Abstract
Introduction:
Pheochromocytomas are catecholamine-producing tumors presenting with various clinical symptoms and a serious potentially lethal cardiovascular complications due to the potent effects of secreted catecholamines. Glucoregulation disorders could also occur leading to impaired glucose tolerance and diabetes mellitus. The aim of our study was to determine the effects of adrenalectomy on patient recovery with regard to their glycemic status.
Materials and Methods:
Case notes of all patients who underwent adrenalectomy surgery for pheochromocytoma from 2009 to 2018, followed up in the Department of Diabetology, Endocrinology, and Nutrition at University Hospital Center Hassan II of Fez, were retrieved, and data were collected from them to identify those with preoperative diagnosis of glucoregulation disorder and to verify if adrenalectomy can reverse or improve glycemic abnormality.
Results:
Overall, 23 patients underwent surgery for pheochromocytoma, 26% of cases had diabetes mellitus, whereas 34.78% had glucose intolerance. One year after surgery, diabetes and glucose intolerance were cured in 57.14% of cases. We noticed also that patients with large and symptomatic tumors were more likely to develop preoperative diabetes; it was also more likely to persist in patients who had an elevated body mass index (BMI).
Conclusions:
In our data, diabetes and glucose intolerance were found concurrently with pheochromocytoma in 60.78% of patients. Thus, it is important for clinicians to screen for glycemic disorder when pheochromocytoma is diagnosed, especially in patients with other risk factors for developing type 2 diabetes such as elevated BMI. Removal of these tumors can reduce insulin secretion and severe peripheral insulin resistance making early diagnosis important.
Keywords: Diabetes mellitus, glucose intolerance, pheochromocytoma, resolution after resection, Diabète sucré, intolérance au glucose, phéochromocytome, résolution après résection
Résumé
Introduction:
Les phéochromocytomes sont des tumeurs productrices de catécholamines, ils se manifestent par divers symptômes cliniques et des complications cardiovasculaires mortelles dues aux effets puissants des catécholamines sécrétées. Des troubles de la glucorégulation peuvent également survenir, à savoir une intolérance au glucose ou un diabète sucré. Le but de notre étude est de déterminer l'effet de la surrénalectomie de nos patients sur l'amélioration du statut glycémique.
Matériels et méthodes:
Il s'agit d'une étude rétrospective, incluant tous les patients qui ont subi une surrénalectomie pour phéochromocytome et suivis au Département de Diabétologie, Endocrinologie et Nutrition du Centre Hospitalier Universitaire Hassan II de Fès de 2009 à 2018. Nous avons recueilli les données pour identifier les personnes ayant un diagnostic préopératoire de trouble de glucorégulation et pour vérifier si la surrénalectomie a pu guérir ou améliorer l'anomalie glycémique.
Résultats:
Dans l'ensemble, 23 patients ont été opérés d'un phéochromocytome, 26% des cas avaient un diabète sucré, alors que 34,78% avaient une intolérance au glucose. Un an après la chirurgie, le diabète et l'intolérance au glucose ont été guéris dans 57,14% des cas. Nous avons également remarqué que les patients atteints de tumeurs volumineuses et symptomatiques étaient plus susceptibles de développer un diabète préopératoire; il était également plus susceptibles de persister chez les patients ayant un indice de masse corporelle (IMC) élevé.
Conclusions:
Dans nos données, le diabète et l'intolérance au glucose ont été retrouvés simultanément avec un phéochromocytome chez 60,78% des patients. Ainsi, il est important pour les cliniciens de dépister les troubles glycémiques lorsque le phéochromocytome est diagnostiqué, en particulier chez les patients présentant d'autres facteurs de risque de développer un diabète de type 2 tels qu'un IMC élevé. La résection de ces tumeurs peut réduire la sécrétion d'insuline et la résistance périphérique sévère à l'insuline, ce qui rend le diagnostic précoce important.
INTRODUCTION
Pheochromocytomas are rare neuroendocrine tumors of the adrenal medullar, and the first diagnosis was made in 1886, by Frankel.[1]
The pathogenesis of glucoregulation disorders in pheochromocytomas may be explained by the relationship between catecholamines, metanephrine levels, and insulin resistance. Elevated catecholamine levels result in increased insulin resistance and decreased insulin secretion through receptors α2-adrenergic.[2,3] Furthermore, increased catecholamine levels are also associated with decreased glucose uptake and increased gluconeogenesis and glycogenolysis.[4]
Consequently, 15%–35% of patients with pheochromocytoma could be complicated with impaired glucose tolerance or diabetes.[4,5]
These relationships have been shown to reverse after the resection of pheochromocytoma.
