ABSTRACT
The outbreak of the novel SARS-CoV-2 virus has an enormous impact on health. People’s views about the virus impact public health efforts to mitigate the pandemic. In this study, we measured misconceptions toward coronavirus in the Jordanian population; 2,544 participants from the Jordanian population completed an online survey. Questions in the survey addressed misconceptions divided into four categories: optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs. Questions were evaluated on a Likert scale, and average/median scores for each category were evaluated (“one” high misconception to “five” low misconception). Overall, the most common misconceptions involved conspiracy theory beliefs (2.68 ± 0.83), whereas the least common involved magical beliefs (2.25 ± 0.75). Females had more misconceptions than males (2.52 versus 2.47, P = 0.04). Participants who had attended a lecture on coronavirus, had a higher level of education, worked in a medical field, lived in urban area, or resided in Amman or northern Jordan had fewer misconceptions about SARS-CoV-2/COVID-19 (2.64, 2.34, 2.33, 2.50 and 2.50 versus 2.53, 2.73, 2.72, 2.64, and 2.66, respectively, P < 0.001). The use of social media appeared to be an important factor influencing the likelihood of false beliefs (2.61 versus 2.38, P < 0.001). Understanding of the factors influencing public perceptions surrounding the SARS-CoV-2/COVID-19 pandemic will help public health authorities improve public understanding and compliance with public health recommendations directed at combatting the virus, including the use of surgical masks, thorough handwashing, and avoiding close contact. These messages will be better received by the public through correcting misconceptions surrounding COVID-19.
INTRODUCTION
Since the emergence of this pandemic, governments and international agencies across the world have worked to slow the spread of the virus and reduce the number of infections and consequent deaths resulting from COVID-19. Different strategies have been implemented in different countries to reduce the transmission of SARS-CoV-2. These strategies include community testing, isolation of symptomatic cases and quarantine of their contacts, contact tracing using app-digital tracing, physical distancing, school closures, remote working, community testing, cancellation of events and mass gatherings, travel restrictions (both between and within countries), and promotion of improved hand hygiene.1 These preventive and control measures have been implemented in different countries across the world at various levels and with different degrees of effectiveness.2 Understanding factors that limit the effectiveness of these measures is important to public health efforts to combat the pandemic.
Jordan was among the countries that adopted strict national and local strategies to curb the spread of coronavirus. In the middle of March, after just a few cases of SARS-CoV-2/COVID-19 were reported (29 confirmed COVID-19 cases on March 173), the government of Jordan led the fight against COVID-19 by activating the Kingdom’s 1992 Defence Law. The government announced a full lockdown and a strictly enforced curfew.2,3 This was described as one of the world’s strictest measures.3
In addition to the 3-month strict lockdown, the government isolated confirmed cases in hospitals assigned to exclusively treat COVID-19, provided quarantine of asymptomatic contacts, and conducted random viral testing surveillance. These measures significantly reduced the daily reported confirmed cases of COVID-19, resulting in a “flattening of the curve” for COVID-19 infections and number of confirmed cases, reducing the impact of COVID-19 on healthcare systems3. This was the worldwide goal for a successful response to the outbreak, preventing the epidemic from overwhelming health resources and consequently spiraling out of control as it has in some countries such as the United States. As a result, these measures resulted in low mortality rates in Jordan: only 4,170 deaths from 316,427 confirmed cases. This is a disease incidence rate of only 0.3%, compared with more than 10% in the United States. In Jordan, a case mortality rate of 1.3% was observed, with deaths primarily occurring in elderly patients with underlying conditions.
Whereas Jordan and the world is still suffering from the coronavirus pandemic, a large number of misconceptions, partially promulgated by false information about COVID-19 distributed on social media, are circulating among Jordanians.4 These misconceptions can hamper public health efforts. The persistence of these misconceptions might ironically be related in part to the low number of confirmed cases and deaths in Jordan because most Jordanians lack personal experience with the disease through affected friends and family members. These misconceptions about COVID-19 are spread online via social media platforms such as Facebook, Twitter, Instagram, and YouTube.5 These misconceptions involve false or misleading beliefs concerning the etiology, outcomes, prevention, or treatment of the disease, including supposed “cures” of various kinds. The prevalence of these misconceptions has resulted in reduced compliance with the precautions and guidelines that the Ministry of Health is asking from the people, such as social distancing, diligent hygiene, avoidance of public gatherings, self-quarantine when exposed to an infected individual, and the consistent wearing of face masks in public.5
Four categories of misconceptions, which surround the COVID-19 outbreak, were studied in the Jordanian population. These misconceptions were reported previously by Pennycook et al.6 and were categorized as optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs. It was necessary to evaluate these misconceptions as these beliefs limit the ability of healthcare agencies in Jordan and worldwide in mitigating the spread of the disease. By assessing the level and nature of the misconceptions surrounding COVID-19, we believe that targeted information campaigns can be formulated in a way that will improve public understanding of the disease and awareness of the necessary public health actions that will help to minimize the impact of COVID-19 on the health system. Such a campaign will in turn emphasize the importance of reducing the spread of the virus through physical distancing, handwashing, wearing masks in public, and other important public health measures. Also, these measures will improve compliance that might be limited by public misconceptions. To the best of our knowledge, this study represents the first evaluation of misconceptions surrounding the COVID-19 outbreak in the Jordanian population. Similar misconceptions are likely to exist across the globe, and many of the factors which influence the prevalence of these misconceptions will similarly affect people worldwide, perhaps even more so in countries that have had less effective responses to the outbreak such as in the United States.
MATERIALS AND METHODS
Design and ethics.
This was a cross-sectional web-based survey conducted in the Jordanian population. The sample was limited to individuals of 18 years and older. The purpose of this study was to examine misconceptions toward COVID-19. The study was approved by the Al-Zaytoonah University of Jordan Research Ethics Committee (Ref. 26/12/2019-2020).
Survey.
The survey consisted of two sections. The first section consisted of 11 multiple-choice questions which asked for anonymous demographic information about the respondents. The second section included 31 questions measuring the respondents’ views of different misconceptions about COVID-19. These questions were created based on a previous study,6 with some additional questions derived from falsehoods that have been spread about COVID-19 in news reports, in social media reports, and identified in fact-checking efforts. The misperceptions that we considered fit broadly into four categories: optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs (see Appendix 1). Participants were asked to rate their opinions on a five-point Likert scale, from 1 (strongly disagree) to 5 (strongly agree), when the question involved agreeing with a correct statement. The Likert scale was reversed, from 5 (strongly disagree) to 1 (strongly agree), when the direction of the question involved disagreeing with an incorrect statement. This represented the score for each question. The mean of the questions in each misconception category represented the category score. The final misconception score was the mean of the 31 questions included in the questionnaire. The survey took approximately 5–10 minutes to complete. Reliability was assessed for total misconceptions using Cronbach’s α.
Procedure.
