Abbreviations
- COVID‐19
coronavirus disease 2019
- AHRF
acute hypoxemic respiratory failure
- ICU
intensive care unit
- HFNC
high‐flow nasal cannula
- FiO2
fraction of inspired oxygen
- SpO2
peripheral oxygen saturation
- IMV
invasive mechanical ventilation
1. INTRODUCTION
During the coronavirus disease 2019 (COVID‐19) pandemic, oxygen support management for critically ill patients with acute hypoxemic respiratory failure (AHRF) was a key component of clinical decision‐making. 1 There is a lack of knowledge regarding the use of high‐flow nasal cannula (HFNC) in COVID‐19 patients with AHRF. Most hospitals adopted an early‐intubation strategy leading to a high intubation rate and the demand for intensive care unit (ICU)‐beds overwhelmed hospital resources. With a low ICU bed‐to‐population ratio in our area, we adopted a large high‐flow nasal cannula (HFNC) therapy use in COVID‐19 patient‐related AHRF. Here, we assessed, retrospectively, the benefit of HFNC use in this population.
2. METHODS
Forty‐two COVID‐19‐confirmed patients with AHRF treated with at least 2 hours of HFNC in first line were included in the study between March 1 and May 23, 2020 (Figure 1). The study was declared at European General Data Protection Regulation (Identifier RMR004‐25052020). Inclusion criteria were laboratory‐confirmed COVID‐19 patients over 18 years of age suffering from AHRF treated with HFNC as first‐line therapy and admitted to the medical ICU of the Reims University Hospital. Exclusion criteria were under 18 years of age, urgent need to intubate (less than 2 hours after HFNC initiation), previous intubation in the same hospital stay, and presence of a do‐not‐resuscitate order.
FIGURE 1.
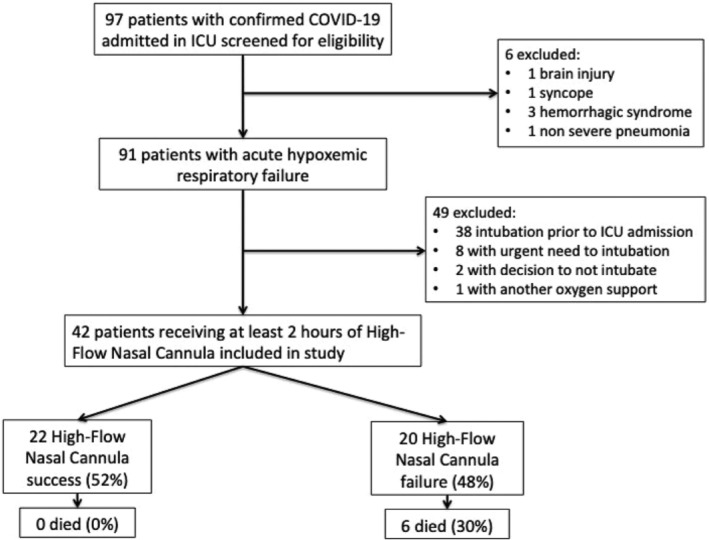
Flow chart
HFNC was initiated with a minimum flow of 50 L/min with a FiO2 of 50%. Then, FiO2 was titrated targeting an SpO2 above 92%, and flow rate was adjusted up to 60 L/min or according to the maximum tolerated dose. HFNC failure was defined as the subsequent need for invasive mechanical ventilation. Intubation criteria were left at the discretion of physicians. Respiratory parameters were measured under HFNC conditions. The ROX index was defined as the ratio of SpO2/FiO2(%) to respiratory rate (breaths/min). In patients with AHRF treated with HFNC, a ROX index higher than 4.88 measured after 12 hours of HFNC was significantly associated with a lower risk of intubation. 2 , 3
Quantitative parameters were analyzed with nonparametric tests. Differences in categorical variables were assessed with chi‐square. All tests were two‐sided with a 5% significance level.
3. RESULTS
Results are displayed in Table 1. Twenty‐two patients were treated successfully with HFNC (52%) and twenty patients subsequently required IMV support (48%).
TABLE 1.