In this study, we aimed to determine the incidence of diabetes in patients with pheochromocytoma and the outcomes of these patients after surgery. In addition, we attempted to identify the factors associated with the development or resolution of diabetes.
MATERIALS AND METHODS
A retrospective study was conducted at the Department of Endocrinology, Diabetology, and Nutrition at the University Hospital Center Hassan II in Fez, from January 2009 to December 2018. We had included all patients with pheochromocytoma confirmed biologically (all patients had 24 h urine metanephrines and catecholamines measured) and histologically.
Inclusion criteria
Patients operated on during this period, with pre- and postoperative glycemic assessment were included in the study.
Exclusion criteria
Patients with incomplete information in the case notes were excluded from the study.
Factors evaluated were patient age, body mass index (BMI), family history of diabetes mellitus, type and treatment of diabetes mellitus, duration of diabetes mellitus; information on pre- and postoperative blood glucose was also collected. Fasting blood glucose and hemoglobin A1c (for diabetic patients) were determined by the routine analysis in our laboratory. Fasting blood glucose was measured before, and then was repeated on the day of discharge, at 3 months postoperative and 1 year after the pheochromocytoma surgery. A value ≥7 mmol/l confirms the diagnosis of diabetes mellitus; values within these limits 6.1–6.9 mmol/l are an indication for oral glucose tolerance test (OGTT), looking for glucose intolerance, performed as described by the World Health Organization, using a glucose load containing the equivalent of 75 g anhydrous glucose dissolved in water.[6] Diabetic patients were evaluated on postoperative blood tests, insulin requirements, and dosage of oral hypoglycemic, to assess whether any of them had an improvement or even a resolution of diabetes after pheochromocytoma surgery. Fasting blood glucose was used to determine the glucose intolerance evolution.
Data were plotted on a table in the Microsoft Excel 2010 program. The statistical analysis was performed using the SPSS 23.0 (IBM Corporation, Armonk, NY, USA); P < 0.05 was considered statistically significant. Multivariate analysis was performed using binary logistic regression; the results are presented in terms of percentages and numbers, otherwise as median.
RESULTS
During the study period, 25 pheochromocytoma patients were identified, 2 patients (8%) were excluded due to incomplete information, and 23 patients (92%) were included in the study.
Concerning the 23 included patients with pheochromocytoma, 60.80% were female with a gender ratio of 1.5 and a mean age of surgery 37.13 ± 9.29 years. The average BMI of our patients was 19.14 ± 4.29 kg/m2, with 24.5 kg/m2 for diabetics and 19.44 kg/m2 for patients with glucose intolerance [Table 1].
Table 1.
Preoperative characteristics of patients undergoing surgery for pheochromocytoma and comparison of pheochromocytoma patients with and without preoperative diabetes or glucose intolerance
| Patients with pheochromocytoma | All patients (n=23) | Diabetes (n=6) | Glucose intolerance (n=8) |
|---|---|---|---|
| Male | 9 | 2 | 2 |
| Female | 14 | 4 | 6 |
| Age at surgery (years) | 37.13 | 39.60 | 32.08 |
| BMI (kg/m²) | 19.14 | 24.5 | 19.44 |
| Size on preoperative imaging (mm) | 50.88 | 74.66 | 46.28 |
BMI=Body mass index
Among 23 patients, 14 patients (60.86%) met the criteria for having preoperative evidence of diabetes or glucose intolerance. For the 6 (26.08%) diabetic patients, 4 of the patients had a history of type 2 diabetes with a duration of evolution ranging from 1 to 5 years, and 2 patients were revealed to be diabetic while diagnosed to have pheochromocytoma by fasting blood glucose ≥7 mmol/l twice. Glucose intolerance was observed in 8 (34.78%) cases with OGTT.
After surgery, histology of different tumors revealed no histological evidence of malignancy.
Regarding the size of pheochromocytoma, the average size was 50.88 mm, with a larger average size in diabetic patients, 74.66 ± 11.98 mm, than in patients with glucose intolerance (46.28 mm), however in patients without a glucoregulation disorder, the mean tumor size was the smallest (39.11 mm).
