Abstract
In this study, multiple-site, cross-sectional area (CSA) reference values were established for major peripheral nerves, including small branches, in the upper extremity of a healthy Asian population.
This study included 107 prospectively recruited age-matched, healthy subjects with a mean age of 46 years (range, 24–75 years). All subjects underwent standardized nerve conduction studies for the median, ulnar, peroneal, posterior tibial, and sural nerves. CSA was measured unilaterally at 21 sites of the median, ulnar, radial, posterior interosseous, superficial radial sensory, musculocutaneous, lateral antebrachial cutaneous, and medial antebrachial cutaneous nerves.
According to their age, the subjects were assigned to the younger group (20–40 years, n = 40), the middle group (40–59 years, n = 40), and the older group (60–80 years, n = 27). The significant differences of CSA values between age groups were found only at certain sites, such as the median (wrist, P = .003), ulnar (medial epicondyle, P = .031; forearm, P = .022), radial (antecubital fossa, P = .037), and superficial radial sensory nerve (P = .028). The CSA significantly correlated with gender, height, weight, and body mass index.
This study provides CSA reference values for nerves, including small sensory nerves in the upper extremity, which can be useful in the ultrasonographic investigation of various peripheral neuropathies in the upper extremity.
Keywords: cross-sectional area, high-resolution ultrasonography, peripheral nerves, reference values, the upper extremity
1. Introduction
Due to improvement in ultrasound technology, high-resolution ultrasonography (HRUS) has become a promising imaging modality for evaluating the peripheral nervous system.[1] The cross-sectional area (CSA) is the most useful and reliable ultrasonographic parameter as a reference for the size of a nerve.[2] As the utility of HRUS is further expanding to various peripheral neuropathies, such as hereditary or acquired polyneuropathies in addition to entrapment neuropathies, traumatic peripheral nerve injuries, and tumors of the peripheral nerves, the importance of normal CSA value of peripheral nerves is increasing.[3–7] The published CSA values tended to vary, probably due to demographic and technical factors.[2,8–25] Furthermore, investigations of CSA reference values in Asians remain insufficient.[9–16] Several studies including screening with nerve conduction studies (NCS) performed nerve conduction studies only a single nerve or F-wave studies of median and posterior tibial nerves.[9,10,14–16] Some studies involved only common entrapment sites of peripheral nerves or only a single peripheral nerve.[9–11]
Therefore, in our study, multiple nerves of the upper extremity including small sensory nerves were examined with 6 to 18 MHz transducer in a healthy Asian population which were recruited using screening tests including NCS of upper and lower extremities. In addition, the demographic features that could affect CSA reference values were analyzed.
2. Methods
2.1. Participants
Based on history taking and physical examinations and NCS, subjects with a history of any neurological disorders, or symptoms or signs associated with peripheral nerve disease were excluded from the study. NCS were unilaterally performed on the median, ulnar, tibial, peroneal, and sural nerves were performed by an experienced technician to the results of the clinical evaluation. Between December 2018 and August 2019, 107 healthy subjects, including physicians, clinical assistants, nurses, and persons who accompanied patients during their clinic visit, were evaluated using HRUS. In all subjects, the following information was collected: age, gender, dominant hand, height, weight, and body mass index (BMI). The study protocol was approved by our Institutional Review Board and all the participants signed informed consent prior to their enrollment in this study.
2.2. Ultrasound measurements
Ultrasound scanning of the upper extremity nerves was performed unilaterally (dominant-hand side) using a linear array transducer with 6 to 18 MHz (ACUSON S2000, Siemens Medical Solutions, Mountain View, CA). All studies were performed by a single neurologist with 4 years of experience in diagnostic neuromuscular ultrasound. The initial settings, except for depth, were kept constant during all measurements. CSA measurements were performed at the inner border of the hyperechoic epineural rim using the continuous tracing technique. The color Doppler mode was used to differentiate nerves from blood vessels. The predetermined sites for each nerve measurement were selected based on anatomic landmarks or clinically important points.
Median nerve: Ultrasonography was performed in a supine position with the examined arm supinated and abducted 45° from the body. Six sites along the median nerve were evaluated:
-
(1)
wrist crease (Fig. 1A),
-
(2)
forearm (between flexor digitorum superficialis and flexor digitorum profundus in the forearm) (Fig. 1B),
-
(3)
below-elbow (before the nerve passes between the 2 heads of pronator teres muscle) (Fig. 1C),
-
(4)
antecubital fossa (next to the brachial artery at the antecubital fossa) (Fig. 1D),
-
(5)
mid-arm (mid-point between the elbow crease and the axilla) (Fig. 1E), and
-
(6)
axilla (Fig. 1F).
