Abstract
Deficits in executive control functions are some of the most common and disabling consequences of both military and civilian brain injury. However, effective interventions are scant. The goal of this study was to assess whether cognitive rehabilitation training that was successfully applied in chronic civilian brain injury would be effective for military veterans with traumatic brain injury (TBI). In a prior study, participants with chronic acquired brain injury significantly improved after training in Goal-Oriented Attentional Self-Regulation (GOALS) on measures of attention/executive function, functional task performance, and goal-directed control over neural processing on functional magnetic resonance imaging. The objective of this study was to assess effects of GOALS training in veterans with chronic TBI. A total of 33 veterans with chronic TBI and executive difficulties in their daily life completed either 5 weeks of manualized GOALS training or Brain-Health Education (BHE) matched by time and intensity. Evaluator-blinded assessments at baseline and post-training included neuropsychological and complex functional task performance and self-report measures of emotional regulation. After GOALS, but not BHE training, participants significantly improved from baseline on primary outcome measures of Overall Complex Attention/Executive Function composite neuropsychological performance score (F = 7.10, p = 0.01; partial η2 = 0.19), and on overall complex functional task performance (Goal Processing Scale Overall Performance; F = 6.92, p = 0.01, partial η2 = 0.20). Additionally, post-GOALS participants indicated significant improvement on emotional regulation self-report measures (Profile of Mood States Confusion Score; F = 6.05, p = 0.02, partialη2 = 0.20). Training in attentional self-regulation applied to participant-defined goals may improve cognitive functioning in veterans with chronic TBI. Attention regulation training may not only impact executive control functioning in real-world complex tasks, but also may improve emotional regulation and functioning. Implications for treatment of veterans with TBI are discussed.
Keywords: : cognitive rehabilitation, traumatic brain injury, veterans
Introduction
Traumatic brain injury (TBI) and co-morbid conditions are prevalent in veterans from the Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn conflicts,1–4 with the reported rates ranging from 14–22%.1,2 TBI and associated conditions also are common among veterans of the Vietnam and Gulf War eras.5–7 Chronic sequela of TBI, including deficits in attention, executive functions, and memory, can be highly debilitating.8,9 Deficits in these cognitive control functions have been linked with difficulties in community reintegration and educational and occupational functioning, and are some of the leading causes of long-term disability among veterans.1–4,10 Reintegration difficulties are a common problem among returning veterans with mild TBI: A recent study reported that 1 year post-deployment, 65% of returning veterans with history of mild TBI (mTBI) sought treatment for concerns related to reintegration.11 Similarly, a study by Mac Donald and colleagues12 found that 5 years post-deployment, veterans with history of combat-related blast mTBI had significantly worse neurobehavioral and psychiatric symptom severity, global disability, and sleep impairment, compared with combat veterans without history of TBI.
Recovery from military-related TBI may be complicated by several factors that differentiate it from civilian TBI,13 including the emotionally and physically traumatic circumstances in which injuries are sustained and high incidence of comorbid mental health conditions such as post-traumatic stress disorder (PTSD) and depression. Military-related TBI, PTSD, and depression may have both independent and additive roles in impacting cognition and daily functioning.14 Features of each may interact at multiple levels to reduce functioning and/or interfere with treatment effectiveness, including at the genesis of injury, the maintenance of symptoms, different aspects of cognitive-emotional functioning, and at the level of neural mechanisms.15,16 Sequela of military TBI and comorbid conditions such as PTSD can include disruption of core cognitive and emotional regulation mechanisms that are essential for goal-directed functioning in daily life.
Emotional regulation is also known to be negatively impacted by TBI.17,18 PTSD and depression are highly comorbid with TBI, especially in a veteran population.19 Problems with planning and response inhibition, aspects of cognitive function, contribute to emotional regulation difficulties, as well.20 There is a great deal of overlap between executive control functions and emotional regulation. In fact, the modulation of emotional responses is considered an aspect of executive function, an area of cognition disproportionately affected by TBI. Therefore, it follows logically that treatments targeted at executive control functions also may have a positive impact on emotional regulation for TBI patients.
Interventions that target cognitive and emotional self-regulatory functions may be particularly valuable in treating combat-related TBI.15 In particular, interventions that strengthen goal-directed cognitive control functions, such as the selection of goal-relevant information, along with inhibition of distracting information, may be helpful for improving those functionally important and integrated aspects of self-regulation that contribute to goal attainment. Training in mindfulness is one such promising approach. A recent study illustrated that a modified mindfulness-based stress reduction training program, Mindfulness-Based Mind Fitness Training, may help healthy military reservists preparing for deployment to regulate their emotions by improving self-regulation.21 Although this general approach holds promise, there has been little research and development of applied interventions that target executive control functioning for military-related TBI.
The overall objective of this study was to determine whether a training intervention for goal-oriented attentional self-regulation that has been successfully applied in individuals with chronic civilian brain injury22,32 would be effective for military veterans with history of chronic TBI. Goal-Oriented Attentional Self-Regulation (GOALS) is a cognitive rehabilitation training that targets executive control functions by training participants in applied mindfulness-based attention regulation and goal management strategies.22,23 In contrast to training via practice on isolated tasks, this training protocol involves application of attention regulation skills and strategies to participant-defined goals in their own lives and community in ecologically valid settings. One of the main training aims is to improve self-regulatory control mechanisms as they contribute to goal attainment.
Two lines of theory and research converged to identify target processes for this intervention. (For a more detailed review, see Novakovic-Agopian and colleagues.22) First, information processing from perception to action requires mechanisms for selecting goal-relevant information, as well as maintenance and protection of this information from disruption during working memory, learning, decision-making, and/or problem-solving.24 If one cannot hold key information active in mind or protect it from distractions, then subsequent actions are less likely to be effectively guided towards goal attainment. Second, many individuals with executive control difficulties show an overall “life disorganization” or “goal neglect,” with poor ability to manage and attain goals, even when they may be able to describe their intentions at the outset.25,26 Selective maintenance of goal-related information and protection from both internal (e.g., feeling anxious) and external disruptions are important for establishing and following sequences of steps (sub-goals) required to accomplish the goal. Therefore, intervening in these processes may help to ameliorate symptoms of goal neglect.
The GOALS protocol was based on training interventions that have been applied to patients with brain injury,27,28 and includes meta-cognitive goal management strategies outlined in Goal Management Training, with special emphasis on mindfulness-based attention regulation strategies applied to progressively more challenging daily life situations and goals. Cognitive and emotional issues are addressed as they become important in achieving personal goals. An overarching hypothesis is that improving attention regulation while engaging in goal-directed behavior will help establish more efficient and better integrated functional networks for the performance of goal-relevant tasks, and ultimately, goal attainment in real life contexts.
In our prior study, predominantly civilian patients with chronic acquired brain injury significantly improved after GOALS, but not after a brief control intervention, on neurocognitive measures of attention/executive function and memory, complex functional task performance, and goal-directed control over neural processing on functional magnetic resonance imaging (fMRI).22,32 One limitation of our previous study was that the brief control intervention was not matched to GOALS with respect to time. For the current study, we have developed a new time- and intensity-matched active comparison training. Brain Health Education (BHE) includes education about brain anatomy and functioning and effects of brain injury, as per current Veterans Affairs (VA) practice recommendations for mTBI treatment. However, BHE does not include the training in attention regulation and problem solving or the assistance in linking the information provided to participants' daily lives that is integral to GOALS training.
The objective of the current study was to assess the effects of GOALS training versus an active time-matched BHE intervention in military veterans with history of chronic TBI and difficulties in executive function in their daily lives. We tested whether GOALS training would lead to greater improvements on the multiple levels of executive functioning it is hypothesized to target—specifically, performance on neurocognitive measures of attention and executive function and on complex functional tasks. We aimed to compare the effects of two trainings (Aim A), as well as to evaluate the effectiveness of each training in improving neurocognitive and complex functional task performance (Aim B). Given the prevalence of psychiatric co-morbidity in this population, secondary objectives included comparison of the effects of the two trainings (Aim C), and assessment of the impact of each training on emotional adjustment (Aim D). fMRI measures were also collected and will be reported in a separate manuscript.
Methods
Design and participants
This study was approved by the Institutional Review Boards at participating institutions including University of California San Francisco, San Francisco VA Medical Center, and VA Northern California Health Care System (VANCHS) Martinez. All participants provided informed consent prior to any of the study procedures taking place. Behavioral assessments and interventions took place at VA medical centers in San Francisco and Martinez.