Improvement or resolution of diabetes and glucose intolerance after the resection of pheochromocytoma was obtained from 71.42%, including 57.14% resolution. In detail, 33.33% of diabetic patients got complete resolution, which was defined as being off medication with evidence of either normal fasting blood glucose or hemoglobin A1c. The same percentage had been found in diabetic patients who were reported to have better glucose control with reduced dose of medication. However, 33% of diabetic patients did not get any improvement in their diabetes after surgery [Figure 1]. They all needed the same dose of medication for their diabetes and found no improvement in glucose control during the postoperative period.
Figure 1.
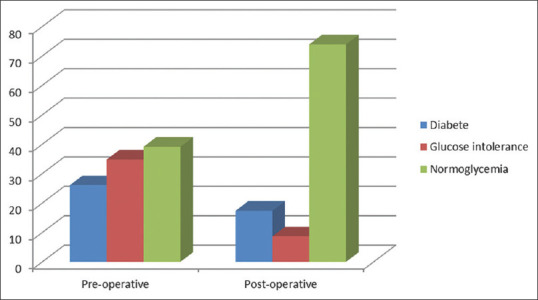
Evolution of diabetes and glucose intolerance in pre- and postsurgery of pheochromocytoma
Moreover, 75% of patients with glucose intolerance achieved normalization of glycemic control.
The BMI of patients with complete or partial resolution of diabetes was lower than that of patients without resolution. Finally, patients with larger symptomatic tumors and family history of diabetes were less likely to have their diabetes resolved.
DISCUSSION
In this study, we examined a series of patients undergoing surgery for pheochromocytoma to determine both the prevalence of preoperative diabetes or glucose intolerance and the probability of becoming normoglycemic after tumor resection.
Of the 23 patients, 26% had signs of diabetes mellitus, which is similar to the 12.41%–40% incidence reported by other series of patients with pheochromocytoma.[4,7,8,9,10,11] Regarding glucose intolerance, only a few series put the points on this subgroup, with a very variable prevalence reaching up to 71% in the study by Pogorzelski et al.[7] and only 5.22% in the series by Beninato et al.,[8] whereas the median observed in our study was 34.78% [Table 2].
Table 2.
Comparison with other studies examining pheochromocytoma and diabetes
| Study | Number | Preoperative | Postoperative | ||
|---|---|---|---|---|---|
| Diabetes (%) | Glucose intolerance (%) | Resolution diabetes and glucose intolerance (%) | Improvement diabetes (%) | ||
| Our study | 23 | 26.08 | 34.78 | 57.14 | 33.33 |
| Pogozeliski et al.[5] | 67 | 28.6 | 71.4 | 90.47 | - |
| Benito et al.[6] | 153 | 12.41 | 5.22 | 78.57 | 14.28 |
| Stenstom et al.[7] | 60 | 31.66 | - | 78.94 | - |
| La Batide-Alanore et al.[8] | 191 | 35.6 | - | 90 | - |
| Liu et al.[9] | 185 | 36.2 | - | 78.7 | - |
| Sahli et al.[10] | 27 | 40 | - | 14.8 | - |
We found that diabetic patients were more likely to have large symptomatic tumors, which agrees with the other series.[8] Indeed, the average size of the tumor in our study was 50.88 mm, and the larger tumors were more common in diabetic patients (male size 74.66 ± 11.98 mm) and were associated with higher catecholamine levels than smaller tumors.
This can be explained by the fact that larger tumors might increase the risk of diabetes or glucose intolerance by exposing patients to higher catecholamine levels. This finding was initially observed in a study by Stenström et al.,[9] who published a study in 1984 involving sixty pheochromocytoma patients, of whom 31.66% had hyperglycemia.
However, all patients with large symptomatic tumors do not develop diabetes. Other factors that may make some patients more susceptible than others to hyperglycemia include high BMI and tumor characteristics, in addition to the metabolic stress of pheochromocytoma.
We also found that patients with diabetes or glucose intolerance had a normal BMI, but their BMI was higher compared to that of normal patients. However, other studies have shown that lower BMI was associated with large tumors and the development of diabetes.[8] Other studies did not find a positive relationship between BMI and the risk of diabetes.[4,10]
It is assumed that the relationship between increased BMI and diabetes development is masked by weight loss due to catecholamine-induced lipolysis in some patients.[9]
After the surgery, 33.33% of patients improved their diabetes, and it is higher than the percentage observed in Beninato et al.,[8] whereas healing has affected more than half of the cases (57.14%) in our series. However, some researchers have reported that even more than 90% of patients could resolve diabetes [Table 2].