The survey was formulated on Google Forms, and the participant information sheet was hosted on an online platform. The link to the survey was distributed through different social media sites, including different Jordanian all-purpose Facebook groups that included thousands of members, including coronavirus “COVID-19”/Jordan. There was no maximum enrolment on the Google Form. To ensure the fulfillment of the inclusion criteria, questions about age and area of residence were included in the questionnaire. No financial incentives were offered. The survey was distributed, and data were collected, between May 2020 and June 2020.
Data analysis.
Categorical variables were expressed as frequencies and percentages, whereas continuous variables were expressed as means and SD. Dummy variables were created for questions that allowed multiple options, including the source of information on COVID-19. For each category, a mean value was calculated for the average Likert value of all questions for that category. The normal distribution for the category means and for the total mean values were evaluated using the Kolmogorov–Smirnov test. The Mann–Whitney U test and the Kruskal–Wallis one-way analysis of variance (ANOVA) were applied to compare mean ranks when normality was not observed, whereas t-tests and ANOVA were applied when normality was observed to evaluate the differences in category scores between each subgroup. Friedman and Wilcoxon tests were used to determine the differences between the mean ranks of each category of misconception toward COVID-19. In each category, participants were separated into two groups according to their scores in each category and in the total misconception; those who scored above the mean were included in the high misconception group, whereas those who scored below the mean were placed in the low misconception group. Multiple binary logistic regression models were conducted to evaluate factors associated with a degree of misconception in each category and in total misconception. Finally, analysis of covariance (ANCOVA) with post hoc models were conducted to evaluate the association of the demographic variables with mean misconception values. The assumption of equal variance was evaluated using Levene’s test. All data analyses were conducted using SPSS version 25 (SPSS Inc., Chicago, IL).
RESULTS
Sociodemographic characteristics of participants.
A total of 2,544 participants completed the survey. Most of the respondents were women (81.5%). More than half of the respondents (60.5%) were aged between 18 and 29 years. In addition, 61.2% of the respondents were not married, and 64.5% did not have any children. Almost all of the participants (91.2%) lived in Amman city, and about 72.2% of them had a university degree (bachelor degree). When the participants were asked whether they were students or employed, and in what field, it was found that the most common working group (27.2%) worked in a nonmedical field, whereas the most common student group was medical students (21.1%). A majority of the participants (73.9%) had not viewed a lecture, such as a public health presentation or discussion about COVID-19. The full sociodemographic characteristics of participants are given in Table 1.
Table 1.
Sociodemographic characteristics of all participants (n = 2,544) and the general population
| Variable | N (%) | General population (n = 6,015,780)%*,†,‡ | P-value |
|---|---|---|---|
| Gender | |||
| Male | 470 (18.5) | 54.07 | < 0.001 |
| Female | 2074 (81.5) | 45.93 | |
| Age-group (years) | |||
| 18–29 | 1,538 (60.5) | 53.48 | < 0.001 |
| 30–39 | 515 (20.2) | 20.11 | |
| 40–49 | 286 (11.2) | 19.49 | |
| 50 and older | 205 (8.1) | 6.92 | |
| Marital status | |||
| Not married | 1,557 (61.2) | 44.50 | < 0.001 |
| Married | 987 (38.8) | 55.50 | |
| Do you have children? | NA | ||
| Yes | 903 (35.5) | ||
| No | 1,641 (64.5) | ||
| Educational level | |||
| High-school degree or less | 194 (7.6) | NA | |
| Community college level | 179 (7.0) | ||
| University level | 1836 (72.2) | ||
| Postgraduate | 335 (13.2) | ||
| Employment status | |||
| Working in a medical field | 526 (20.7) | NA | |
| Working in a nonmedical field | 691 (27.2) | ||
| Student in a medical school | 534 (21.1) | ||
| Student in a scientific and an engineering school | 274 (10.8) | ||
| Student in other schools | 519 (20.4) | ||
| Place of residence | NA | ||
| Urban | 2,320 (91.2) | 91.50 | |
| Rural | 224 (8.8) | 8.50 | |
| Residential area | < 0.001 | ||
| Amman | 1,674 (65.8) | 55.40 | |
| Northern Jordan | 417 (16.4) | 20.50 | |
| Middle Jordan | 314 (12.3) | 15.87 | |
| East Jordan | 37 (1.5) | 2.00 | |
| Southern Jordan | 102 (4.0) | 6.20 | |
| Took a lecture, such as a public health presentation or discussion, about COVID-19 (yes) | 685 (26.9) | NA | NA |
| The place where COVID-19 lecture was taken | |||
| At work | 67 (2.6) | NA | NA |
| At university | 146 (5.7) | ||
| Online | 472 (18.6) |
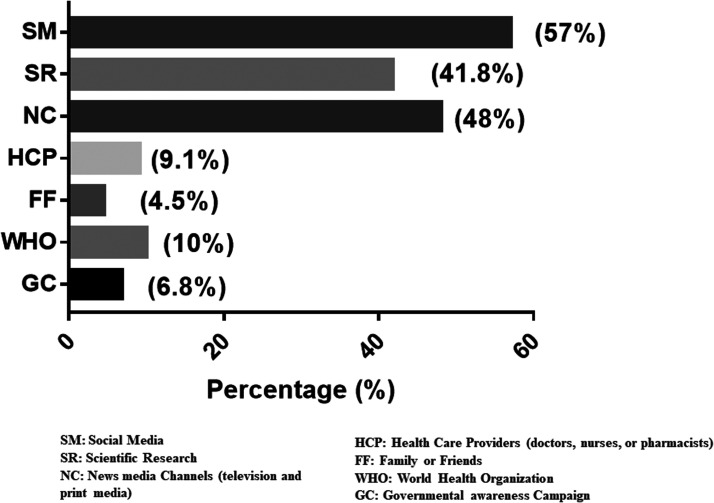
Different sources of information about COVID-19 were used by the respondents; 57% of them used the social media as their main source for information about the disease (Figure 1).
Figure 1.
Participant-stated primary sources of information on COVID-19.
Participants’ misconceptions toward the COVID-19 pandemic.
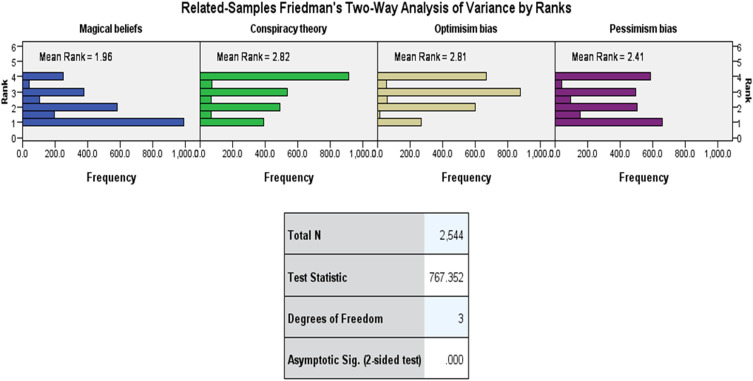
The Kolmogorov–Smirnov test showed that the means of the Likert scores for each of the four categories (optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs) were not normally distributed. Therefore, Freidman and Wilcoxon tests were applied to evaluate the differences in scores between each category. The results of the test indicated that there were significant differences between the four categories. The score with the highest mean rank was for conspiracy theory beliefs (2.82), and the lowest score was for the magical beliefs (1.96), whereas the scores for the optimism bias and pessimism bias were 2.81 and 2.41, respectively (Figure 2).