Patient characteristics on ICU admission, clinical course, and outcomes
| Characteristics | All patients (N = 42) | HFNC success (n = 22) | HFNC failure (n = 20) | P value a |
|---|---|---|---|---|
| Baseline | ||||
| Age, median [IQR], years | 67 [59‐72.5] | 65 [54‐70] | 69 [64‐75] | 0.03 |
| Male, sex, n (%) | 28 (66) | 15 (68) | 13 (65) | 1 |
| Obesity, BMI≥30 kg/m2, n (%) | 16 (38) | 9 (41) | 7 (35) | 0.76 |
| Sequential organ failure assessment, median [IQR] | 3.5 [3‐5] | 3 [3–4] | 4 [3‐6] | 0.02 |
| White blood cell counts, median [IQR], ×10^9/L | 8.0 [6.8‐9.3] | 9.0 [7.6‐10.7] | 6.9 [6.1‐7.8] | 0.01 |
| Platelet counts, median [IQR], ×10^9/L | 256 [205‐318] | 313 [246‐398] | 199 [163‐238] | 0.002 |
| Chest computed tomography b Percentage of lung damage, median [IQR] (%) |
52.5 [50‐63.75] |
55 [50‐60] |
50.0 [50.0‐67.5] |
0.51 |
| Respiratory measures of patients at ICU admission, median [IQR] | ||||
| Respiratory rate, per min | 24 [19.5‐28.5] | 23 [18‐27] | 25 [21‐30] | 0.09 |
| Ratio PaO2/FiO2 | 125.5 [96‐161] | 128 [100‐176] | 121.5 [88.5135.5] | 0.16 |
| FiO2 HFNC, % | 66 [59‐80] | 65 [60‐80] | 67.5 [57.5‐80] | 0.60 |
| Flow HFNC, L/min | 57.5 [59–80] | 60 [50‐60] | 55 [50‐60] | 0.80 |
| Respiratory measures of patients at Nadir, median [IQR] | ||||
| Respiratory rate, per min | 32 [28‐37] | 31 [28‐35]] | 33.5 [28‐39] | 0.53 |
| Ratio PaO2/FiO2 | 99.5 [78.5‐112] | 110 [87.5‐127.5] | 89 [69.5‐96] | 0.01 |
| FiO2, (%) | 86 [80‐100] | 72.5 [60‐100] | 100 [100‐100] | 0.003 |
| Flow HFNC, L/min | 60 [60‐60] | 60 [60‐60] | 60 [60‐60] | 1 |
| Prediction of HFNC success by ROX index c | ||||
| ROX index at H2, median [IQR] d | 6,23 [5,13‐7,63] | 6,33 [4,98‐8,30] | 6,12 [5,29‐6,91] | 0,64 |
| ROX index at H6, median [IQR] | 6,78 [4,89‐8,56] | 7,03 [5,20‐9,37] | 6,52 [4,57‐7,75] | 0,18 |
| ROX index at H12, median [IQR] | 6.19 [5.20‐7.89] | 6.82 [5.80‐9.12] | 5.56 [4.60‐6.67] | 0.04 |
| ROX index >4.88 at H12, n (%) e | 28 (78) | 20 (91) | 8 (57) | 0.04 |
| ICU clinical course | ||||
| Time from ICU admission to intubation, median [IQR] hours | ‐ | ‐ | 24 [10–49] | ‐ |
| Use of vasopressors f | 20 (48) | 0 (0) | 20 (100) | 0.0003 |
| Acute kidney injury g | 17 (40) | 4 (18) | 13 (65) | 0.004 |
| Acute liver injury h | 7 (17) | 1 (4) | 6 (30) | 0.04 |
| Ventilator‐associated pneumonia i | ‐ | ‐ | 7 (35) | ‐ |
| Outcomes | ||||
| Median length of stay in ICU survivors, median [IQR] days | 8 [5‐19] | 7 [4‐8] | 23 [18‐42] | 0.0001 |
| Died at day 28, n (%) | 6 (13) | 0 (0) | 6 (30) | 0.007 |
| Discharged from hospital at day 28, n (%) | 17 (40) | 16 (73) | 1 (0.5) | 0.00001 |
Abbreviations: BMI, body mass index; FiO2, fraction of inspired oxygen; ICU, intensive care unit; IQR, interquartile; HFNC, high‐flow nasal cannula; PaO2, partial pressure of oxygen.
Nonparametric tests or Fischer exact test comparing HFNC success vs HFNC failure, as appropriate.
Data available for 29/42 patients.
