Abstract
Enteric duplication cysts (EDCs) are rare congenital malformations of the children and can develop everywhere along the gastrointestinal (GI) tract, being the ileum the most frequent localization. We herein present an unusual case of duplication cyst of ileal origin who show a tubular morphology and doesn't communicate with GI lumen.
A 2-month-old boy was admitted to our hospital for investigation of an anechoic formation of the lower right abdomen for the surgical planning. The patient was asymptomatic. Ultrasound (US) and magnetic resonance imaging (MRI) showed features of a cystic lesion. Laparoscopic surgery was performed and the cyst excised. Macroscopic examination and histologic findings confirmed the diagnosis of a enteric duplication cyst arising from the ileum.
In a patient with an abdominal cystic mass, although asymptomatic, it's worth assessing the nature of the lesion and planning a surgery in order to avoid future complications. A correct use of diagnostic it's fundamental to identify the etiology and the characteristics of a cystic mass.
Keywords: Enteric duplication cyst, Abdominal cystic mass, Magnetic resonance imaging, Pediatric ultrasound
Introduction
Enteric duplication cysts (EDCs) are rare (1:4,500 births, 0.2% of all children, and show a slight male predominance [1], [2], [3], [4]) congenital lesions that can develop anywhere along the alimentary tract, although it is most frequently observed in the terminal part of the ileum. They are characterized by the presence of gastrointestinal mucosal lining (not necessarily correlate with the adjacent Gastrointestinal (GI) tissue, ectopic gastric mucosa is found in 20%--30% of these cysts, more frequently in small bowel and esophageal duplications [5,6]), a layer of smooth muscle tissue and a common wall with the GI tract (serous or muscle membrane), that usually show no communication with the lumen of the GI tract [7].
Duplications are most frequently single. They characteristically arise from the mesenteric border of the intestine and can be cystic (Type I: 79%) or tubular (Type 2: 21%). Cystic duplications usually present in early childhood as abdominal masses or acute abdomen. Acute onset is due to obstruction or volvulus. However, certain location are more likely to be discovered in adulthood, like an esophageal cyst (approximately 30% [8,9]). Tubular duplication cysts (20%) run parallel to the GI tract, with a communication with it (Fig. 3) [10], [11], [12], [13]. It's worthful in these cases, demonstrating the connection with a magnetic resonance imaging (MRI) for surgical planning [14].
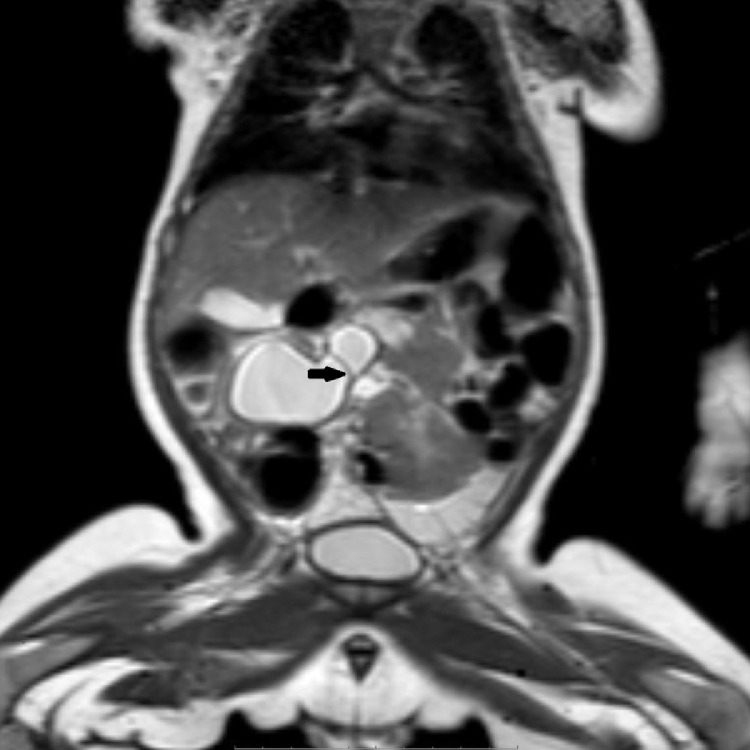
Fig. 3.