Figure 2.
Related-samples Friedman’s two-way analysis of variance by ranks for total misconception in each category. This figure appears in color at www.ajtmh.org.
The individual mean values for each question and for each category are shown in Table 2. For the first category, optimism bias, the highest mean Likert value was for “an antidote will be discovered soon” (3.59), and the lowest mean was for “you can’t spread the virus unless you feel sick” (1.79). For the second category, pessimism bias, the highest mean was for “most people who get infected will need to go to the hospital” (2.90) and the lowest mean was for “COVID-19 will kill most people who are infected” (1.84). For the third category, magical beliefs, the highest mean was for “Vitamin C can treat COVID-19” (2.52), and the lowest mean was for “Eating bananas treats COVID-19” (1.97). Finally, for the fourth category, conspiracy theory beliefs, the highest means were for “COVID-19 is laboratory made” (3.25) and “COVID-19 was made as a biological weapon” (3.25), whereas the lowest mean was for “COVID-19 was made to insert a microchip into humans” (2.08). The overall mean misconception value was reliable with Cronbach’s α = 0.86.
Table 2.
Mean and SD for each question of the four categories
| Category | Question | Mean (SD) |
|---|---|---|
| Optimism bias | Seasonal flu is as dangerous as coronavirus. | 2.75 (1.10) |
| You cannot spread the virus unless you feel sick. | 1.79 (0.95) | |
| Coronavirus does exist but it is not very dangerous. | 3.13 (1.20) | |
| Coronavirus does not stay on plastic steel or clothes for more than a few minutes. | 2.26 (1.05) | |
| Coronavirus symptoms are of short term. | 2.49 (0.95) | |
| Warm weather stops the spread of coronavirus in an effective level. | 2.22 (1.01) | |
| Warm weather stops the aggressiveness of coronavirus in an effective level. | 2.37 (1.02) | |
| You can immediately know (within a day) if you get affected. | 2.19 (1.06) | |
| The virus is relatively big, which is why any face mask can prevent it from reaching the face. | 2.45 (1.15) | |
| Coronavirus stays alive on your hand for 5–10 minutes. | 2.89 (1.16) | |
| Coronavirus does not move through atmosphere. | 2.98 (1.24) | |
| Coronavirus will disappear with time. | 3.31 (1.13) | |
| There will not be a second wave of coronavirus. | 2.58 (0.96) | |
| An antidote will be discovered soon. | 3.59 (0.88) | |
| Total mean (SD) | 2.64 (0.50) | |
| Pessimism bias | Wearing masks and gloves will not protect us from getting infected. | 2.66 (1.19) |
| Most people who get infected will need to go to the hospital. | 2.90 (1.19) | |
| Coronavirus will kill most people who are infected by it. | 1.84 (0.84) | |
| It is very likely that people who leave their house and go out for a walk will get infected. | 2.22 (1.03) | |
| Based on the natures of the virus it is hard to make a cure. | 2.73 (0.99) | |
| Total mean (SD) | 2.47 (0.59) | |
| Magical beliefs | Vitamin C can treat coronavirus. | 2.52 (1.01) |
| Holding my breath for 10 seconds is an effective way to tests whether you have the virus or not. | 2.37 (1.01) | |
| Garlic and olive oil can treat coronavirus. | 2.12 (0.93) | |
| Eating bananas treats coronavirus. | 1.97 (0.83) | |
| If a person gargles with warm water and salt or vinegar it will help to get rid of the virus. | 2.29 (1.02) | |
| Total mean (SD) | 2.25 (0.75) | |
| Conspiracy theory | Coronavirus is laboratory made. | 3.25 (1.16) |
| Coronavirus is made as a biological weapon. | 3.25 (1.12) | |
| An antidote is already discovered but is kept away by those who want the virus to stay. | 2.94 (1.10) | |
| Coronavirus is lie. | 2.19 (1.06) | |
| Coronavirus is actually bacteria that clots blood. | 2.16 (1.06) | |
| Coronavirus was made to insert a microchip into humans. | 2.08 (1.07) | |
| Coronavirus was made for political reasons. | 2.93 (1.21) | |
| Total mean (SD) | 2.68 (0.83) |
Association between different sample characteristics and category mean ranks.
Comparisons between groups based on demographic characteristics are shown in Table 3. Women had a higher mean rank value for conspiracy theory beliefs (1,295.01) than men (1,173.19; P-value < 0.01). When comparing different age-groups, the 18–29 age-group had a higher total mean rank for pessimism bias, and a lower rank for magical beliefs and conspiracy theory beliefs (1,420.68, 1,209.96, and 1,236.39, respectively) than the 50 and older age-group (948.32, 1,462.23, and 1,304.78, respectively; P-value < 0.01 for all comparisons). It was also clear that married participants had significantly higher total mean ranks for magical beliefs and conspiracy theory beliefs (1,357.94 and 1,344.46, respectively) than unmarried subjects (1,218.34 and 1,226.88, respectively; P-value < 0.01). By contrast, unmarried participants had significantly higher mean rank values for pessimism bias (1,370.38) than married participants (1,118.10; P-value < 0.01). Participants with children had significantly higher mean rank values for optimism bias, magical beliefs, and conspiracy theory beliefs (1,318.07, 1,364.27, and 1,358.19, respectively) than participants who did not have children (1,247.42, 1,222.00, and 1,225.35, respectively; P-value < 0.01). Moreover, participants who did not have children had significantly higher total mean rank values for pessimism bias (1,356.74) than participants who had children (1,119.41; P-value < 0.01). Participants who had attended a lecture, such as a public health presentation or discussion about COVID-19, had significantly lower total mean rank values for optimism bias, magical beliefs, and conspiracy theory beliefs (1,209.77, 1,220.25, and 1,161.17, respectively) than participants who did not see a lecture about COVID-19 (1,294.70, 1,290.99, and 1,311.90, respectively; P-value ≤ 0.03). Participants with a higher educational level had significantly lower mean rank values for optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs (1,147.67, 957.69, 1,135.25, and 1,106.73, respectively) than participants with other educational levels (P-value < 0.01). Participants who worked in a medical field had lower total mean rank values for optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs (1,129.96, 1,029.56, 1,072.57, and 1,057.59, respectively) than participants who worked in other employment groups (P-value < 0.01). Participants who lived in a rural area had higher total mean rank values for pessimism bias, magical beliefs, and conspiracy theory beliefs (1,448.89, 1,393.03, and 1,439.20, respectively) than participants who lived in urban areas (P-value < 0.01). Participants who lived in east Jordan (a more rural region) had higher mean rank values for pessimism bias (1,651.84) than participants who lived in other residential areas (P-value < 0.01). Finally, participants who used social media as a source of information had a higher mean rank value for optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs (1,366.57, 1,341.56, 1,407.42, and 1,405.58, respectively) than participants who did not use social media as a source of information (1,147.82, 1,180.97, 1,093.68, and 1,096.11, respectively) (P-value < 0.01).