The ROX index was defined as the ratio of SpO2/FIO2(%) to RR (breaths/min). The ROX index is an early marker to predicting the success or failure of HFNC.
Measures performed on 39 patients.
Measures performed on 36 patients.
Use of vasopressors defined as norepinephrine intravenous administration (more than 0.2 μg/kg/min).
Acute kidney injury stages 2 and 3 according to the 2012 Kidney Disease: Improving Global Outcomes (KDIGO).
Defined as alanine aminotransferase or aspartate aminotransferase level greater than three times the upper limit of normal.
Definition according to IDSA/ATS criteria.
At ICU admission, patients had a median PaO2/FiO2 ratio of 128 [100‐176] for HFNC success group and 121.5 [88.5‐135.5] for HFNC failure group (P = .16). Other respiratory parameters studied were not different at admission.
At nadir, PaO2/FiO2 ratio was lower in HFNC failure group 89 [69.5‐96] than in the HFNC success group 110 [87.5‐127.5] (P = .010). HFNC success patients were younger, had a lower SOFA score, less fever, thrombopenia or leukopenia, and a higher ROX index at H12.
No deaths were reported in the HFNC success group with a shorter median ICU stay (7 days [4‐8] vs 23 days [18‐42], P = .0015) and a greater percentage of hospital discharge at day 28, 16 (73%) vs 1 (0.5%; P = .00001) than the HFNC failure group.
In the failure group, the time from ICU admission to intubation was 24 hours [10‐49] and duration of mechanical ventilation was 19.5 days [11.3‐27.8]. In this group, patients experienced significantly more organ dysfunctions (use of vasopressors, kidney, and liver failures) with a 28‐day mortality rate of 30%.
4. DISCUSSION
The main finding of our study is the high rate of HFNC success (52%) in a significant cohort of COVID‐19 patients with severe AHRF. These results contrast with the low success rate reported by first published series such as the study of Wang et al. 4 However, they did not use HFNC as first‐line therapy, which suggests that it was used for selected patients and could therefore explain the differences of outcomes reported. Indeed, recent large cohorts of patients treated with HFNC as first‐line therapy corroborated our results with a rate of success ranging from 44 to 62%. 5 , 6 , 8
Previous studies have reported that delayed intubation could be associated with a worse outcome in de novo AHRF patients. Here, we did not report an excess mortality in the HFNC failure group (30%), compared to patients requiring early intubation in other cohorts. 7 Similarly, Demoule et al. confirmed that HFNC was safe and could significantly reduce the intubation rate in a large cohort of 146 COVID‐19 patients. 8 The first use of noninvasive ventilation has been recently reinforced by Dupuis et al which showed an increased risk of mortality at day‐60 for an early mechanical ventilation strategy. 9
Zucman et al. suggest that ROX index could help for predicting HFNC outcome in this specific population from the very first hours. 10 Here, only the ROX index at H12 was associated with HFNC success. An explanation could be a different management of oxygen support in these patients with easier criteria for intubation use. Moreover, in our study, the first FIO2 reported under HFNC condition was lower than in the Zucman's study. This could suggest that patients should be selected as early as possible to benefit from HFNC which could explain their failure rate of 63% of HFNC. We also reported a higher ROX index at H2 and H6 than previous studies in cohorts of non‐COVID‐19 patients. 3 This is potentially due to the contrast between the absence of dyspnea and the hypoxemia in some COVID‐19 patients, that authors called “happy hypoxemia.” 11 , 12
Thus, we think that the ROX index could be used early but with higher thresholds, notably in patients with a normal respiratory rate but a severe hypoxemia. Larger studies will be necessary to determine the best cut‐off value in this specific population.
Finally, we identified a clinical and biological phenotype of patients with HFNC success. They are younger, have a lower SOFA score, less fever, thrombopenia or leukopenia, and a higher ROX index at H12.
Our study was monocentric with a small sample size, and our results may not be generalizable to all ICUs. Despite these limitations, our experience points out to the potential benefits of HFNC as first‐line treatment for COVID‐19 patients with AHRF and identifies a successful patient profile.
5. CONCLUSION
In this study, we demonstrate that HFNC is effective to treat COVID‐19 patients with moderate to severe AHRF and identify predictive factors of HFNC success, including the ROX index at H12. According to results from recent studies, we think that HFNC should be used to as early as possible at ICU admission. Randomized studies will be necessary to define the best place of HFNC in the COVID‐19 oxygen management support.
