Abstract
Introduction
The median sacral artery injury is a rare entity, especially in trauma. And the injuries are always with pelvic fractures. We describe a case of the median sacral injury which was induced by blunt trauma without pelvic fractures.
Case presentation
A 26-year-old male who suffered L4–5 fracture dislocation and some hemorrhage in pelvic cavity following a motorcycle accident. He had a median sacral artery injury, and we tried to the trans-catheter arterial embolization, however it could not be success. The embolization was performed using of gelatin sponges in bilateral internal iliac artery and left 4th lumber artery. After his admission, a demand of transfusions lasted for 7 days.
Conclusion
We successfully treated a case of median sacral avulsion injury by choosing conservative treatment.
Keywords: Hemorrhage, Median sacral artery, Trans-catheter embolization, Trauma
Introduction
The median sacral artery (MSA) always arises from the posterior wall of the aortic bifurcation, and goes down in front of the sacral bone [1]. To our knowledge, there are some reports of iatrogenic MSA injury [2,3] or trans-catheter embolization (TAE) for rectal bleeding [4], but there were no English reports of trauma-induced MSA injury. As far as we could investigate, there were only three Japanese reports and 4 cases of trauma-induced MSA injury [[5], [6], [7]]. All of these 4 cases had pelvic fractures around of the MSA and were estimated to be caused by direct damage.
In this time, we present a rare case of trauma-induced MSA injury without pelvic fracture.
Case presentation
A 26-year-old male who had no history of any disease or medication, fell on a motorcycle and was hit right side of his abdomen by a tree. At pre-hospital state, his vital sings were as follows; Glasgow Coma Scale E4V5M6, blood pressure 84/60 mmHg, heart rate 130 bpm, respiratory rate 30/min. He complained of bilateral complete paralysis of lower limbs and sensory disorder of his left limb. He was administered tranexamic acid (1 g) and was transported to our hospital by a physician-staffed helicopter.
His vital signs at the emergency room were as follows; Glasgow Coma Scale E4V4M6, blood pressure 74/44 mmHg, heart rate 145 bpm, SpO2 100% (O2 10L), body temperature 37.2 °C. We immediately started blood transfusion and intubated after administration of Ketamine (70 mg) and Fentanyl (100 μg). Portable X-ray performed to assess the presence of unstable pelvic fracture given his unstable vital signs revealed a complex fracture dislocation of the lumber spine from L4–5 (Fig. 1). An enhanced computed tomography (CT) scan showed a right hemopneumothorax, an L4–5 lateral fracture dislocation, some arterial extravasations around the lumber spine and extravasations from MSA (Fig. 2A, B). At the same time, we found that there were no pelvic fractures. After placing a right thoracostomy tube, emergency interventional radiology (IVR) for trans-catheter artery embolization (TAE) was performed. Non-selective TAE was performed using of gelatin sponges in bilateral internal iliac artery as damage control strategies [8]. Moreover, the extravasations from fourth left lumber artery were found, and TAE was performed using the same materials. However, it was difficult to select MSA, radiologist gave up the embolization of MSA, and the patient was transported to intensive care unit (ICU). After his admission to ICU, a demand of transfusions lasted for first 7 days, the consumption of transfusions until this time was follows; red blood cell 30 units, fresh frozen plasma 20 units and platelets 20 units.
Fig. 1.
Portable X-radiograph showing L4–5 fracture dislocation.
