Abstract
Background:
Adverse childhood experiences (ACEs) have life-long health consequences, yet screening remains challenging. Particularly in clinical settings, brief screeners that could lead to comprehensive assessments may be more feasible. We explore how two ACEs (economic hardship; parental/caregiver divorce/separation) are associated with other ACEs, asthma, and emotional, developmental, or behavioral (EDB) problems.
Methods:
Using the 2016 National Survey of Children’s Health, we assessed the associations between ACEs and asthma and EDB problems and calculated sensitivities, specificities and predictive values.
Results:
Parents frequently reported 1+ ACEs for their child (50.3%). Individual ACE frequency ranged from 4.2%-29.6%; all were significantly associated with EDB problems (adjusted odds ratios [aORs]: 2.2-5.1) and more ACEs confirmed higher odds. Two ACES (economic hardship; parental/caregiver divorce/separation) co-occurred frequently with other ACEs; having either predicted EDB problems similarly to other ACEs (aORs 1.8; 95% CI 1.4, 2.3) and having both greatly increased odds (aOR 3.8; 95% CI 2.8, 5.2). The negative predictive value of EDB problems associated with citing neither ACE was high (95.7%). Similar trends with asthma were observed.
Conclusions:
Economic hardship and caregiver separation are strongly associated with other ACEs, EDB problems and asthma. A brief screener including these ACEs may reduce clinical barriers to broader ACEs screening.
Introduction
There is ample evidence that adverse childhood experiences (ACEs) cause toxic stress and lead to lifelong negative health outcomes.{1-4] Almost half of all U.S. children have experienced at least one ACE,{3} with documented, detrimental effects on life-long health for those that experience two or more.{3,5-8} The American Academy of Pediatrics’ Bright Futures endorses ‘psychosocial/ behavioral assessments’ at every well child check and encourages routine screening for social/emotional, family- and/or community- factors that impact a child’s physical and emotional health, such as ACEs. However, there are no clear guidelines recommended for ACEs surveillance or screening, even though they list ACE screening within the AAP toolbox.{9-12} This lack of direction, based on preliminary evidence, underscores the importance of further translating research knowledge into prevention practices within primary care settings.{13,14}
This screening gap is due, in part, to the difficulty in defining a manageable list of items on which to screen for ACEs, a likely precursor to toxic stress, as well as understanding process and philosophical barriers to screening. The list of contributing ACEs experienced during childhood continues to grow beyond those originally identified by Felitti et.al.{8} Yet the degree to which toxic stress occurs at the individual level depends on the nature and extent of adverse experiences, environmental elements, and protective factors, making a definitive diagnosis of toxic stress elusive and screening for ACEs a challenge.{15,16} Consequently, many pediatricians are not routinely screening for ACEs in primary care, citing lack of time, discomfort in asking about the topics, and the belief that social/emotional risk factors within the family may be outside the scope of the pediatric medical home.{8,17-19}, {20} Additionally, routine screening for ACEs is problematic given that it is unclear who to ask, the parent or the child, and about whose ACEs, the parents’ or child’s.{18} Finally, implementing effective trans-disciplinary coordination to address identified ACEs has been hard to coordinate in clinical settings,{21} so clinicians understandably justify not screening when interventions and support are not easily available.
In an effort to respond to primary care provider concerns about the length of time it takes to screen and to encourage more consistent screening for social/ emotional factors, it may be worthwhile to examine the relationship between ACEs to see if any can be prioritized when asking families about risk during routine health maintenance visits.{10} To do this accurately and efficiently, one could focus on a screening program for those ACEs that are most prevalent; or on those that frequently co-occur; or on those that predict other ACEs; or on those that combine in ways that lead to increased harm. Such analyses also require measurement of proximal health outcomes, especially those that emerge during childhood, such as asthma, and emotional, developmental and behavioral outcomes.{22}
Therefore, to address clinical barriers to screening, this study examines the relationship between ACEs, asthma and persistent emotional, developmental and behavioral (EDB) problems in children using a large, national sample of parental report of diverse children in the 2016 National Survey of Children’s Health. We hypothesize that certain ACEs may occur frequently enough find significant and meaningful associations with EDB or asthma outcomes. With the high prevalence and growing list of ACEs combined with the lifelong and diverse harms caused by toxic stress, identifying an effective yet simplified series of questions may lead to more feasible and consistent screening in a clinical setting than screening for many or all ACEs.
Methods
Survey Characteristics:
We used anonymous survey data from the 2016 National Survey of Children’s Health (NSCH), a cross-sectional survey led by the Centers for Disease Control and Prevention under the direction and sponsorship of the federal Maternal and Child Health Bureau (MCHB). In 2016, the NSCH mailed invitations to households and provided participants with the option to complete the screener and questionnaire through a secure website or as a mailed, paper-based version. This is a change from previous years where the NSCH was administered by telephone. The 2016 NSCH survey includes an initial household screener followed by age-specific child-level questionnaires. Between June 2016 to January 2017, 138,009 screener questionnaires were completed to determine if there were any children 0 – 17 years old in the home. Of those screened, 67,047 households included at least one age-eligible child. Parents or guardians in those households were asked to complete the questionnaire on the one child in their household randomly selected during the screening process. A total of 50,212 survey responses were received between June 10, 2016 and February 10, 2017 (http://childhealthdata.org/learn/nsch). Data were weighted to be representative of non-institutionalized children nationally and within each state and the District of Columbia. This study was deemed exempt by the study’s Institutional Review Board as the dataset is publically available and de-identified.
Primary Exposure: Adverse Childhood Experiences
The NSCH asks parents and guardians to report whether their child experienced any of nine ACEs: (ACE1) economic hardship based on family’s income; (ACE3) parental/guardian divorce or separation; (ACE4) death of parent or guardian; (ACE5) incarceration of parent or guardian; ((ACE6) witness to domestic violence; (ACE7) witness to or victim of neighborhood violence; (ACE8) household member with mental illness; (ACE9) household member with drug/alcohol problems; and (ACE10) discrimination based on race/ethnicity. Maltreatment and neglect (ACE2) from the original ACEs study{8} were not asked in the NSCH due to the lack of reliability and inappropriateness of asking parents about these experiences electronically or on paper. Note that there is no ACE2 in the survey due to this purposeful omission.
