Abstract
Hypothesis
Three-dimensional (3D) printed temporal bones are comparable to cadaveric temporal bones as a training tool for otologic surgery.
Background
Cadaveric temporal bone dissection is an integral part of otology surgical training. Unfortunately, availability of cadaveric temporal bones is becoming much more limited and concern regarding chemical and biological risks persist. In this study, we examine the validity of 3D-printed temporal bone model as an alternative training tool for otologic surgery.
Methods
Seventeen otolaryngology trainees participated in the study. They were asked to complete a series of otologic procedures using 3D-printed temporal bones. A semi-structured questionnaire was used to evaluate their dissection experience on the 3D-printed temporal bones.
Results
Participants found that the 3D-printed temporal bones were anatomically realistic compared to cadaveric temporal bones. They found that the 3D-printed temporal bones were useful as a surgical training tool in general and also for specific otologic procedures. Overall, participants were enthusiastic about incorporation of 3D-printed temporal bones in temporal bone dissection training courses and would recommend them to other trainees.
Conclusion
3D-printed temporal bone model is a viable alternative to human cadaveric temporal bones as a teaching tool for otologic surgery.
Keywords: Temporal bone, Otologic surgery, 3D-printing, 3D-printed temporal bone, Surgical training, Surgical simulation
Introduction
The anatomy of the temporal bone is amongst the most complex in the human body. In order to master this anatomy, otologic surgeons in training are required to spend many hours in the temporal bone lab, learning to dissect human cadaveric temporal bones. Fortunately, the human cadaveric temporal bone is a highly realistic model which allows trainees to practice most otologic/neurotologic procedures to acquire basic levels of competence and safety prior to further skill development under supervision in patients. Despite their usefulness as a training tool, human cadaveric temporal bones have several significant drawbacks: (1) Human cadaveric temporal bones carry the risk of disease transmission. When donors are improperly screened, working with human cadaveric temporal bones carries the risk of contracting diseases such as hepatitis B and Creutzfeldt-Jakob disease (CJD).1 (2) Human cadaveric temporal bones have a finite “shelf life”. They need to be carefully packaged and stored in refrigeration in order to delay the decay of cadaveric tissues. (3) Human cadaveric temporal bones are difficult and expensive to obtain. The cost of maintaining a lab for harvesting cadaveric temporal bone is expensive, and the supply is diminishing.1 In many countries, it is difficult to obtain human cadaveric temporal bones to practice otologic surgical procedures.1 Given these drawbacks, there has been many efforts to find valid alternatives to human cadaveric temporal bones which can provide trainees a realistic surgical dissection experience.
In a previous study, we reported the validity of a three-dimensional (3D) printed synthetic temporal bone model for surgical training in a cohort of final-year surgical trainees in Australia and New Zealand.2 We found that the synthetic temporal bone model provided a realistic dissection experience for trainees that is comparable to human cadaveric temporal bones. In this study, we examine the validity of this 3D printed synthetic temporal bone model for otologic surgical training in a group of trainees from one program in the United States of America.
Materials and methods
Three-dimensional printed synthetic temporal bone model
The 3D-printed temporal bone model used in this study is manufactured by Phacon GmbH (Leipzig, Germany). The details of the development of this synthetic temporal bone model was previously described in detail.2 Briefly, it was developed based on data acquired by micro CT images of normal human cadaveric temporal bone (12 μm resolution). The bone is constructed using a cast powder and a bonding agent with similar properties to human cadaveric bones. Color was added to different anatomic structures (e.g. facial nerve, carotid artery, sigmoid sinus) to increase the realism of the model.
Temporal bone dissection evaluation
Seventeen otolaryngology residents from the Johns Hopkins Otolaryngology training program participated in the study. All residents that participated in the study had some otological surgical experiences at the time of the study. The participants were asked to perform a series of otologic procedures, beginning with cortical mastoidectomy, epitympanectomy, posterior tympanotomy, cochleostomy/round window surgery, canalplasty, canal wall down mastoidectomy, labyrinthectomy, and temporal bone resection. This was done as a part of a temporal bone instruction course, which took place in four sessions, each lasting ~2 h. Prior to each dissection session, there was a 30-min lecture on various aspects of otologic surgery. Following the conclusion of the instruction course, each resident received feedback from attending surgeons at the institution regarding dissection performance.