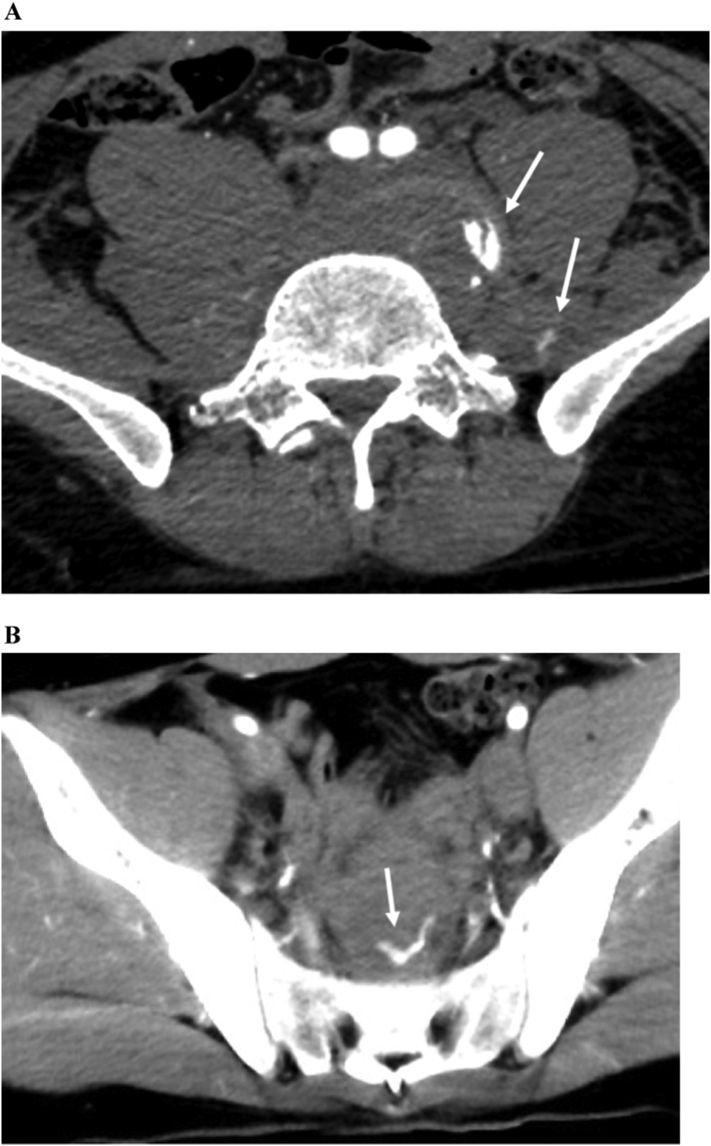
Fig. 2.
A. Contrast enhanced CT scan showing some extravasations (white arrows) around L4–5 fracture dislocation. B. Contrast enhanced CT scan showing an extravasation (white arrow) from median sacral artery.
We fixed the trunk by connecting the external fixation of the pelvis and the halo vest until the intervertebral fixation had been performed by surgery (Fig. 3).
Fig. 3.
Trunk fixation connecting the external fixation of the pelvis and the halo vest.
The surgical operation was performed via a posterior approach to combine L2 to S1 using pedicular screws and titanium rods on day 7, and oblique lateral interbody fusion of L4 to L5 was performed on day 25 (Fig. 4A, B).
Fig. 4.
A, B. X-radiograph of around L4-L5 after the surgical operation on day 25.
He was transferred to a rehabilitation hospital on the day 46. At this time, all of his muscular strength reached 5/5 in hip flexors and quadriceps femoris and 0/5 in dorsiflexion strength of both ankles. Neurological examination revealed hypoesthesia over the surface of both ankles and loss of bowel and bladder function.
Discussion
This case presents a very rare type of injury, mainly in two respects. The first reason is that he was injured the median sacral artery by blunt trauma. We could have found only two cases of MSA injury which were caused by not trauma, but iatrogenic injury [2,3]. As far as we could investigate, there were only three Japanese reports and 4 cases of trauma-induced MSA injury [[5], [6], [7]]. The present case is the first paper which reported trauma-induced MSA injury.
The second is what this MSA injury was without any pelvic fractures. The two English reports were both iatrogenic [2,3], thus we described the five MSA injury cases in Table 1 except for the two reports. All cases, except for the present case, had pelvic fractures, thus the mechanism of these MSA injuries seems to be that the MSA was damaged directly. On the other hand, in this case, there were no fractures or other organ damage around the site of MSA hemorrhage. Since there was a L4–5 dislocation fracture, it is possible that the pulling force of the soft tissue around the dislocation fracture caused the arterial “avulsion” on the MSA.
Table 1.
Trauma-induced MSA injury, review of the literature.
| Reference/year | Age | Sex | Etiology | Site of pelvic fracture | Site of TAE | Outcome | |
|---|---|---|---|---|---|---|---|
| 1 | Kawamata et al., 1991 Japanese [5] | 72 | M | Traffic accident | B pubis, B sacrum |
B internal iliac, MSA | Death |
| 2 | 35 | F | Fall | Lt sacroiliac joint, pubis and ilium, coccyx | B internal iliac, Lt 4th lumber MSA |
Survive | |
| 3 | Nishiyama et al., 2010 Japanese [6] | 70 | M | Traffic accident | L5/S1 chip fracture | B sacral, Lt lumber | Survive |
| 4 | Tohma et al., 2019 Japanese [7] | 80 | F | Fall | pelvic ring, sacrum | B internal iliac, MSA | Survive |
| 5 | Present case | 26 | M | Traffic accident | N/A | B internal iliac, Lt 4th lumber | Survive |
B: bilateral, Lt: left, MSA: median sacral artery, N/A: not applicable.