Coronal single-shot TSE SENSE T2-weighted (T2W) shows an internal septum (black arrow) between the round and the tubular portion of the cyst.
Case report
A 2-month-old boy was admitted to our hospital for investigation of an anechoic formation of the lower right abdomen founded in prenatal ultrasound.
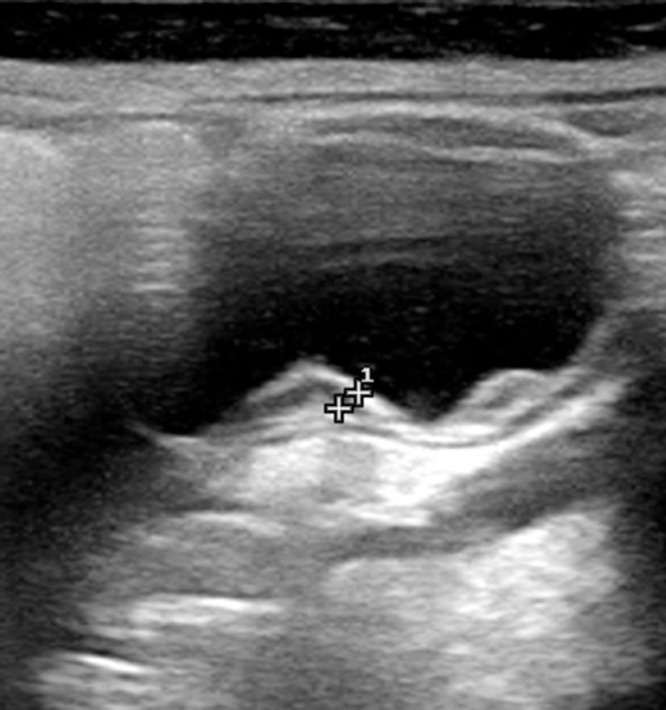
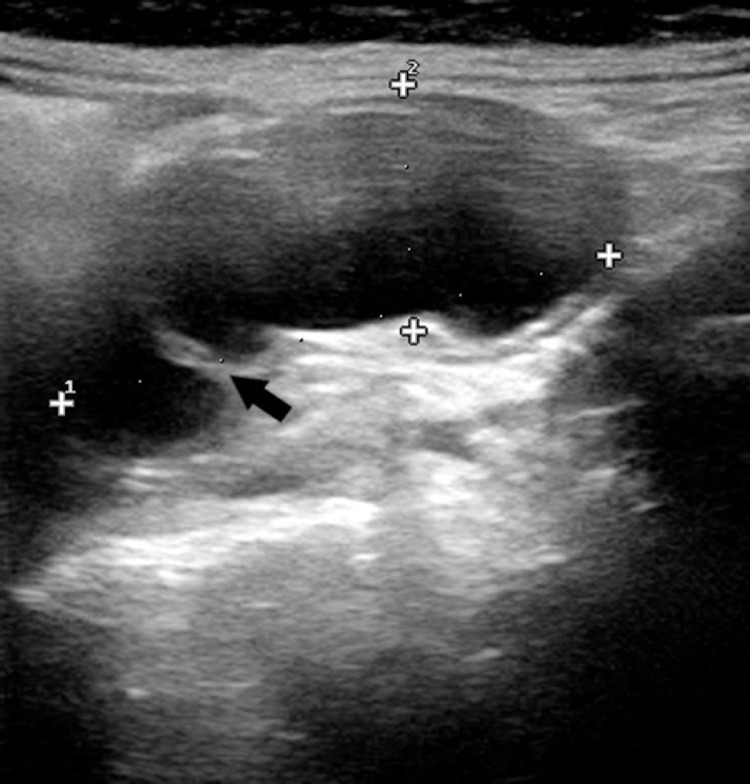
There was no history of recent acute illness or trauma. Blood tests, including liver function tests,and his vital signs were normal on admission. The patient was also afebrile. He performed an ultrasonography (US) after the birth that showed a cystic formation (34 × 23 mm) in the right lower abdomen with a parietal stratification (Fig. 1) of three alternating hyper- and hypoechoic layers (gut sign [15]) with an internal septum (Fig. 2)
Fig. 1.