Evaluation survey
Immediately following the completion of the temporal bone dissection course, the trainees were asked to complete a de-identified survey on their experiences with the 3D-printed synthetic bones. The survey consists of 23 questions grouped into four domains: anatomical realism, task-based usefulness, usefulness as a training tool, and overall reactions.2 The answers were scaled using a five point system, varying from strongly agreeing (5), agreeing (4), neutral (3), disagreeing (2), to strongly disagreeing (1). A score of 3 indicated that the 3D-printed synthetic bone was an acceptable alternative to cadaveric human temporal bones; scores of less than 3 indicated that the 3D-printed synthetic bone was a poor substitute for cadaveric temporal bones. Scores of 4 and higher indicated that the 3D-printed synthetic bone was an excellent substitute for human cadaveric temporal bones.
Results
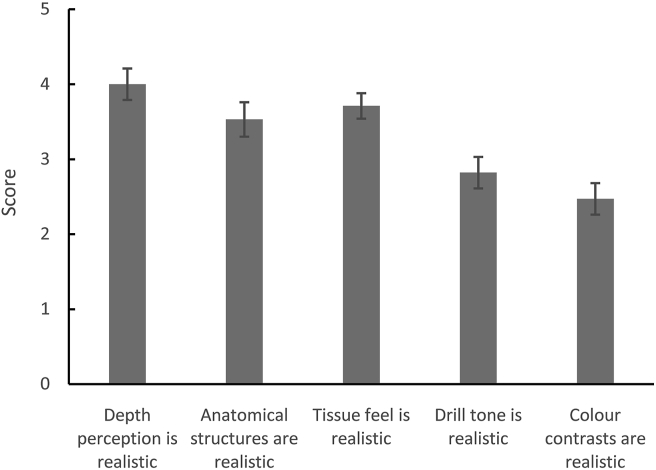
The seventeen otolaryngology residents that participated in the study were in different stages of their training, from PGY2 to PGY7 (4 residents took part in the T32 research grant which added two additional years to their residency training). The survey data are shown in Table 1. When evaluating the anatomic realism of the 3D-printed temporal bones (Fig. 1), participants felt that the depth perception (mean ± SE: 4.00 ± 0.21), tissue feel (3.71 ± 0.17), and anatomic structures (3.53 ± 0.23) were realistic compared to cadaveric temporal bones. The drill tone (2.82 ± 0.21)and color contrast (2.47 ± 0.21) were felt to be less realistic than cadaveric temporal bones.
Table 1.
The survey data of dissection experience on the 3D-printed temporal bones.
| Domain | Subdomain | Reponses (n) | Mean score | SE |
|---|---|---|---|---|
| Anatomical realism | Depth perception is realistic | 17 | 4.00 | 0.21 |
| Anatomical structures are realistic | 17 | 3.53 | 0.23 | |
| Tissue feel is realistic | 17 | 3.71 | 0.17 | |
| Drill tone is realistic | 17 | 2.82 | 0.21 | |
| Color contrasts are realistic | 17 | 2.47 | 0.21 | |
| Usefulness as a training tool | Useful for teaching anatomy | 17 | 4.59 | 0.15 |
| Useful for teaching surgical planning | 17 | 4.53 | 0.15 | |
| Useful for improving hand-eye coordination | 17 | 4.59 | 0.15 | |
| Useful as an overall training tool | 17 | 4.65 | 0.12 | |
| Useful for improving operative technique | 17 | 4.35 | 0.21 | |
| Task-based usefulness | Useful for teaching cortical mastoidectomy | 17 | 4.59 | 0.12 |
| Useful for teaching atticotomy | 15 | 3.87 | 0.19 | |
| Useful for teaching facial recess dissection | 15 | 3.73 | 0.23 | |
| Useful for teaching round window surgery | 15 | 3.47 | 0.22 | |
| Useful for teaching canalplasty | 15 | 3.33 | 0.27 | |
| Useful for teaching wall down mastoidectomy | 15 | 4.13 | 0.19 | |
| Useful for teaching labyrinthectomy | 15 | 3.87 | 0.22 | |
| Useful for teaching temporal bone resection | 15 | 3.33 | 0.23 | |
| Overall reactions | I would recommend this model to other trainees | 16 | 4.25 | 0.19 |
| Working with synthetic 3D bones will help me feel more confident performing procedures in operating theatre | 16 | 4.19 | 0.21 | |
| This 3D printed synthetic temporal bone model should be incorporated into training curriculum | 16 | 4.19 | 0.21 | |
| Skills leaned on course are transferable to operating theatre | 16 | 4.19 | 0.19 | |
| Working with synthetic 3D bone was as useful as working with traditional frozen or formalinised cadaveric bones | 16 | 3.19 | 0.28 |
Fig. 1.
