Abstract
We report a case of severe amnestic syndrome following theophylline overdose. A woman in her early 30s was admitted to hospital where she developed status epilepticus following an intentional overdose of theophylline and lansoprazole. She developed a profound acidosis and required intubation in the intensive care unit. Following extubation the patient was noted to have a severe amnestic syndrome with poor short-term memory. A work-up to exclude infectious, autoimmune and paraneoplastic causes for encephalitis was undertaken. Cerebrospinal fluid analysis was normal and autoimmune encephalitis titres were negative. Initial MRI brain imaging demonstrated hyperintensities of the mesial temporal lobes bilaterally. Follow-up imaging at 4 months identified further interval reduction but persistent hippocampal hyperintensities. Theophylline toxicity with corresponding amnestic syndrome and hippocampal hyperintensities has been rarely reported. We believe this case with persistent abnormal Montreal Cognitive Assessment Score at 12 months correlates with persistent hippocampal abnormalities seen on imaging.
Keywords: memory disorders, drugs: CNS (not psychiatric), toxicology
Background
This case highlights the toxic effects of supratherapeutic dosing of theophylline. Theophylline is a widely prescribed medication used as adjunctive therapy in obstructive airways disease such as in asthma management.1 2 Given that it is a drug widely prescribed we believe it is important that the medical community is aware of the neurotoxicity profile seen even at therapeutic or low-toxic serum concentrations.3 This includes long-term neurological consequences with persistent short-term memory problems.3 Although rarely reported in the literature this side effect of theophylline toxicity should be highlighted to general practitioners and hospital doctors alike.
Case presentation
A woman in her 30s was brought to hospital by ambulance following an intentional overdose of 12.6 g theophylline and 630 mg lansoprazole. The patient had taken an intentional overdose 6.5 hours before presenting to hospital with dizziness, diaphoresis, nausea, vomiting and abdominal pain. On arrival she was transferred to the resuscitation bay. At the initial assessment her heart rate was 110/min, blood pressure was 144/89 mm Hg, oxygen saturations 98% on room air and a respiratory rate of 17. She was apyrexic. The patient developed generalised seizure activity terminated with intravenous midazolam. This was followed by a recurrent generalised seizure 30 min later which failed to terminate with 8 mg of intravenous lorazepam. At this time the patient had a sinus tachycardia of 148/min, blood pressure of 75/40 mm Hg, a respiratory rate of 17/min, oxygen saturations of 94% on room air and a temperature of 36.5°C. She was reviewed by the intensive care team and in order to manage the evolving acidosis and recurrent seizures a decision to intubate and ventilate was made. The patient’s blood pressure was closely monitored and a mean arterial pressure of >65 mmHg was maintained.
This woman had a medical history of asthma and depression. She was prescribed theophylline as part of her asthma treatment for a number of years and there had been no previous concerns about thoughts of self-harm or overdose.
The patient remained in the intensive care unit for 7 days. On day 5 there was no concern for further seizures and the patient was extubated. The intensive care unit staff noted the patient appeared to have very poor short-term recall. This was confirmed on Montreal Cognitive Assessment (MoCA). The patient was extensively worked up for evaluation of amnesia. Other causes of encephalitis were investigated and excluded.
Investigations
Within 3 hours of presenting the patient developed a profound mixed respiratory and metabolic acidosis with a raised anion gap (see table 1).
Table 1.
Serial arterial blood gas (ABG) measurements
| ABG 1 | ABG 2 | ABG 3 | ABG 4 | ABG 5 | ABG 6 | |
| pH | 7.19 | 6.99 | 7.25 | 7.32 | 7.27 | 7.4 |
| pCO2 (kPa) | 5.0 | 7.8 | 5.2 | 4.9 | 6.5 | 4.4 |
| pO2 (kPa) | 10.1 | 37.3 | 27.7 | 21.3 | 11.5 | 10 |
| HCO3 (mmol/L) | 14.2 | 14 | 17.1 | 18.9 | 22.1 | 20.5 |
| Lactate (mmol/L) | 5.8 | 13.9 | 6.8 | 2.8 | 2.1 | 1.2 |
| Glucose (mmol/L) | 8.9 | 10.6 | 9.6 | 8.1 | 9.1 | 7.8 |
Initial measurement taken after first generalised seizure in the emergency department. The patient was intubated following the second ABG outlined above. ABG 6 taken 10 hours post-intubation.
pCO2, partial pressure of carbon dioxide; pO2, partial pressure of oxygen.