Table 3.
Association between different sample characteristics and misconception categories
| Independent variables | Optimism bias | Pessimism bias | Magical beliefs | Conspiracy theory beliefs | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean rank | P-value | Mean rank | P-value | Mean rank | P-value | Mean rank | P-value | Mean (SD) | P-value | ||
| Gender | Male | 1,260.02 | 0.68 | 1,215.59 | 0.06 | 1,248.25 | 0.43 | 1,173.19 | < 0.001 | 2.47 (0.54) | 0.04 |
| Female | 1,275.33 | 1,285.40 | 1,278.00 | 1,295.01 | 2.52 (0.46) | ||||||
| Age-group (years) | 18–29 | 1,253.68 | 0.38 | 1,420.68 | < 0.001 | 1,209.96 | < 0.001 | 1,236.39 | < 0.001 | 2.51 (0.48) | 0.98 |
| 30–39 | 1,306.24 | 1,111.12 | 1,302.84 | 1,345.23 | 2.52 (0.48) | ||||||
| 40–49 | 1,315.53 | 998.60 | 1,418.18 | 1,312.60 | 2.51 (0.48) | ||||||
| 50 and older | 1,268.89 | 948.32 | 1,462.23 | 1,304.78 | 2.50 (0.48) | ||||||
| Marital status | Not married | 1,255.89 | 0.15 | 1,370.38 | < 0.001 | 1,218.34 | < 0.001 | 1,226.88 | < 0.001 | 2.50 (0.48) | 0.27 |
| Married | 1,298.71 | 1,118.10 | 1,357.94 | 1,344.46 | 2.53 (0.48) | ||||||
| Children | Yes | 1,318.07 | 0.02 | 1,119.41 | < 0.001 | 1,364.27 | < 0.001 | 1,358.19 | < 0.001 | 2.54 (0.48) | 0.06 |
| No | 1,247.42 | 1,356.74 | 1,222.00 | 1,225.35 | 2.50 (0.48) | ||||||
| Educational level | High-school degree or less | 1,514.95 | < 0.001 | 1,566.52 | < 0.001 | 1,504.49 | < 0.001 | 1,450.66 | < 0.001 | 2.73 (0.52) | < 0.001 |
| Community college level | 1,487.86 | 1,410.78 | 1,555.74 | 1,522.77 | 2.72 (0.46) | ||||||
| University level | 1,248.66 | 1,285.39 | 1,245.42 | 1,259.52 | 2.50 (0.46) | ||||||
| Postgraduate | 1,147.67 | 957.69 | 1,135.25 | 1,106.73 | 2.34 (0.49) | ||||||
| Employment status | Working in a medical field | 1,129.96 | < 0.001 | 1,029.56 | < 0.001 | 1,072.57 | < 0.001 | 1,057.59 | < 0.001 | 2.33 (0.45) | < 0.001 |
| Working in a nonmedical field | 1,310.39 | 1,184.86 | 1,393.05 | 1,393.87 | 2.56 (0.47) | ||||||
| Student in a medical school | 1,136.48 | 1,418.45 | 1,128.62 | 1,081.00 | 2.42 (0.46) | ||||||
| Student in a scientific or engineering school | 1,250.67 | 1,240.18 | 1,255.77 | 1,297.25 | 2.51 (0.48) | ||||||
| Student in other schools | 1,517.99 | 1,502.29 | 1,471.50 | 1,512.68 | 2.72 (0.45) | ||||||
| Place of residence | Urban | 1,268.56 | 0.38 | 1,255.47 | < 0.001 | 1,260.86 | 0.01 | 1,256.40 | < 0.001 | 2.50 (0.48) | < 0.001 |
| Rural | 1,313.31 | 1,448.89 | 1,393.03 | 1,439.20 | 2.64 (0.50) | ||||||
| Residential area | Amman | 1,265.05 | 0.90 | 1,241.35 | < 0.001 | 1,258.18 | 0.34 | 1,261.18 | 0.28 | 2.50 (0.48) | 0.03 |
| Northern Jordan | 1,279.81 | 1,249.83 | 1,279.81 | 1,244.17 | 2.50 (0.47) | ||||||
| Middle Jordan | 1,299.15 | 1,389.24 | 1,286.24 | 1,333.90 | 2.56 (0.47) | ||||||
| East Jordan | 1,214.57 | 1,651.84 | 1,380.43 | 1,392.23 | 2.66 (0.46) | ||||||
| Southern Jordan | 1,303.82 | 1,379.42 | 1,396.15 | 1,341.68 | 2.59 (0.54) | ||||||
| Lecture, such as public health presentation or discussion, about coronavirus? | Yes | 1,209.77 | 0.01 | 1,261.08 | 0.64 | 1,220.25 | 0.03 | 1,161.17 | < 0.001 | 2.46 (0.50) | < 0.001 |
| No | 1,294.70 | 1,276.54 | 1,290.99 | 1,311.90 | 2.53 (0.47) | ||||||
| Social media as a source of information | Yes | 1,366.57 | < 0.001 | 1,341.56 | < 0.001 | 1,407.42 | < 0.001 | 1,405.58 | < 0.001 | 2.61 (0.47) | < 0.001 |
| No | 1,147.82 | 1,180.97 | 1,093.68 | 1,096.11 | 2.38 (0.46) | ||||||
Odds ratios for comparisons between groups are shown in Table 4. There was a significant association between educational level and optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs. Having an high-school degree or less, or a university-level education, increased optimism bias compared with post-graduate level education, with odds ratios of 1.83 and 1.73, respectively. Similarly, a lower level of education increased pessimism bias, with odds ratios of 2.26 and 1.83, respectively. However, having an high-school degree or less, a community college–level education, or a university-level education, increased magical beliefs, with odds ratios of 2.04, 1.44, and 2.39, respectively; and increased conspiracy theory beliefs, with odds ratios of 1.99, 1.68, and 2.76, respectively, compared with a postgraduate level of education. Equally, a significant association was found between employment status and optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs. Being a student in a scientific or an engineering school increased optimism bias compared with other professions, with an odds ratio of 1.66. Working in a nonmedical field, being a student in a scientific or an engineering school, or being a student in a medical field increased pessimism bias compared with other professions, with odds ratios of 1.53, 2.11, and 1.40, respectively. Working in a nonmedical field decreased magical beliefs compared with other professions, with an odds ratio of 0.70, whereas being a student in a scientific or an engineering school increased magical beliefs compared with other professions, with an odds ratio of 1.43. Working in a medical field reduced conspiracy theory belief compared with other professions, with an odds ratio of 0.58. Being a student in a scientific or an engineering school increased conspiracy theory beliefs compared with other professions, with an odds ratio of 1.68. Significant associations were found between age and pessimism bias and magical beliefs. The 18–29 and 30–39 age-groups had greater pessimism bias than the 50 and older age-group, with odds ratios of 3.22 and 1.64, respectively. Moreover, the 18–29 and 30–39 age-groups had reduced magical beliefs compared with the 50 and older age-group, with odds ratios of 0.58 and 0.70, respectively. A significant association was revealed between residential area and magical beliefs. Living in Amman reduced magical beliefs compared with living in the middle of Jordan, with an odds ratio of 0.73. Also, attending a lecture, such as a public health presentation or discussion about COVID-19, had a significant association with conspiracy theory beliefs, resulting in fewer conspiracy theory–based beliefs than not viewing a lecture, with an odds ratio of 1.23. Finally, getting information from social media increased optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs, compared with getting information from other sources, with odds ratios of 1.60, 1.40, 1.92, and 1.90, respectively.