Figure 1.
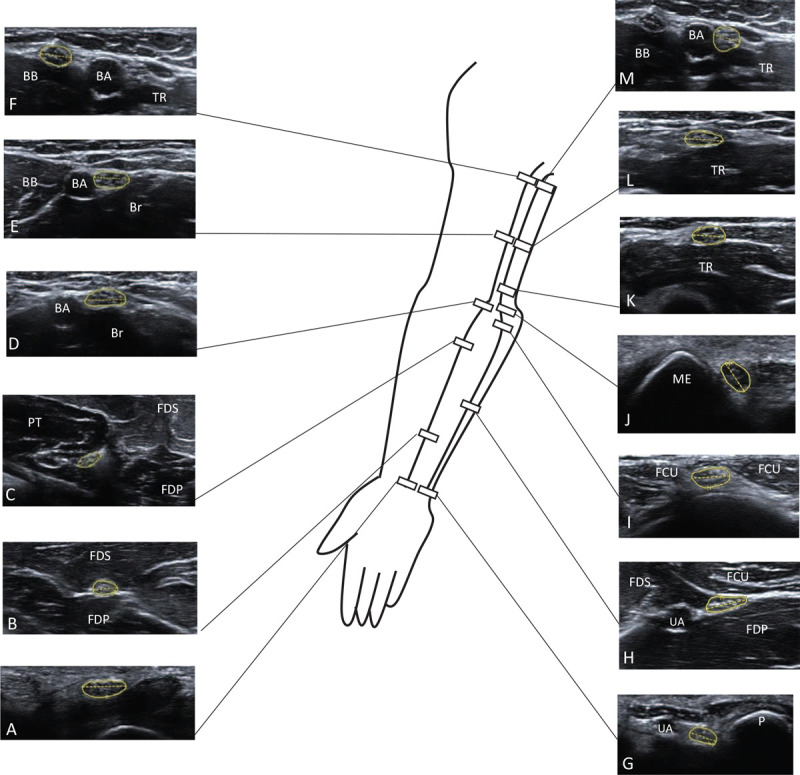
Ultrasonography at the predetermined sites for cross-sectional area in the median and ulnar nerve. Median nerve at the wrist (A), forearm (B), below-elbow (C), antecubital fossa (D), mid-arm (E), and axilla (F). Ulnar nerve at the wrist (G), arterial split (H), outlet of the cubital tunnel (I), tip of the medial epicondyle (J), 2 cm proximal to the tip of the medial epicondyle (K), mid-arm (L), and axilla (M). BA = brachial artery, BB = biceps brachii, Br = brachialis, FCU = flexor carpi ulnaris, FDS = flexor digitorum superficialis, FDP = flexor digitorum profunuds, ME = medial epicondyle, P = pisiform bone, PT = pronator teres, TR = triceps, UA = ulnar artery.
Ulnar nerve: Ultrasonography was performed in the supine position and the forearm supinated, the elbow flexed to 90°, and shoulder abducted 45° from the body. The arm was slightly rotated externally to facilitate imaging. The 7 sites evaluated were the following:
-
(1)
wrist crease (Fig. 1G),
-
(2)
arterial split (where the nerve separates from the ulnar artery, usually in the mid-forearm) (Fig. 1H),
-
(3)
the outlet of the cubital tunnel (between the 2 heads of flexor carpi ulnaris muscle) (Fig. 1I),
-
(4)
the tip of medial epicondyle (ME) (Fig. 1J),
-
(5)
2 cm proximal to the tip of ME (Fig. 1K),
-
(6)
mid-arm (mid-point between the elbow crease and the axilla) (Fig. 1L), and
-
(7)
axilla (Fig. 1M).
Radial nerve: The radial nerve was identified at the antecubital fossa with the subject in a supine position, the forearm pronated, and elbow moderately flexed. The following 5 sites were predetermined:
-
(1)
above spiral groove (SG) (just after exiting SG winding around humerus) (Fig. 2A),
-
(2)
SG (between the triceps brachii and humerus) (Fig. 2B),
-
(3)
antecubital fossa (Fig. 2C) (between extensor carpi radialis and brachioradialis, before branching posterior interosseous nerve (PIN) and superficial radial sensory (SRS) nerve),
-
(4)
PIN at the proximal forearm (just after entering between the 2 heads of the supinator) (Fig. 2D), and
-
(5)
SRS nerve at the proximal forearm (same level as the PIN measurement) (Fig. 2E).