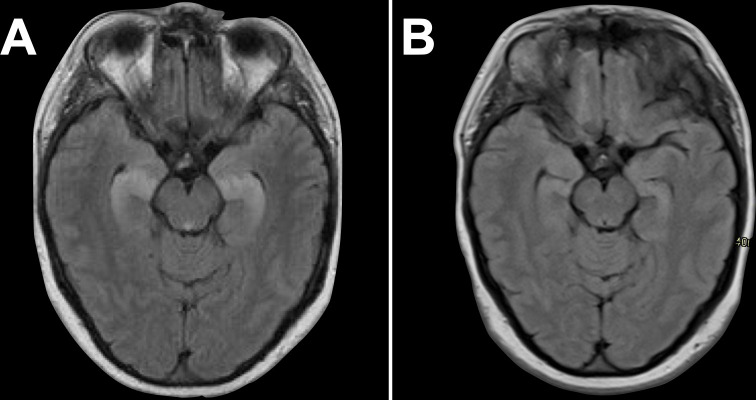
On serial blood gases the acidosis had corrected within 14 hours of admission (see table 1). The patient was noted to have a theophylline level of >40 mg/L (normal range 10–20 mg/L). She was treated with continuous haemofiltration until the theophylline level was not detectable. Following extubation the patient was noted to have a persistent short-term memory deficit and was worked up for other causes of encephalitis. A MoCA score was 15/30 (points missed: visuospatial/executive:1, naming:1, attention:3, language:1, abstraction:1, delayed recall:5, orientation:3). Ten days following extubation an MRI brain was performed and demonstrated bilateral hippocampal hyperintensities (figure 1A). Cerebrospinal fluid analysis was normal. Anti-NMDA, anti-VGKC, anti-AMPA1, anti-AMPA2 and anti-GABA antibody titres were negative. Electroencephalogram (EEG) was performed 21 days into admission and demonstrated runs of sharp theta occurring independently in the temporal regions, more marked on the right, suggesting significant bitemporal dysfunction, but without epileptiform features. Repeat MRI brain imaging after a further 14 days showed partial interval improvement corresponding to an improved MoCA score of 19/30 (points missed: naming:1, attention:2, language:1, delayed recall:5, orientation:2). Additional interval imaging was carried out at 4 months and identified improved but persistent bilateral hippocampal hyperintensities (figure 1B).
Figure 1.
(A) MRI brain T2-fluid attenuated inversion recovery (FLAIR)—admission scan demonstrating bilateral hyperintensities in the hippocampi. (B) MRI brain T2-FLAIR—4-month follow-up scan, demonstrates significantly reduced bilateral but persistent hippocampal hyperintensities.
Differential diagnosis
We considered status epilepticus in the first instance as the cause of the bilateral hippocampal hyperintensities. Given the amnestic syndrome other causes of encephalitis were investigated including infectious, autoimmune and paraneoplastic. Serum and cerebrospinal fluid tests failed to identify any other autoimmune or infectious aetiologies of the amnestic syndrome. EEG was also considered and carried out as non-convulsive status can present in many ways. Of note the electroencephalograph recording did not identify any suggestion of epileptiform activity.
On review of the literature we identified a number of case reports where theophylline toxicity was found to cause a persistent amnestic syndrome with corresponding MRI changes evident in some cases.4 Given no other cause was found to be responsible for the persistent neuroimaging abnormalities in our patient; we believe theophylline toxicity is responsible for the patient’s persistent amnestic syndrome.