Table 4.
A binary regression indicating different variables’ association with the degree of misconception in each category (n = 2,544)
| B | S.E. | Wald | df | P-value | Odds ratio | 95% CI of odds ratio | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Optimism bias | ||||||||
| Educational level | ||||||||
| High-school degree or less compared with postgraduate | 0.61 | 0.20 | 9.52 | 1.00 | < 0.001 | 1.83 | 1.25 | 2.70 |
| University level compared with postgraduate | 0.55 | 0.19 | 8.03 | 1.00 | < 0.001 | 1.73 | 1.18 | 2.52 |
| Employment status | ||||||||
| Student in scientific or an engineering school compared with student in other schools | 0.51 | 0.16 | 10.59 | 1.00 | < 0.001 | 1.66 | 1.22 | 2.25 |
| Social media as a source of information | ||||||||
| Yes compared with no | 0.47 | 0.08 | 31.58 | 1.00 | < 0.001 | 1.60 | 1.36 | 1.89 |
| Pessimism bias | ||||||||
| Age-group (years) | ||||||||
| 18–29 compared with 50 and older | 1.17 | 0.20 | 34.48 | 1.00 | < 0.001 | 3.22 | 2.18 | 4.76 |
| 30–39 compared with 50 and older | 0.49 | 0.19 | 6.65 | 1.00 | 0.01 | 1.64 | 1.13 | 2.39 |
| Educational level | ||||||||
| High-school degree or less compared with postgraduate | 0.81 | 0.21 | 15.50 | 1.00 | < 0.001 | 2.26 | 1.51 | 3.39 |
| University level compared with postgraduate | 0.61 | 0.20 | 8.93 | 1.00 | < 0.001 | 1.83 | 1.23 | 2.72 |
| Employment status | ||||||||
| Working in a nonmedical field compared with student in other schools | 0.43 | 0.16 | 7.12 | 1.00 | 0.01 | 1.53 | 1.12 | 2.09 |
| Student in scientific or an engineering school compared with student in other schools | 0.75 | 0.16 | 21.55 | 1.00 | < 0.001 | 2.11 | 1.54 | 2.89 |
| Student in a medical school compared with student in other schools | 0.34 | 0.16 | 4.58 | 1.00 | 0.030 | 1.40 | 1.03 | 1.91 |
| Residential area | ||||||||
| Amman compared with middle Jordan | −0.32 | 0.13 | 6.15 | 1.00 | 0.01 | 0.73 | 0.56 | 0.93 |
| Social media as a source of information | ||||||||
| Yes compared with no | 0.33 | 0.09 | 14.74 | 1.00 | < 0.001 | 1.40 | 1.18 | 1.65 |
| Magical beliefs | ||||||||
| Age-group (years) | ||||||||
| 18–29 compared with 50 and older | −0.55 | 0.18 | 9.06 | 1.00 | 0.003 | 0.58 | 0.40 | 0.83 |
| 30–39 compared with 50 and older | −0.36 | 0.18 | 4.20 | 1.00 | 0.041 | 0.70 | 0.50 | 0.98 |
| Educational level | ||||||||
| High-school degree or less compared with postgraduate | 0.72 | 0.20 | 12.94 | 1.00 | < 0.001 | 2.04 | 1.38 | 3.02 |
| Community college level compared with postgraduate | 0.36 | 0.13 | 7.29 | 1.00 | 0.01 | 1.44 | 1.10 | 1.87 |
| University level compared with postgraduate | 0.87 | 0.20 | 19.45 | 1.00 | < 0.001 | 2.39 | 1.62 | 3.51 |
| Employment status | ||||||||
| Working in a nonmedical field compared with student in other schools | −0.35 | 0.16 | 4.75 | 1.00 | 0.03 | 0.70 | 0.51 | 0.97 |
| Student in scientific or an engineering school compared with student in other schools | 0.35 | 0.16 | 5.02 | 1.00 | 0.03 | 1.43 | 1.05 | 1.94 |
| Social media as a source of information | ||||||||
| Yes compared with no | 0.66 | 0.08 | 56.91 | 1.00 | < 0.001 | 1.92 | 1.63 | 2.29 |
| Conspiracy theory beliefs | ||||||||
| Taken a lecture on coronavirus | ||||||||
| No compared with yes | 0.20 | 0.10 | 4.31 | 1.00 | 0.04 | 1.23 | 1.01 | 1.49 |
| Educational level | ||||||||
| High-school degree or less compared with postgraduate | 0.67 | 0.20 | 11.68 | 1.00 | 0.001 | 1.99 | 1.34 | 2.95 |
| Community college level compared with postgraduate | 0.52 | 0.13 | 15.04 | 1.00 | < 0.001 | 1.68 | 1.29 | 2.19 |
| University level compared with postgraduate | 1.02 | 0.20 | 25.42 | 1.00 | < 0.001 | 2.76 | 1.86 | 4.09 |
| Employment status | ||||||||
| Working in a medical field compared with student in other schools | −0.54 | 0.16 | 11.41 | 1.00 | 0.001 | 0.58 | 0.43 | 0.80 |
| Student in scientific or an engineering school compared with student in other schools | 0.52 | 0.16 | 10.77 | 1.00 | 0.001 | 1.68 | 1.23 | 2.29 |
| Social media as a source of information | ||||||||
| Yes compared with no | 0.64 | 0.90 | 55.88 | 1.00 | < 0.001 | 1.90 | 1.60 | 2.24 |
B = coefficient; standard error = SE; Wald chi-square test = Wald; degrees of freedom = df; P-value = P.
Analysis of covariance and post hoc analysis of demographic effects on mean misconception values.
The results of the ANCOVA for the differences between demographic subgroups in mean misconception values are shown in Table 5. Normality of the total misconception means was confirmed with the Kolmogorov–Smirnov test. In addition, the assumption of equal variance was met as indicated by Levene’s test. The mean total misconception values were significantly associated with educational level, employment status, residential area, and having social media as a source of information; F (3,2544) = 28.24, F (1,2544) = 19.28, F (4,2543) = 33.76, and F (1,2543) = 117.08, respectively, P < 0.01 for all analyses. Post hoc comparisons between demographic groups indicated that for the educational level, respondents with a postgraduate education had significantly lower mean misconceptions overall than those with other educational levels. Similarly, those with a university-level education had significantly less total mean misconceptions than those with other educational levels, except for the postgraduate educational level. Participants who worked in a medical field had significantly lower total mean misconceptions than those with other employment categories, except for medical students. Similarly, participants who were students in a medical field had significantly lower total mean misconceptions than those with other employment categories, except for participants who worked in a medical field. Participants who lived in an urban area had significantly lower total mean misconceptions than those who lived in a rural area. Finally, participants who used social media as a source of information had significantly higher total mean misconceptions than those who did not use social media as a source of information.