Primary Outcome
Beyond the ACEs themselves, we chose two other primary outcomes as reported by the parent: the presence of a persistent EDB condition and current asthma. We chose EDB problems as a plausible proximal consequence of ACEs, and asthma given that it is one of the most common childhood chronic illnesses and is known to worsen with ACEs.{23} An EDB condition is defined by the caregivers’ positive responses to the following two questions: “Does [child] have any kind of emotional, developmental, or behavioral problem for which [he/she] needs treatment or counseling?” and “Has [his/her] emotional, developmental, or behavioral problem lasted or is it expected to last 12 months or longer?” These questions, part of the Children with Special Health Care Needs Screener,{24} are known to identify children who may not use traditional medical care in the same way as other children with special health care needs might.{25} Current asthma in this study was defined as positive responses to the following questions: “Has a doctor or other health care provider ever told you that this child has…Asthma?” and “Does this child currently have the condition?” Children with current asthma and/or EDB of interest for this study since it is plausible that ACEs may lead to higher associations with mental and physical conditions such as EDB problems and asthma.{23}
Study Inclusion:
The majority of NSCH survey questions were asked for all respondents, although some were age-dependent, as they divided some questions for parents of children and adolescents 6-17 years or those of infants and children less than 6 years. The authors felt this survey grouping was appropriate and chose to focus only on children and adolescents, instead of the infants and children, as the causes of EDB problems in infants and toddlers differ substantially compared to children and adolescents. As such, we included caregiver responses from all children ages 6-17 years (n=35,718) to represent a plausible situation where ACEs may be associated with asthma or EDB problems (Figure 1). Children with diagnosed EDB conditions who were likely already identified within primary care as needing intensive neurodevelopmental services were also excluded; this included caregiver report of diagnosed autism, Asperger’s Syndrome, pervasive developmental disorders, developmental delay, intellectual disability or mental retardation, Cerebral Palsy, or Tourette’s Syndrome (8.2% of the sample population).population). Of children ages 6-17 years (n=35,718), we excluded any with missing data regarding medical or developmental conditions (1.8% of the sample population) and missing questions for EDB problems (<1%). We also excluded children with missing responses for any of the nine ACEs exposures (6.6%), or demographic factors used in analyses: race, ethnicity, sex, adequate health insurance, household size, household education (defined as the highest reported education of a parent/guardian) and household income which was expressed as a percent of the Federal Poverty level (<1%). This yielded a final analytic sample of 29,450 children, (see figure 1 for further details).
Figure 1.
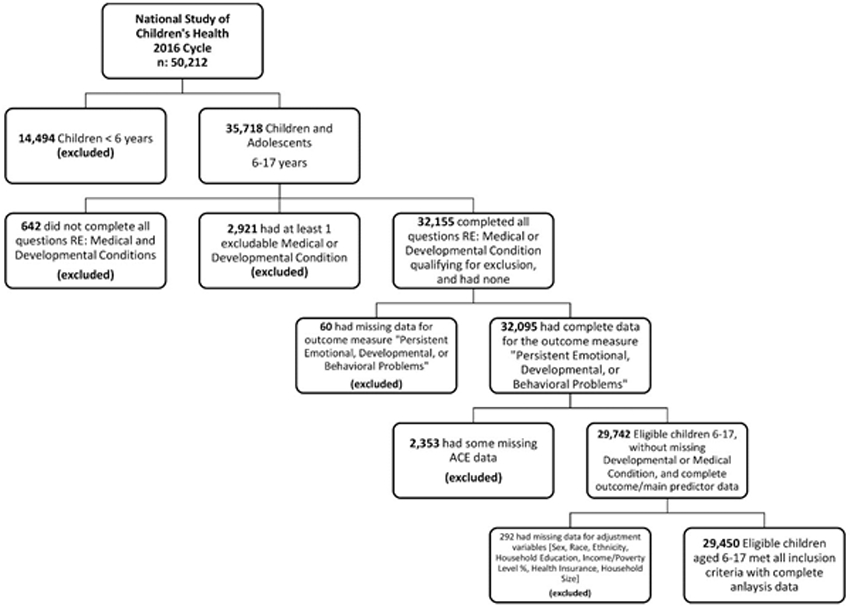
Study Sample Selection
Analytic Plan:
We used survey procedures in SAS (Version 9.4) to account for the complex design of the NSCH to interpret results as nationally representative of the US population and are presented throughout unless otherwise noted. Any numbers describing frequency of individual predictors are presented unweighted. We assessed the prevalence of each ACE individually, and by sex and racial/ethnic group. We then sought to understand the co-occurrences of ACEs, and their relationship with EDB problems and asthma. Logistic regression determined the odds of other ACEs, EDB problems or asthma using three models: unadjusted, adjusted for potential confounders and adjusted for potential confounders and all other ACEs to determine each ACE’s independent association with other ACEs, EDB and asthma outcomes. Potential confounders included age of the child in years, sex, race/ethnicity, household size, household income and household education. To protect participant anonymity, household income was not directly available in released data. Instead, income represented as % of Federal Poverty Level was available as a continuous variable ranging from <=50% to 400%+. In the final fully adjusted model, we assessed for collinearity via variance inflation factors (VIFs), with a VIF > 5 as an indication of substantial collinearity. Lastly, we examined the cumulative association with EDB problems or asthma among all ACEs, those that had significant independent associations with EDB problems or asthma and the most frequent (ACEs), again using logistic regression, adjusted for the confounders listed above. Sensitivity and specificity calculations were performed using weighted frequencies and traditional formulae to assess the screening utility of specific ACE groupings for the outcomes of asthma and EDB problems, as well as ACE1 (economic hardship) and ACE3 (parental/guardian divorce or separation) to screen for other ACEs.
Results
Overall Demographics and ACEs
Table 1 demonstrates the sample demographics, with almost equal unweighted representation of male (49.5%) and female (50.5%) children. The majority (71.3%) were non-Hispanic whites with 5.5% non-Hispanic Black and 10.8% Hispanic. All subsequent descriptives are presented weighted to be nationally representative; weights provided by the NSCH. A third (30.0%) had a household with the maximum education of high school or less. The total mean household income was 247.3% (SE=1.9) of the Federal Poverty Level with lower income percentages for non-Hispanic Black (190.7%, SE=5.1) and Hispanic (186.1%, SE=4.2) children (p <.0001). The average household size was 4.2 (SE=0.01) with higher means reported for Hispanic children (p < .0001) and there is similar prevalence of adequate health insurance across groups. Over half (50.3%) reported at least one ACE with an average lifetime ACE count of 1.02 (SE=0.02). The prevalence of ACEs varied greatly (range 4.2% to 29.6%). Two ACEs had particularly high prevalence: experienced difficulties getting by on family income (24.7%) and a parent/guardian who was divorced or separated (29.6%; see also Figure 2).
Table 1.
Distribution of ACEs and general demographics.