Figure 2.
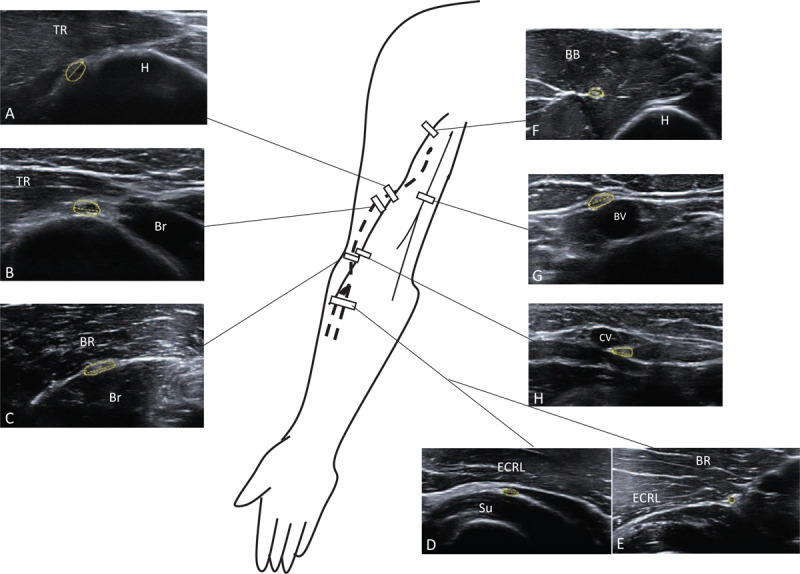
Ultrasonography at the predetermined sites for cross-sectional area in the radial, musculocutaneous, lateral and medial antebrachial cutaneous nerve. Radial nerve at the level above the spiral groove (A), spiral groove (B), and antecubital fossa (C). Posterior interosseous nerve (D) and superficial radial sensory nerve (E) in the proximal forearm. Musculocutaneous nerve in the axilla (F). Medial antebrachial cutaneous nerve in the arm (G). Lateral antebrachial cutaneous nerve in the elbow (H). BB = biceps brachii, BR = brachioradialis, Br = brachialis, BV = basilica vein, CV = cephalic vein, ECRL = extensor carpi radialis longus, H = humerus, Su = supinator, TR = triceps.
Musculocutaneous nerve: Ultrasonography was performed with the subject in a supine position and the shoulder abducted 90°. The measurement was taken distal to the axilla and between the long and short heads of the biceps brachii and coracobrachialis (Fig. 2F).
Medial antebrachial cutaneous nerve (MACN) and lateral antebrachial cutaneous nerve (LACN): Ultrasonography was performed with the subject in a supine position with elbow extended, forearm supinated, and arm abducted 45°. The transducer was placed at the elbow crease with care not to apply pressure to prevent collapse of the veins. MACN was identified running parallel to the brachial and basilic veins at the medial side of mid-arm (Fig. 2G). In subjects with the splitting of MACN identified after tracing MACN up to 10 cm above the elbow crease, each CSA was summated. LACN measurement was taken around the antecubital fossa, where LACN lies just adjacent to the cephalic vein (Fig. 2H).
2.3. Statistical analysis
Statistical analysis was conducted using SAS Version 9.4 (SAS Institute, Cary, NC). The Shapiro–Wilk test was used to examine the normality of the measured variables. The reference range was then determined as the mean ± standard deviation for normally distributed data and from the 2.5th to 97.5th percentile for non-normally distributed data. One-way analysis of variance or Kruskal–Wallis tests were used for data analysis based on age group, and 2 sample t tests or the Wilcoxon rank sum test were used to compare data between the 2 groups based on gender. The Spearman correlation analysis was used to investigate the correlation between the CSA obtained from height, weight, and BMI of the subjects. A P-value < .05 was considered statistically significant.