Table 5.
Post hoc analysis indicating the statistical difference in total misconception means among different significance subgroups
| Educational level | ||||
|---|---|---|---|---|
| General certificate | Diploma | University level | Postgraduate | |
| High-school degree or less | 1 | −0.15* | 0.05 | −0.30* |
| Community college level | – | 1 | 0.19* | −0.15* |
| University level | – | – | 1 | −0.34* |
| Postgraduate | – | – | – | 1 |
| Employment status | |||||
|---|---|---|---|---|---|
| Working in a medical field | Working in a non-medical field | Student in other schools | Student in a medical school | Student in a scientific and an engineering school | |
| Working in a medical field | 1 | 0.22* | 0.33* | 0.05 | 0.16* |
| Working in a nonmedical field | – | 1 | 0.12* | −0.16* | −0.06 |
| Student in other schools | – | – | 1 | −0.28* | −0.17* |
| Student in a medical school | – | – | – | 1 | 0.11* |
| Student in a scientific and an engineering school | – | – | – | – | 1 |
| Place of residence | |||||
|---|---|---|---|---|---|
| Urban | Rural | ||||
| Rural | 0.14* | 1 | |||
| Social media as a source of information | |||||
|---|---|---|---|---|---|
| Yes | No | ||||
| Yes | 1 | 0.19* | |||
P-value < 0.01.
DISCUSSION
In this study, we developed a questionnaire to measure the major misconceptions associated with the COVID-19 pandemic in the Jordanian population. We divided the misconceptions into four categories according to the nature of the misconceptions: optimism bias, pessimism bias, magical beliefs, and conspiracy theory beliefs. All questions were included in the analysis based on the high reliability score measured by Cronbach’s α, which was not increased if any individual item was eliminated. We found that the highest mean of misconceptions surrounding COVID-19 was related to conspiracy theory beliefs, whereas the lowest mean of misconceptions was associated with magical beliefs. In a general way, the demographic analysis is consistent with previous observations of the relationship of many of these variables to these types of beliefs. Conspiracy theory beliefs are greater in individuals who are more likely to infer events in terms of preexisting belief systems.7,8 Several related psychological and sociological explanations can clarify the nature of this phenomenon. Previous studies have shown that people who believe in multiple conspiracy theories are likely to have a predisposition to infer information in a way that links patterns, connections, and causal relationships to events whether there is evidence of a causal relationship or not.9–11 Those people are also more likely to only concentrate on evidence that is consistent with current hypotheses,12 ignoring information that is inconsistent with those hypotheses, thus exhibiting a form of confirmation bias. Confirmation bias can be described as the search for, and compilation of, evidence, information, and data that support a particular belief, and a simultaneous failure to adequately consider information indicating that the belief is incorrect; for instance, some people go to an exceptional length to validate (confirm) conclusions, but seldom attempt to disprove, refute, or falsify cherished beliefs.13,14 For such individuals, any effort to consider a different point of view may produce cognitive dissonance.15 The sensitivity to cognitive dissonance may contribute to this bias as an undesirable psychological state.16 Consequently, all new knowledge will more likely be interpreted through the lens of current belief systems, particularly when facing events that are not open to immediate explanation.
Many of the demographic variables assessed here directly or indirectly suggest the importance of education in countering this type of thinking. Individuals with higher levels of education, and who worked or studied in scientific or medical fields that require extensive education, were less likely to have misconceptions surrounding COVID-19 based on conspiracy theories. Moreover, the overview of people from these demographic groups could be considered to be more “rational,” in that their beliefs are more factually based, with both reduced optimism bias and pessimism bias. It may be that education itself makes individuals more open to considering new ideas, perhaps through exposure to the process of considering the causes of a problem by looking for facts that may disprove the initial belief. Alternatively, it may also be true that individuals without this capacity are less likely to succeed in an advanced educational setting, to attain higher levels of educational success, and, in particular, might be unlikely to succeed in medical or scientific fields.
Importantly, believers of conspiracy theories may find it hard to trust that a virus could originate naturally because of their predetermined view that events have a reason, and usually a human or government source that causes it. This idea was supported by the results from some of the individual questions that contributed to the conspiracy theory belief score, such as asking the participant “Is the virus lab made” or “Is the virus a lie.” Previous studies have indicated that conspiracy theories often develop from dissatisfaction. Thus, it is common to find that stronger conspiracy theory beliefs are linked to more negative attitudes toward government.17,18 This was supported in the present study, where we found that the highest means were associated between COVID-19 conspiracy theories and stronger confirmation of the belief that the government was hiding things from the public, doing things for its own interest (political reasons), and was too strict in its measures. These beliefs might affect the attitude and behavior toward COVID-19 in terms of protection against the virus. In that respect, a recent study conducted in Jordan about SARS-CoV-2 vaccination acceptance found that only 36% of the study sample were willing to take the vaccine.19
Other misconceptions are based on a common “optimism bias,” one version of which is the belief that bad things are less likely to happen to oneself than to others. Although optimism bias may be beneficial for avoiding negative emotions,20 it can lead individuals to underestimate the likelihood of catching a disease21 and to therefore disregard public health warnings.22 In this study, we found that optimism bias was the second most common type of misconception, and this might therefore contribute to the low number of COVID-19 cases among the Jordanian population during the period of May 2020 to June 2020. Importantly, the highest question means for COVID-19 optimism bias involved a strong belief that an antidote will be discovered soon, the virus will disappear with time, and the virus is not very dangerous. All of these beliefs might lead people to take the virus less seriously, and consequently make them less likely to follow the recommendations of public health agencies. Communication approaches must demonstrate a balance between breaking through optimism bias without inducing unwarranted feelings of nervousness, fear, and trepidation. Similar to misconceptions surrounding other issues, we found that a higher educational level and working or studying in a medical field decreased optimism bias. Educational level might affect awareness of the likelihood of catching a disease, making an individual more responsive to public health warnings and recommendations.