A total of 33 veterans of the Vietnam, Gulf War, and OEF/OIF eras with history of chronic TBI completed the study. Participants were primarily recruited from San Francisco VA and VANCHS-Martinez TBI Clinics. Inclusion criteria included history of chronic TBI (> 6 months post-injury) sustained either in combat or as a civilian; stable psychoactive medication regimen; self-reported cognitive difficulties in areas of concentration, planning, multitasking and memory that interfere with daily function; and interest/availability to participate in cognitive training. Exclusion criteria included: unstable medical, neurologic, or psychiatric conditions; psychosis, severe depression, anxiety, or PTSD precluding participation in research activities; ongoing illicit drug or alcohol abuse; or poor English comprehension. TBI diagnosis and severity was established using VA/Department of Defense TBI classification criteria, via review of participant medical records as well as detailed interview conducted by a clinician (neurologist or neuropsychologist) experienced in the diagnosis of brain injury.
Participants' average age was 43.3 years (standard deviation [SD] 11.57; range 25–66 years); 85% of participants were male, 67% of participants were white, and participants had an average of 14.45 years of education (SD, 1.82). A majority of participants (n = 19) sustained mTBI, with the remainder experiencing moderate (n = 7) or severe (n = 7) injury. The injuries sustained were from mixed causes including blunt injuries, motor vehicle accidents, and blasts. Eighteen participants reported experiencing multiple (i.e., more than one) TBIs. The injuries occurred at least 1 year prior to study participation (median time since injury = 6 years). All participants were independent in basic activities of daily living but reported continuing to experience mild to moderate difficulties on tasks involving organization, problem solving, multitasking, and distractibility. A majority of participants (n = 20) were not working or going to school. Seven participants were gainfully employed and six were students, but indicated having difficulties completing work and/or school tasks.
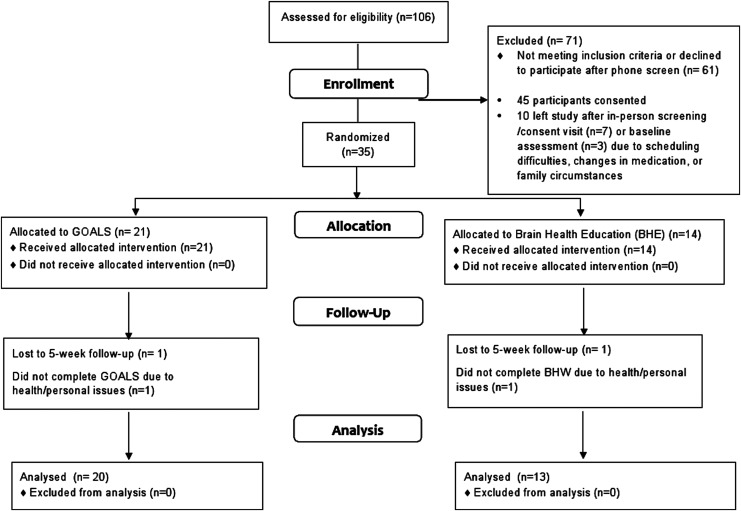
As shown in Figure 1, ten participants discontinued the study after either consent or baseline evaluations due to scheduling difficulties, change in medication, and/or family circumstances, and an additional two discontinued after starting the interventions due to illness and to a severe stressor (one after starting GOALS and one after starting BHE), leaving a total of 33 participants who completed the study.
FIG. 1.
Enrollment information.
Consecutively recruited participants were placed in small groups following completion of baseline evaluation (average group size: three participants), and the entire group was then randomized to receive either GOALS (n = 20) or an active comparison BHE training intervention (n = 13). BHE and GOALS were closely matched for therapist time and training intensity. Participants in the two intervention groups did not differ based on age (t = −1.59, df = 31, p = 0.12), education (t = −1.20, df = 31, p = 0.24), time since injury (t = −0.05, df = 31, p = 0.96), gender (χ2 = 0.93, df = 1, p = 0.34), ethnicity (χ2 = 1.59, df = 1, p = 0.21), or TBI severity (χ2 = 2.39, df = 2, p = 0.30).
Pre-and post-training, participants were evaluated with a multilevel battery consisting of neuropsychological and complex functional performance assessment and self-report measures of daily and emotional functioning. The assessments were administered by the same evaluator at both time-points, and every attempt was made to administer them at the same time of the day. Evaluators were blinded to participants' treatment conditions, and evaluators and therapists were separate individuals.
Interventions
GOALS training involved ten 2-h sessions of group-based training, three individual 1-h training sessions, and approximately 20 h of home practice over 5 weeks. It was conducted in a small group format with two to five participants and two therapists per group. For a detailed review of GOALS training, see Novakovic-Agopian and colleagues.22
The GOALS intervention emphasizes two key components. First, regulation of distractibility (i.e., redirection of attention to goal-relevant processes and the filtering of non-relevant “noise,” especially in the context of distractions) is addressed with attention regulation training. This aspect of the training emphasizes principles of applied mindfulness-based attention regulation to redirect cognitive processes towards task-relevant activities even when distracted. This requires identifying the current primary task, separating information into relevant and non-relevant categories, and working to selectively maintain relevant information while letting go of non-relevant information. Participants are trained in applying a meta-cognitive strategy (“Stop-Relax-Refocus”) to stop activity when distracted, anxious, and/or overwhelmed; relax; and then re-focus attention on the current primary goal. They are taught to actively apply goal-directed attention regulation skills to a range of situations, from simple information processing tasks to complex multi-step problems and challenging low-structure situations occurring in their own lives. Training via in-class exercises and homework is applied to progressively more challenging situations, including holding increasing amounts of information in mind, culminating with maintaining information while exposed to distractors. Homework includes practice in maintaining goal-direction during challenging real-life situations identified by participants. At the beginning of each session, participants discuss their experiences completing the homework with the rest of the group.
The second major component of GOALS training involves the active application of these goal-oriented attentional self-regulation skills to the identification, selection, and execution of self-generated complex goals. Participants are asked to identify personally relevant and feasible functional goals (e.g., finding an apartment, looking for a job, writing a school term paper, planning a vacation) as individual and group projects. They are then trained in applying the goal management strategies on the functional task(s) of their choice. The step-wise meta-cognitive goal management strategies trained were modified from the Goal Management Training28,30 and Problem Solving Therapy26,27,29,31 protocols. The main objective is to allow extensive practice and application of skills, thereby linking the attentional regulation directly to goal attainment efforts.
Three individual sessions are distributed at the beginning, middle, and towards the end of the training. Individual Session 1 occurs after Group Session 1 or 2. It covers orientation to the training program, including orientation to and clarification of the Participant Handbook and discussion of the following: a) brainstorming feasible individual goals; b) common internal and external distractions encountered and potential solutions; and c) homework implementation (e.g., noticing absentminded slips in daily life). Individual Session 2 occurs after Group Session 4 or 5 and involves review and implementation of training strategies. This includes discussion of plans for individual and group projects, identification of challenges to project completion (e.g. anxiety provoking situations, procrastination), and discussion of successes and failures in homework implementation (e.g., use of Stop-Relax-Refocus in daily life). Individual Session 3 occurs after Group Session 6 or 7 and covers review and implementation of training strategies in daily life, and review of execution, obstacles, and adjustments required for individual and group projects.
To ensure consistency of administration, intervention manuals were written for instructors and participants (Instructor and Participant Manuals of Goal-Orientated Attentional Self-Regulation –GOALS).23 If a session is missed, every effort is made for the participant to complete a make-up session.
BHE training is an active comparison matched with GOALS for therapist time, homework load, and participation in a group. It involved ten 2-h sessions of group-based training, three individual 1-h training sessions, and approximately 20 h of home practice over 5 weeks. It is conducted in a small group format with two to five participants and two therapists per group. The BHE training was designed to be engaging and provide information about brain functioning and brain health. Although session materials include information about sleep, diet, and effects of stress, they are educational in nature, emphasizing knowledge and not skills. Group leaders do not assist participants with making connections between the material presented and possible positive effects on their own daily functioning, or how to integrate into their daily lives. Further, the presumed active ingredients of GOALS training, which include applied problem-solving and attention regulation, are not part of the BHE intervention.
Intervention manuals were written for instructors and participants.33 Participants were provided with a make-up session if a session was missed. Participants also were given up to 30–60 min of daily homework between sessions (approximately 4 h per week). Homework consisted of reading articles related to session content and watching DVDs about brain functions and health.