A cystic formation with a parietal stratification of three alternating hyper- and hypoechoic layers (gut sign).
Fig. 2.
Black arrow point the internal septum between the round and the tubular components of the cyst.
The lesion was consistent with an ileal duplication cyst. A RM was then needed for further investigation and pre-operatory planning.
Abdominal MR was performed by a 1.5 T Philips on narcosis (sedation of the child to prevent movement artifact) and included axial, TSE SENSE T1-weighted (T1W) (TR/TE = 1360.7/11), axial, coronal and sagittal single-shot TSE SENSE T2-weighted (T2W) (TR/TE = 324.7/80), axial and sagittal TFE SENSE T2W (TR/TE = 3.7/1.8) and axial and coronal GRE SPAIR T1W (TR/TE = 4.1/2) imaging.
The exam showed a cystic lesion (simple fluid signal, hyperintense in T2, hypointense in T1) inz the right lower quadrant of the abdomen of 50 × 34 × 30 mm, the cyst had an internal septum between a tubular portion and the terminal round portion (Fig 3), that seems not communicate with the GI tract (Fig. 4)
Fig. 4.

Sagittal single-shot TSE SENSE T2-weighted (T2W) shows the cyst and the GI tract separated by a common wall (white arrow).
There were no vertebral or other abnormalities on MRI.
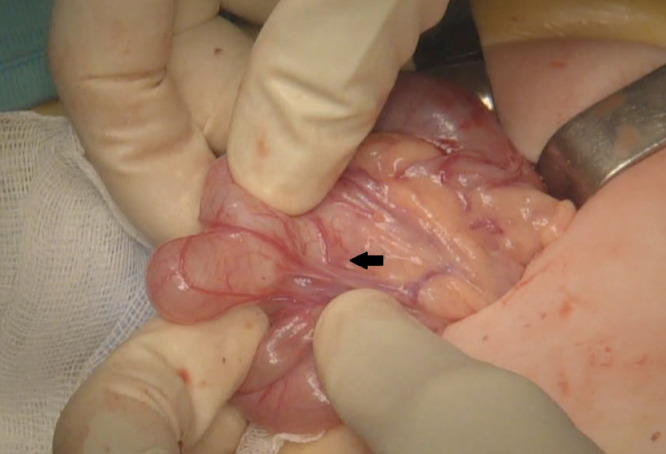
All these findings together strongly suggested the diagnosis of an isolated duodenal duplication cyst. An additional US showed Shortly after undergoing these studies, patient was taken to the operating room and underwent a video-assisted laparoscopy. Laparoscopy showed a duplication cyst originating from the mesenteric side of the bowel, sharing a common muscularis layer with the adjacent bowel (Fig. 5), without communication to the ileal lumen (Fig. 6) at 2 cm from the ileo-cecal valve. The cyst was exteriorized along the cecum and the appendix, drained of 50 cc of colloidal fluid and completely excised. A prophylactic appendicectomy was esecuted.
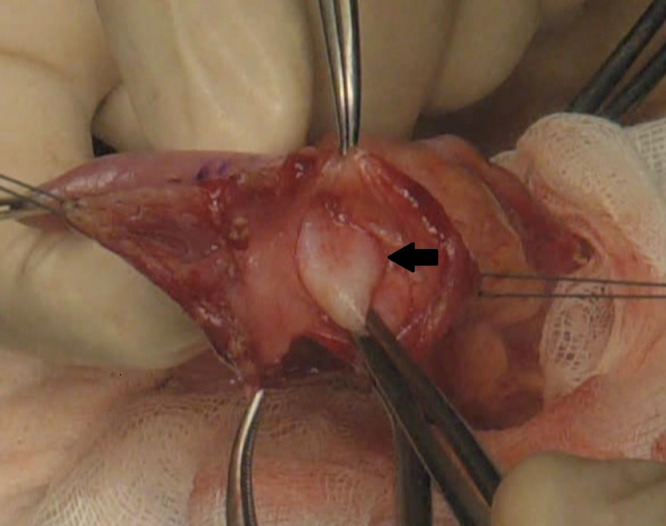
Fig. 5.