| Overall sample | Sex |
Race/ethnicity |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | p value | NHW | NHB | Hispanic | Other, NH | p value | |||
| N (% of total sample)a | 29,450 (100%) | 14,589 (49.5%) | 14,861 (50.5%) | 21,004 (71.3%) | 1616 (5.5%) | 3177 (10.8%) | 3653 (12.4%) | |||
| Mean age in years [Mean ± S.E.]c | 11.5 ± 0.05 | 11.5 ± 0.07 | 11.5 ± 0.07 | <0.0001 | 11.6 ± 0.05 | 11.8 ± 0.15 | 11.3 ± 0.14 | 11.2 ± 0.10 | <0.0001 | |
| Maximum household education [%, S.E.]b | ||||||||||
| Less than high school | 9.8 (0.6) | 10.0 (0.9) | 9.6 (0.9) | 0.8191 | 2.7 (0.3) | 6.8 (1.2) | 26.6 (2.0) | 8.2 (1.8) | <0.0001 | |
| High school | 20.2 (0.6) | 20.7 (0.9) | 19.7 (0.9) | 16.5 (0.5) | 25.9 (2.1) | 27.2 (1.8) | 14.7 (1.4) | |||
| Some college | 22.7 (0.5) | 22.4 (0.8) | 23.0 (0.8) | 22.1 (0.6) | 32.5 (2.0) | 20.2 (1.4) | 19.6 (1.3) | |||
| College degree or higher | 47.4 (0.7) | 46.9 (0.9) | 47.8 (1.0) | 58.7 (0.7) | 34.8 (1.8) | 26.0 (1.5) | 57.5 (1.9) | |||
| Mean income represented as % FPL [Mean ± S.E.]b, c | 247.3 ± 1.9 | 248.5 ± 2.6 | 246.2 ± 2.8 | <0.0001 | 288.0 ± 1.8 | 190.7 ± 5.1 | 186.1 ± 4.2 | 260.0 ± 5.1 | <0.0001 | |
| Household size [Mean ± S.E.]b | 4.2 ± 0.01 | 4.2 ± 0.02 | 4.2 ± 0.02 | <0.0001 | 4.2 ± 0.01 | 4.0 ± 0.04 | 4.3 ± 0.03 | 4.2 ± 0.03 | <0.0001 | |
| Adequate health insuranceb | ||||||||||
| Current insurance adequate for health needs | 67.9 (0.6) | 67.4 (0.9) | 68.4 (0.9) | 0.4395 | 67.5 (0.6) | 72.3 (1.9) | 66.1 (1.8) | 68.8 (1.7) | 0.0723 | |
| Current insurance not adequate for health needs | 32.1 (0.6) | 32.6 (0.9) | 31.6 (0.9) | 32.5 (0.6) | 27.7 (1.9) | 33.9 (1.8) | 31.2 (1.7) | |||
| Any adverse childhood experiencesb | 50.3 (0.7) | 49.6 (1.0) | 51.0 (1.0) | 0.3189 | 44.9 (0.7) | 69.4 (1.8) | 54.3 (2.0) | 45.4 (1.9) | <0.0001 | |
| ACE count [Mean ± S.E.]b | 1.02 ± 0.02 | 0.99 ± 0.03 | 1.06 ± 0.03 | <0.0001 | 0.90 ± 0.02 | 1.52 ± 0.08 | 1.07 ± 0.05 | 0.97 ± 0.07 | <0.0001 | |
| Adverse childhood experiences (ACEs) | ACE frequencya | ACE % (SE)b | ACE % (SE)b | |||||||
| ACE 1: Sometimes or very often it has been very hard to get by on your family’s income (for example, it was hard to cover the basics like food or housing) | 5449 | 24.7 (0.6) | 24.8 (0.8) | 24.7 (0.9) | 0.8909 | 21.0 (0.6) | 37.4 (2.2) | 27.0 (1.7) | 23.1 (1.8) | <0.0001 |
| ACE 3: Lived with a parent or guardian who got divorced or separated after they were born | 7638 | 29.6 (0.6) | 29.3 (0.9) | 30.0 (0.9) | 0.6009 | 27.6 (0.6) | 41.4 (2.2) | 30.5 (1.7) | 23.2 (1.6) | <0.0001 |
| ACE 4: Lived with a parent or guardian who died | 1014 | 4.2 (0.2) | 4.5 (0.4) | 3.8 (0.3) | 0.1749 | 3.5 (0.3) | 8.1 (1.1) | 3.7 (0.6) | 4.1 (0.8) | <0.0001 |
| ACE 5: Lived with a parent or guardian who served time in jail or prison in their lifetime | 1882 | 9.1 (0.4) | 8.8 (0.6) | 9.5 (0.6) | 0.4567 | 7.1 (0.4) | 17.1 (1.7) | 9.9 (1.1) | 7.9 (1.3) | <0.0001 |
| ACE 6: Saw or heard any parents, guardians, or any other adults in [his/her] home slap, hit, kick, punch, or beat each other up | 1490 | 6.4 (0.4) | 6.2 (0.5) | 6.5 (0.5) | 0.6876 | 5.4 (0.3) | 10.5 (1.7) | 6.5 (0.9) | 6.0 (0.7) | 0.0003 |
| ACE 7: Was the victim of violence or witnessed any violence in [his/her] neighborhood | 1018 | 4.5 (0.3) | 4.3 (0.4) | 4.7 (0.5) | 0.4352 | 3.0 (0.2) | 8.0 (1.2) | 5.6 (0.9) | 5.1 (0.8) | <0.0001 |
| ACE 8: Lived with anyone who was mentally ill or suicidal, or severely depressed for more than a couple of weeks | 2639 | 8.7 (0.4) | 7.9 (0.4) | 9.5 (0.6) | 0.0240 | 10.1 (0.4) | 7.2 (1.1) | 6.8 (0.9) | 8.3 (1.3) | 0.0077 |
| ACE 9: Lived with anyone who had a problem with alcohol or drugs | 2969 | 10.5 (0.4) | 9.3 (0.5) | 11.6 (0.7) | 0.0066 | 10.7 (0.4) | 9.5 (1.5) | 10.9 (1.2) | 9.0 (1.3) | 0.6408 |
| ACE 10: Was treated or judged unfairly because of [his/her] race or ethnic group | 1034 | 4.8 (0.3) | 4.3 (0.4) | 5.3 (0.5) | 0.1298 | 1.3 (0.1) | 12.8 (1.5) | 5.9 (0.9) | 10.2 (1.3) | <0.0001 |
NHW non-Hispanic, White, NHB non-Hispanic, Black, Other, NH non-Hispanic.
Unweighted.
Weighted.
% FPL is capped at 50 or below, and 400 or above.
Figure 2. Distribution of Multiple Aces; Overall Prevalence, and Row Percentages within ACEs.
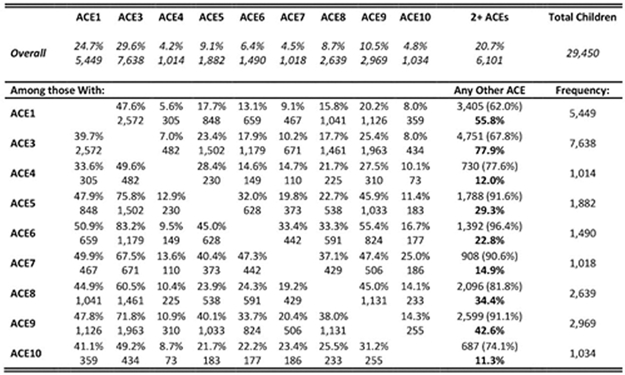
In bold: within that ACE, the number of children who screen positive for any of the other ACEs (I.e. have 2+ ACEs total), divided by the total number of children with 2+ ACEs (6,101 kids); this highlights what proportion of those children with 2+ ACEs we “catch” within that particular ACE For example: Row ACE1 – Among all the children with ACE1, we catch 55.8% of all children with 2+ ACEs (Figure 2, unweighted)
ACE KEY: ACE 1: income instability; There is no ACE 2; ACE 3: parent/guardian divorced/ separated; ACE 4: parent or guardian death; ACE 5: parent or guardian who served time in jail or prison; ACE 6: witness to domestic violence; ACE 7: victim of violence or witnessed any violence in neighborhood; ACE 8: live with anyone with mental illness or suicidality; ACE 9: live with anyone who used alcohol or drugs; ACE 10: treated or judged unfairly because of [his/her] race or ethnic group.