CONFLICT OF INTEREST
The authors declare there is no conflict of interest.
AUTHOR CONTRIBUTIONS
Concept and design: Antoine Goury, Jean‐Adoumngar Moussanang, Bruno Mourvillier
Acquisition, analysis, or interpretation of data: All authors
Drafting of the manuscript: Antoine Goury, Jean‐Adoumngar Moussanang, Bruno Mourvillier
Critical revision of the manuscript for important intellectual content: All authors
Statistical analysis: Antoine Goury
Administrative, technical, or material support: Bruno Mourvillier
Supervision: Bruno Mourvillier
All authors have read and approved the final version of the manuscript.
Dr GOURY had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was declared at European General Data Protection Regulation (GRPD) (Identifier RMR004‐25052020). Patients and their relatives were informed of the use of medical data and did not manifest opposition.
ACKNOWLEDGMENTS
The authors would like to formally acknowledge our medical staff for their help in collecting of the database. We thank Dr Sylvie Touche, Sandrine Marchet, Anne Rousseaux and Sebastien Gayet for their help in collecting COVID‐19 confirmed cases in healthcare workers. We thank Grace Stockton Bliard for her precious writing assistance. We thank Jennifer Lepage for her legal assistance. None of these individuals received compensation for their contributions. Dr Goury affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Goury A, Moussanang J‐A, Bard M, et al. Predictive factors associated with high‐flow nasal cannula success for COVID‐19‐related acute hypoxemic respiratory failure. Health Sci Rep. 2021;4:e287. 10.1002/hsr2.287
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- 1. Ramachandran P, Swamy L, et al. A national strategy for ventilator and ICU resource allocation during the COVID‐19 pandemic. Chest. 2020;158(3):887‐889. 10.1016/j.chest.2020.04.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high‐flow therapy. Am J RespirCrit Care Med. 2019;199:1368‐1376. 10.1164/rccm.201803-0589OC. [DOI] [PubMed] [Google Scholar]
- 3. Ricard JD, Roca O, Lemiale V, et al. Use of nasal high flow oxygen during acute respiratory failure. Intensive Care Med. 2020;46:2238‐2247. 10.1007/s00134-020-06228-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang Y, Lu X, Li Y, et al. Clinical course and outcomes of 344 intensive care patients with COVID‐19. Am J Respir Crit Care Med. 2020;201(11):1430‐1434. 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chandel A, King CS, et al. High‐flow nasal cannula in COVID‐19: outcomes of application and examination of the ROX index to predict success. Resp Care. 2020;08631. 10.4187/respcare.08631. [DOI] [PubMed] [Google Scholar]
- 6. Hu, Zhou Q, Zheng R, et al. Application of high‐flow nasal cannula in hypoxemic patients with COVID‐19: a retrospective cohort study. BMC Pulm Med 20. 2020;324. 10.1186/s12890-020-01354-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Auld SC, Caridi‐Scheible M, Blum JM, et al. ICU and ventilator mortality among critically ill adults with coronavirus disease 2019. Crit Care Med. 2020;48(9):e799‐e804. 10.1097/CCM.0000000000004457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Demoule A, Vieillard Baron A, Darmon M, Azoulay E, et al. High flow nasal Canula in critically ill severe COVID‐19 patients. Am J Respir Crit Care Med. 2020;202(7):1039‐1042. 10.1164/rccm.202005-2007LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dupuis C, Bouadma L, Timsit JF, et al. Association between early invasive mechanical ventilation and Day‐60 mortality in acute hypoxemic respiratory failure related to coronavirus Disease‐2019 pneumonia. Crit Care Explor. 2021;3(1):e0329. 10.1097/cce.0000000000000329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zucman N, Mullaert J, Roux D, Roca O, Ricard J‐D. Prediction of outcome of nasal high flow use during COVID‐19‐related acute hypoxemic respiratory failure. Intensive Care Med. 2020;46:1924‐1926. 10.1007/s00134-020-06177-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gattinoni L, Chiumello D, Caironi P, et al. COVID‐19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46(6):1099‐1102. 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Herrmann J, Mori V, Bates JHT, Suki B. Modeling lung perfusion abnormalities to explain early COVID‐19 hypoxemia. Nat Commun. 2020;11:4883. 10.1038/s41467-020-18672-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


