Abstract
Background
This year, pollen season coincided with the first wave of the coronavirus disease 2019 pandemic. Strict preventive measures have been implemented during April and May and then a normalization phase started in our country in June. Our aim is to evaluate the effect of preventive measures during the pandemic process on allergic airway disease symptoms.
Methods
A prospective questionnaire-based study was planned and a questionnaire form was sent to the cell-phones of the subjects with pollen allergy followed in our clinic. Number of airborne grass pollens was determined by Burkard volumetric 7-day spore trap.
Results
A total of 222 pollen allergic patients were included in the study. At the beginning of the pandemic, majority of the subjects were spending time mostly indoors. The rate of home-office workers gradually decreased and the rate of office workers and the number of days at work increased from April to June, significantly. Nasal and ocular symptoms of the patients, also increased in June compared to April and May and, approximately one-third of the patients had less symptoms when compared to the same period of the previous year. The rates of using a face mask and taking a shower on return home were high among the subjects during all season.
Conclusion
Our study showed that spending less time outside during the pollen season and wearing a mask outdoors reduces exposure to pollens and causes a reduction in symptoms. Thus, strict application of measures that cannot be applied in daily practice can make a significant contribution to the management of seasonal allergic rhinitis.
Keywords: Allergic rhinitis, Pollen season, COVID-19 outbreak, Preventive measures
INTRODUCTION
Coronavirus disease 2019 (COVID-19) caused by the new coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first broke out in Wuhan, China. The virus transmitted from person to person has spread rapidly all over the world [1]. The first COVID-19 incident in Turkey was detected on 11th March 2020. Following the announcement of the first case, some preventive measures have been implemented at the end of March 2020 across the country. Within the scope of the measures applied during the pandemic process, it became compulsory to wear a disposable facial mask before going out, many employees switched to home-working system, schools were closed and students continued their education at home. A curfew was imposed on individuals under 20 and over 65 constantly, and on certain days for those between the ages of 20 and 65. After April and May with quarantine, the Turkish government initiated the new normalization phase at the beginning of June 2020 [2,3].
Symptoms of seasonal allergic rhinitis due to grass pollen allergy occur in April, May, and June when grass pollen is high in the air in the northern hemisphere. In order to prevent allergic airway disease symptoms, pollen atopic patients are advised to wear a mask to reduce exposure to pollen as much as possible, and avoid going out and doing outdoor activities during periods of high pollen Concentration [4,5]. However, due to the social conditions, our daily routines, and negligence, the recommendations cannot be followed sufficiently and it is not possible to be protected from exposure to pollen allergens. Therefore, it is not known to what extent preventive measures are effective in pollen allergy [4,5,6].
This year, as in many countries, the pollen season coincided with the first wave of the pandemic in our country. Due to the measures taken, people mostly stayed inside, wore a mask when they got out during April and May. But with the start of the normalization process in June, they began spending more time outside. With the precautions taken during the pandemia period, indirectly, individuals allergic to pollen are expected to have less contact with the allergen [7]. Therefore we hypothesized that individuals with seasonal allergic rhinitis and/or asthma due to grass pollen would be less symptomatic in the 2020 pollen season.
The aim of our study is to evaluate the effect of lockdown and wearing masks during the pandemic process on allergic airway disease symptoms and to compare them with the previous pollen season.
MATERIALS AND METHODS
This study was planned as a prospective questionnare based study performed in accordance with the Declaration of Helsinki. The study protocol was approved by Ankara University Ethics Committee (code: i6-341-20). A 24-item multiple choice questionnaire was prepared in Google forms and sent to the cell-phones of the subjects who were followed up in our polyclinic with the diagnosis of seasonal allergic rhinitis ± asthma with grass pollen allergy. All of the subjects live in Ankara Province. This survey questioned the attitude of patients about spending time outside the home, going to work, wearing masks, and taking shower on return home. Presence of nasal and ocular symptoms between April and July 2020 was also evaluated by the use of survey. In addition, subjects were asked to compare this year’s symptoms of allergic rhinitis and asthma with the same period of last year.