3. Results
We recruited a total of 107 healthy subjects. The mean age was 46.2 years (range 24–75 years), 56 (52%) were females, 2 were left-handed, the mean height was 165 cm, mean weight was 64.4 kg, and mean BMI was 23.3. A bifid median nerve at the wrist was observed in 9 subjects (8.4%), and the persistent median artery was located within the median nerve at the wrist in 4 subjects (3.7%). We included CSA values of median nerve at the wrist in 98 subjects, except for those with bifid median nerve and persistent median artery. During elbow flexion over 90°, ulnar nerves showed dislocation in 29 of 107 subjects (27.1%). The CSA values were not normally distributed at all sites. The mean CSA and reference range for each measured site and mean of wrist-to-forearm median nerve CSA ratio (WFR) are listed in Table 1. Height, weight, and BMI correlated significantly with nerve CSA (Table 2). In particular, BMI was positively correlated in 19 of 21 nerve sites. Males had significantly larger values than females in 19 of 21 nerve sites (Table 3). The mean CSA values at 21 sites of upper extremity nerves in 3 age groups (20–40 years, 40–59 years, 60–80 years). Among the age groups, the median nerve in the wrist, the ulnar nerve in the ME and forearm, the radial nerve in the antecubital fossa, and SRS nerve showed statistically significant differences. These sites, except the SRS nerve, showed an increase with advancing age. The WFR did not correlate significantly with height, weight, or BMI, but a significant difference was observed between genders (Table 2).
Table 1.
HRUS CSA of upper extremity nerves in healthy Asian adults.
| Percentiles | |||||
| Nerve | Site | Mean | SD | 2.5th, 97.5th | Reference range∗ |
| Median | Wrist | 9.33 | 1.55 | 7, 13 | 7–13 |
| Forearm | 6.31 | 1.49 | 4, 10 | 4–10 | |
| Below-elbow | 6.85 | 1.64 | 4, 11 | 4–11 | |
| Antecubital fossa | 8.96 | 2.41 | 4, 14 | 5–14 | |
| Mid-arm | 9.34 | 2.38 | 6, 15 | 6–15 | |
| Axilla | 9.88 | 2.52 | 6, 16 | 6–16 | |
| WFR | 1.57 | 2.38 | 2. 4 | 1–2.4 | |
| Ulnar | Wrist | 5.09 | 1.29 | 3, 8 | 3–8 |
| Arterial split | 5.74 | 1.42 | 4, 9 | 4–9 | |
| CT outlet | 6.93 | 1.79 | 4, 11 | 4–11 | |
| ME | 7.31 | 1.69 | 5, 11 | 5–11 | |
| Proximal 2 cm to ME | 7.11 | 1.64 | 4, 10 | 4–10 | |
| Mid-arm | 6.37 | 1.56 | 4, 11 | 4–11 | |
| Axilla | 6.94 | 1.97 | 4, 12 | 4–12 | |
| Radial | Above SG | 7.02 | 1.87 | 4, 11 | 4–11 |
| SG | 6.81 | 1.75 | 4, 11 | 4–11 | |
| Antecubital fossa | 7.26 | 1.70 | 5, 11 | 5–11 | |
| SRS | Proximal forearm | 2.50 | 0.86 | 1, 4 | 1–4 |
| PIN | Proximal forearm | 2.02 | 0.69 | 1, 3 | 1–3 |
| MACN | Mid-arm | 3.30 | 1.13 | 2, 7 | 2–7 |
| LACN | Elbow | 3.28 | 1.29 | 2, 6 | 2–6 |
| MC | Axilla | 3.81 | 1.28 | 2, 7 | 2–7 |
All values are in mm2 except WFR. The reference range is determined as the mean ± 2 SD for normally distributed data and from 97.5th percentile for non-normally distributed data. CSA = cross-sectional area, CT = cubital tunnel, HRUS = high-resolution ultrasonography, LACN = lateral antebrachial cutaneous nerve, MACN = medial antebrachial cutaneous nerve, MC = musculocutaneous nerve, ME = medial epicondyle, PIN = posterior interosseous nerve, SD = standard deviation, SG = spiral groove, SRS = superficial radial sensory, WFR = wrist-to-forearm median nerve CSA ratio.
The reference range∗ is determined ∼
Table 2.