Treatment
The patient was transferred to the intensive care unit where she was intubated and ventilated following the unsuccessful treatment of the generalised seizure activity with lorazepam. Sedation was maintained with a combination of propofol and midazolam. The patient was commenced on anticonvulsant therapy with intravenous levetiracetam to aid seizure control. Furthermore, the patient was placed on continuous venovenous haemofiltration. In addition, the patient received activated charcoal via nasogastric tube as part of the treatment regime to aid theophylline clearance. Norepinephrine therapy was required in the initial 24 hours to maintain blood pressure, and was weaned on day 2. Due to development of fever and elevated inflammatory markers the patient was commenced on intravenous piperacillin-tazobactam for management of lower respiratory tract infection on day 3 of admission. Sedation was weaned after 3 days and the patient was extubated on day 5. Antibiotic therapy was completed after 1 week at which time the patient had been deescalated to the high dependency unit. The patient was transferred to the ward on day 9 of admission. At this point the multidisciplinary team was involved in the patient’s care with a focus on cognitive function and rehabilitation.
Outcome and follow-up
After 4 weeks in hospital the patient was discharged to rehabilitation locally. The patient spent a number of months here before a dedicated neurorehabilitation bed was available in a national rehabilitation centre. On further outpatient assessment at 12 months the patient had persistent short-term memory difficulties and required ongoing supervision at home. This was evidenced on a repeat MoCA 20/30 (points missed: visuospatial:1, attention:3, language:1, delayed recall:5). This woman will be continued to be followed up in the outpatient setting. She has ongoing input from the Community Mental Health Team and has been linked with local organisations for patients with brain injuries.
Discussion
Seizures have been reported as a complication of theophylline toxicity.3 On review of the literature seizures can occur even in instances where patients have ingested therapeutic or what is deemed ‘low toxic’ levels of the drug.3 In a case series by Bahls et al, 9 of 12 patients had prolonged seizure activity despite aggressive anticonvulsant therapy. Of note this cohort cannot be directly compared with our patient as this patient group was older with a mean age of 67.2 years. 66% of the patients had underlying neurological conditions which likely increased their risk of developing seizures. However, this report highlights the need to cautiously prescribe theophylline to patients with underlying seizure risk factors.3 As mentioned earlier the young woman we report had a profound mixed metabolic and respiratory acidosis. On review of the literature, an excellent clinical response to lipid emulsion and activated charcoal for a mixed overdose of salbutamol and theophylline was described in one patient.5 Similarly, in this case activated charcoal was given to aid elimination of theophylline. Furthermore, theophylline clearance was aided by continuous venovenous haemofiltration. The literature suggests that the combination of haemofiltration and oral activated charcoal is useful treatment method in such cases.6 The patient described in this case report developed distributive shock; this appears to be a feature of theophylline toxicity.7 The haemodynamic instability resolved in our patient following theophylline removal.
Theophylline toxicity with corresponding amnestic syndrome and hippocampal hyperintensities has been rarely reported.4 8 The presumed pathogenesis of this is via inhibition of adenosine receptors resulting in hippocampal damage.4 Adenosine acts as both a homoeostatic regulator and neuromodulator in the central nervous system.9
The neuromodulatory role relies on balancing the activation of inhibitory A1 receptors and facilitatory A2 receptors via the control on excitatory glutamatergic synapses.9 Dragunow by using an animal model demonstrated that aminophylline may prolong seizure activity through the inhibition of A1 receptors.10
This lends support that other methylxanthine drugs likely play a role in the prolongation of seizure as was seen in our case. Kohl et al hypothesise excitation of glutamate due to failure of activation of A1 inhibitory receptors results in structural damage. We postulate that in our patient the persistent bilateral hippocampal MRI signal intensities and abnormalities on neurological testing are supportive of theophylline induced status epilepticus and damage to the hippocampi. This is supported by a number of cases of theophylline associated seizures resulting in cerebral damage. A case series that reviewed the neuropathology of five patients who died following status epilepticus and concurrent theophylline treatment identified lesions in the amygdala, hippocampus and thalamus.11
Learning points.