Another study, La Batide-Alanore et al.,[4] conducted in 2003, revealed that 90% of diabetic patients resolved after surgery; the 10% who did not resolve had an incomplete resection of their tumor. They identified age, duration of hypertension, plasma adrenaline concentration, and urinary excretion of metanephrine as risk factors for developing diabetes.
However, rates close to 78% of resolution have been revealed by the studies by Beninato et al., Stenström et al., and Liu et al.[8,9,10] Finally, the lowest rate of resolution (14.8%) was reported by Sahli et al.[11]
Among the six diabetic patients, two did not have any change in their glycemic profile, these two patients had high BMI (24.2 kg/m2 and 28.5 kg/m2), unlike those who presented an improvement see a resolution of their glycemic disorder.
We find that BMI no high was perhaps one of the factors for the postoperative improvement in glycemic disorder in diabetic patients with pheochromocytoma.
The prior study had shown that patients with higher BMI were more likely to develop diabetes independent of pheochromocytoma. They might need continuous treatment for diabetes even after the resection of pheochromocytoma and removal of the effects of the elevated catecholamine because of the high BMI. Hence, BMI might be the predictive factor on the resolution or improvement of postoperative diabetes among pheochromocytoma patients.[10]
In our series, patients with symptomatic and larger tumors are less likely to resolve their diabetes. However, in the Beninato and Liu series, the resolution of diabetes concerned patients with larger tumors and higher preoperative catecholamine levels, but not statistically.[8,10]
CONCLUSIONS
Pheochromocytoma has a very close relationship with disorders of glucoregulation as demonstrated in this study. Large symptomatic tumors and elevated BMI are associated with preoperative diabetes mellitus. Complete tumor resection results in complete resolution of the diabetic disease in a significant number of the patients, although those patients with high BMI may continue use of diabetic medication postoperatively.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pacak K, Henri J, Timmers LM, Eisenhofer G. Pheochromocytoma. Endocrinol Adult Pediatr. 2016;10:1902–30. [Google Scholar]
- 2.Clutter WE, Cryer PE. Plasma dose-response studies with noradrenaline and adrenaline in man. Prog Biochem Pharmacol. 1980;17:84–9. [PubMed] [Google Scholar]
- 3.Wiesner TD, Blüher M, Windgassen M, Paschke R. Improvement of insulin sensitivity after adrenalectomy in patients with pheochromocytoma. J Clin Endocrinol Metab. 2003;88:3632–6. doi: 10.1210/jc.2003-030000. [DOI] [PubMed] [Google Scholar]
- 4.La Batide-Alanore A, Chatellier G, Plouin PF. Diabetes as a marker of pheochromocytoma in hypertensive patients. J Hypertens. 2003;21:1703–7. doi: 10.1097/00004872-200309000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Chen Y, Hodin RA, Pandolfi C, Ruan DT, McKenzie TJ. Hypoglycemia after resection of pheochromocytoma. Surgery. 2014;156:1404–8. doi: 10.1016/j.surg.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization & International Diabetes Federation. Geneva: World Health Organization; 2006. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation. [Google Scholar]
- 7.Pogorzelski R, Toutounchi S, Krajewska E, Fiszer P, Łykowski M, Zapała Ł, et al. The effect of surgical treatment of phaeochromocytoma on concomitant arterial hypertension and diabetes mellitus in a single-centre retrospective study. Cent European J Urol. 2014;67:361–5. doi: 10.5173/ceju.2014.04.art9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beninato T, Kluijfhout WP, Drake FT, Lim J. Resection of pheochromocytoma improves diabetes mellitus in the majority of patients. Ann Surg Oncol. 2017;24:1208–13. doi: 10.1245/s10434-016-5701-6. [DOI] [PubMed] [Google Scholar]
- 9.Stenström G, Sjöström L, Smith U. Diabetes mellitus in phaeochromocytoma.Fasting blood glucose levels before and after surgery in 60 patients with phaeochromocytoma. Acta Endocrinol (Copenh) 1984;106:511–5. doi: 10.1530/acta.0.1060511. [DOI] [PubMed] [Google Scholar]
- 10.Liu ZH, Zhou L, Lin LD, Chen T, Jiang QY, Liu ZH, et al. Will the resection of pheochromocytoma improve preoperative diabetes mellitus? Asian J Surg. 2019;42:990–4. doi: 10.1016/j.asjsur.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Sahli N, Antit M, Rojbi I, Mokaddem M. Clinical aspect and post-surgical evolution of carbohydrate metabolism in pheochromocytoma. Ann Endocrinol. 2014;75:398–9. [Google Scholar]