Correlation between CSA and height, weight, and BMI.
| Correlation coefficient (P-value) | ||||
| Nerve | Site | Height | Weight | BMI |
| Median | Wrist | 0.213 (.035) | 0.390 (<.001) | 0.391 (<.001) |
| Forearm | 0.326 (.001) | 0.397 (<.001) | 0.310 (.001) | |
| Below-elbow | 0.250 (.009) | 0.332 (.001) | 0.266 (.006) | |
| Antecubital fossa | 0.359 (<.001) | 0.425 (<.001) | 0.332 (.001) | |
| Mid-arm | 0.301 (.002) | 0.438 (<.001) | 0.402 (<.001) | |
| Axilla | 0.409 (<.001) | 0.481 (<.001) | 0.368 (<.001) | |
| WFR | −0.144 (.159) | −0.133 (.272) | −0.04 (.695) | |
| Ulnar | Wrist | 0.318 (.001) | 0.444 (<.001) | 0.421 (<.001) |
| Arterial split | 0.225 (.020) | 0.404 (<.001) | 0.423 (<.001) | |
| CT outlet | 0.367 (<.001) | 0.479 (<.001) | 0.396 (<.001) | |
| ME | 0.266 (.006) | 0.352 (<.001) | 0.292 (.002) | |
| Proximal 2 cm to ME | 0.237 (.014) | 0.367 (<.001) | 0.343 (<.001) | |
| Mid-arm | 0.358 (<.001) | 0.398 (<.001) | 0.276 (.004) | |
| Axilla | 0.413 (<.001) | 0.460 (<.001) | 0.345 (<.001) | |
| Radial | Above SG | 0.145 (.136) | 0.275 (.004) | 0.286 (.003) |
| Spiral groove | 0.095 (.333) | 0.306 (.001) | 0.382 (<.001) | |
| Antecubital fossa | −0.022 (.821) | 0.156 (.109) | 0.267 (.005) | |
| SRS | Proximal forearm | −0.077 (.433) | −0.069 (.479) | −0.012 (.902) |
| PIN | Proximal forearm | 0.188 (.053) | 0.279 (.004) | 0.231 (.017) |
| MACN | Mid-arm | 0.271 (.005) | 0.304 (.002) | 0.218 (.024) |
| LACN | Elbow | 0.372 (<.001) | 0.378 (<.001) | 0.233 (.016) |
| MC | Axilla | 0.202 (.037) | 0.190 (.051) | 0.098 (.316 |
The correlation coefficient between the nerve CSA and height, weight, and BMI were calculated using Spearman's correlation. BMI = body mass index, CSA = cross-sectional area, CT = cubital tunnel, LACN = lateral antebrachial cutaneous nerve, MACN = medial antebrachial cutaneous nerve, MC = musculocutaneous nerve, ME = medial epicondyle, PIN = posterior interosseous nerve, SG = spiral groove, SRS = superficial radial sensory, WFR = wrist-to-forearm median nerve CSA ratio.
Table 3.
Overview of CSA with based on age and gender.
| Age | Gender | |||||||
| Nerve | Site | <40 y (n = 40) | 40–59 y (n = 40) | ≥60 y (n = 27) | P∗ | Male (n = 51) | Female (n = 56) | P† |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Median | Wrist‡ | 8.70 (1.41) | 9.64 (1.33) | 9.8 (1.76) | .003 | 9.73 (1.42) | 8.98 (1.57) | .008 |
| Forearm | 6.25 (1.51) | 6.13 (1.30) | 6.69 (1.69 | .397 | 7 (1.47) | 5.70 (1.22) | <.001 | |
| Below-elbow | 6.55 (1.62) | 7 (1.78) | 7.07 (1.41) | .219 | 7.49 (1.65) | 6.27 (1.39) | <.001 | |