There were notable differences in prevalence of certain ACEs by sex of the child as well as race and ethnicity. Parents and guardians in the sample reported that females were more likely to live with someone who had problems with alcohol and drugs (11.6% vs 9.3%, p=0.0066) and to live with someone with mental health conditions (9.5% vs 7.9%, p=0.0240). Relative to non-Hispanic white children, Hispanic children and non-Hispanic Black children had higher caregiver-reported rates for ACEs 1, 3, 5, 6, 7 and 10 (p<.0001). Non-Hispanic Black children also had about two times the rates of having lived with a parent or guardian who died (ACE4) compared to other groups. Children identified as non-Hispanic ‘other’ were reported as having higher rates for racial/ethnic discrimination, similar to non-Hispanic Black children.
Screening for Other ACES, Asthma and EDB Problems
Figure 2 illustrates the relative prevalence of co-occurring ACEs. Visual inspection shows that both ACE 1 and ACE 3 co-occur more than a third of the time with all of the other ACEs. ACE 3 co-occurs at very high rates with ACEs 5, 6 and 9. Importantly, having either ACE 1 or ACE3 leads to a high likelihood of having any other ACE (55.8% and 77.9% respectively) with the highest absolute population affected.
Table 2 illustrates the screening statistics of combinations of ACE screening options as they associate with other ACEs, EDB and asthma. With respect to associations with the health outcomes of interest, having any one of the nine available ACEs yielded the highest sensitivity of 73.4% (specificity, 51.3%) for EDB and 63.2% (specificity 51.1%) for asthma. Using a commonly used criterion of two or more ACEs yielded a sensitivity of 51.9 % (specificity, 76.6%) for EDB and 36.8% (76.0%) for asthma. A criterion of at least one of ACE1 or ACE3 yielded slightly higher sensitivities but lower specificities: 62.5% (58.8%) for EDB and 55.2% (58.8%) for asthma. Notably, ACE1 and ACE3, either having experienced one or both, were found to be effective screeners for other ACEs with a relatively high sensitivity of 71.2%. Specificity was highest when both ACE1 and ACE 3 were positive for any other ACE (93.9%), but was also high for EDB problems (89.3%) and asthma (88.8%). Having either only ACE1 or ACE3 had low sensitivities for outcomes, though generally good specificities (69.8-74.1%) with its highest utility as a means of ‘ruling out’ the need for further screening with an NPV above 90% for both EDB and Asthma (93.9%, 91.2% respectively), and still high for other ACEs (78.3%). The ability of ACE 1 and/or ACE 3 to positively predict other ACEs was adequate, but had a strong negative predictive value.
Table 2.
Sensitivity and specificity of the ACE screener on EDB and asthma.
| ACE screener tool | Outcome | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|
| ACE 1 or 3 or both | Any other ACE | 71.2 | 68.0 | 45.0 | 86.5 |
| EDB problems | 62.5 | 58.8 | 9.5 | 95.7 | |
| Asthma | 55.2 | 58.8 | 12.7 | 92.3 | |
| ACE 1 and 3 | Any other ACE | 27.1 | 93.9 | 61.9 | 77.8 |
| EDB problems | 27.0 | 89.3 | 14.9 | 94.6 | |
| Asthma | 17.0 | 88.8 | 14.3 | 90.8 | |
| ANY ACEs (of all 9) | EDB problems | 73.4 | 51.3 | 9.5 | 96.5 |
| Asthma | 63.2 | 51.1 | 12.4 | 92.7 | |
| 2+ ACES (of all 9) | EDB problems | 51.9 | 76.6 | 13.4 | 95.8 |
| Asthma | 36.8 | 76.0 | 14.3 | 91.7 | |
| 3+ ACES (of all 9) | EDB problems | 35.1 | 88.7 | 17.8 | 95.2 |
| Asthma | 19.9 | 87.9 | 15.2 | 91.0 | |
| Any other ACE | EDB problems | 54.2 | 75.0 | 13.1 | 95.9 |
| Asthma | 37.0 | 74.2 | 13.5 | 91.5 |
ACE KEY: ACE 1: income instability; there is no ACE 2; ACE 3: parent/guardian divorced/separated; ACE 4: parent or guardian death; ACE 5: parent or guardian who served time in jail or prison; ACE 6: witness to domestic violence; ACE 7: victim of violence or witnessed any violence in neighborhood; ACE 8: live with anyone with mental illness or suicidality; ACE 9: live with anyone who used alcohol or drugs; ACE 10: treated or judged unfairly because of [his/her] race or ethnic group.
ACEs and Emotional, Developmental and Behavioral Problems in Childhood and Asthma
Table 3 summarizes the distribution of ACEs and groupings on persistent emotional, developmental and behavioral (EDB) problems in children and adolescents. The total study population had an overall prevalence of 6.5% of children with caregiver-reported EDB problems (95% CI 5.9, 7.1) and each ACE conferred an increased prevalence of EDB problems (range 10.7-23.6%). We present three sets of models of the odds of persistent EDB problems. The first model provides the unadjusted odds ratio quantifying the association with each ACE and EDB problems, with odds ratios ranging from 2.2-5.1 (all p < .05). The second set of models provides odds ratios adjusted for sex, race/ethnicity, age, household income as percent federal poverty level, household size and household education (aOR). Adjustment for these potential confounders did not substantially change the odds ratios for any of the ACEs (aORs range 1.9-4.8, all p<.05). The third and final model included all aforementioned potential confounders and all other ACEs as covariates to ascertain each ACE’s independent association with EDB problems. These calculations revealed that five ACEs (1, 3, 7, 8 and 9) remained significantly associated with EDB problems (aOR range 1.3-2.2). ACE 5 maintained a positive independent association (aOR = 1.4; 95% CI = (1.0, 1.9)) but was not statistically significant, potentially due to a smaller frequency of children exposed to this ACE. Collinearity was not observed (VIF’s < 2) in this final model.
Table 3.
Distribution of ACEs and ACE groupings, rates and odds of persistent emotional, developmental and behavioral problems in children and adolescents.