Measures
Participants were evaluated with a multi-level battery consisting of neuropsychological and ecologically valid functional performance measures of complex attention and executive function, and self-report measures of daily functioning at pre- and post-GOALS or BHE group intervention. Additionally, they completed self-report measures of emotional functioning. These measures were administered by the same evaluator at both time-points and every attempt was made to administer them at the same time of the day. Evaluators were blinded to participants' treatment conditions, and evaluators and therapists were separate individuals.
Neuropsychological assessments
Similar to our previous studies,22,32 the current study used a neuropsychological battery specifically designed to assess performance in cognitive domains of complex attention and executive function that are commonly affected by TBI and targeted by GOALS training. Working Memory was assessed with 1) Auditory Consonant Trigrams,34 requiring recall of three consonants after counting backward by threes (e.g., 100, 97, 94, etc.) from a specified number for a variable amount of time, and 2) the Letter Number Sequencing subtest from the Wechsler Adult Intelligence Scale, Third Edition,35 requiring mental reordering of scrambled letter-number series of increasing lengths.
Inhibition of automatic responding was assessed with the Stroop Inhibition task (time and errors) from the Delis-Kaplan Executive Function System (DKEFS),36 in which words are printed in dissonant ink color and participants are instructed to name the color of the ink instead of providing the more automatic response of reading the word. Mental Flexibility was assessed with 1) Trail Making Test-Part B,37 requiring rapid alternation between letters and numbers to connect them in order; 2) Design Fluency-Switching (DKEFS),36 requiring alternating between empty and filled dots while generating different designs using four lines; 3) Verbal Fluency Switching (DKEFS),36 requiring the generation of words that belong to two specified categories and alternating between them; and 4) Stroop Inhibition-Switching (time and errors; DKEFS),36 during which the participant is presented with words printed in dissonant ink color, some of which are contained in boxes, and the participant is instructed to name the color of the ink unless the word is inside the box, in which case they are to read the word. Sustained Attention was assessed using the Digit Vigilance Test37 time and error scores. A composite Overall Attention and Executive Function domain (primary neurocognitive outcome measure) was constructed using Z scores on measures from the Inhibition, Working Memory, Sustained Attention, and Mental Flexibility domains.
Participants' performance in cognitive domains commonly affected by TBI, but not targeted by the intervention, also was assessed as a marker of potential nonspecific changes. To this end, the neuropsychological battery also contained measures of verbal and visual learning and memory, performance on which may be indirectly affected by changes in attention and executive functioning. Immediate Recall was assessed with Hopkins Verbal Learning Test–Revised (HVLT-R),38 requiring participants to learn 12 words presented over three learning trials, and with Brief Visual Memory Test–Revised (BVMT-R),39 requiring participants to learn and reproduce six abstract designs over three learning trials. Delayed Recall was assessed with HVLT-R and BVMT-R Delayed Recall trails, requiring participants to recall the word list or figures after a 20–25 min delay. A Memory composite score was created using the Total Recall and Delayed Recall scores. It is important to note that Overall Attention and Executive Function and Memory composite domain scores were not based on factor structure, but were constructed based on theory and authors' previous work.
To minimize practice effects, alternative test forms (DKEFS, HVLT-R, BVMT-R) and/or norms for repeated testing (Auditory Consonant Trigrams) were used for repeated administrations whenever feasible.
Functional assessment
It may be argued that the accurate measurement of executive control functioning requires observation and quantification of performance with real-life functional tasks that require planning, multitasking, and goal management in a low structure environment. To address the functional and ecological limitations of conventional clinical neuropsychological tests in characterizing executive dysfunction, we included a complex functional task assessment in the neurobehavioral test battery. (For further discussions, see Burgess and colleagues40 and Novakovic-Agopian and colleagues41). The Goal Processing Scale (GPS)41 involves the observation and rating of a participant completing a challenging task that engages executive control using a scoring system to quantify observations. Participants are instructed to plan and execute a task requiring them to gather and compare information about three different activities (or products/services, as designated on alternate forms) of their choice, using the available means while following specified rules in a limited time (30 min). Participants work in an office equipped with a computer with Internet access, a telephone, yellow pages telephone book, blank paper, pen, calculator, and clock. They are given a task instructions page, which contains the key requirements of the task and the task rules.
The subdomains of executive function evaluated during the Planning stage include the ability to comprehend task instructions and ask for clarifications when needed, to decide on and identify realistic goal(s), and to organize and prioritize steps involved in actual task execution. After the task goals and plan are decided upon, the participants are told to execute the task on the basis of their identified plan and task rules. The domains assessed during the task execution stage include the ability to initiate task-directed activities; Maintain Attention on a task both in a non-distracting environment and during the built-in task distractions; Self-Monitoring of performance (including inhibiting task activities to stop at specified times, review performance, notice, and correct errors); Sequence and Switch attention between and among the identified task subcomponents; and demonstrate Flexibility in approaching alternate solutions when the situation changes (e.g., the ability to continue with specified task goals when the preferred means of obtaining information such as the Internet or phone becomes unavailable). Memory, including both the ability to recall strategies when needed and the ability to correct previously noted errors, also was assessed. The Execution score reflects the accuracy of completion of identified task goals and effectiveness of time management while executing steps relevant to the identified plan and goals. Functional performance in these domains is rated on a scale ranging from 0 (not able) to 10 (absolutely not a problem). The GPS Overall Performance Score (primary functional performance outcome measure) is the average of the seven subdomain scores.
To assist in rating of performance on the subdomains and to ensure rating consistency, the GPS Rating Instruction Manual operationally defines and calibrates the following: 1) the cognitive domains evaluated; 2) the task-based context; 3) the rating scale; and 4) the objective criterion-based scoring used for evaluation. For further information about the development and validation of this measure, see Novakovic-Agopian and colleagues.41
Measures of daily and emotional functioning
Participants also completed self-report measures of daily and emotional functioning. Participants completed the Mayo-Portland Adaptability Inventory-4 (MPAI-4),42 a measure of common sequelae of TBI including impact on activities of daily living, emotional adjustment, and community integration. The Goal Processing Questionnaire (GPQ),22 a self-report measure of post-training improvement in ability to plan and execute aspects of complex goal-directed behavior in daily life, also was completed (available online at www.liebertpub.com/neu).
Level of psychological distress was assessed using the Profile of Mood States (POMS).43 Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II).44 Symptoms of PTSD were evaluated with the PTSD Checklist, Military Version (PCL-M).45
Primary outcome measures
Based on theory and previous research, primary outcome measures were selected for each level of functioning assessed. Attention and Executive Function Domain Score was the primary outcome measure for neurocognitive functioning. The primary complex functional task performance measure was GPS Overall Performance Score. POMS Total Mood Disturbance was the primary outcome for self-report of emotional functioning, and MPAI-4 Total Score was the primary outcome for self-report of daily functioning.
Statistical analysis
Descriptive statistics were calculated for the neuropsychological, functional, and self-report variables for the whole sample and both intervention groups separately (GOALS and BHE). All analyses were conducted using SPSS Version 23.46
All neuropsychological test data were scored based on standardized age and when available, educational and repeated administration norms, and transformed into z scores for consistency. To assess the impact of training on targeted cognitive domains and reduce the variability and number of multiple comparisons, z scores for individual neuropsychological tests were averaged into the overall Attention and Executive Function Domain Score, as well as the following Memory Domain scores:
Attention and Executive Function Domain Score primary neurocognitive outcome measure (average of z scores): Letter Number Sequencing; Auditory Consonant Trigrams 9, 18, and 36 sec; Digit Vigilance Test–Time and Errors; Design Fluency Switching; Verbal Fluency Switching; Trails B; Stroop Inhibition/Switching- Time and Errors; Stroop Inhibition–Time and Errors;
Working Memory Sub-Domain Score (average of z scores): Letter Number Sequencing; Auditory Consonant Trigrams 9, 18, and 36 sec;
Mental Flexibility Sub-Domain Score (average of z scores): Design Fluency Switching; Verbal Fluency Switching; Trails B; Stroop Inhibition/Switching– Time and Errors;
Sustained Attention Sub-Domain Score (average of z scores): Digit Vigilance Test–Time and Digit Vigilance Test-Errors;
Inhibition Sub-Domain Score (average of z scores): Stroop Inhibition–Time and Stroop Inhibition Errors;
Memory Domain Score (average of z scores): HVLT-R Total Recall; BVMT-R Total Recall; HVLT-R Delayed Recall; and BVMT-R Delayed Recall.