A duplication cyst originating from the mesenteric side of the bowel, sharing a common muscularis layer (black arrow) with the adjacent bowel.
Fig. 6.
Cyst does not communicate with the ileal lumen (black arrow show the intact ileal wall beneath the opened cyst).
The patient made an uneventful recovery. Macroscopic and microscopic findings confirmed the diagnosis of a enteric duplication cyst arising from the ileum with a layer of cilindric ciliate epithelium poorly developed (Breath-way like mucosa).
Presently, the patient is in optimal clinical condition and is undergoing a semestral US follow-up.
Discussion
Enteric Duplication cysts (EDCs) are rare congenital malformation that consist in cystic formation in communication with the native GI tract, sharing a common muscular wall and blood supply. The anatomical structure resemble the enteric stratification and the mucosal layer can include ectopic gastric tissue and, less commonly, pancreatic [16,17]. The majority of duplications show clinically at pediatric age, mostly within 2 years of life (80%) [18].
The percentage of early diagnosis, before the onset of clinical symptoms, is raising due the prenatal US screening in the 2° quarter of pregnancy. Less frequently they are diagnosed in adult age incidentally or for complications [19]. The manifestations can be vary and depends on size, localization and the type of mucosal layer [20]. Ileum is the most common localization thus our discussion will be focus on the enteric duplications.
Midgut duplication can be associated with abdominal pain, vomit and abdominal distension, asymptomatic palpable mass, bleeding [21].
The acute onset can be related to an enteric obstruction for the mass effect of the cyst bloated by enteric fluids on the neighboring intestinal loops or for intussusception/volvulus (it also happens during pregnancy).
The cysts with ectopic gastric mucosa or pancreatic tissue can develop ulceration, perforation and acute bleeding with melena [22,23]. Chronic bleeding can cause anemia [24].
US has a central role and often perform diagnosis and surgical planning without further imaging [25].
It's of first choice for his lack of ionizing radiation (essential factor in pediatric age), for being easily repeatable and for being broadly available on territory.
US demonstrates the cystic nature of ECDs, which appear as a hollow structure with anechoic content on the mesenteric side, round shaped (more common) or tubular, frequently unilocular.; sometimes can be multilocular (as in our patient).
Less commonly they are separated with the GI lumen.
US show the intimal connection with the nearby intestine with the “Y-configuration” made by the separation of the common muscular wall shared by the cyst and the near intestine [26].
More specific is the “gut sign” with a hyperechoic internal layer (mucosa) and and a hypoechoic outer layer (smooth muscular tissue) [27]. However other abdominal masses can show a double layer, like the mesenteric cysts and Meckel's diverticulum.
The enteric wall with 5 layer of hyperechoic (mucosa, submucosa, sierosa) and hypoechoic (muscolaris mucosae, muscular layer) can be visible in some cases by expert sonographers and with high-frequencies probes (12-18 Mhz) [28,29].
Being a dynamic imaging, US can show peristaltic activity and eventually changes in shape and size of the cyst [30].
The content can be anhechoic or irregular for the presence of proteic material, blood and sovra-infection [31].
Color-doppler and Power-doppler can show a moderate vascular signal in the cyst wall and the absence of internal vascular signal, thus excluding endoluminal solid components.
Ulceration, inflammation and internal bleeding can make complex the assessment of the nature of the lesion, causing loss of the typical “gut sign” [32].
Phlogosis can cause an increased vascular signal, a dishomogeneous content and a hyperechoic peri-visceral fat [33].
US and abdominal plain film [34] are of first choice in the case of an EDC with acute abdomen.