Accurate health decisions depend on precise insights into the costs and benefits of certain choices for oneself and for society,23,24 but risk perceptions are often influenced more by emotions than by factual information.25,26 Emotions focus the attention of individuals on particular types of information, like negative information when feeling afraid, resulting in differences in optimism and pessimism bias. Consequently, this biased information affects decisions in risky situations in ways that may not be optimal.27 As negative emotions elevate, individuals may rely on negative evidence about COVID-19 to form opinions more than other data. Importantly, in the event of robust emotional reactions, individuals may also disregard vital numeric information such as probabilities28 and a problem’s scope.29 Certain types of education may be particularly critical in this regard, such as those that require high degrees of mathematical understanding, such as medical or scientific fields. Information with negative emotional connotations captures attention, particularly for individuals who have weaker skills in mathematics or science in general,30 perhaps because they do not have other strategies for forming an understanding of the world. The media reports on COVID-19 are usually reported in a negative fashion—for example, by giving the number of people infected and those who die or who are in a critical condition, rather than as those who improve or experience only mild symptoms. This may intensify negative emotions and sensitize people to otherwise ignored risks for themselves or others. In this study, although the mean pessimism bias is not as high as other categories among the Jordanian population, further examination is still warranted to explore the influence of pessimism bias on COVID-19 attitudes. In addition, studies are needed to explore whether a more positive frame of mind could protect the public from the consequences of negative emotions without negatively affecting conformation to public health recommendations.31 In addition, in this study, we showed that older people, those with a higher educational level, and those working or studying in a medical-related field had a lower pessimism bias and magical beliefs. Although it is difficult to determine the reason for this effect of age, one might speculate that it is related to the other factors, for instance, that continued education and work experience lead to a greater understanding of the world. Also, in a broader sense, it might mean that maturity, and having more experience, may help individuals to form more accurate models of the world. On the other hand, this may also reflect differences across age-groups in the use of social media to acquire information and form a worldview. As is discussed in the following text, the use of social media has a substantial impact on misconceptions surrounding COVID-19.
Several sociological variables are also known to influence misconceptions toward COVID-19. One of these main effects is of gender. A previous study has shown that women are more likely to consider COVID-19 as a very serious health problem, to approve restrictive public policy measures adopted in response to it, and to submit to those measures.32 In this study, we found gender differences in misconceptions between men and women, where women have more misconceptions associated with conspiracy theories. Although this compliance with public health directives is positive, the root of this compliance, at least in part, in misconceptions about the disease may lead to other problems, particularly if it results from increased anxiety. Gender differences in attitudes and behavior toward COVID-19 may have important consequences on the spread of the pandemic, which may contribute to gender differences in vulnerability to COVID-19. These results are in accordance with other gender differences in the literature. For instance, women have been found to be more acquiescent33 and more compliant with rules.34,35 We also found that individuals with children have more misconceptions than individuals who do not have children. This result might be due to parents having more fear on behalf of their children, having less time for news, or it may be a covariant, whereby people with more education have children later than people with less education. Finally, individuals who live in urban regions, especially Amman, have fewer COVID-19 misconceptions. This might be due to several reasons, including covariates such as a lower educational level among people who live in rural areas than among those who live in urban areas, a smaller number of people who are either employed or a student in a medical field in rural areas, less likelihood of having attended a lecture on coronavirus in a rural area, or reduced access to reliable sources of information, like the WHO.
In this study, participants who used social media as a source of information had higher rates of misconceptions than participants who did not use social media as a source of information. This is consistent with a previous study showing that the use of social media as a source of COVID-19 information was connected to stronger beliefs in conspiracy theories and reduced conformity to public health advice during the pandemic.36 More than half of the people on social media have encountered information about the COVID-19 pandemic that appeared to them to be entirely made up.37 More than a quarter of the most watched videos related to COVID-19 on YouTube, the second most widely used social media site (second to Facebook), featured false statements about COVID-19, while garnering more than 62 million views.38 This obviously shows that social media is a major source of false beliefs about COVID-19. This led the WHO to strengthen its communication efforts to provide correct answers for rapidly circulating rumors that had been promulgated on social media channels. The WHO is also using search optimization techniques on social media networks to guide anyone asking questions about the pandemic toward credible sources.39 Likewise, when looking for updates on COVID-19 and other health-related problems, social media sites are starting to provide alerts or “warnings” with links to credible sources and fact-checkers.40
Based on the foregoing discussion, it might be thought that it would be very difficult to change public opinion if the causes of COVID-19 misconceptions are rooted in demographics—after all, individuals cannot really change their demographic groups. One of the more encouraging findings was that individuals who had viewed a lecture about coronavirus had a reduced number of misconceptions about COVID-19. This directly suggests that dissemination of public health information, in detail, leads to a reduction in misconceptions, and that although many demographic variables may be associated with COVID-19 misconceptions, public information campaigns can have meaningful and measurable positive effects.
In comparing the demographics of the study respondents with the overall demographics of Jordan, it is clear that this is not a fully representative sample. There were clearly more female respondents than males, and the overall cohort was more educated and more likely to be a student, especially in a scientific or medical field, than that general population. There may be several reasons for this, including the platforms through which the subjects were recruited, or that such individuals might have been more likely to respond to such a survey request. Furthermore, we recognize that nearly half of the sample was in the medical sector, either as students or workers (47.9%), which is one way that the sample differed from the overall population. It should be noted that the number of medical workers in Jordan is considerably higher than that in other nations worldwide. For example, Jordan is ranked 33rd in the healthcare sector in global ranking according to the Medical Tourism Index (60.2 healthcare workers per 10,000 people in the population).41 The authors believe that the medical staff's perception is especially interesting because their views can affect the general public, although this still constitutes a departure from the overall population. Despite these differences, the study still has substantial statistical power. Moreover, there were explicit comparisons across all of these demographic variables. Based on the clear demographic trends found in this study, if anything, the problem of misconceptions in the broader population may be even greater than that represented here, given that the broader population is probably less educated, less connected to the medical field, and more rural than the overall sample population. Another potential limitation of the present study is that interactions between different variables in the post hoc models were not assessed. Investigating these interactions would produce a very complex model that will be hard for the readers to follow as well as lacking sufficient statistical power, so would be best left to studies targeting specific interactions.
In conclusion, the findings of this study shed light on the causes of misconceptions toward COVID-19 in the Jordanian population. The results of this study could be used to set priorities in information campaigns on COVID-19 by public health authorities and the media. Information campaigns should be targeted toward people who have more COVID-19 misconceptions, namely, people with a lower educational level, younger age, and who are employed or studying in nonmedical and nonscientific fields. Through such campaigns, the public health authorities and media can target individuals who have been less likely to follow public health recommendations due to conflicting belief systems. Reducing their misconceptions may lead them to focus their attention on prevention measures that are most effective, such as the use of surgical masks, frequent and thorough handwashing, social distancing, and avoiding close contact with people who are sick. Furthermore, more awareness lectures should be offered to the public through the nonsocial media and social media platforms to fight misconceptions toward this pandemic, as these may reach a broader demographic range of the Jordanian population.
Supplemental Appendix and tables
ACKNOWLEDGMENT
The American Society of Tropical Medicine and Hygiene has waived the Open Access fee for this article due to the ongoing COVID-19 pandemic and has assisted with publication expenses.
Note: Supplemental appendix appears at www.ajtmh.org.