Immediate Recall Sub-Domain Score (average of z scores): HVLT-R Total Recall and BVMT-R Total Recall;
Delayed Recall Sub-Domain Score (average of z scores): HVLT-R Delayed Recall and BVMT-R Delayed Recall.
Scores on GPS, BDI-II, GPQ, and PCL-M were analyzed in their original scales; POMS and MPAI-4 raw scores were converted to z scores.
A 2 × 2 repeated measures multivariate analysis of variance (MANOVA) was used to compare group performances on neurocognitive domain scores at pre- and post-intervention, and to compare within-group changes over time on neurocognitive domain scores (Attention and Executive Function, and Memory) for GOALS versus BHE (Aim A). Additional repeated measures MANOVAs examining changes pre- to post-training also were conducted for each group (GOALS and BHE) separately (Aim B).
Similarly, a repeated measures MANOVA was used to compare group performance on GPS functional task domain scores at pre- and post-intervention, and to compare changes over time for GOALS versus BHE (Aim A). Additional repeated measures MANOVAs were then conducted for each group separately (Aim B).
Separate repeated measures MANOVAs were conducted to compare changes in scores on measures of everyday and emotional functioning (raw-score measures BDI-II and PCL; z-score measures POMS and MPAI-4) for the whole sample (Aim C) and each group separately (Aim D). Finally, post-training GPQ scores were compared for the two groups using a single MANOVA.
Although we have examined a number of cognitive domains and sub-domains, we report nominal p values, without adjustment for multiple testing, consistent with our previous work.22 Such adjustments are focused on avoidance of one or more results with p < 0.05 in the case where all differences are truly zero,47–49 which is an unrealistic hypothesis about the state of nature in this context. In addition, adjustment would require that each result detract from the others, but there are clear relationships between the domains under study as they represent different levels of the same hypothesized constructs, and these permit coherent sets of findings to reinforce each other rather than detract from one another.
In order to demonstrate the strength and relative significance of our results, we report partial η2, which is a standardized estimate of effect size equivalent to the partial proportion of the variance in the dependent variable explained uniquely by the predictor divided by the proportion of variance explained by the other variables.50 Values of around 0.01 are considered small, 0.09 is considered medium, and values of 0.25 and above are considered large.51,52
Results
Neuropsychological measures
A repeated measures MANOVA was used to compare the impact of GOALS training versus the BHE training on neurocognitive performance (Table 1).
Table 1.
Effects of Training (GOALS vs. BHE) on Neurocognitive Outcomes
| Pre-training | Post-training | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GOALS | BHE | GOALS | BHE | F (1,30) | ||||||||||
| M | SD | M | SD | M | SD | M | SD | Group | Partial η2 | Time | Partial η2 | Group × Time | Partial η2 | |
| Overall Attention/EF | −0.29 | 0.64 | −0.38 | 0.68 | −0.03 | 0.53 | −0.37 | 0.70 | 0.93 | 0.03 | 8.16** | 0.21 | 7.10*1 | 0.19 |
| Working Memory | −0.37 | 0.88 | −0.36 | 0.89 | −0.08 | 0.78 | −0.56 | 1.13 | 0.56 | 0.02 | 0.18 | 0.01 | 6.12*1 | 0.17 |
| Sustained Attention | −0.52 | 0.74 | −0.45 | 0.77 | −0.40 | 0.56 | −0.37 | 0.81 | 0.04 | 0.00 | 1.81 | 0.06 | 0.09 | 0.00 |
| Mental Flexibility | −0.16 | 0.63 | −0.37 | 0.76 | 0.15 | 0.52 | −0.19 | 0.70 | 1.51 | 0.05 | 12.74** | 0.30 | 0.88 | 0.03 |
| Inhibition | −0.23 | 0.94 | −0.37 | 0.78 | 0.00 | 0.72 | −0.43 | 0.76 | 1.04 | 0.03 | 1.27 | 0.04 | 3.74 | 0.11 |
| Memory | −0.61 | 0.98 | −0.90 | 1.09 | −0.22 | 0.92 | −0.73 | 1.20 | 1.36 | 0.04 | 4.46* | 0.13 | 0.74 | 0.02 |
| Immediate Recall | −0.45 | 1.02 | −0.95 | 1.15 | −0.25 | 1.06 | −0.78 | 1.30 | 1.90 | 0.06 | 1.50 | 0.05 | 0.01 | 0.00 |
| Delayed Recall | −0.77 | 1.08 | −0.85 | 1.08 | −0.18 | 0.95 | −0.69 | 1.16 | 0.71 | 0.02 | 5.88* | 0.16 | 1.92 | 0.06 |
Significant at the p < 0.05 level.
Significant at the p < 0.01 level.
Participants in GOALS group improved significantly more from pre to post-training, compared with BHE.
GOALS, Goal-Oriented Attentional Self-Regulation; BHE, Brain-Health Education; M, mean; SD, standard deviation; EF, executive function.
Significant group by time interactions effects were identified for primary neurocognitive outcome score Overall Attention/Executive Function composite and Working Memory, such that individuals who received GOALS demonstrated more improvement on tasks of Overall Attention/Executive Function [F (1,30) = 7.10, p = 0.01; partial η2 = 0.19] and Working Memory [F (1,30) = 6.12, p = 0.02; partial η2 = 0.17], compared with those individuals who participated in the BHE intervention. See Table 1 for results of within-subjects analysis of effect of time (pre- vs. post-training) on neurocognitive performance.
When the groups were analyzed separately, significant improvement post-training was found for the GOALS group, but not the BHE group, in primary neurocognitive outcome measure Overall Attention/Executive Function [F (1,18) = 17.68, p = 0.001, partial η2 = 0.50], Working Memory [F (1,18) = 4.65, p = 0.045, partial η2 = 0.21], Mental Flexibility[F (1,18) = 11.327, p = 0.003, partial η2 = 0.39], Inhibition [F (1,18) = 7.29, p = 0.02, partial η2 = 0.29], as well as Delayed Recall [F (1,18) = 8.13, p = 0.01, partial η2 = 0.31] and Memory Composite [F (1,18) = 5.01, p = 0.04, partial η2 = 0.22; Table 2]. No statistically significant changes were observed for the BHE group on neurocognitive outcomes when analyzed separately. (See Supplementary Table 1 at www.liebertpub.com/neu for impact of training [GOALS vs. BHE] on individual neuropsychological measures.)
Table 2.
Effects of GOALS Training on Neurocognitive Outcomes
| Pre-training | Post-training | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | F (1,18) | Partial η2 | |
| Overall Attention/EF | −0.29 | 0.64 | −0.03 | 0.53 | 17.68** | 0.50 |
| Working Memory | −0.37 | 0.88 | −0.08 | 0.78 | 4.65* | 0.21 |
| Sustained Attention | −0.52 | 0.74 | −0.40 | 0.56 | 0.27 | 0.07 |
| Mental Flexibility | −0.16 | 0.63 | 0.15 | 0.52 | 11.33** | 0.39 |
| Inhibition | −0.23 | 0.94 | 0.00 | 0.72 | 7.29* | 0.29 |
| Memory | −0.61 | 0.98 | −0.22 | 0.92 | 5.01* | 0.22 |
| Immediate Recall | −0.45 | 1.02 | −0.25 | 1.06 | 0.94 | 0.05 |
| Delayed Recall | −0.77 | 1.08 | −0.18 | 0.95 | 8.13* | 0.31 |
Significant at the p < 0.05 level.
Significant at the p < 0.01 level.
GOALS, Goal-Oriented Attentional Self-Regulation; M, mean; SD, standard deviation; EF, executive function.
Functional measure of executive function
A repeated measures MANOVA was used to compare the impact of GOALS training versus the BHE training on functional task performance (Table 3).
Table 3.
