CP, Weintraub WS, Demopoulos L, Robertson D, DeLucca P, McCabe CH, et al. Results of the Treat angina with Aggrastat and determine the Cost of Therapy with an Invasive or Conservative Strategy (TACTICS-TIMI 18) Trial. A comparison of invasive and conservative strategy in patients with unstable angina and non-ST-segment elevation myocardial infarction [abstract]. Circulation 2000;102:a2672.
- 37.Yusuf S, for the CURE Investigators. Clopidogrel in unstable angina to prevent recurrent events. Presented as a late-breaking clinical trial at the 50th Scientific Session of the American College of Cardiology, Orlando, Fla., Mar 2001.
- 38.Farkouh ME, Smars PA, Reeder GS, Zinsmeister AR, Evans RW, Meloy TD, et al. A clinical trial of a chest-pain observation unit for patients with unstable angina. Chest Pain Evaluation in the Emergency Room (CHEER) Investigators. N Engl J Med 1998;339:1882-8. [DOI] [PubMed]