| N (%)a,b | Persistent EDB problemsa | Odds ratios (95% CI)a,c,d |
|||
|---|---|---|---|---|---|
| Unadjusted | Adjustede | Adjustede for all ACEs | |||
| Overall | 6.5 (5.9, 7.1) | ||||
| ACE 1: Sometimes or very often it has been very hard to get by on your family’s income (e.g., it was hard to cover the basics like food or housing) | 5449 (24.7) | 10.7 (9.2, 12.3) | 2.2 (1.8, 2.7) | 2.1 (1.7, 2.6) | 1.6 (1.3, 2.0) |
| ACE 3: Lived with a parent or guardian who got divorced or separated after they were born | 7638 (29.6) | 10.7 (9.3, 12.0) | 2.4 (2.0, 2.9) | 2.2 (1.8, 2.7) | 1.3 (1.1, 1.7) |
| ACE 4: Lived with a parent or guardian who died | 1014 (4.2) | 13.1 (9.7, 16.5) | 2.3 (1.7, 3.1) | 1.9 (1.4, 2.7) | 1.3 (0.9, 1.9) |
| ACE 5: Lived with a parent or guardian who served time in jail or prison in their lifetime | 1882 (9.1) | 15.0 (12.1, 17.9) | 3.0 (2.3, 3.8) | 2.7 (2.1, 3.6) | 1.4 (1.0, 1.9) |
| ACE 6: Saw or heard any parents, guardians, or any other adults in [his/her] home slap, hit, kick, punch, or beat each other up | 1490 (6.4) | 18.3 (14.4. 22.1) | 3.7 (2.8, 4.9) | 3.3 (2.5, 4.4) | 1.2 (0.8, 1.7) |
| ACE 7: Was the victim of violence or witnessed any violence in [his/her] neighborhood | 1018 (4.5) | 23.6 (17.6, 29.5) | 5.1 (3.6, 7.2) | 4.8 (3.4, 6.7) | 2.2 (1.4, 3.5) |
| ACE 8: Lived with anyone who was mentally ill or suicidal, or severely depressed for more than a couple of weeks | 2639 (8.7) | 19.2 (16.1, 22.3) | 4.2 (3.4, 5.3) | 4.0 (3.2. 5.0) | 2.2 (1.7, 2.9) |
| ACE 9: Lived with anyone who had a problem with alcohol or drugs | 2969 (10.5) | 16.6 (13.7, 19.5) | 3.5 (2.8, 4.5) | 3.4 (2.7, 4.3) | 1.4 (1.1, 1.8) |
| ACE 10: Was treated or judged unfairly because of [his/her] race or ethnic group | 1034 (4.8) | 14.2 (9.5, 18.8) | 2.5 (1.7, 3.7) | 2.6 (1.7, 3.7) | 1.3 (0.9, 1.9) |
| N (%)a,b | Persistent EDB problemsa |
Odds ratios (95% CI)a,d |
|||
| Unadjusted | Adjustede | ||||
| Dose–response relationship | |||||
| Among all nine ACEs | |||||
| REF: No ACEs | 16,572 (49.7) | 3.5 (2.9, 4.0) | — | — | |
| 1 ACE | 6777 (25.0) | 5.6 (4.6, 6.6) | 1.6 (1.3, 2.1) | 1.7 (1.3, 2.2) | |
| 2 ACEs | 3013 (12.4) | 8.8 (7.0, 10.6) | 2.7 (2.0, 3.5) | 2.8 (2.0, 3.7) | |
| 3 ACEs | 1439 (5.6) | 11.7 (9.1, 14.4) | 3.7 (2.7, 5.0) | 3.9 (2.8, 5.5) | |
| 4+ ACEs | 1649 (7.3) | 22.4 (18.3, 26.6) | 8.0 (6.0, 10.7) | 8.6 (6.2, 11.9) | |
| Comparability of ACE groups | |||||
| Among all nine ACEs | |||||
| REF: No ACEs | 16,572 (49.7) | 3.5 (2.9, 4.0) | — | — | |
| Any ACEs | 12,878 (50.3) | 9.5 (8.6, 10.5) | 2.9 (2.4, 3.6) | 2.8 (2.3, 3.5) | |
| Among all nine ACEs | |||||
| REF: No ACEs | 16,572 (49.7) | 3.5 (2.9, 4.0) | — | — | |
| 1 ACE | 6777 (25.0) | 5.6 (4.6, 6.7) | 1.6 (1.3, 2.1) | 1.7 (1.3, 2.3) | |
| 2 ACEs | 3013 (12.4) | 8.8 (7.0, 10.6) | 2.7 (2.0, 3.5) | 2.7 (2.0, 3.7) | |
| 3+ ACEs | 3088 (12.9) | 17.8 (15.2, 20.4) | 6.0 (4.7, 7.7) | 6.4 (4.8, 8.5) | |
| Among FIVE ACEs which had significant independent effects | |||||
| REF: None of these five ACEs | 17,430 (53.1) | 3.6 (3.1, 4.2) | — | — | |
| 1 ACE | 7063 (27.1) | 6.1 (5.1, 7.1) | 1.7 (1.4, 2.2) | 1.8 (1.4, 2.3) | |
| 2 ACEs | 3022 (12.0) | 10.4 (8.5, 12.4) | 3.1 (2.4, 4.0) | 3.1 (2.3, 4.1) | |
| 3 ACEs | 1935 (7.8) | 21.4 (17.6, 25.2) | 7.2 (5.5, 9.5) | 7.4 (5.4, 10.0) | |
| Among ACE 1 and ACE 3 | |||||
| REF: Neither of these ACEs | 18,935 (57.4) | 4.3 (3.7, 4.9) | — | — | |
| 1 ACE | 7943 (30.8) | 7.5 (6.5, 8.5) | 1.8 (1.5, 2.2) | 1.8 (1.4, 2.3) | |
| 2 (both) ACEs | 2572 (11.8) | 14.9 (12.2, 17.7) | 3.9 (3.0, 5.1) | 3.8 (2.8, 5.2) | |
Weighted.
Within row.
Referent category: Those without that particular ACE.
Odds ratios in bold indicate statistical significance (p < 0.05).
Adjusted for: Sex, race/ethnicity, maximum household education, age, household size and income as % of poverty level (Caps: Min = 50, Max = 400).
Table 3 also describes the dose-response relationship of ACEs as well as how ACE groups compare. Increasing numbers of ACEs were significantly associated in a dose-response pattern with higher odds of EDB problems, for both the unadjusted and the adjusted odds ratios. For example, having any one ACE yielded an aOR 1.7 (1.3, 3.2) yet four or more ACEs yielded an aOR of 8.6 (6.2, 11.9). When limiting to only the five ACEs that were independently associated with EDB problems as described above, the same dose-dependent relationship exists, reflecting increasing odds of EDB for increasing numbers of ACEs. Having one of these five ACEs yielded an aOR of 1.8 (1.4, 2.3) and having 3+ ACEs quadrupled this association to aOR 7.4 (5.4, 10.0). Finally, drawing on the dominant prevalence of ACE1 (economic hardship) and ACE3 (caregiver divorce/separation), limiting the analysis to only these two ACEs again revealed the same pattern of increased odds for EDB problems. Examining only ACE 1 and ACE 3, which affected the greatest number of children experiencing ACEs, having either ACE conferred a similar association with EDB problems (aOR 1.8, 95% CI 1.4, 2.3) and having both quadrupled the odds of having an EDB problem (aOR 3.8, 95% CI 2.8, 5.2).
Table 4 illustrates the outcomes for children who have ever been diagnosed with asthma and those whose parents or guardians cite current asthma. There is an overall prevalence of 9.8% of the population with current asthma (95% CI 9.0, 10.6). Similar to EDB problems, the dose-repose effects of ACEs were significantly associated with higher odds of having asthma. After adjusting for all ACEs and potential confounders, ACE1 (aOR: 1.5; 95% CI 1.2, 1.9) and ACE8 (aOR: 1.6; 95% CI 1.1, 2.3) were independently associated with current asthma. In terms of the additive or dose-response relationship, having three or more ACEs yielded an aOR or 1.9 (95% CI 1.4, 2.7) compared to no ACEs. Children with exposure to both ACE1 and ACE8 were 2.2 times as likely (95% CI 1.4, 3.5) for the caregiver to report current asthma.
Table 4.