REFERENCES
- 1.Kucharski AJ, Klepac P, Conlan A, Kissler SM, Tang ML, Fry H, Gog JR, Edmunds WJ; CMMID COVID-19 working Group , 2020. Effectiveness of isolation, testing, contact tracing and physical distancing on reducing transmission of SARS-CoV-2 in different settings. Lancet Infect Dis 20: 1151–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Tammemi AB, 2020. The battle against COVID-19 in Jordan: an early overview of the Jordanian experience. Front Public Health 8: 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samrah SM, Al-Mistarehi AHW, Ibnian AM, Raffee LA, Momany SM, Al-Ali M, Hayajneh WA, Yusef DH, Awad SM, Khassawneh BY, 2020. COVID-19 outbreak in Jordan: epidemiological features, clinical characteristics, and laboratory findings. Ann Med Surg 57: 103–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khasawneh AI, et al. 2020. Medical students and COVID-19: knowledge, attitudes, and precautionary measures. A descriptive study from Jordan. Front Public Health 8: 253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tasnim S, Hossain MM, Mazumder H, 2020. Impact of rumors and misinformation on COVID-19 in social media. J Prev Med Public Health 53: 171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pennycook G, McPhetres J, Bago B, Rand D, 2020. Predictors of attitudes and misperceptions about COVID-19 in Canada, the UK, and the USA. PsyArXiv 10: 1–25. [Google Scholar]
- 7.Sutton RM, Douglas KM, 2020. Conspiracy theories and the conspiracy mindset: implications for political ideology. Curr Opin Behav Sci 34: 118–122. [Google Scholar]
- 8.Swami V, Barron D, Weis L, Voracek M, Stieger S, Furnham A, 2017. An examination of the factorial and convergent validity of four measures of conspiracist ideation, with recommendations for researchers. PLoS One 12: e0172617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Georgiou N, Delfabbro P, Balzan R, 2019. Conspiracy beliefs in the general population: the importance of psychopathology, cognitive style and educational attainment. Pers Individ Diff 151: 109521. [Google Scholar]
- 10.van Prooijen JW, Douglas KM, 2018. Belief in conspiracy theories: basic principles of an emerging research domain. Eur J Soc Psychol 48: 897–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Prooijen JW, Douglas KM, De Inocencio C, 2018. Connecting the dots: illusory pattern perception predicts belief in conspiracies and the supernatural. Eur J Soc Psychol 48: 320–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balzan R, Delfabbro P, Galletly C, Woodward T, 2012. Reasoning heuristics across the psychosis continuum: the contribution of hypersalient evidence–hypothesis matches. Cogn Neuropsych 17: 431–450. [DOI] [PubMed] [Google Scholar]
- 13.Oswald ME, Grosjean S, 2004. Confirmation Bias. Cognitive Illusions: A Handbook on Fallacies and Biases in Thinking, Judgement and Memory. 79. [Google Scholar]
- 14.Glick M, 2017. Believing is seeing: confirmation bias. J Am Dental Assoc 148: 131–132. [DOI] [PubMed] [Google Scholar]
- 15.Festinger L, 2017. Cognitive dissonance. Sci Am 207: 93–106. [DOI] [PubMed] [Google Scholar]
- 16.Steindl C, Jonas E, Sittenthaler S, Traut-Mattausch E, Greenberg J, 2015. Understanding psychological reactance. Z für Psychol 223: 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Prooijen JW, 2017. Why education predicts decreased belief in conspiracy theories. Appl Cognitive Psychology 31: 50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Prooijen JW, Van Lange PA, 2014. Power, Politics, and Paranoia: Why People Are Suspicious of Their Leaders. Cambridge, UK: Cambridge University Press. [Google Scholar]
- 19.Al-Qerem WA, Jarab AS, 2021. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front Public Health 9: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Strunk DR, Lopez H, DeRubeis RJ, 2006. Depressive symptoms are associated with unrealistic negative predictions of future life events. Behav Research Therapy 44: 861–882. [DOI] [PubMed] [Google Scholar]
- 21.Sharot T. The optimism bias. Curr Biol 21: R941–R945. [DOI] [PubMed] [Google Scholar]
- 22.Wise T, Zbozinek TD, Michelini G, Hagan CC, 2020. Changes in risk perception and protective behavior during the first week of the COVID-19 pandemic in the United States. R Soc Open Sci 7: 200742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fischhoff B, 2013. The sciences of science communication. Proc Natl Acad Sci U S A 110 (Suppl 3): 14033–14039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slovic P, 1987. Perception of risk. Science 236: 280–285. [DOI] [PubMed] [Google Scholar]
- 25.Slovic P, Finucane ML, Peters E, MacGregor DG, 2004. Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Anal Int J 24: 311–322. [DOI] [PubMed] [Google Scholar]
- 26.Loewenstein GF, Weber EU, Hsee CK, Welch N, 2001. Risk as feelings. Psychol Bulletin 127: 267–286. [DOI] [PubMed] [Google Scholar]
- 27.Peters E, Lipkus I, Diefenbach MA, 2006. The functions of affect in health communications and in the construction of health preferences. J Communication 56: S140–S162. [Google Scholar]
- 28.Rottenstreich Y, Hsee CK, 2001. Money, kisses, and electric shocks: on the affective psychology of risk. Psychol Sci 12: 185–190. [DOI] [PubMed] [Google Scholar]
- 29.Hsee CK, Rottenstreich Y, 2004. Music, pandas, and muggers: on the affective psychology of value. J Exp Psychol Gen 133: 23. [DOI] [PubMed] [Google Scholar]
- 30.Peters E, Västfjäll D, Slovic P, Mertz C, Mazzocco K, Dickert S, 2006. Numeracy and decision making. Psychol Sci 17: 407–413. [DOI] [PubMed] [Google Scholar]
- 31.Van Bavel JJ, et al. 2020. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 4: 460–471. [DOI] [PubMed] [Google Scholar]
- 32.Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M, 2020. Gender differences in COVID-19 related attitudes and behavior: evidence from a panel survey in eight OECD countries . Proc Natl Acad Sci U S A 117: 27285–27291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bouchard TJ, Loehlin JC, 2001. Genes, evolution, and personality. Behav Genetics 31: 243–273. [DOI] [PubMed] [Google Scholar]
- 34.Tittle CR, 1980. Sanctions and Social Deviance: The Question of Deterrence, 45–60. [Google Scholar]
- 35.Torgler B, 2007. Tax Compliance and Tax Morale: A Theoretical and Empirical Analysis. Cheltenham, UK: Edward Elgar Publishing. [Google Scholar]
- 36.Allington D, Duffy B, Wessely S, Dhavan N, Rubin J, 2020. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol Med 20: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jurkowitz M, Mitchell A, 2020. Americans Who Primarily Get News through Social Media Are Least Likely to Follow COVID-19 Coverage, Most Likely to Report Seeing Made-Up News. Washington, DC: Pew Research Center. [Google Scholar]
- 38.Li HOY, Bailey A, Huynh D, Chan J, 2020. YouTube as a source of information on COVID-19: a pandemic of misinformation? BMJ Glob Health 5: e002604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zarocostas J, 2020. How to fight an infodemic. Lancet 395: 676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xue J, Chen J, Hu R, Chen C, Zheng C, Su y, Zhu T, 2020. Twitter discussions and emotions about the COVID-19 pandemic: machine learning approach. J Med Internet Res 22: e20550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.2018. Health Care Sector Profile. Available at: https://www.jic.gov.jo/wp-content/uploads/2018/12/Healthcare-Sector-Profile.pdf. Accessed October 10, 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.