| Antecubital fossa | 8.58 (2.54) | 9.18 (2.55) | 9.22 (1.99) | .303 | 10.20 (2.45) | 7.84 (1.76) | <.001 | |
| Mid-arm | 9.03 (2.11) | 9.53 (2.86) | 9.52 (1.99) | .597 | 10.39 (2.6) | 8.38 (1.68) | <.001 | |
| Axilla | 9.53 (2.65) | 10.03 (2.72) | 10.19 (1.96) | .284 | 11.2 (2.5)) | 8.68 (1.86) | <.001 | |
| WFR | 1.49 (0.4) | 1.66 (0.35) | 1.58 (0.4) | .083 | 1.47 (0.33) | 1.66 (0.41) | .033 | |
| Ulnar | Wrist | 4.85 (1.14) | 5.38 (1.43) | 5.04 (1.26) | .178 | 5.73 (1.22) | 4.52 (1.08) | <.001 |
| Arterial split | 5.28 (1.36) | 6 (1.38) | 6.04 (1.43) | .022 | 6.35 (1.41) | 5.18 (1.18) | <.001 | |
| CT outlet | 6.55 (1.85) | 7.10 (1.57) | 7.26 (1.95) | .143 | 7.88 (1.84) | 6.07 (1.22) | <.001 | |
| ME | 6.78 (1.46) | 7.58 (1.71) | 7.73 (1.85) | .031 | 8 (1.77) | 6.7 (1.36) | <.001 | |
| Proximal 2 cm to ME | 6.75 (1.45) | 7.28 (1.83) | 7.41 (1.58) | .252 | 7.53 (1.64) | 6.73 (1.55) | .008 | |
| Mid-arm | 6.25 (1.46) | 6.53 (1.72) | 6.33 (1.49) | .813 | 7.08 (1.7) | 5.73 (1.09) | <.001 | |
| Axilla | 6.68 (2.25) | 7.1 (1.88) | 7.11 (1.67) | .213 | 7.9 (2.08) | 6.07 (1.39) | <.001 | |
| Radial | Above SG | 6.63 (1.79) | 6.95 (1.71) | 7.7 (2.07) | .122 | 7.49 (1.75) | 6.59 (1.89) | .005 |
| Spiral groove | 6.33 (1.59) | 6.88 (1.54) | 7.41 (2.08) | .063 | 7.16 (1.69) | 6.5 (1.75) | .03 | |
| Antecubital fossa | 6.8 (1.36) | 7.33 (1.87) | 7.85 (1.75) | .037 | 7.41 (1.9) | 7.13 (1.5) | .521 | |
| SRS | Proximal forearm | 2.2 (0.79) | 2.73 (0.96) | 2.59 (0.69) | .028 | 2.43 (0.94) | 2.55 (0.78) | .377 |
| PIN | Proximal forearm | 1.83 (0.64) | 2.13 (0.69) | 2.15 (0.72) | .088 | 2.24 (0.62) | 1.82 (0.69) | .001 |
| MACN | Mid-arm | 3.2 (1.22) | 3.53 (1.22) | 3.11 (0.8) | .342 | 3.76 (1.19) | 2.88 (0.9) | <.001 |
| LACN | Elbow | 3.18 (1.28) | 3.48 (1.47) | 3.15 (0.99) | .54 | 3.92 (1.38) | 2.7 (0.85) | <.001 |
| MC | Axilla | 3.78 (1.25) | 3.9 (1.43) | 3.74 (1.13) | .96 | 4.18 (1.35) | 3.48 (1.13) | .004 |
All values are in mm2 except for WFR. CSA = cross-sectional area, CT = cubital tunnel, LACN = lateral antebrachial cutaneous nerve, MACN = medial antebrachial cutaneous nerve, MC = musculocutaneous nerve, ME = medial epicondyle, n = number of subjects, PIN = posterior interosseous nerve, SD = standard deviation, SG = spiral groove, SRS = superficial radial sensory, WFR = wrist-to-forearm median nerve CSA ratio, y = years.
P-values calculated using the Kruskal–Wallis test or ANOVA test.
P-values calculated using Wilcoxon rank sum test or t test.
The CSA values at the wrist obtained from 98 subjects were analyzed (male = 47, female = 51, <40 = 37, 40–59 = 36, ≥60 = 25).