They can detect signs of enteric obstruction with distension of the intestinal loops, of intussusception or volvulus and eventually of vascular suffering.
Prenatal US can identify around 20-30% of EDCs showing characteristic similar to the post-natal US, although the “gut sign” can be partial or not present [35,36].
MRI and CT aren't diagnostic of routine, the first for the necessity of sedation of the little patient, the later for the use of ionizing radiation [37,38].
They can be used in doubtful cases or for localization hard to reach with the US exploration (Esophagus, rectum). The advantages are multi-planarity (TC and MRI) that allow to gain more information on the anatomical relationships for surgical planning and the multi-parametricity (MRI) that allow to further characterize the lesion [39].
MRI shows the cystic nature of the lesion with high signal on T2W and low signal on T1W sequences (can be high if the cyst has hemorrhagic or proteic content).
In DWI sequences at high value of b they don't show restricted diffusion.
In post-contrast sequences show a good parietal enhancement of similar entity of the near intestine. If complicated can show strong enhancement and parietal thickening, perivisceral edema, hemorrhagic content [40].
TC has scarce indication in pediatric age; even with an onset of acute abdomen the first choice are US and plain film.
In TC the ECD appear as a formation with fluid-density content with mild vascularized wall. If hemorrhagic can be hyperdense on the basal acquisition.
Infection can cause parietal thickening and hyperemia, air-fluid levels, hyperdensity of perivisceral fat [41,42].
Scintigraphy with 99-Technetium pertechnetate can localize ectopic gastric mucosa in patients with enteric bleeding. Differential diagnosis had to be done with the Meckel's Diverticulum, which show similar clinical manifestation and imaging characteristics.
It's a real diverticulum, way more frequent than EDCs and often localized near the ileo-cecal valve on the anti-mesenteric side (unlike EDCs) [43,44].
The contrast follow-through exam can show enteric loop dislocated and the communication with the intestinal lumen of the cyst [45].
Diagnosis it's confirmed after surgical excision and histopathology demonstrate the nature of the mucosal layer.
The authors vastly agree on the necessity of surgical management of EDCs [46].
Surgical treatment is needed in both symptomatic patient and in asymptomatic with incidental diagnosis for the high frequency of complications like enteric obstruction, bleeding, and rare malignant transformation on adult age [47,48]. Moreover, many Authors promote the early surgical treatment (within 6 months of life) [49,50].
In our patient the EDC was diagnosed before the onset of clinical manifestation, allowing an elective laparoscopy, thus significantly reducing the post-operatory morbidity and operatory risks.
The surgical approach consists in complete excision of the EDC with closure of the parietal defect with metallic clips or hand suture. Another laparoscopic approach is the unroofing: partial shell-out of the cyst, optional with draining, closure.
Despite the common blood supply with the near intestine, only in few cases is necessary a segmental resection with end to end or end to side anastomosis [51].
Patient consent
Informed consent was obtained by both the parents of the patient for publication of this case.
Footnotes
Competing interests: We confirm that this work is original and has not been published elsewhere nor is it currently under consideration for publication elsewhere. Publication is approved by all authors and by the responsible authorities where the work was carried out. Each author has participated sufficiently in any submission to take public responsibility for its content. The authors have no conflicts of interest.