As secondary outcome analysis, we investigated the rates of ever or current asthma, and odds of current asthma within our cohort among those with non-missing data.
| N (%)d | Asthma |
Odds ratios for current asthma (95% CI)c,e |
||||
|---|---|---|---|---|---|---|
| Ever | Current | Unadjusted | Adjustedc | Adjustedc for all ACEs |
||
| Overall: N = 29,186a | 4214 (14.6, [13.7, 15.5])b | 2691 (9.8 [9.0, 10.6])b | ||||
| ACE 1: Sometimes or very often it has been very hard to get by on your family’s income, (for example, it was hard to cover the basics like food or housing) | 5394 (24.7) | 19.6 (17.4, 21.9) | 14.5 (12.5, 16.6) | 1.9 (1.5, 2.3) | 1.6 (1.3, 2.1) | 1.5 (1.2, 1.9) |
| ACE 3: Lived with a parent or guardian who got divorced or separated after they were born | 7544 (29.6) | 17.9 (16.0, 19.8) | 11.9 (10.3, 13.5) | 1.4 (1.1, 1.7) | 1.1 (0.9, 1.4) | 1.0 (0.8, 1.2) |
| ACE 4: Lived with a parent or guardian who died | 1006 (4.2) | 21.3 (15.7, 26.9) | 13.5 (9.1, 17.8) | 1.5 (1.0, 2.2) | 1.2 (0.8, 1.7) | 1.1 (0.7, 1.6) |
| ACE 5: Lived with a parent or guardian who served time in jail or prison in their lifetime | 1857 (9.1) | 21.3 (16.9, 25.7) | 14.6 (10.6, 18.5) | 1.6 (1.2, 2.3) | 1.4 (0.9, 2.0) | 1.2 (0.8, 1.8) |
| ACE 6: Saw or heard any parents, guardians, or any other adults in [his/her] home slap, hit, kick, punch, or beat each other up | 1473 (6.4) | 18.4 (14.7, 22.0) | 13.6 (10.3, 16.9) | 1.5 (1.1, 2.0) | 1.3 (0.9, 1.7) | 1.0 (0.6, 1.5) |
| ACE 7: Was the victim of violence or witnessed any violence in [his/her] neighborhood | 1006 (4.5) | 20.0 (14.9, 25.0) | 14.0 (9.8, 18.3) | 1.5 (1.1, 2.2) | 1.2 (0.9, 1.8) | 0.9 (0.6, 1.4) |
| ACE 8: Lived with anyone who was mentally ill or suicidal, or severely depressed for more than a couple of weeks | 2617 (8.7) | 21.8 (17.8, 25.8) | 15.4 (11.5, 19.3) | 1.8 (1.3, 2.4) | 1.8 (1.3, 2.4) | 1.6 (1.1, 2.3) |
| ACE 9: Lived with anyone who had a problem with alcohol or drugs | 2941 (10.5) | 18.4 (15.1, 21.8) | 12.8 (9.7, 15.9) | 1.4 (1.0, 1.9) | 1.3 (1.0, 1.8) | 1.0 (0.7, 1.4) |
| ACE 10: Was treated or judged unfairly because of [his/her] race or ethnic group | 1022 (4.8) | 22.1 (16.4, 27.8) | 16.7 (11.4, 22.0) | 1.9 (1.3, 2.8) | 1.6 (1.1, 2.4) | 1.4 (1.0, 2.1) |
| N (%)d | Asthma |
Odds ratios for current asthma (95% CI)c,e |
||||
| Ever | Current | Unadjusted | Adjustedc | |||
| Dose response relationship | ||||||
| Among all nine ACEs | ||||||
| REF: No ACEs | 16,441 (49.8) | 11.2 (10.2, 12.3) | 7.3 (6.4, 8.2) | — | — | |
| 1 ACE | 6710 (25.0) | 15.2 (13.2, 17.1) | 10.4 (8.6, 12.2) | 1.5 (1.2, 1.9) | 1.3 (1.0, 1.7) | |
| 2 ACEs | 2981 (12.4) | 19.8 (16.9, 22.7) | 13.4 (11.0, 15.7) | 2.0 (1.5, 2.5) | 1.6 (1.2, 2.2) | |
| 3 ACEs | 1426 (5.6) | 23.6 (18.8, 28.5) | 15.6 (11.4, 19.9) | 2.4 (1.7, 3.3) | 2.0 (1.4, 3.0) | |
| 4+ ACEs | 1628 (7.3) | 20.0 (15.7, 24.3) | 15.0 (10.9, 19.1) | 2.2 (1.6, 3.2) | 1.9 (1.3, 2.8) | |
| Comparability of ACE groups | ||||||
| Among all nine ACEs | ||||||
| REF: No ACEs | 16,441 (49.8) | 11.2 (10.2, 12.3) | 7.3 (6.4, 8.2) | — | — | |
| ANY ACEs | 12,745 (50.2) | 17.9 (16.5, 19.4) | 12.4 (11.1, 13.7) | 1.8 (1.5, 2.2) | 1.5 (1.2, 1.9) | |
| Among all nine ACEs | ||||||
| REF: No ACEs | 16,441 (49.8) | 11.2 (10.2, 12.3) | 7.3 (6.4, 8.2) | — | — | |
| 1 ACE | 6710 (25.0) | 15.2 (13.2, 17.1) | 10.4 (8.6, 12.2) | 1.5 (1.2, 1.9) | 1.3 (1.0, 1.7) | |
| 2 ACEs | 2981 (12.4) | 19.8 (16.9, 22.7) | 13.4 (11.0, 15.7) | 2.0 (1.5, 2.5) | 1.6 (1.2, 2.2) | |
| 3+ ACEs | 3054 (12.8) | 21.6 (18.3, 24.8) | 15.3 (12.3, 18.2) | 2.3 (1.8, 3.0) | 1.9 (1.4, 2.7) | |
| Among ACE1 and ACE8 which had significant independent effects | ||||||
| REF: None of these ACEs | 22,204 (70.5) | 12.5 (11.5, 13.5) | 7.9 (7.1, 8.7) | — | — | |
| 1 ACE | 5953 (25.6) | 18.9 (16.8, 21.1) | 14.1 (12.1, 16.1) | 1.9 (1.6, 2.3) | 1.7 (1.4, 2.1) | |
| 2 (Both) ACEs | 1029 (3.9) | 24.4 (18.3, 30.4) | 17.1 (11.3, 22.9) | 2.4 (1.6, 3.7) | 2.2 (1.4, 3.5) | |
Presented are weighted percentages and 95% confidence intervals unless otherwise noted with superscript b.
264 participants refused or had incomplete/missing data regarding asthma, this is 0.90% of the full sample (N = 29,450), and will not drastically alter the distribution of demographics or ACEs.
Unweighted N, weighted percent and 95% confidence interval.
Adjusted for: Sex, race/ethnicity, maximum household education, age, household size and income as % of poverty level (caps: Min = 50, Max = 400).
Within row.
Odds ratios in bold indicate statistical significance (p < 0.05).