Ratings for questions regarding the anatomic realism of the 3D-printed temporal bone models. The mean and standard errors are shown.
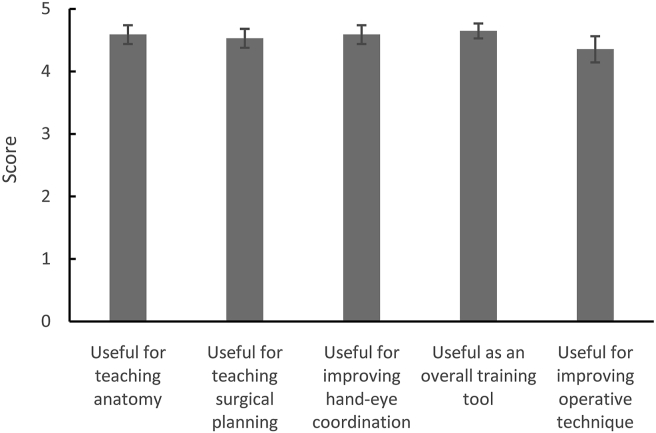
In terms of the usefulness of the 3D-printed temporal bones as a training tool (Fig. 2), the participants found that the synthetic model was a useful tool for teaching temporal bone anatomy (4.59 ± 0.15), surgical planning (4.53 ± 0.15), and improving operative techniques (4.35 ± 0.21). Interestingly, most participants found that working on the 3D-printed temporal bones was useful for improving hand-eye coordination (4.59 ± 0.15). Overall, participants found the 3D-printed temporal bones to be a useful training tool (4.65 ± 0.12).
Fig. 2.
Ratings for questions regarding the usefulness of the 3D-printed temporal bone model as a training tool. The mean and standard errors are shown.
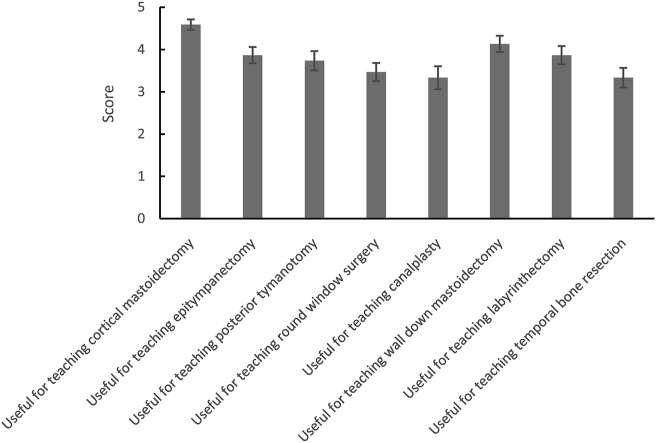
When the participants were asked to rate their experiences with the 3D-printed temporal bones on specific otologic procedures (Fig. 3), cortical mastoidectomy received the highest rating as being most realistic compared to cadaveric temporal bones (4.59 ± 0.12), followed by canal wall down mastoidectomy (4.13 ± 0.19), atticotomy (3.87 ± 0.19), labyrinthectomy (3.87 ± 0.22), round window surgery (3.47 ± 0.22), canalplasty (3.33 ± 0.27) and temporal bone resection (3.33 ± 0.23).