Effects of Training (GOALS vs. BHE) on GPS Functional Performance
| Pre-training | Post-training | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GOALS | BHE | GOALS | BHE | F (1,28) | ||||||||||
| M | SD | M | SD | M | SD | M | SD | Group | Partial η2 | Time | Partial η2 | Group × Time | Partial η2 | |
| GPS Overall Performance | 7.14 | 1.39 | 7.16 | 1.24 | 8.20 | 1.15 | 7.30 | 1.04 | 1.09 | 0.04 | 11.69** | 0.30 | 6.92*1 | 0.20 |
| Planning | 7.01 | 1.54 | 6.81 | 1.44 | 8.01 | 1.25 | 6.95 | 1.57 | 1.62 | 0.06 | 6.37* | 0.19 | 3.62 | 0.12 |
| Initiation | 9.86 | 0.33 | 10.0 | 0.00 | 10.0 | 0.00 | 9.92 | 0.29 | 0.22 | 0.01 | 0.22 | 0.01 | 3.53 | 0.11 |
| Self-monitoring | 6.16 | 2.06 | 6.12 | 1.72 | 7.60 | 1.56 | 6.66 | 1.54 | 0.80 | 0.03 | 7.81** | 0.22 | 1.61 | 0.05 |
| Maintenance of Attention | 7.70 | 1.63 | 7.38 | 1.47 | 8.46 | 1.53 | 7.57 | 1.45 | 1.31 | 0.05 | 4.41* | 0.14 | 1.59 | 0.05 |
| Sequencing/Switching | 6.58 | 2.28 | 7.02 | 2.26 | 7.95 | 1.87 | 7.08 | 1.61 | 0.10 | 0.00 | 5.12* | 0.16 | 4.28*1 | 0.13 |
| Divergent Thinking | 7.83 | 2.26 | 8.00 | 1.68 | 8.39 | 2.00 | 7.63 | 2.13 | 0.23 | 0.01 | 0.04 | 0.00 | 1.11 | 0.04 |
| Execution | 5.88 | 2.03 | 6.39 | 1.82 | 7.30 | 2.12 | 6.69 | 2.15 | 0.01 | 0.00 | 5.70* | 0.17 | 2.37 | 0.08 |
| Learning and Memory | 6.12 | 2.66 | 5.58 | 2.00 | 7.89 | 1.95 | 5.89 | 2.05 | 3.28 | 0.11 | 5.73* | 0.17 | 2.81 | 0.09 |
Significant at the p < 0.05 level.
Significant at the p < 0.01 level.
Participants in GOALS group improved significantly more from pre to post-training, compared with BHE.
GOALS, Goal-Oriented Attentional Self-Regulation; BHE, Brain-Health Education; GPS, Goal Processing Scale; M, mean; SD, standard deviation.
Significant group by time interactions were observed for primary functional outcome measure GPS Overall Performance [F(1,28) = 6.92, p = 0.01, partial η2 = 0.20] and Sequencing/Switching of Attention [F(1,28) = 4.28, p = 0.048, partial η2 = 0.13] such that GOALS participants improved more after training, compared with BHE participants (Table 3). See Table 3 for results of within-subjects analysis of effect of time (pre- vs. post-training) on functional task performance.
When the groups were analyzed separately, significant improvement post-GOALS training was observed for primary functional outcome measure GPS Overall Performance [F(1,17) = 15.18, p = 0.0001, partial η2 = 0.47], Planning [F(1,17) = 14.19, p = 0.002, partial η2 = 0.46], Self-monitoring [F(1,17) = 8.77, p = 0.009, partial η2 = 0.34], Maintenance of Attention [F(1,17) = 6.01, p = 0.03, partialη2 = 0.26], Sequencing/Switching of Attention [F(1,17) = 9.90, p = 0.006, partialη2 = 0.37], Execution [F(1,17) = 6.93, p = 0.02, partialη2 = 0.29], and Learning and Memory [F(1,17) = 8.88, p = 0.008, partialη2 = 0.34; Table 4]. There were no significant improvements detected for BHE participants in the separate by-group analysis.
Table 4.
Effects of GOALS Training on GPS Functional Performance
| Pre-training | Post-training | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | F (1,17) | Partial η2 | |
| GPS Overall Performance | 7.14 | 1.39 | 8.20 | 1.15 | 15.18** | 0.47 |
| Planning | 7.01 | 1.54 | 8.01 | 1.25 | 14.19** | 0.46 |
| Initiation | 9.86 | 0.33 | 10.0 | 0.00 | 3.10 | 0.15 |
| Self-monitoring | 6.16 | 2.06 | 7.60 | 1.56 | 8.77** | 0.34 |
| Maintenance of Attention | 7.70 | 1.63 | 8.46 | 1.53 | 6.01* | 0.26 |
| Sequencing/Switching | 6.58 | 2.28 | 7.95 | 1.87 | 9.90** | 0.37 |
| Divergent Thinking | 7.83 | 2.26 | 8.39 | 2.00 | 0.83 | 0.05 |
| Execution | 5.88 | 2.03 | 7.30 | 2.12 | 6.93* | 0.29 |
| Learning and Memory | 6.12 | 2.66 | 7.89 | 1.95 | 8.88** | 0.34 |
Significant at the p < 0.05 level.
Significant at the p < 0.01 level.
GOALS, Goal-Oriented Attentional Self-Regulation; GPS, Goal Processing Scale; M, mean; SD, standard deviation.
Measures of daily functioning
Repeated measures MANOVAs (Table 5A and 5B) and an analysis of variance (Table 6) were used to compare the impact of GOALS training versus the BHE training on self-report measures of daily functioning. No significant interaction effects between time and type of training were observed on primary daily functioning outcome measure MPAI-4. When groups were analyzed separately, improvement was observed for GOALS participants on MPAI-4 Total Score [F(1,16) = 4.61, p = 0.048, partialη2 = 0.22] and Adjustment [F(1,16) = 5.47, p = 0.03, partialη2 = 0.26; Table 5B]. No significant improvements were observed for the BHE group when analyzed separately (data not shown). See Table 5A for within-subjects analysis of effect of time (pre- vs. post-training) and between-subjects effect of group (GOALS vs. BHE) on MPAI-4 outcomes.
Table 5A.
Effects of GOALS vs BHE Training on Daily Functioning Outcomes
| Pre-training | Post-training | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| GOALS | BHE | GOALS | BHE | F (1,25) | |||||||
| M | SD | M | SD | M | SD | M | SD | Group | Time | Group × Time | |
| Mayo-Portland | |||||||||||
| Ability | −0.39 | 0.93 | −0.51 | 0.84 | 0.10 | 1.34 | −0.52 | 1.20 | 0.85 | 1.64 | 1.78 |
| Adjustment | −0.56 | 0.76 | −1.05 | 0.56 | −0.24 | 0.67 | −0.85 | 0.76 | 4.70* | 5.26* | 0.31 |
| Participation | 0.33 | 1.38 | −0.50 | 1.29 | 0.52 | 0.84 | −0.03 | 1.00 | 2.67 | 3.36 | 0.61 |
| Total | −0.38 | 0.73 | −0.71 | 0.64 | −0.02 | 0.76 | −0.57 | 0.79 | 2.66 | 4.40* | 0.85 |
Table 5.
Table 5B. Effects of GOALS Training on Daily Functioning Outcomes
| Pre-training | Post-training | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | F (1,16) | Partial η2 | |
| Mayo-Portland | ||||||
| Ability | −0.39 | 0.93 | 0.10 | 1.34 | 3.28 | 0.17 |
| Adjustment | −0.56 | 0.76 | −0.24 | 0.67 | 5.47* | 0.26 |
| Participation | 0.33 | 1.38 | 0.52 | 0.84 | 0.75 | 0.05 |
| Total | −0.38 | 0.73 | −0.02 | 0.76 | 4.61* | 0.22 |
Significant at the p < 0.05 level.
GOALS, Goal-Oriented Attentional Self-Regulation; BHE, Brain-Health Education; M, mean; SD, standard deviation.
Table 6.
Effects of Training (GOALS vs BHE) on GPQ Change (Baseline-Week 5) Outcomes
| GOALS | BHE | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | F (1,22) | Partial η2 | |
| Planning | 6.92 | 1.98 | 5.69 | 1.04 | 2.96 | 0.12 |
| Initiation | 6.69 | 2.29 | 5.84 | 1.12 | 1.07 | 0.05 |
| Self-Monitoring | 7.22 | 1.56 | 5.78 | 0.92 | 6.37* | 0.22 |
| Working Memory/Attention | 6.45 | 1.86 | 5.01 | 0.12 | 5.27* | 0.19 |
| Sequencing | 6.91 | 1.92 | 5.25 | 0.36 | 6.53* | 0.23 |
| Divergent Thinking | 6.95 | 1.88 | 5.84 | 1.43 | 2.31 | 0.10 |
| Execution | 6.98 | 1.70 | 5.55 | 0.88 | 5.47* | 0.20 |
| Learning/Past Experience | 7.20 | 1.65 | 5.74 | 0.75 | 6.19* | 0.22 |
| Awareness | 6.55 | 1.98 | 5.27 | 0.44 | 3.59 | 0.14 |
| Fatigue/Energy Management | 6.47 | 1.88 | 5.20 | 1.06 | 3.38 | 0.13 |
| Social Interaction | 6.43 | 2.40 | 5.91 | 1.28 | 0.35 | 0.02 |
| Anxiety | 6.51 | 1.90 | 5.44 | 0.68 | 2.57 | 0.11 |
| Sleep | 5.94 | 2.64 | 4.81 | 0.70 | 1.55 | 0.07 |
Significant at the p < 0.05 level.