Pollen counts
During the season, number of airborne grass pollen was determined by Burkard volumetric 7-day spore trap. Burkard volumetric spor trap is currently the most common method of sampling airborne pollens. Samples collected with this method are analyzed by using light microscopes. The trap was placed on the roof of the building at the campus of Ankara University at an altitude of 30 m above ground level. Atmospheric sampling and analysis were performed according to the method described by the Spanish Aerobiological Network (REA) [8]. The pollen counts were converted into daily average concentrations (grains/m3).
Statistics
Statistical analyzes were made using SPSS ver. 15 (SPSS Inc., Chicago, IL, USA). The normality of distribution was examined by visual (histogram and probability graphs) and analytical methods (Kolmogrov-Smirnov/Shapiro-Wilk tests). Frequency of distrubitions was analyzed and descriptive statistics were calculated using the mean and standard deviation for normally distributed variables, using the median and interquartile range for nonnormally distributed variables. Categorical data were evaluated by chi-square test. For p < 0.05 for all tests performed, the results were considered statistically significant.
RESULTS
A total of 222 grass pollen allergic patients (129 females, 93 males) were included in the study with the mean age of 35.04 ± 11.06 years. Thirty-three percent (n = 75) of them had asthma as well as allergic rhinitis. Sixty-six percent of the study group (n = 147) were employed. At the beginning of the study; among these 147 patients; 17.6% (n = 26) were on unpaid leave, 37.41% (n = 55) were working from home and 44.89% (n = 66) continued office working. Approximately half of the subjects who go to work (42.5%) stated that they went 5–7 times a week, 33.3% for 3–4 days, 20% for 1–2 days a week. One-third of the subjects said that they did not spend more than 3 hours outside, while the rates of using a face mask and taking a shower when they get home were as high as 83.3% and 60.8%, respectively.
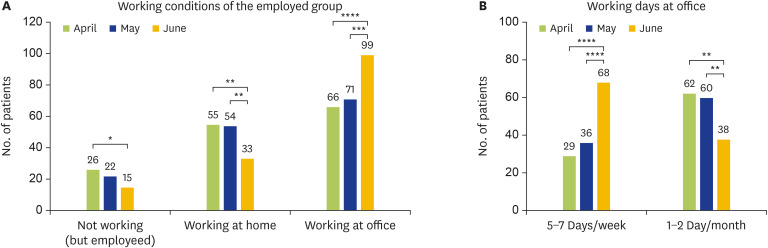
Among the employed patients from beginning of April to the end of June, it was observed that the rate of home-office workers gradually decreased and the rate of office workers increased significantly. Moreover, it is noteworthy that there was a significant increase in the number of days at work. (Fig. 1) In addition, it was observed that the number of people who said they very rarely went outside decreased both among the employed (n = 147) and the unemployed ones (n = 75) from April to June (Table 1). The time spent outdoors was higher among employed patients than unemployed subjects and increased gradually in both groups from April to June. For employed people proportion of the patients spending more than 3 hours outdoors by months (April, May, June) were 24%, 27%, and 49% and for unemployed group, the rates were 23%, 25%, 27%, respectively. In general, subjects in our study group spent 1–3 hours when they went outside during these three months (33.8%, 35.1%, 38.7%, respectively). But the percentage of the patients who spent more than 3 hours outdoors increased from April to June (18.5%, 21.7%, 39.4%, respectively). Monthly distribution of the rate of using face mask was 83.3%, 86%, 85% in April, May, and June respectively. Most of our subjects prefered to take a shower on their return home with 60.8%, 58.1%, 54.5%, respectively by months.
Fig. 1. (A) Working conditions of the employed subjects. While the number of patients on unpaid leave was lower in April compared to June (p < 0.05), the number of home workers was lower in June compared to April and May (p < 0.01). In contrast, the number of subjects working from the office in June was higher compared to April and May (p < 0.001, p = 0.000, respectively). (B) In terms of working days, the number of subjects working 5–7 days a week in June was more than in April and May (p = 0.000), and the number of subjects reporting that they rarely went to work was far less in June than in April and May (p < 0.01).