Fig. 3.
Ratings for questions regarding the usefulness of the 3D-printed temporal bone model for specific otologic procedures. The mean and standard errors are shown.
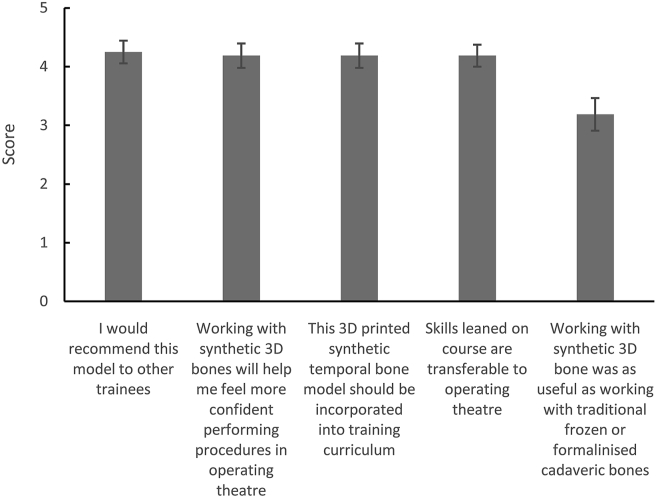
The overall impression of working with the 3D-printed temporal bones was very positive (Fig. 4). Participants felt that the techniques they learned working with the 3D-printed bones were transferable to the operating room (4.19 ± 0.19) and that working with these synthetic bones helped them feel more confident performing otologic procedures in the operating room (4.19 ± 0.21). Even though participants were neutral when asked about whether working with the 3D-printed temporal bones was as useful as working with cadaveric bones (3.19 ± 0.28), most participants felt that the 3D-printed temporal bones should be incorporated into the temporal bone dissection training curriculum (4.19 ± 0.21), and that they would recommend the 3D-printed temporal bones to other trainees (4.25 ± 0.19).
Fig. 4.
Ratings for questions regarding the overall reactions the trainees had after working with 3D-printed temporal bones. The mean and standard errors are shown.
Discussion
Working with human cadaveric temporal bones provides an invaluable experience to otologic surgeons in training. The cadaveric temporal bone is a highly realistic model for trainees to learn otologic/neurotologic procedures without putting patients at risk. In a study examining the usefulness of cadaveric temporal bone dissection in improving surgeon competency for singular neurectomy, Feigl et al3 found that repeated practice on cadaveric temporal bones improved the surgeon’s ability to accurately identify the posterior ampullary nerve. Furthermore the acquisition of mastoidectomy skills can be measured in the temporal bone laboratory, and overall competence is strongly correlated with increasing facility with specific procedural tasks.
Despite its importance in otological surgical training, human cadaveric temporal bones have several important drawbacks. Because of the risk of disease transmission, shortage of supply, as well as the ethical and financial concerns related to temporal bone harvesting, it is becoming increasingly difficult to obtain human cadaveric temporal bones. As a result, many trainees have to travel a great distance to attend temporal bone dissection courses in order to progress their otologic surgical development.
To overcome the problems associated with human cadaveric temporal bones, many investigators have attempted to find alternative models which can potentially substitute cadaveric temporal bones in otology surgical training. One example is the development of virtual reality (VR) technology for temporal bone dissection training.4, 5, 6, 7, 8, 9 The VR system usually consists of high-resolution CT images loaded onto a computer terminal, which generates a virtual temporal bone. This is usually coupled to a haptic device which serves as an otologic drill for dissection. In a randomized controlled multicenter study comparing surgical training results between cadaveric temporal bones and VR temporal bones, Wiet et al6 found that the otologic dissection performance was similar between trainees who underwent dissection training using cadaveric temporal bones vs. VR temporal bones. The main advantage of VR temporal bone is the fact that one could upload any patient’s temporal bone CT images to the computer system and generate a VR temporal bone model of that patient. This allows the surgeon the opportunity to perform any planned otologic operation on the VR temporal bone model prior to performing the operation on the actual patient, which is invaluable for surgical planning and rehearsal. However, in a study examining the face and content validation of a VR temporal bone model, using a similar questionnaire as that in the current study, Arora et al4 found that the realism of a VR temporal bone model is suboptimal compared to the cadaveric temporal bone.