GOALS, Goal-Oriented Attentional Self-Regulation; BHE, Brain-Health Education; M, mean; SD, standard deviation.
Results of the post-treatment between-group Goal Processing Questionnaire analysis (Table 6) revealed that GOALS participants, compared with BHE participants, indicated significantly more post-training improvement in their daily lives in the areas of Self-Monitoring [F(1,22) = 6.37, p = 0.02, partialη2 = 0.22], Working Memory[F(1,22) = 5.27, p = 0.03, partialη2 = 0.19], Sequencing [F(1,22) = 6.53, p = 0.02, partialη2 = 0.23], Execution [F(1,22) = 5.47, p = 0.03, partialη2 = 0.20], and Learning from Past Experience [F(1,22) = 6.19, p = 0.02, partialη2 = 0.22].
Measures of emotional functioning
Repeated measures MANOVAs were used to compare the impact of GOALS training versus the BHE training on emotional functioning outcomes (Table 7). There was a significant interaction effect of intervention group and time on POMS Confusion, such that GOALS participants improved more than BHE participants after training [F(1,25) = 6.05, p = 0.02, partialη2 = 0.20]. See Table 7 for within-subjects analyses of effect of time (pre- vs. post-training) and group (GOALS vs. BHE) on POMS scale outcomes.
Table 7.
Effects of Training (GOALS vs BHE) on Emotional Functioning Outcomes
| Pre-training | Post-training | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| GOALS | BHE | GOALS | BHE | F (1,24) | |||||||
| M | SD | M | SD | M | SD | M | SD | Group | Time | Group × time | |
| BDI-II | 22.88 | 11.44 | 27.40 | 9.95 | 16.00 | 9.17 | 23.80 | 9.13 | 4.15 | 5.54* | 0.63 |
| PCL-M | |||||||||||
| Total | 42.94 | 19.33 | 57.40 | 10.38 | 38.38 | 13.98 | 53.90 | 12.90 | 7.03* | 3.08 | 0.05 |
| Re- experiencing | 11.75 | 7.13 | 15.50 | 5.54 | 9.81 | 4.45 | 14.70 | 5.66 | 3.65 | 4.76* | 0.82 |
| Avoidance | 18.44 | 8.70 | 22.90 | 4.51 | 16.00 | 6.80 | 22.00 | 5.72 | 4.02 | 2.80 | 0.60 |
| Arousal | 14.31 | 5.26 | 18.70 | 3.02 | 13.91 | 5.21 | 17.20 | 3.05 | 7.20* | 1.93 | 0.04 |
Significant at the p < 0.05 level.
GOALS, Goal-Oriented Attentional Self-Regulation; BHE, Brain-Health Education; M, mean; SD, standard deviation; BDI-II, Beck Depression Inventory-II; PCL-M, Posttraumatic Stress Disorder Checklist, Military Version,
In addition, when the groups were analyzed separately, improvements were noted for GOALS participants in POMS Total Mood Disturbance [F(1,16) = 8.33, p = 0.01, partialη2 = 0.34], Tension [F(1,16) = 12.16, p = 0.003, partialη2 = 0.43], Depression [F(1,16) = 8.77, p = 0.009, partialη2 = 0.35], Anger [F(1,16) = 7.56, p = 0.01, partialη2 = 0.32], and Confusion [F(1,16) = 8.41, p = 0.01, partialη2 = 0.35; Table 8]. No significant improvements were observed for the BHE group in a separate analysis. For the PCL-M and BDI-II analysis, there were no significant interaction effects (Table 7). See Table 7 for effect of time (pre- vs. post-training) and group (GOALS vs. BHE) on BDI-II and PCL-M outcomes.
Table 8.
Effects of GOALS Training on Emotional Functioning Outcomes
| Pre-training | Post-training | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | F (1,15) | Partial η2 | |
| BDI-II | 22.44 | 11.67 | 15.19 | 8.81 | 5.69* | 0.28 |
| PCL-M | ||||||
| Total | 42.94 | 19.33 | 38.38 | 13.98 | 1.77 | 0.11 |
| Re- experiencing | 11.75 | 7.13 | 9.81 | 4.45 | 4.72* | 0.24 |
| Avoidance | 18.44 | 8.70 | 16.00 | 6.80 | 3.27 | 0.18 |
| Arousal | 14.31 | 5.26 | 13.91 | 5.21 | 0.72 | 0.05 |
| POMS | F (1,16) | |||||
| Overall Mood Disturbance | −1.73 | 1.09 | −0.86 | 0.96 | 8.33* | 0.34 |
| Tension | −0.66 | 1.06 | 0.01 | 0.93 | 12.16** | 0.43 |
| Depression | −2.10 | 1.47 | −0.74 | 1.59 | 8.77** | 0.35 |
| Anger | −1.38 | 1.56 | −0.58 | 1.25 | 7.56* | 0.32 |
| Confusion | −1.72 | 0.90 | −0.88 | 0.92 | 8.41* | 0.35 |
| Vigor | −0.58 | 1.08 | −0.22 | 1.25 | 2.33 | 0.13 |
| Fatigue | −1.24 | 0.78 | −0.92 | 0.98 | 1.01 | 0.06 |
Significant at the p < 0.05 level.
Significant at the p < 0.01 level.
GOALS, Goal-Oriented Attentional Self-Regulation; BHE, Brain-Health Education; M, mean; SD, standard deviation; BDI-II, Beck Depression Inventory-II; PCL-M, Posttraumatic Stress Disorder Checklist, Military Version; POMS, Profile of Mood States.
When the groups were analyzed separately, GOALS participants improved post-training on BDI-II Total Score [F(1,15) = 5.69, p = 0.03, partial η2 = 0.28] and PCL Re-experiencing [F(1,15) = 4.72, p = 0.046, partial η2 = 0.24; Table 8], whereas BHE participants did not improve significantly on BDI-II or any of the PCL-M scales post-training.
Discussion
This study examined the effects of a cognitive rehabilitation intervention targeting attentional control and executive function for veterans with a history of chronic TBI and complaints of executive difficulties in their daily lives. Our results show that participants who completed GOALS training showed greater improvement than those who completed a time-matched psycho-educational training on measures of neurocognitive, daily, and emotional functioning, particularly in the domains of attention/executive function, complex functional task performance, and emotional regulation.
Similar to results of our previous smaller study with civilians with chronic acquired brain injury,22 the results of the current study showed that veterans with chronic TBI improved more after GOALS training than time-matched psycho-educational training on neuropsychological measures of overall complex attention and executive functions composite score and working memory. These findings are consistent with the hypothesized cognitive targets of the training, indicating transfer of skills to improvements in non-trained tasks. We theorized that the essential ingredients of this intervention included mindfulness-based attention regulation techniques that were introduced during the initial training sessions and applied throughout classroom and home practice, including activities requiring complex goal management in participants' daily lives. Relevant to questions of generalization of training gains among cognitive domains, within-group analyses show participants' improvements on memory measures occurred despite the use of alternative test forms to minimize practice effects and the absence of direct memory training. This suggests that improvements in the memory domain could have been related to improvements in attention and executive functions for those who completed GOALS training. In particular, decreased distractibility and improved ability to select and hold goal-relevant information in mind are likely to optimize one's ability to learn new information, and improve efficiency in retrieving it later.
Ecologically valid measurement of executive control functioning requires observation and quantification of performance on functional tasks performed in a low-structure real-world environment. Following GOALS, significant interaction effects show that participants showed more improvement in performance on the GPS complex functional task than participants who completed BHE in domains of overall performance and sequencing/switching of attention. These findings suggest generalization of training effects to functional performance in complex, unstructured ecologically valid settings.
To assess the subjective changes in strategy use applicable to everyday life, participant self-reports on the Goal Processing Questionnaire post-GOALS or BHE training were collected. A post-training between-group comparison showed that after GOALS but not BHE training, participants reported successfully applying strategies resulting in significant improvements in several areas of their daily lives including self-monitoring, working memory, task execution, and learning from past experiences.