References
- 1.Sharma S, Yadav AK, Mandal AK. Enteric duplication cysts in children: a clinicopathological dilemma. J Clin Diagn Res. 2015;9:8–11. doi: 10.7860/JCDR/2015/12929.6381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tiwari C, Shah H, Waghmare M. Cysts of gastrointestinal origin in children: varied presentation. Pediatr Gastroenterol Hepatol Nutr. 2017;20:94–99. doi: 10.5223/pghn.2017.20.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okur MH, Arslan MS, Arslan S. Gastrointestinal tract duplications in children. Eur Rev Med Pharmacol Sci. 2014;18:1507–1512. [PubMed] [Google Scholar]
- 4.Van Zitteren LM, Ruppert M, Op de Beeck B. Infected enteric duplication cyst. BMJ Case Rep. 2017;21:220–221. doi: 10.1136/bcr-2017-222391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erginel B, Soysal FG, Ozbey H. Enteric duplication cysts in children: a single-institution series with forty patients in twenty-six years. World J Surg. 2017;41:620–624. doi: 10.1007/s00268-016-3742-4. [DOI] [PubMed] [Google Scholar]
- 6.Górecki W, Bogusz B, Zajac A. Laparoscopic and laparoscopy assisted resection of enteric duplication cysts in children. J Laparoendosc Adv Surg Tech A. 2015;25:838–840. doi: 10.1089/lap.2015.0103. [DOI] [PubMed] [Google Scholar]
- 7.Berrocal T, Torres I, Gutierrez J. Congenital anomalies of the upper gastrointestinal tract. Radiographics. 1999;19:855–872. doi: 10.1148/radiographics.19.4.g99jl05855. [DOI] [PubMed] [Google Scholar]
- 8.Kuhlman JE, Fishman EK, Wang KP. Esophageal duplication cyst: CT and transesophageal needle aspiration. Am J Roentgenol. 1985;145:531–532. doi: 10.2214/ajr.145.3.531. [DOI] [PubMed] [Google Scholar]
- 9.Salo JA, Ala-Kulju KV. Congenital esophageal cysts in adults. Ann Thorac Surg. 1987;44:135–138. doi: 10.1016/s0003-4975(10)62023-1. [DOI] [PubMed] [Google Scholar]
- 10.Macpherson RI. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13:1063–1080. doi: 10.1148/radiographics.13.5.8210590. [DOI] [PubMed] [Google Scholar]
- 11.Rasool N, Safdar CA, Ahmad A. Enteric duplication in children: clinical presentation and outcome. Singapore Med J. 2013;54:343–346. doi: 10.11622/smedj.2013129. [DOI] [PubMed] [Google Scholar]
- 12.Glazer HS, Siegel MJ, Sagel SS. Low-attenuation mediastinal masses on CT. Am J Roentgenol. 1989;152:1173–1177. doi: 10.2214/ajr.152.6.1173. [DOI] [PubMed] [Google Scholar]
- 13.Graeber GM, Thompson LD, Cohen DJ. Cystic lesion of the thymus. an occasionally malignant cervical and/or anterior mediastinal mass. J Thorac Cardiovasc Surg. 1984;87:295–300. [PubMed] [Google Scholar]
- 14.Olajide AR, Yisau AA, Abdulrasees NA. Gastrointestinal duplications: experience in seven children and a review of the literature. Saudi J Gastroenterol. 2010;16:105–109. doi: 10.4103/1319-3767.61237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Serafino M, Mercogliano C, Vallone G. Ultrasound evaluation of the enteric duplication cyst: the gut signature. J Ultrasound. 2016;19:131–133. doi: 10.1007/s40477-015-0188-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berrocal T, Hidalgo P, Gutiérrez J. Imagen radiológica de las duplicaciones del tubo digestivo. Radiología. 2004;46:282–292. [Google Scholar]
- 17.Erginel B, Soysal FG, Ozbey H. Enteric duplication cysts in children: a single-institution series with forty patients in twenty-six years. World J Surg. 2017;41:620–624. doi: 10.1007/s00268-016-3742-4. [DOI] [PubMed] [Google Scholar]
- 18.Karnak I, Ocal T, Senocak ME. Alimentary tract duplications in children: report of 26 years’ experience. Turk J Pediatr. 2000;42:118–125. [PubMed] [Google Scholar]