Given the limitation of VR temporal bone models at providing haptic feedback, investigators have examined the use of 3D-printed temporal bones as an alternative. Three-dimensional printing technology has been applied widely in the medical and surgical fields over the past few years. Several studies have reported the use of 3D-printed temporal bones in various applications, including patient education, pre-surgical planning, and surgical dissection training.2,10, 11, 12, 13, 14 Various manufacturing techniques have been used to make the 3D-printed temporal bones as realistic as possible.15 In a study by Hochman et al,11 dissections on cadaveric temporal bones vs. 3D-printed bones were compared in a group of surgical trainees. The 3D-printed temporal bones used in the study were made of composite powder base, similar to the 3D-printed bones used in the current study. Participants in the study found that 3D-printed temporal bones were very similar to cadaveric temporal bones and provided a viable alternative for temporal bone dissection training.11 The safety of drilling on 3D-printed temporal bones was assessed in a study by Freiser et al,16 and it was shown that drilling on 3D-printed temporal bones was safe by Occupational Safety and Health Administration (OSHA) standards.
In the current study, the face and content validation of a 3D-printed temporal bone model was evaluated. Participants in this study found the 3D-printed temporal bones to be anatomically realistic compared to human cadaveric temporal bones. They also found the 3D-printed temporal bones to be very useful as a training tool for various otologic procedures. Most participants stated that the 3D-printed temporal bones should be incorporated into temporal bone dissection training curriculum and that they would recommend the 3D-printed temporal bone model to other trainees. These results are similar to our previous study in a different cohort.2 In our previous study, a group of nine Australian otolaryngology residents near completion of residency training participated in the study. The current study involved otolaryngology residents from a US training program in all training levels. Both studies have shown that the 3D-printed temporal bone model is a valuable training tool for learning otologic procedures.
Currently there are only a limited number of available temporal bone models made by Phacon which poses a disadvantage to surgical training compared to human cadaveric temporal bones, which offers the benefit of anatomic variations. Despite this limitation, the 3D-printed temporal bone is an easily accessible model that allows trainees to gain basic otologic technical skills and can be used as an adjunct training tool along with human cadaveric temporal bones. The limitations of this study include the small sample size as well as the inability to randomize exposure to cadaveric versus synthetic temporal bones. Despite these limitations, our study demonstrated that 3D-printed temporal bone is a highly useful otologic teaching tool when surveyed among two different groups of trainees with vastly different backgrounds, and it is a viable alternative in places where cadaveric temporal bones may not be readily available.
Conclusions
Three-dimensional printed temporal bone model is an attractive alternative to cadaveric temporal bones as an otology surgical training tool. It is cheaper, safer, cleaner to use, and easier to obtain compared to cadaveric temporal bones. Our study showed that 3D-printed temporal bones provided an anatomically realistic dissection experience for trainees and that they are highly useful as a teaching tool for otologic procedures. It is our hope that the 3D-printed temporal bones will enable more otolaryngology training programs around the world to provide temporal bone dissection opportunities to their trainees.
Declaration of competing interest
The authors have no conflict of interest to report.
Acknowledgement
We would like to thank Dr. Mohamed Lehar for his help with organizing the temporal bone laboratory at Johns Hopkins Hospital. We also thank the otolaryngology residents who participated in this study.