Given the high prevalence of co-morbid depression and PTSD in veterans with history of TBI, we also assessed effects of training on self-report measures of emotional functioning. An interaction effect showed that participants report more improvement after GOALS than after BHE on POMS Confusion subscale. Further, within-group analysis showed that after GOALS, participants indicated improvement on a range of self-report measures of emotional regulation and functioning, including the POMS Total Mood Disturbance Score, and POMS Tension, Depression, Anger, and Confusion domain scores; the Beck Depression Inventory II; and on the PCL-M Re-Experiencing sub-score. Participants did not endorse similar improvement based on within-group analysis of the BHE group separately. These findings suggest that improving cognitive control, and attentional self-regulation in particular, also may improve functioning in other domains. For example, as discussed earlier, improvements in the memory domain may be related to improved ability to select and hold goal-relevant information in mind. Similarly, improved ability to maintain goal-related information and protect it from internal disruptions (e.g., feeling anxious) may play a role in improving emotional regulation. An additional factor worth exploring is the possibility of improved self-efficacy, with the experience of goal attainment associated with completion of personally relevant functional goals.
The findings from this study add support to previous predominantly civilian studies demonstrating the efficacy of problem solving and meta-cognitive strategies also included in a number of other interventions such as problem-solving and goal-management protocols developed by D'Zurilla and Goldfried,26 Von Cramon and colleagues,27 Rath and colleagues.,29 Levine and colleagues,28 Evans,53 and Miotto and colleagues.54 The current intervention extends these findings by placing greater emphasis on applied mindfulness-based attention regulation, with the hypothesis that improving goal-directed attention regulation would benefit all subsequent stages of goal management.
Connection between in-group training and the real-life situations and goals identified by participants, in which attention regulation and problem solving play an important functional role, is a crucial aspect of training, and helps with both training adherence and maintenance. Nearly all participants (94%) from the previous GOALS study with predominantly civilian participants with acquired brain injury spontaneously reported continued use of at least one trained strategy in their daily lives up to 2 years post-training.55 Preliminary results of a recently completed long-term follow-up study suggest that the majority of veterans with chronic TBI who underwent GOALS training were able to retain post-training benefits in cognitive, functional, and emotional regulation domains for as long as 2 years post-intervention.56
Strengths of this study include the randomized design, blinded evaluators, multi-level assessment, and the use of a control intervention matched for time and intensity. One important limitation of this study is a relatively small sample size, and replication of this research with larger samples is needed. This also may have resulted in our interaction analyses being underpowered, possibly leading to failure to detect true effects of group on outcomes from pre- to post-training.
Future Directions
The findings of the current study suggest GOALS training may be a promising intervention for individuals with chronic TBI. Improving cognitive control functioning also may improve functioning in other domains such as emotional regulation and functional performance, potentially making it relevant for veterans with history of TBI and co-morbid PTSD and/or depressive symptoms. Our ongoing study with veterans with current diagnosis of PTSD and history of mild TBI seeks to address this question in more detail. Ongoing and future work will also examine the impact of baseline cognitive status, injury severity, and mood dysfunction on outcomes of GOALS training.
Supplementary Material
Acknowledgments
This material is based upon work supported by the Department of Veterans Affairs Rehabilitation Research and Development Service Merit Review Awards (VANCHS Project # B7467I and VA 1IO1RX001111-01A1).
We wish to thank participating veterans and a number of individuals who made this study possible, in particular: Deborah Binder, MS, for helping with development of Brain Health Education training protocol, and Gerald Carlin, OTR/L, Brian Curran, MS, Michelle Madore, PhD, Jim Muir, PhD, Michelle Murphy, PhD, Annemarie Rossi, OTR/L, and Nick Rodriguez for their exceptional work with participant training and evaluations. We are grateful to Brian Levine PhD, Ian Robertson PhD and Tom Manly PhD for providing us with the Goal Management Training material to review during the development of the GOALS training manuals.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Tanielian T. and Jaycox L. (2008) Invisible Wounds of War: Psychological and Cognitive Injuries, their Consequences, and Services to Assist Recovery. RAND: Santa Monica, CA; [Google Scholar]
- 2.Seal K., Metzler T.J., Gima K.S., Bertenthal D., Maguen S., and Marmar C.R. (2009) Increasing prevalence of mental disorders among Iraq and Afghanistan veterans. Am. J. Public Health, 99, 1651–1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoge C.W., McGurk D., Thomas J.L., Cox A.L., Engel, and Castro C.A. (2008) Mild traumatic brain injury in U.S. soldiers returning from Iraq. N. Engl. J. Med. 358, 453–463 [DOI] [PubMed] [Google Scholar]
- 4.Hoge C.W., Goldberg H.M., and Castro C.A. (2009) Care of war veterans with mild traumatic brain injury—flawed perspectives. N. Engl. J. Med. 360, 1588–1591 [DOI] [PubMed] [Google Scholar]
- 5.Hayward P. (2008). Traumatic brain injury: the signature of modern conflicts. Lancet Neurol. 7, 200–201 [DOI] [PubMed] [Google Scholar]
- 6.Reiber G.E., McFarland L.V., Hubbard S., Maynard C., Blough D.K., Gambel J.M., and Smith D.G. (2010). Service members and veterans with major traumatic limb loss from Vietnam war and OIF/OEF conflicts: survey methods, participants, and summary findings. J. Rehabil. Res. Dev. 47, 275 [DOI] [PubMed] [Google Scholar]
- 7.Rutherford G.W. and Corrigan J.D. (2009). Long‐term consequences of traumatic brain injury. J Head Trauma Rehabil, 24, 421–423 [DOI] [PubMed] [Google Scholar]
- 8.Vasterling J. and Brewin C.R. (2005). Neuropsychology of PTSD. The Guilford Press: New York; [Google Scholar]
- 9.Vasterling J. (2007). PTSD and neurocognition. Res. Quarterly 18 [Google Scholar]
- 10.Schneiderman A.I., Braver E.R., and Kang H.K. (2008). Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent post-concussive symptoms and posttraumatic stress disorder. Am. J. Epidemiol. 167, 1446–1452 [DOI] [PubMed] [Google Scholar]
- 11.Polusny M.A., Kehle S.M., Nelson N.W., Erbes C.R., Arbisi P.A., and Thuras P. (2011). Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in national guard soldiers deployed to Iraq. Arch. Gen. Psychiatry 68, 79–89 [DOI] [PubMed] [Google Scholar]
- 12.Mac Donald C.L., Barber J., Jordan M., Johnson A.M., Dikmen S., Fann J., and Temkin N. (2017). Early clinical predictors of 5 year outcome after concussive brain injury. JAMA Neurol. 74, 821–829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cornis-Pop M., Mashima P.A., Roth C.R., MacLennan D.L., Picon L.M., Hammond C.S., Goo-Yashino S., Isaki E., Singson M., and Frank E.M. (2012). Cognitive-communication rehabilitation for combat-related mild traumatic brain injury. J. Rehabil. Res. Dev. 49, xi–xxxii [DOI] [PubMed] [Google Scholar]
- 14.Vanderploeg R.D., Belanger H.G., and Curtiss G. (2009). Mild traumatic brain injury and posttraumatic stress disorder and their associations with health symptoms. Arch. Phys. Med. Rehabil. 90, 1084–1093 [DOI] [PubMed] [Google Scholar]
- 15.Chen A. and Novakovic-Agopian T. (2012). Intervening to improve cognitive functioning after neurotrauma, in: Traumatic Brain Injury: A Neurologic Approach to Diagnosis, Management and Rehabilitation. Tsao J. (ed). Springer: New York: [Google Scholar]