TAE is the general treatment of choice for the MSA injury. However, the diameter of MSA of adult person is about 2 mm [1], it is difficult to select by the catheter [4]. Especially in the case of acute phase of polytrauma where urgent treatment is desired, it becomes more difficult because of time constraints. In this case, contrast enhanced CT showed extravasations from the MSA, however at the time of IVR, no remarkable extravasations were observed from the abdominal aortic contrast, then we opted for conservative therapy rather than forcible vessel selection or surgery of laparotomy. As a result, the demand for blood transfusion was prolonged, however the coagulation function could be observed without failure. Conservative treatment reduced the invasion due to laparotomy and avoided complications, such as infection, deep venous thromboembolism, and bleeding [9]. This approach may have had the potential advantage of performing operation for vertebral body fixation at early stage.
Conclusion
TAE is generally the treatment of first choice for MSA injury, but there are some situations in which the vascular diameter is thin, making catheter selection difficult. In the present case, the demand for blood transfusion was prolonged by conservative therapy; however the patient was able to undergo vertebral body fusion for L4–5 lateral dislocation fracture without any deteriorating in the general condition and ultimately survived to discharge.
Funding
None.
CRediT authorship contribution statement
HN drafted the work; KO and YY substantively revised it. All authors approved the submitted version, have agreed both to be personally accountable for the author's own contributions. All authors read and approved the final manuscript.
Declaration of competing interest
None.
Acknowledgments
Acknowledgement
The drafting of this manuscript was financially supported by the Ministry of Education, Culture, Sports, Science and Technology (MEXT)-Supported Program for the Strategic Research Foundation at Private Universities, 2015-2019 concerning [The constitution of total researching system for comprehensive disaster, medical management, corresponding to wide-scale disaster]. The funds are used for payment of English correction fees and posting fees.
References
- 1.Dimov I., Sobczak S., Grabs D. The median sacral artery in rectal blood supply: a cadaveric study. Clin. Anat. 2020 Apr;22:1–6. doi: 10.1002/ca.23611. [DOI] [PubMed] [Google Scholar]
- 2.Al Zahrani Y., Peck D. Median sacral artery injury following a bone marrow biopsy successfully treated with selective trans-arterial embolization: a case report. J. Med. Case Rep. 2016 Feb 24;10:42. doi: 10.1186/s13256-016-0827-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Young U.K., Eun Y.C., Ji Hoon L. Median sacral artery injury during percutaneous mechanical disc decompression using Dekompressor. Korean J. Anesthesiol. 2014;67(Suppl):S60–S61. doi: 10.4097/kjae.2014.67.S.S60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee J.H., Lee K.H., Chung W.S. Transcatheter embolization of the middle sacral artery: collateral feeder in recurrent rectal bleeding. ARJ Am. J. Roentgenol. 2004 Apr;182(4):1055–1057. doi: 10.2214/ajr.182.4.1821055. [DOI] [PubMed] [Google Scholar]
- 5.Kawamata H., Kumazaki T., Tajima H. Value of “additional arterial embolization” to bilateral internal iliac TAE in patients with severe pelvic fracture. Nihon Igaku Houshasen Gakkai Zasshi. 1991 Jun 25;51(6):649–655. (Japanese) [PubMed] [Google Scholar]
- 6.Nishiyama R., Maruyama T., Shichijyo Y. A case of median sacral artery bleeding stopped by direct surgical ligation. J. Abdom. Emerg. Med. 2010;30(4):587–590. doi: 10.11231/jaem.30.587. (Japanese) [DOI] [Google Scholar]
- 7.Tohma T., Okabe Y., Inada D. Life-threatening injury of the median sacral artery due to severe pelvic fracture successfully treated by transcatheter arterial embolization: a case report. J. Abdom. Emerg. Med. 2019;39(1):105–107. doi: 10.11231/jaem.39.105. (Japanese) [DOI] [Google Scholar]
- 8.Otsuka H., Sato T., Sakurai K. Use of interventional radiology as initial hemorrhage control to improve outcomes for potentially lethal multiple blunt injuries. Injury. 2018;49(2):226–229. doi: 10.1016/j.injury.2017.11.038. [DOI] [PubMed] [Google Scholar]
- 9.Williams M.D., Watts D., Fakhry S. Colon injury after blunt abdominal trauma: results of the EAST multi-institutional hollow viscus injury study. J. Trauma. 2003;55(5):906–912. doi: 10.1097/01.ta.0000093243.01377.9b. [DOI] [PubMed] [Google Scholar]