Edited by Xin Jin
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Naik S.M., Naik M.S., Bains N.K. Cadaveric temporal bone dissection: is it obsolete today. Int Arch Otorhinolaryngol. 2014;18:63–67. doi: 10.1055/s-0033-1351681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Da Cruz M.J., Francis H.W. Face and content validation of a novel three-dimensional printed temporal bone for surgical skills development. J Laryngol Otol. 2015;129(Suppl 3):S23–S29. doi: 10.1017/S0022215115001346. [DOI] [PubMed] [Google Scholar]
- 3.Feigl G., Kos I., Anderhuber F., Guyot J.P., Fasel J. Development of surgical skill with singular neurectomy using human cadaveric temporal bones. Ann Anat. 2008;190:316–323. doi: 10.1016/j.aanat.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Arora A., Khemani S., Tolley N. Face and content validation of a virtual reality temporal bone simulator. Otolaryngol Head Neck Surg. 2012;146:497–503. doi: 10.1177/0194599811427385. [DOI] [PubMed] [Google Scholar]
- 5.Andersen S.A., Cayé-Thomasen P., Sørensen M.S. Mastoidectomy performance assessment of virtual simulation training using final-product analysis. Laryngoscope. 2015;125:431–435. doi: 10.1002/lary.24838. [DOI] [PubMed] [Google Scholar]
- 6.Wiet G.J., Stredney D., Kerwin T. Virtual temporal bone dissection system: OSU virtual temporal bone system: development and testing. Laryngoscope. 2012;122(Suppl 1):S1–S12. doi: 10.1002/lary.22499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Leary S.J., Hutchins M.A., Stevenson D.R. Validation of a networked virtual reality simulation of temporal bone surgery. Laryngoscope. 2008;118:1040–1046. doi: 10.1097/MLG.0b013e3181671b15. [DOI] [PubMed] [Google Scholar]
- 8.Morris D., Sewell C., Barbagli F., Salisbury K., Blevins N.H., Girod S. Visuohaptic simulation of bone surgery for training and evaluation. IEEE Comput Graph Appl. 2006;26:48–57. doi: 10.1109/mcg.2006.140. [DOI] [PubMed] [Google Scholar]
- 9.Jackson A., John N.W., Thacker N.A. Developing a virtual reality environment in petrous bone surgery: a state-of-the-art review. Otol Neurotol. 2002;23:111–121. doi: 10.1097/00129492-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Cohen J., Reyes S.A. Creation of a 3D printed temporal bone model from clinical CT data. Am J Otolaryngol. 2015;36:619–624. doi: 10.1016/j.amjoto.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Hochman J.B., Rhodes C., Kraut J., Pisa J., Unger B. End User comparison of anatomically matched 3-dimensional printed and virtual haptic temporal bone simulation: a pilot study. Otolaryngol Head Neck Surg. 2015;153:263–268. doi: 10.1177/0194599815586756. [DOI] [PubMed] [Google Scholar]
- 12.Mowry S.E., Jammal H., Myer C., 4th, Solares C.A., Weinberger P. A novel temporal bone simulation model using 3D printing techniques. Otol Neurotol. 2015;36:1562–1565. doi: 10.1097/MAO.0000000000000848. [DOI] [PubMed] [Google Scholar]
- 13.Rose A.S., Webster C.E., Harrysson O.L., Formeister E.J., Rawal R.B., Iseli C.E. Pre-operative simulation of pediatric mastoid surgery with 3D-printed temporal bone models. Int J Pediatr Otorhinolaryngol. 2015;79:740–744. doi: 10.1016/j.ijporl.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Rose A.S., Kimbell J.S., Webster C.E., Harrysson O.L., Formeister E.J., Buchman C.A. Multi-material 3D models for temporal bone surgical simulation. Ann Otol Rhinol Laryngol. 2015;124:528–536. doi: 10.1177/0003489415570937. [DOI] [PubMed] [Google Scholar]
- 15.Crafts T.D., Ellsperman S.E., Wannemuehler T.J., Bellicchi T.D., Shipchandler T.Z., Mantravadi A.V. Three-dimensional printing and its applications in otorhinolaryngology-head and neck surgery. Otolaryngol Head Neck Surg. 2017;156:999–1010. doi: 10.1177/0194599816678372. [DOI] [PubMed] [Google Scholar]
- 16.Freiser M.E., Ghodadra A., Hart L., Griffith C., Jabbour N. Safety of drilling 3-dimensional-printed temporal bones. JAMA Otolaryngol Head Neck Surg. 2018;144:797–801. doi: 10.1001/jamaoto.2018.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]