Table 1. Proportion of those who rarely go out.
| Month | Employed (n = 147) | Unemployed (n = 75) | Total (n = 222) |
|---|---|---|---|
| April | 46 (31) | 38 (50) | 84 (37.8) |
| May | 37 (25) | 27 (36) | 64 (28.8) |
| June | 19 (12) | 17 (22) | 36 (16.2) |
| p value | <0.001 | <0.001 | <0.001 |
Values are presented as number (%).
Patients were examined in terms of nasal and eye symptoms, and it was seen that their complaints increased in June compared to April and May (p = 0.000). There was no significant difference in nasal and eye symptoms between employed and unemployed groups. Furthermore, symptoms did not differ between the subjects on unpaid leave, home-office workers, and office workers. In addition, there was no difference in symptoms in terms of using face mask. However, patients on unpaid leave and unemployed subjects who stated that they very rarely went outside had less nasal itching (p = 0.009) in April and less nasal obstruction in April (p = 0.007), and May (p = 0.006) compared to those who spent more time outside.
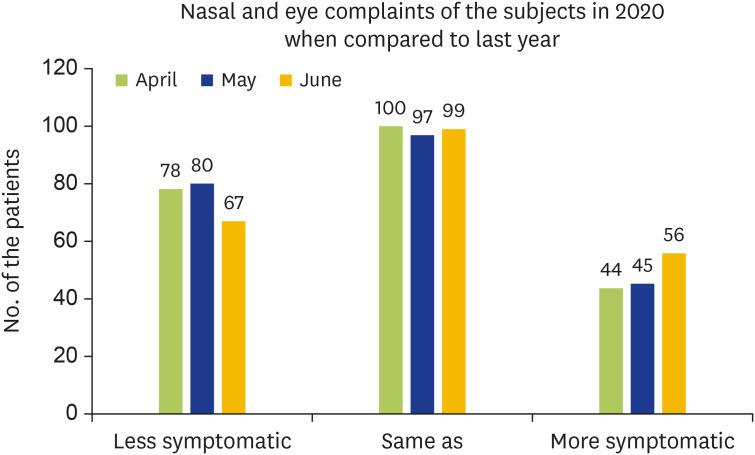
When nasal and eye symptoms of the patients were compared with the same period of the previous year; 35.1% (n = 78) of the patients stated that their symptoms were less, while 45% (n = 100) said they were the same in April; 36% (n = 80) of the individuals reported less, 43.7% (n = 97) had similar symptoms this year in May. The rate of those who said their symptoms were less than previous year was 30% (n = 67) and more than last year was 25.2% (n = 56) in June (Fig. 2). While there was no difference in asthma symptoms in April, May, and June in patients with asthma, nearly half of the group stated that their complaints were same as the previous year.
Fig. 2. The subjects' nose and eye complaints. The number of less symptomatic subjects compared to the previous year was higher in April and May than in June, individuals who declared to be the same as the previous year were evenly distributed for each three months and the number of patients reporting more symptomatic this year was less in April and May.
The patients describing symptoms less than, same as or more than the previous year were compared according to being outdoors or indoors. During April and May 2020, the proportion of active work days in all groups was seen to decrease significantly. However, compared to last year, it was observed that the rate of going to work decreased more in those who stated that they were less symptomatic this year than those with complaints the same or more than last year (Table 2).
