As stated at the start of the anti-SARS-CoV-2 vaccination campaign, all patients followed in oncology must be able to benefit from an anti-COVID vaccination as a priority, regardless of the nature of their neoplasia [1], [2]. Taking into account the regular follow-up of patients treated for cancer in the active phase of treatment with positron emission CT scan with F-FDG (PET/FDG), we report the case of a locoregional inflammatory reaction to be known by clinicians.
A 76-year-old female patient undergoing treatment for a recurrent ovarian neoplasia previously treated for 4 cycles of CARBOPLATINE GEMCITABINE and BEVACIZUMAB underwent a PET/FDG in early February 2021 for reassessment. While imaging demonstrated a complete metabolic response to the peritoneal targets initially present, hypermetabolism was noted in the right deltoid muscle with a standardized uptake value (SUV) of 4.3 associated with a hypermetabolic lymphadenopathy with SUV of 7.1 (figure 1 ). The patient had actually been vaccinated with a second dose of COMIRNATY® (Pfizer/BioNTech) five days previously. On examination, inflammatory edema in the deltoid was noted, mildly painful with no rash, associated with a 2 cm painless lymphadenopathy in the axillary. The patient did not report any fever for the days following the vaccination and the clinical examination normalized a few days later.
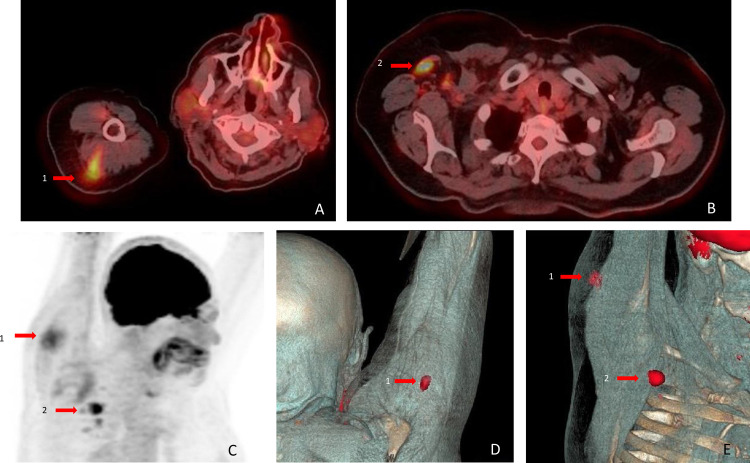
Figure 1.
PET/FDG imaging after SARS-CoV-2 vaccination
A–B: axial PET/CT fusion; C: Coronal CT scan; D–E: volume rendering PET/CT fusion. 1: right deltoid muscle hypermetabolism (SUV 4.3). 2: right axillary lymphadenopathy hypermetabolism (SUV 7.1).
Vaccination is known to cause transient inflammation of lymph nodes inducing positive findings on F-FDG PET scans with for instance with flu vaccine [3] or human papillomavirus vaccines [4]. Considering the high immunogenicity of anti-SARS-CoV-2 vaccines, clinicians should be aware of local benign and transient side effects in order to avoid invasive diagnostic procedures. We must inform patients of the possibility of an inflammatory lymph node reaction following the anti-COVID vaccination and clinicians need to reassure them that there is no risk of cancer stimulation, especially women undergoing follow-up for breast cancer.
Finally, we consider that SARS-CoV-2 vaccination should be avoided on the side of a recently treated breast tumor to avoid the risk of lymphedema. In case of an evolutive loco-regional breast cancer, PET/FDG could lead to the wrong conclusion of tumor progression.
Disclosure of interest
the authors declare that they have no competing interest.
References
- 1.Spano J.P., Barre-Sinoussi F., Kieny M.P., Marcelin A.G., Blay J.Y. [COVID-19 vaccination for cancer patients: Medical and ethical need] Bull Cancer. 2021;108(3):225–227. doi: 10.1016/j.bulcan.2021.02.001. [French. Epub 2021 Feb 16. PMID: 33674059; PMCID: PMC7885674] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barrière J., Audigier-Valette C., Borchiellini D., Hoch B., Castelnau O., Francois E. [We must respect the anti-SARS-CoV-2 vaccine schedule without delay in cancer patients under treatment] Bull Cancer. 2021;108(4):341–342. doi: 10.1016/j.bulcan.2021.02.003. [French. Epub 2021 Mar 5. PMID: 33741139; PMCID: PMC7934697] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burger I.A., Husmann L., Hany T.F., Schmid D.T., Schaefer N.G. Incidence and intensity of F-18 FDG uptake after vaccination with H1N1 vaccine. Clin Nucl Med. 2011;36(10):848–853. doi: 10.1097/RLU.0b013e3182177322. [PMID: 21892032] [DOI] [PubMed] [Google Scholar]
- 4.Coates E.E., Costner P.J., Nason M.C., Herrin D.M., Conant S., Herscovitch P. Lymph node activation by PET/CT Following Vaccination With Licensed Vaccines for Human Papillomaviruses. Clin Nucl Med. 2017;42(5):329–334. doi: 10.1097/RLU.0000000000001603. [PMID: 28288041] [DOI] [PubMed] [Google Scholar]