Discussion
This analysis of a national survey confirms the dose-dependent harm that ACEs confer {2,26-28} for childhood emotional, developmental and behavioral problems and asthma. It also shows that the two most prevalent ACEs (ACE1, economic hardship, and ACE3, parent/caregiver divorce or separation) are strongly associated with occurrence of other ACEs and thus may make strategic screening for children in need of additional support or evaluation more feasible. The absence of these two ACEs is also significant in ruling out the need for further evaluation to detect additional ACEs, physical or mental conditions. This approach is in keeping with the current recommendation by Dube, (2018), who recommends a pragmatic conceptualization of surveillance and/or screening for ACEs.{14} Our study confirms the full 9-item screener is the most comprehensive and sensitive means of evaluation, although given the high negative predictive value, asking only about parental/caregiver divorce or separation and family income instability could be part of an initial brief screener to identify those patients at greater risk for additional ACEs or emotional/physical conditions. This study shows that children and families could possibly be more easily screened to receive targeted in-depth evaluation for possible toxic stress as well as be prospectively identified for their higher likelihood of worse asthma symptoms and emotional, developmental and behavioral problems.{14} This research joins a robust and growing literature on the associations of ACEs with health outcomes, and it adds significantly to the literature for its use of a newly released dataset with statistical techniques that isolate and possibly reduce the number of questions needed to identify patients at risk for ACEs using a focused screening process. This study bridges the gap between confirming the associations of ACEs with poor health outcomes, in this case, asthma and EDB problems, but also suggests a path forward where scalable screening in primary care may be possible given that two ACEs are associated with so many other ACEs.
However, moving from ACEs research to systematic screening is not straightforward given debates on how best to characterize the gamut of child adversities. If a screener could ideally include all possible adverse experiences a child might potentially encounter, it would become a gold standard and as such many advocate for expanding the number of questions for screening to approach this goal. {5-7} However, this is not the first study to suggest that a comprehensive screener may not be necessary. Prospective studies are emerging, confirming the additive effect of multiple ACEs on stress responses irrespective of which combination of precipitating stresses had occured.{29} Existing literature also supports aggregating questions as both valid and reliable because ACEs frequently co-occur and thus reflect cumulative psychosocial risk.{7,10,30} One study even noted that including a question about socioeconomic status (similar to ACE1, experiencing economic hardship) improved the predictive validity of ACE screening even when reducing the overall number of questions.{30} Another study of ACEs screening in adults used a simplified scoring that groups ACEs together,{10} although with different items than what emerged in this study of children. Additionally, while many screening tools exist, none was specifically designed for children, and often bridge concepts like social determinants of health or focus only on a single sentinel adverse experience.{6,31,32} Finally, many screeners currently available (although not necessarily systematically implemented) have overlapping themes, such as the food insecurity item endorsed specifically by the American Academy of Pediatrics,{33} and screening for developmental delays. Future research will need to compare and streamline questions, particularly how each question is worded, to thoroughly and efficiently capture the stressors that children and their families face.
Importantly, just asking parents about two ACEs (economic hardship and caregiver separation/divorce) appears to be nearly as effective as inquiring about all nine non-maltreatment/neglect ACEs as a means of screening out children who are at very low risk of chronic physical and mental health problems. For those who screen positively, appropriate tailored follow-up could then occur, reducing the burden of an in-depth screening of all children. A brief two-question approach matches well with clinical capacity in the primary care or population health settings where patient flow is typically high. Those who respond affirmatively to one or both of these two ACEs could receive additional ACEs screening or in-depth counseling as well as referral to support services. While most of the ACEs in the NSCH were significantly associated with asthma and EDB problems and convey cumulative associations, these two ACEs combined were associated with a four-fold increased odd of persistent EDB problems, and an excellent predictive value for occurrence of other ACEs, as well as an excellent “rule-out” tool for EDB with a near 95% NPV. While adding another tool for screening into primary care can be difficult due to the minimal time providers have to address the diverse demands of screening, prevention, anticipatory guidance and current and chronic medical conditions, the potential reduction in childhood adversities and lifelong age-related disease makes screening for ACEs justifiable and much needed. Given the negative predictive value of asking only two fairly routine questions, combined with minimal expense or discomfort to providers and relative ease to administer, we believe implementation of an initial two-question brief ACE screener consisting of only these two ACEs questions may efficiently start the process of systematically screening for childhood adversity.
Together, these findings may help resolve the conundrum of implementing ACEs screening in public health and primary care settings. Given that comprehensive ACEs screening is important but difficult to implement, perhaps asking just a few questions can help identify those children who could benefit from a more in-depth investigation into their health and well-being. Beginning with fewer questions may also increase the number of primary care physicians and other child health care providers who regularly screen for ACEs. Increased screening capacity could enable population level surveillance for this important public health issue. The findings in this study do not negate the importance of screening for all ACEs but may help move research knowledge into practice to begin routine screening for social/emotional factors by simplifying the process. Having a simplified screener, especially if performed pre-visit, may help to identify and track children longitudinally who may be at increased risk for having physical or emotional, developmental and behavioral problems.
Several limitations merit discussion. First, this national survey is cross-sectional, based solely on parent report, and cannot confirm causality, directionality or directly estimate risk. As true of any large survey, the NSCH acknowledges possible response bias, but seeks to mitigate this through its careful weighting structure that we mirror in this analysis and its ability to offer Spanish language options. Nonetheless, our findings may be an underrepresentation of findings given that populations most at risk, especially those at risk for economic hardship (ACE1) may be underrepresented in the national survey. Current evidence, however, prospectively demonstrates an association between ACEs and EDB problems{22} and how some positive interventions may mitigate the negative associations of ACEs on asthma onset.{34} Additionally, this survey purposely avoids asking parents about physical and sexual abuse, since parents may not answer honestly if they are the perpetrator and survey administrators would be unable to intervene as answers are provided via paper or electronically. Future prospective studies may be able to link to diagnoses of child abuse, arguably the most extreme experience of childhood adversity. This study additionally may be underestimating the magnitude of asthma and EDB problems associated with ACE exposures since by age 17, children may not have had sufficient time to demonstrate the harmful effects of ACEs through EDB problems. Also, asking parents about ACEs may reflect their own stress, and not that of the child, although parental and child stress are intertwined. Further, it is plausible that we missed residual confounders that explain our observed associations. Finally, we only examined asthma and EDB problems, and not the myriad intermediate- and long-term poor health outcomes associated with ACEs, such as increased lifelong risks of cardiovascular disease and cancer, and intergenerational risks like poor pregnancy outcomes.{35} Nonetheless, the literature suggests the impact of toxic stress, such as ACEs,, does not differentiate the sources of stress,{29,36} affirming the approach that screening for two common ACEs may identify children at risk for having other ACEs, and health complications such as asthma or EDB problems that warrant further screening and intervention.
In conclusion, we believe that these data support the possible implementation of an initial brief ACE screener, as we found that two common ACEs are strongly associated with other ACEs, warranting this a valuable first step to in-depth screening. With evidence-based simplification of screening, pediatricians and other child health providers might be more likely to universally screen and implement support services for those children and families who most need them and might otherwise elude identification for services. While this will require a prospective study and a transdisciplinary approach,{37} this simplified process asks about only two ACEs: income insecurity and parental/guardian separation or divorce. Some may argue that limiting questioning to two ACEs will miss some children, but this process offers a streamlined way to begin in clinical and public health settings, thus increasing the likelihood that more children will be screened and able to be identified. To begin to address the toxic stress that many children endure, future studies need to understand how parents in clinical settings answer these ACE questions, and compare the effectiveness of screening for all ACEs to this simplified process as a surveillance tool or a stand-alone screener in general and high-risk populations.