Table 2. Comparison of the nasal and eye symptoms of the subjects between 2020 and 2019.
| Variable | Less symptomatic than previous year | Same as previous year | More symptomic than previous year | ||
|---|---|---|---|---|---|
| April | |||||
| Total | 78 | 100 | 44 | ||
| Active working* | |||||
| 2019 | 56 (71.8) | 55 (55) | 32 (72.7) | ||
| 2020 | 23 (29.5) | 21 (21) | 17 (38.6) | ||
| p value | 0.000 | 0.000 | 0.001 | ||
| May | |||||
| Total | 80 | 97 | 45 | ||
| Active working* | |||||
| 2019 | 54 (67.5) | 57 (58.8) | 32 (71.1) | ||
| 2020 | 22 (27.5) | 24 (24.7) | 18 (40) | ||
| p value | 0.000 | 0.000 | 0.003 | ||
*Working at 5-7 days/week.
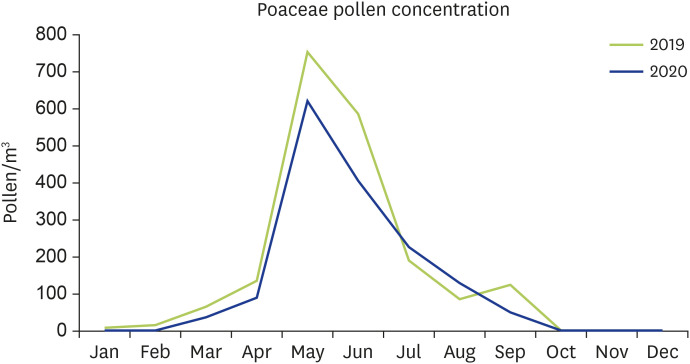
Grass pollen measurement results were evaluated as monthly averages, and it was seen that the pollen level was lower this year in every 3 months compared to the previous year (Fig. 3).
Fig. 3. Monthly airborne poaceae pollen concentration in 2020 and 2019.
DISCUSSION
Our study showed that, patients with pollen allergy were less symptomatic when they spent less time outdoors during the pollen season. The treatment of seasonal allergic rhinitis include avoidance of pollen exposure and prescription of allergy medications [9,10]. Most physicians are well informed of the pharmacologic treatment, whereas advising about avoidance of pollen exposure may be challenging because of lack of compliance with the measures during pollen season [4,6]. Since the pollen season coincided with the COVID-19 outbreak this year, recommendations, such as wearing a face mask when going out, taking a shower on return home, and spending less time outdoors during the peak pollen periods have been spontaneously implemented [11]. Accordingly, with the strict quarantine measures, people mostly stayed at home, especially in April and May 2020 [12]. This study revealed that the number of days worked in the office decreased among the employed subjects, but with the start of the normalization period in June, the proportion of working days and the time spent outdoors increased. In line with this finding, subjects were less symptomatic in May 2020 when the grass pollen peak was seen than in June 2020. This data shows us that, spending less time outside during the pollen season is an effective preventive measure.
Patients with pollen allergy are adviced to spend less time outdoors, wear a face mask when going out, and take a shower when they return home in the spring [4,6,9,13,14]. There are very few studies evaluating the clinical effectiveness of preventive measures in the literature. One of them is about the use of face mask in nurses during COVID-19 pandemic which revealed that face mask may reduce allergic rhinitis symptom severity in chronically affected individuals with intermittent allergic rhinitis. The study supports the hypothesis that face masks may reduce the symptoms of allergic rhinitis [15]. Another study investigated the efficacy of wearing eyeglasses showed that it was effective in controlling symptoms, improving the quality of life, and reducing the need for medicine in patients with seasonal allerjic rhinitis [16]. In our study, we evaluated the protective effect of spending less time outdoors, wearing a face mask, and taking a shower on return home in patients with seasonal allergic rhinitis and asthma. The rate of wearing a face mask outdoors and taking a shower was quite low last year; but with the strict precautions taken this year, it was seen that almost all of the patients wore a face mask, and half of them said that they were taking a shower on return home this year. Furthermore, people spent less time outdoors during 2020 pollen season. About three-quarters of the subjects stated that, they had less or almost similar rate of symptoms this year compared to previous year. Taken together, patients with pollen allergy were less symptomatic this year, pointing to the importance of the prevention measures. Almost two-thirds of the participants of this study were employed and the rate of active working subjects decreased significantly during the pandemic compared to 2019. However, there have been some variations in terms of active working during COVID-19 outbreak. Thus, the proportion of active workers have been increased with the normalization phase in June 2020. This study revealed that the group who described lesser symptoms than the previous year were the ones who had much greater reduction in the percentage of active working days compared with individuals who reported the same or worse symptoms this year. Moreover, subjects who reported being less symptomatic this year had a much greater reduction in the percentage of actively working days during the period with strict rules compared to the normalization phase. These findings once again showed that staying at home for whatever the reason was, reduces the exposure to pollens and leads to lesser symptoms even in the pollen peak period.