Theophylline while a commonly used drug in obstructive airway disease can have profound and long-lasting neurological sequelae if consumed in supra-therapeutic quantities as seen in overdose.
Theophylline should be administered with caution in older patients and those with underlying seizure risk factors.
Mesial temporal lobe hyperintensity can be seen following status epilepticus. These changes typically resolve following recovery. We postulate that in this case, the toxic effect of theophylline significantly contributed to the persistent neuroimaging abnormalities.
Footnotes
Contributors: EJ and DAO contributed equally to the paper. EJ, DAO, SD and TJC were all involved in the planning of this article. DAO, EJ, SD, TJC were involved in acquisition of data for the article including MRI and review and completion of MOCA. EJ, DAO, SD, TJC were involved in the design and layout of the article. EJ, DAO, SD, TJC were all involved in interpretation of data for the article and discussion was held over the findings in relation to the patient’s clinical condition. EJ, DAO, SD, TJC all contributed considerably to the article at each stage. TJC, DAO, SD, EJ were all involved in revising the article and agreeing on the final version to be submitted.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Barnes PJ. Theophylline. Am J Respir Crit Care Med 2013;188:901–6. 10.1164/rccm.201302-0388PP [DOI] [PubMed] [Google Scholar]
- 2. Weinberger M, Hendeles L. Theophylline in asthma. N Engl J Med Overseas Ed 1996;334:1380–8. 10.1056/NEJM199605233342107 [DOI] [PubMed] [Google Scholar]
- 3. Bahls FH, Ma KK, Bird TD. Theophylline-associated seizures with "therapeutic" or low toxic serum concentrations: risk factors for serious outcome in adults. Neurology 1991;41:1309. 10.1212/WNL.41.8.1309 [DOI] [PubMed] [Google Scholar]
- 4. Kohl Z, Uyanik G, Lürding R, et al. Selective bilateral hippocampal lesions after theophylline-induced status epilepticus causes a permanent amnesic syndrome. J Clin Neurosci 2011;18:964–6. 10.1016/j.jocn.2010.11.017 [DOI] [PubMed] [Google Scholar]
- 5. Chandrasekaran VP, Parthasarathy A, Muruga B, et al. Theophylline toxicity: successful management of a patient with distributive shock secondary to drug overdose. Am J Emerg Med 2020;38:2491.e1–2491.e2. 10.1016/j.ajem.2020.05.112 [DOI] [PubMed] [Google Scholar]
- 6. Shannon M. Life-Threatening events after theophylline overdose. Arch Intern Med 1999;159:989. 10.1001/archinte.159.9.989 [DOI] [PubMed] [Google Scholar]
- 7. Henderson JH, McKenzie CA, Hilton PJ, et al. Continuous venovenous haemofiltration for the treatment of theophylline toxicity. Thorax 2001;56:242–3. 10.1136/thorax.56.3.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. O'Riordan JI, Hutchinson J, FitzGerald MX, et al. Amnesic syndrome after theophylline associated seizures: iatrogenic brain injury. J Neurol Neurosurg Psychiatry 1994;57:643–5. 10.1136/jnnp.57.5.643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gomes CV, Kaster MP, Tomé AR, et al. Adenosine receptors and brain diseases: neuroprotection and neurodegeneration. Biochim Biophys Acta 2011;1808:1380–99. 10.1016/j.bbamem.2010.12.001 [DOI] [PubMed] [Google Scholar]
- 10. Dragunow M. Adenosine receptor antagonism accounts for the seizure-prolonging effects of aminophylline. Pharmacol Biochem Behav 1990;36:751–5. 10.1016/0091-3057(90)90072-P [DOI] [PubMed] [Google Scholar]
- 11. Mori H, Mizutani T, Yoshimura M, et al. Unilateral brain damage after prolonged hemiconvulsions in the elderly associated with theophylline administration. J Neurol Neurosurg Psychiatry 1992;55:466–9. 10.1136/jnnp.55.6.466 [DOI] [PMC free article] [PubMed] [Google Scholar]