Acknowledgments
Statement of Financial Support: Funding for this study was covered in part by the Child Health Research Acceleration Through Multisite Planning Pilot funding and the UC Irvine grant UL1 TR001414 and the Children’s National grant UL1TR001876.
Footnotes
Disclosure Statement: The authors have no financial relationships relevant to this article to disclose.
Category of Study: Population study
Bibliography
- 1.Palusci VJ. Adverse childhood experiences and lifelong health. JAMA Pediatrics 2013;167:95–6. [DOI] [PubMed] [Google Scholar]
- 2.Nurius PS, Green S, Logan-Greene P, Borja S. Life course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse Negl 2015;45:143–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bethell C, Gombojav N, Solloway M, Wissow L. Adverse Childhood Experiences, Resilience and Mindfulness-Based Approaches: Common Denominator Issues for Children with Emotional, Mental, or Behavioral Problems. Child Adolesc Psychiatr Clin N Am 2016;25:139–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bethell CD, Newacheck P, Hawes E, Halfon N. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health Aff (Millwood) 2014;33:2106–15. [DOI] [PubMed] [Google Scholar]
- 5.Finkelhor D, Shattuck A, Turner H, Hamby S. A revised inventory of Adverse Childhood Experiences. Child Abuse Negl 2015;48:13–21. [DOI] [PubMed] [Google Scholar]
- 6.Greeson JK, et al. Traumatic childhood experiences in the 21st century: broadening and building on the ACE studies with data from the National Child Traumatic Stress Network. J Interpers Violence 2014;29:536–56. [DOI] [PubMed] [Google Scholar]
- 7.Ford DC, et al. Examination of the Factorial Structure of Adverse Childhood Experiences and Recommendations for Three Subscale Scores. Psychol Violence 2014;4:432–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Felitti VJ, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998;14:245–58. [DOI] [PubMed] [Google Scholar]
- 9.Fuller-Thomson E, Sawyer JL. Is the cluster risk model of parental adversities better than the cumulative risk model as an indicator of childhood physical abuse?: findings from two representative community surveys. Child Care Health Dev 2014;40:124–33. [DOI] [PubMed] [Google Scholar]
- 10.Wade R Jr., Becker BD, Bevans KB, Ford DC, Forrest CB. Development and Evaluation of a Short Adverse Childhood Experiences Measure. Am J Prev Med 2017;52:163–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Academy of Pediatrics. Recommendations for Preventive Pediatric Health Care. Chicago: American Academy of Pediatrics; 2017:https://www.aap.org/en-us/documents/periodicity_schedule.pdf. [Google Scholar]
- 12.Bethell CD, Simpson LA, Solloway MR. Child Well-being and Adverse Childhood Experiences in the United States. Acad Pediatr 2017;17:S1–S3. [DOI] [PubMed] [Google Scholar]
- 13.Garner AS, Shonkoff JP. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics 2012;129:e224–31. [DOI] [PubMed] [Google Scholar]
- 14.Dube SR. Continuing conversations about adverse childhood experiences (ACEs) screening: A public health perspective. Child Abuse Negl 2018;85:180–4. [DOI] [PubMed] [Google Scholar]
- 15.Thompson R, et al. Trajectories of Adverse Childhood Experiences and Self-Reported Health at Age 18. Acad Pediatr 2015;15:503–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finkelhor D Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse Negl 2018;85:174–9. [DOI] [PubMed] [Google Scholar]
- 17.Bright MA, Thompson L, Esernio-Jenssen D, Alford S, Shenkman E. Primary Care Pediatricians' Perceived Prevalence and Surveillance of Adverse Childhood Experiences in Low-Income Children. J Health Care Poor Underserved 2015;26:686–700. [DOI] [PubMed] [Google Scholar]
- 18.Szilagyi M, et al. Factors Associated With Whether Pediatricians Inquire About Parents' Adverse Childhood Experiences. Acad Pediatr 2016;16:668–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dubowitz H, Feigelman S, Lane W, Kim J. Pediatric primary care to help prevent child maltreatment: the Safe Environment for Every Kid (SEEK) Model. Pediatrics 2009;123:858–64. [DOI] [PubMed] [Google Scholar]
- 20.Kerker BD, et al. Do Pediatricians Ask About Adverse Childhood Experiences in Pediatric Primary Care? Acad Pediatr 2016;16:154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ford DE. The Community and Public Well-being Model: A New Framework and Graduate Curriculum for Addressing Adverse Childhood Experiences. Acad Pediatr 2017;17:S9–S11. [DOI] [PubMed] [Google Scholar]
- 22.Hunt TK, Slack KS, Berger LM. Adverse childhood experiences and behavioral problems in middle childhood. Child Abuse Negl 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wing R, Gjelsvik A, Nocera M, McQuaid EL. Association between adverse childhood experiences in the home and pediatric asthma. Ann Allergy Asthma Immunol 2015;114:379–84. [DOI] [PubMed] [Google Scholar]
- 24.Bethell CD, Read D, Stein RE, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr 2002;2:38–48. [DOI] [PubMed] [Google Scholar]
- 25.Mental health in the United States: health care and well being of children with chronic emotional, behavioral, or developmental problems--United States, 2001. MMWR Morb Mortal Wkly Rep 2005;54:985–9. [PubMed] [Google Scholar]
- 26.Bjorkenstam E, Hjern A, Mittendorfer-Rutz E, Vinnerljung B, Hallqvist J, Ljung R. Multi-exposure and clustering of adverse childhood experiences, socioeconomic differences and psychotropic medication in young adults. PLoS One 2013;8:e53551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse Negl 2010;34:454–64. [DOI] [PubMed] [Google Scholar]
- 28.Brown DW, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med 2009;37:389–96. [DOI] [PubMed] [Google Scholar]
- 29.Danese A, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med 2009;163:1135–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatr 2013;167:70–5. [DOI] [PubMed] [Google Scholar]
- 31.Masten AS, Narayan AJ. Child development in the context of disaster, war, and terrorism: pathways of risk and resilience. Annu Rev Psychol 2012;63:227–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rutter ML. Psychosocial adversity and child psychopathology. Br J Psychiatry 1999;174:480–93. [DOI] [PubMed] [Google Scholar]
- 33.The Pediatrician’s Role in Optimizing School Readiness. Pediatrics 2016;138:e20162293. [DOI] [PubMed] [Google Scholar]
- 34.Abarca NE, Garro AC, Pearlman DN. Relationship between breastfeeding and asthma prevalence in young children exposed to adverse childhood experiences. J Asthma 2018:1–10. [DOI] [PubMed] [Google Scholar]
- 35.Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: Unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsychiatry 2017;87:3–14. [DOI] [PubMed] [Google Scholar]
- 36.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav 2012;106:29–39. [DOI] [PubMed] [Google Scholar]
- 37.Bethell CD, et al. Prioritizing Possibilities for Child and Family Health: An Agenda to Address Adverse Childhood Experiences and Foster the Social and Emotional Roots of Well-being in Pediatrics. Acad Pediatr 2017;17:S36–S50. [DOI] [PubMed] [Google Scholar]