There are some limitations of the study. First of all, this was a questionnaire study based on subjective measures. If symptom and medication scores were used, the evaluation could be more objective. However, the study population included the registered patients in the outpatient clinic and they are frequently asked for self-evaluation of their symptoms. Because of that, they could express the difference in symptoms very precisely for each month during the pollen season. Secondly, although the answers given to the questions about the 3 months of this year are considered to be reliable, the comparison made with the same period of last year was based on memory and reasoning abilities of the people and was inevitably subjective.
On the other hand, it is the first study in the literature that comprehensively evaluates the effectiveness of preventive measures in patients with pollen allergy. Although the patients are advised to adhere to preventive measures, it is not possible to monitor whether they are implementing them effectively in the real life. In this context, restrictions imposed during the pollen season due to the pandemic provided us this opportunity this year.
In conclusion, COVID-19 outbreak in concomitance with pollen season this year showed us that spending less time outside during the pollen season and wearing a mask outdoors reduces exposure to pollens and causes a reduction in symptoms. From a practical and clinical viewpoint, our data suggest that, if precautions are strictly followed, symptoms of seasonal allergic rhinitis may be improved.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Zeynep Çelebi Sözener, Dilşad Mungan.
- Formal analysis: Zeynep Çelebi Sözener.
- Investigation: Zeynep Çelebi Sözener, Betül Özdel Öztürk.
- Methodology: Zeynep Çelebi Sözener, Betül Özdel Öztürk, Nur Münevver Pınar.
- Project administration: Zeynep Çelebi Sözener, Betül Özdel Öztürk, Dilşad Mungan.
- Writing - original draft: Zeynep Çelebi Sözener, Betül Özdel Öztürk, Dilşad Mungan.
- Writing - review & editing: Zeynep Çelebi Sözener, Betül Özdel Öztürk, Ömür Aydın, Yavuz Selim Demirel, Nur Münevver Pınar, Sevim Bavbek, Betül Ayşe Sin, Dilşad Mungan.
References
- 1.World Health Organization. Novel coronavirus (2019-nCoV) situation reports [Internet] Geneva (Switzerland): World Health Organization; [cited 2021 Jan 2]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situationreports. [Google Scholar]
- 2.Demirbilek Y, Pehlivantürk G, Özgüler ZÖ, Alp Meşe E. COVID-19 outbreak control, example of ministry of health of turkey. Turkish J Med Sci. 2020;50 SI-1(SI-1):489–494. doi: 10.3906/sag-2004-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Güner R, Hasanoğlu İ, Aktaş F. Covid-19: Prevention and control measures in community. Turkish J Med Sci. 2020;50:571–577. doi: 10.3906/sag-2004-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wise SK, Lin SY, Toskala E, Orlandi RR, Akdis CA, Alt JA, Azar A, Baroody FM, Bachert C, Canonica GW, Chacko T, Cingi C, Ciprandi G, Corey J, Cox LS, Creticos PS, Custovic A, Damask C, DeConde A, DelGaudio JM, Ebert CS, Eloy JA, Flanagan CE, Fokkens WJ, Franzese C, Gosepath J, Halderman A, Hamilton RG, Hoffman HJ, Hohlfeld JM, Houser SM, Hwang PH, Incorvaia C, Jarvis D, Khalid AN, Kilpeläinen M, Kingdom TT, Krouse H, Larenas-Linnemann D, Laury AM, Lee SE, Levy JM, Luong AU, Marple BF, McCoul ED, McMains KC, Melén E, Mims JW, Moscato G, Mullol J, Nelson HS, Patadia M, Pawankar R, Pfaar O, Platt MP, Reisacher W, Rondón C, Rudmik L, Ryan M, Sastre J, Schlosser RJ, Settipane RA, Sharma HP, Sheikh A, Smith TL, Tantilipikorn P, Tversky JR, Veling MC, Wang Y, Westman M, Wickman M, Zacharek M. International Consensus Statement on Allergy and Rhinology: allergic rhinitis. Int Forum Allergy Rhinol. 