- 19.Ashish G, Karikal C, Bramhadatta P. Duplication cyst of ileum presenting as acute intestinal obstruction in an adult. BMJ Case Rep. 2016;2016:211–213. bcr2016214775. [Google Scholar]
- 20.Iyer CP, Mahour GH. Duplications of the alimentary tract in infants and children. Journal of Pediatric Surgery. 1995;30(9):1267–1270. doi: 10.1016/0022-3468(95)90482-4. [DOI] [PubMed] [Google Scholar]
- 21.Okur MH, Arslan MS, Arslan S. Gastrointestinal tract duplications in children. Eur Rev Med Pharmacol Sci. 2014;18:1507–1512. [PubMed] [Google Scholar]
- 22.Sakamoto K, Hasegawa S, Yamazaki Y. Ileal duplication presenting as perforation: report of a case. Surg Today. 2000;30:445–447. doi: 10.1007/s005950050621. [DOI] [PubMed] [Google Scholar]
- 23.Niesche JW. Duplication of the small bowel with peptic ulcer perforation. Aust NZ J Surg. 1973;42:4. doi: 10.1111/j.1445-2197.1973.tb06818.x. [DOI] [PubMed] [Google Scholar]
- 24.Yumi T, Katsushi H, Yosuke M. Duplication cyst of the ileum presenting with severe anemia detected by double-balloon endoscopy. Endoscopy International Open. 2018;06:E395–E398. doi: 10.1055/s-0043-125142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mihmanli I, Erdogan N, Kurugoglu S. Radiological workup in mesenteric cysts: insight of a case report. J Clinical Imaging. 2001;25:47–49. doi: 10.1016/s0899-7071(01)00250-9. [DOI] [PubMed] [Google Scholar]
- 26.Kim YJ, Kim YK, Jeong YJ. Ileal duplication cyst: Y-configuration on in vivo sonography. J Pediatr Surg. 2009;44:1462–1464. doi: 10.1016/j.jpedsurg.2009.03.034. [DOI] [PubMed] [Google Scholar]
- 27.Fonseca EKUN, Sameshima YT. Gut signature sign in en- teric duplication cysts. Abdom Radiol (NY) 2018 doi: 10.1007/s00261-018-1620-2. [DOI] [PubMed] [Google Scholar]
- 28.Kumar D, Ramamathan S, Haider E. Gastroenterology: revisiting the forgotten sign: five layered gut sig-nature and Y configuration in enteric duplication cysts on high-resolution ultrasound. J Gastroenterol Hepatol. 2015;30:1111. doi: 10.1111/jgh.12903. [DOI] [PubMed] [Google Scholar]
- 29.Cheng G, Soboleski D, Daneman A. Sonographic pitfalls in the diagnosis of enteric duplication cysts. AJR Am J Roentgenol. 2005;184:521–525. doi: 10.2214/ajr.184.2.01840521. [DOI] [PubMed] [Google Scholar]
- 30.Spottswood SE. Peristalsis in duplication cyst: a new diagnostic sonographic finding. Pediatr Radiol. 1994;24(5):344–345. doi: 10.1007/BF02012124. [DOI] [PubMed] [Google Scholar]
- 31.Liu R, Adler D. Duplication cysts: diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound. 2014;3:152–160. doi: 10.4103/2303-9027.138783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheng G, Soboleski D, Daneman A. Sonographic pitfalls in the diagnosis of enteric duplication cysts. AJR Am J Roentgenol. 2005;184:521–525. doi: 10.2214/ajr.184.2.01840521. [DOI] [PubMed] [Google Scholar]
- 33.Van Zitteren LM, Ruppert M, Op de Beeck B. Infected enteric duplication cyst. BMJ Case Rep. 2017;21:220–221. doi: 10.1136/bcr-2017-222391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iyer C.P., Mahour G.H. Duplications of the alimentary tract in infants and children. J. Pediatr. Surg. 1995;30:1267–1270. doi: 10.1016/0022-3468(95)90482-4. [DOI] [PubMed] [Google Scholar]
- 35.Basany L, Aepala R, Mohan Reddy Bellary M. Intestinal obstruction due to ileal duplication cyst and malrotation in a preterm neonate. J Neonatal Surg. 2015;4:48. [PMC free article] [PubMed] [Google Scholar]
- 36.Nishizawa C, Cajusay-Velasco S, Mashima M. HDlive imaging of fetal enteric duplication cyst. J Med Ultrason. 2014;41:511. doi: 10.1007/s10396-014-0548-6. [DOI] [PubMed] [Google Scholar]