- 16.Vasterling J., Bryant R., and Keane T. (2012). PTSD and mild traumatic brain injury. Guilford: New York: [Google Scholar]
- 17.Cattran Cattran C., Oddy M., and Wood R. (2011). The development of a measure of emotional regulation following acquired brain injury. J. Clin. Exp. Neuropsychol. 33, 672–679 [DOI] [PubMed] [Google Scholar]
- 18.Tate R.L. (1999). Executive dysfunction and characterological changes after traumatic brain injury: two sides of the same coin? Cortex 35, 39–55 [DOI] [PubMed] [Google Scholar]
- 19.Simmons A.N. and Matthews S.C. (2012). Neural circuitry of PTSD with or without mild traumatic brain injury: a meta-analysis. Neuropharmacology 62, 598–606 [DOI] [PubMed] [Google Scholar]
- 20.Bufkin J.L. and Luttrell V.R. (2005). Neuroimaging studies of aggressive and violent behavior: current findings and implications for criminology and criminal justice. Trauma Violence Abuse, 6, 176–191 [DOI] [PubMed] [Google Scholar]
- 21.Jha A.P., Stanley E. A., Kiyonaga A., Wong L., and Gelfand L. (2010). Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion 10, 54–64 [DOI] [PubMed] [Google Scholar]
- 22.Novakovic-Agopian T., Chen A., Rome S., Abrams G., Castelli H., Rossi A., McKim R., Hills N., and D'Esposito M. (2011). Rehabilitation of executive functioning with training in attention regulation applied to individually defined goals: a pilot study bridging theory, assessment, and treatment. J. Head Trauma Rehabil. 26, 325–338 [DOI] [PubMed] [Google Scholar]
- 23.Novakovic-Agopian T., Chen A.J.W., and Rome S.R. (2007). Goal oriented attentional self-regulation (GOALS) training. Instructor and participant manual. San Francisco, CA: [Google Scholar]
- 24.Duncan J. B.urgess P., and Emslie H. (1995). Fluid intelligence after frontal lobe lesions. Neuropsychologia 33, 261–268 [DOI] [PubMed] [Google Scholar]
- 25.Duncan J., Emslie H., Williams P., Johnson R., and Freer C. (1996). Intelligence and the frontal lobe: the organization of goal-directed behavior. Cognit. Psychol. 30, 257–303 [DOI] [PubMed] [Google Scholar]
- 26.D'Zurilla T.J. and Goldfried M. (1971). Problem solving and behavior modification. J. Abnorm. Psychol. 78, 107–126 [DOI] [PubMed] [Google Scholar]
- 27.VonCramon D., Cramon G.M., and Mai N. (1991). Problem-solving deficits in brain-injured patients: a therapeutic approach. Neuropsychol. Rehabil. 1, 45–64 [Google Scholar]
- 28.Levine B., Robertson I.H., Clare L., Carter G., Hong J., Wilson B.A., Duncan J., and Stuss D.T. (2000). Rehabilitation of executive functioning: an experimental-clinical validation of goal management training. J. Int. Neuropsychol. Soc. 6, 299–312 [DOI] [PubMed] [Google Scholar]
- 29.Rath J.F., Simon D., Langenbahn D.M., Sherr R.L., and Diller L. (2003). Group treatment of problem-solving deficits in outpatients with traumatic brain injury: a randomised outcome study. Neuropsychol. Rehabil. 13, 461–488 [Google Scholar]
- 30.Levine B., Stuss D.T., Winocur G., Binns M.A., Fahy L., Mandic M., Bridges K., and Robertson I.H. (2007). Cognitive rehabilitation in the elderly: effects on strategic behavior in relation to goal management. J. Int. Neuropsychol. Soc. 13, 143–152 [DOI] [PubMed] [Google Scholar]
- 31.Nezu A.M., Nezu C.M. and D'Zurilla T. J. (2007). Solving life's problems. Springer: New York: [Google Scholar]
- 32.Chen A.J.-W., Novakovic-Agopian T., Nycum T.J., Song S., Turner G.R., Hills N.K., Rome S., Abrams G.M., and D'Esposito M. (2011). Training of goal-directed attention regulation enhances control over neural processing for individuals with brain injury. Brain 134 (Pt 5), 1541–1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Binder D., Turner G., Chen A.J.W., and Novakovic-Agopian T. (2009). The brain health education workshop: Instructor and participant training manuals, San Francisco: [Google Scholar]
- 34.Stuss D., Stethem L.L., and Pelchat G. (1998). Three tests of attention and rapid information processing: an extension. Clin. Neuropsychol. 1, 139–152 [Google Scholar]
- 35.Wechsler D. (1997). Wechsler Adult Intelligence Scale-III Manual. Psychological Corporation: San Antonio, TX; [Google Scholar]
- 36.Delis D., Kaplan E., and Kramer J. (2001). Delis-Kaplan Executive Function System. Pearson Assessment and Information: San Antonio, TX; [Google Scholar]
- 37.Heaton R.K., Miller S.W., Taylor M.J., and Grant I. (2004). Comprehensive Norms for an Expanded Halstead-Reitan Battery: Demographically Adjusted Neuropsychological Norms for African American and Caucasian Adults (HRB). Psychological Assessment Resources: Lutz, FL; [Google Scholar]
- 38.Brandt J. and Benedict R. (2001). Hopkins Verbal learning Test-revised. Professional Manual. Psychological Assessment Resources: Odessa, FL; [Google Scholar]
- 39.Benedict R. (1997). Brief Visuospatial Memory Test-Revised. Psychological Assessment Resources: Odessa, FL; [Google Scholar]
- 40.Burgess P.W., Alderman N., Forbes C., Costello A., Laure M.C., Dawson D.R., Anderson N.D., Gilbert S.J., Dumontheil I., and Channon S. (2006). The case for the development and use of “ecologically valid” measures of executive function in experimental and clinical neuropsychology. J. Int. Neuropsychol. Soc. 12, 194–209 [DOI] [PubMed] [Google Scholar]
- 41.Novakovic-Agopian T., Chen A.J.W., Rome S., Rossi A., Abrams G., D'Esposito M., Turner G., McKim R., Muir J., Hills N., and Kennedy C. (2014). Assessment of sub-components of executive functioning in ecologically valid settings: the goal processing scale. J. Head Trauma Rehabil. 29, 136–146 [DOI] [PubMed] [Google Scholar]
- 42.Malec J. (2005). The Mayo-Portland Adaptability Inventory. The Center for Outcome Measurement in Brain Injury. Available at: www.tbims.org. Accessed June10, 2018
- 43.McNair D., Lorr M., and Droppelman L. (1992). Manual for the Profile of Mood States. Educational and Industrial Testing Service, San Diego, CA: [Google Scholar]
- 44.Beck A.T., Steer R.A., and Brown G.K. (1996). The Beck Depression Inventory-II. Psychological Corporation, San Antonio, TX: [Google Scholar]
- 45.Weathers F.W., Litz B.T., Herman D., Huska J., and Keane T. (1994). The PTSD Checklist-Military Version (PCL-M). National Center for PTSD, Boston, MA: [Google Scholar]
- 46.IBM Corp. (2015). IBM SPSS Statistics for Windows, Version 23.0. IBM Corp: Armonk, NY; [Google Scholar]
- 47.Perneger T.V. (1998). What's wrong with Bonferroni adjustments. BMJ 316, 1236–1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rothman K.J. (1990). No adjustments are needed for multiple comparisons. Epidemiology 1, 43–46 [PubMed] [Google Scholar]
- 49.Savitz D.A. and Olshan A.F. (1995). Multiple comparisons and related issues in the interpretation of epidemiologic data. Am. J. Epidemiol. 142, 904–908 [DOI] [PubMed] [Google Scholar]
- 50.Field A. (2013). Discovering Statistics Using IBM SPSS Statistics. Sage: New York, NY; [Google Scholar]
- 51.Watson Peter. (2017). FAQ/Effect Size. In MRC CBSU Wiki. Available at: http://imaging.mrc-cbu.cam.ac.uk/statswiki/FAQ/effectSize. Accessed October26, 2017
- 52.Cohen J., Cohen P., West S. G., and Aiken L.S. (2013). Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Routledge: Abingdon-on-Thames, U.K; [Google Scholar]
- 53.Evans J. (2005). Can executive impairments be effectively treated? in: Effectiveness of Rehabilitation for Cognitive Deficits. P. Halligan and D. Wade (eds), Oxford University Press: New York, pps. 247–257 [Google Scholar]
- 54.Miotto E.C., Evans J.J., Souza de Lucia M.C., and Scaff M. (2009). Rehabilitation of executive dysfunction: a controlled trial of an attention and problem solving treatment group. Neuropsychol. Rehabil. 19, 517–540 [DOI] [PubMed] [Google Scholar]
- 55.Loya F., Novakovic-Agopian T., Binder D., Rossi A., Rome S., Murphy M., and Chen A. (2017). Long-term use and perceived benefits of goal-oriented attentional self-regulation (GOALS) training in chronic brain injury. Rehabil. Res. Pract. 2017, 8379347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Novakovic-Agopian T., Abrams G., Chen A., Kornblith E., Burciaga J., Carlin G., Loya F., Madore M., Marton K., Murphy M., Mayer C., and Rodriguez N. (2016) Short and long term outcomes of executive function training in veterans with chronic TBI. 9th World Congress on Neurorehabilitation, Philadelphia, PA: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.