2018;8:108–352. doi: 10.1002/alr.22073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Global Initiative for Asthma. Global strategy for asthma management and prevention - updated 2020 [Internet] The Global Initiative for Asthma; [cited 2020 Jun 4]. Available from: https://ginasthma.org/wp-content/uploads/2020/06/GINA-2020-report_20_06_04-1-wms.pdf. [Google Scholar]
- 6.Adkinson NF, Bochner BS, Burks AW, Busse WW, Holgate ST, Lemanske RF, O'Hehir RE. Middleton's allergy: principles and practice. 8th ed. Philadelphia (PA): Elsevier Inc.; 2013. [Google Scholar]
- 7.Gallo O, Bruno C, Locatello LG. Global lockdown, pollution, and respiratory allergic diseases: Are we in or are we out? J Allergy Clin Immunol. 2020;146:542–544. doi: 10.1016/j.jaci.2020.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galán C, Cariñanos P, Alcázar P, Domínguez E. Spanish Aerobiology Network (REA): Management and quality manual. Córdoba: Servicio de publicaciones de la Universidad de Co´rdoba; 2007. [Google Scholar]
- 9.Kalyoncu AF. A new approach to an old problem: controversial issues in seasonal rhinoconjunctivitis. J Allergy Ther. 2014;5:164–166. [Google Scholar]
- 10.Das RR. Treatment of allergic rhinitis in children: what's new? J Paediatr Child Health. 2012;48:366. doi: 10.1111/j.1440-1754.2012.02462.x. [DOI] [PubMed] [Google Scholar]
- 11.Nicola M, O'Neill N, Sohrabi C, Khan M, Agha M, Agha R. Evidence based management guideline for the COVID-19 pandemic - review article. Int J Surg. 2020;77:206–216. doi: 10.1016/j.ijsu.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gostin LO, Wiley LF. Governmental public health powers during the COVID-19 pandemic: Stay-at-home orders, business closures, and travel restrictions. JAMA. 2020;323:2137–2138. doi: 10.1001/jama.2020.5460. [DOI] [PubMed] [Google Scholar]
- 13.Xiao SF, Okuda M, Tanimoto H. Inhibitory effect of half-face masks on ınhalation of particles of carbon powder and Japanese Cedar Pollen. Am J Rhinol. 2007;5:57–60. [Google Scholar]
- 14.Gotoh M, Okubo K, Okuda M. Inhibitory effects of facemasks and eyeglasses on invasion of pollen particles in the nose and eye: a clinical study. Rhinology. 2005;43:266–270. [PubMed] [Google Scholar]
- 15.Dror AA, Eisenbach N, Marshak T, Layous E, Zigron A, Shivatzki S, Morozov NG, Taiber S, Alon EE, Ronen O, Zusman E, Srouji S, Sela E. Reduction of allergic rhinitis symptoms with face mask usage during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8:3590–3593. doi: 10.1016/j.jaip.2020.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Comert S, Karakaya G, Kalyoncu AF. Wraparound eyeglasses improve symptoms and quality of life in patients with seasonal allergic rhinoconjunctivitis. Int Forum Allergy Rhinol. 2016;6:722–730. doi: 10.1002/alr.21737. [DOI] [PubMed] [Google Scholar]