- 37.Udiya AK, Shetty GS, Chauhan U. Multiple isolated enteric duplication cysts in an infant - a diagnostic dilemma. J Clin Diagn Res. 2016;10:TD15–TD16. doi: 10.7860/JCDR/2016/15129.7129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rasool N, Safdar CA, Ahmad A. Enteric duplication in children: clinical presentation and outcome. Singapore Med J. 2013;54:343–346. doi: 10.11622/smedj.2013129. [DOI] [PubMed] [Google Scholar]
- 39.Lee NK, Kim S, Jeon TY. Complications of congenital and developmental abnormalities of the gastrointestinal tract in ad adolescents and adults: evaluation with multimodality imaging. Radiographics. 2010;30(6):1489–1507. doi: 10.1148/rg.306105504. [DOI] [PubMed] [Google Scholar]
- 40.Hur J, Yoon CS, Kim MJ. Imaging features of gastrointestinal tract duplications in infants and children: from esophagus to rectum. Pediatr Radiol. 2007;37:691–699. doi: 10.1007/s00247-007-0476-3. [DOI] [PubMed] [Google Scholar]
- 41.Udiya AK, Shetty GS, Chauhan U. Multiple isolated enteric duplication cysts in an infant - a diagnostic dilemma. J Clin Diagn Res. 2016;10:TD15–TD16. doi: 10.7860/JCDR/2016/15129.7129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rasool N, Safdar CA, Ahmad A. Enteric duplication in children: clinical presentation and outcome. Singapore Med J. 2013;54:343–346. doi: 10.11622/smedj.2013129. [DOI] [PubMed] [Google Scholar]
- 43.Yang JG, Yin CH, Li CL. Meckel's diverticulum and intestinal duplication detected by Tc-99m pertechnetate scintigraphy. Clin Nucl Med. 2010;35(4):275–276. doi: 10.1097/RLU.0b013e3181d18eca. [DOI] [PubMed] [Google Scholar]
- 44.Hamza AR, Bicaj BX, Kurshumliu FI. Mesenteric Meckel's diverticulum or intestinal duplication cyst: a case report with review of literature. Int J Surg Case Rep. 2016;26:50–52. doi: 10.1016/j.ijscr.2016.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Olajide AR, Yisau AA, Abdulraseed NA. Gastrointestinal duplications: Experience in seven children and a review of the literature. Saudi J Gastroenterol. 2010;16(2):105–109. doi: 10.4103/1319-3767.61237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Górecki W, Bogusz B, Zajac A. Laparoscopic and laparoscopy assisted resection of enteric duplication cysts in children. J Laparoendosc Adv Surg Tech A. 2015;25:838–840. doi: 10.1089/lap.2015.0103. [DOI] [PubMed] [Google Scholar]
- 47.Blank G, Königsrainer A, Sipos B. Adenocarcinoma arising in a cystic duplication of the small bowel: case report and review of literature. World J Surg Oncol. 2012;10:55. doi: 10.1186/1477-7819-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beltrán MA, Barría C, Contreras MA. Adenocarcinoma and intestinal duplication of the ileum. report of one case. Rev Med Chil. 2009;137:1341–1345. [PubMed] [Google Scholar]
- 49.Laje P, Flake AW, Adzick AS. Prenatal diagnosis and post-natal resection of intra-abdominal enteric duplications. J PediatrSurg. 2010;45:1554–1558. doi: 10.1016/j.jpedsurg.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 50.Foley PT, Sithasanan N, McEwing R. Enteric duplications presenting as antenatally detected abdominal cysts: is delayed resection appropriate? J Pediatr Surg. 2003;38:1810–1813. doi: 10.1016/j.jpedsurg.2003.08.032. [DOI] [PubMed] [Google Scholar]
- 51.Patiño MJ, Bettolli M. Alimentary tract duplications in newborns and children: diagnostic aspects and the role of laparoscopic treatment. World J Gastroenterol. 2014;20(39):14263–14271. doi: 10.3748/wjg.v20.i39.14263. [DOI] [PMC free article] [PubMed] [Google Scholar]