4. Discussion
The CSA values in our study are comparable to the values published in several studies for Asians but the value differed depending upon the nerve or site of the CSA measurement in those studies.[11–14] The CSA values of the median nerve in our study were similar to the values obtained by Won et al[14] (carpal tunnel inlet, 8.33 ± 1.52 mm2; mid-forearm, 6.53 ± 1.05 mm2; antecubital fossa, 8.12 ± 1.58 mm2; mid-humerus, 9.44 ± 1.40 mm2), Sugimoto et al[12] (wrist, 8.5 ± 1.7 mm2; distal forearm, 6.0 ± 1.3 mm2; antecubital fossa, 9.1 ± 2.2 mm2), Seok et al[11] (wrist, 9.58 ± 1.55 mm2; forearm, 6.87 ± 1.61 mm2), and Niu et al[13] (forearm, 5.9 ± 0.9 mm2; antecubital fossa, 8.4 ± 1.3 mm2), but greater than the values reported by Sugimoto et al[12] (mid-humerus, 8.2 ± 1.7 mm2) and Niu et al[13] (wrist, 6.4 ± 0.9 mm2; mid-arm, 7.9 ± 1.2 mm2; axilla, 7.7 ± 1.2 mm2). The CSA values of the ulnar nerve in our study were similar to the values reported by Won et al[14] (wrist, 4.28 ± 0.78 mm2; forearm, 6.30 ± 1.01 mm2; cubital tunnel inlet, 7.21 ± 1.35 mm2; mid-humerus, 5.85 ± 1.05 mm2), Seok et al[11] (wrist, 4.72 ± 0.91 mm2; ME, 6.64 ± 1.33 mm2), and Sugimoto et al[12] (Guyon's canal, 4.1 ± 1.0 mm2; distal forearm, 4.7 ± 1.0 mm2; ME, 6.7 ± 1.9 mm2), but greater than the values obtained by Sugimoto et al[12] (mid-arm, 4.8 ± 1.0 mm2) and Niu et al[13] (wrist, 2.9 ± 0.6 mm2; forearm, 4.6 ± 0.8 mm2; ME, 5.6 ± 1.1 mm2; mid-arm, 4.4 ± 0.9 mm2; axilla, 4.5 ± 0.9 mm2). Compared to the studies by Bathala et al,[9,10] our results were larger at most sites of the median and ulnar nerve. The CSA values of the radial nerve in our study were similar to the values reported by Seok et al[11] (SG, 6.48 ± 1.68 mm2) but greater than the values obtained by Won et al[14] (SG, 4.58 ± 0.85 mm2; antecubital fossa, 4.53 ± 0.75 mm2) and Niu et al[13] (SG, 3.4 ± 0.7 mm2; antecubital fossa, 3.1 ± 0.6 mm2). Studies for reference CSA value of the SRS nerve and PIN in Asians are very rare. As for the study of Won et al[14] (SRS nerve, 2.00 ± 0.53 mm2; PIN, 2.03 ± 0.46 mm2), our study showed similar results. CSA studies of small sensory nerves in the upper extremity such as MACN and LACN are not available for Asians and are extremely rare for non-Asians. Chiavaras et al[26] reported that the mean CSA value of the symptomatic LACN was 12.0 mm2 compared with 3.3 mm2 in the contralateral normal elbows, which are similar to our results. Several studies reported that the reference values of peripheral nerve CSA varied among different countries and continents, and the nerve CSA values in Americans and Europeans were greater than in Asians.[13,25] However, depending upon the nerve or site of the CSA measurement, the CSA values in our study were similar to those in studies for non-Asians.[2,17–19,22,24,27] Thus, it may be necessary to consider other technical factors, such as the location of nerve CSA measurement, measurement accuracy, and equipment rather than ethnic difference as possible causes of this variability of reported reference values.
In previous studies,[9–14,17,18,20,24] the nerve CSA values in males were significantly greater than in females, but differences in gender differed based depending upon the nerve. Our results showed difference of the CSA values in the majority of sites except for the radial nerve (antecubital fossa) and SRS nerve. Although WFR was not affected by demographic factors in previous studies,[14,28,29] statistically significant difference was observed by gender in our study. Sugimoto et al[12] showed the wrist-to-distal forearm CSA ratio was associated with gender, age, height, and BMI, unlike the wrist-to-proximal forearm CSA ratio. Therefore, further studies are needed regarding the effects of gender and CSA measurement site on WFR. A positive correlation between CSA and age has been reported in several studies,[2,9,12,13,20] but was not in some studies.[11,14] A statistical difference was observed in CSA based on age at 5 of 21 sites, such as median nerve (wrist), the ulnar nerve (ME and forearm), the radial nerve (antecubital fossa), and the SRS nerve (elbow) in our study. The effect of age on CSA was more common in the entrapment site of nerves, where the enlargement of the nerve may occur with aging and mechanical stress due to repeated entrapping. Won et al[14] and Cartwright et al[2] described that CSA correlated with height, weight, and BMI. Qrimli et al[22] showed height was not correlated with CSA, and Werner et al[30] found no correlation between the CSA and weight or BMI. In our study, CSA values were positively correlated with height, weight, and BMI. Therefore, consideration of demographic factors is important when assessing CSA results.
Our study had several limitations. First, due to time constraint caused by the addition of NCS of upper and lower extremities as screening tests, only unilateral measurements of the nerves were included, which could have affected the variation in the values reported. Second, a single investigator performed the sonographic examination on all subjects using 1 HRUS machine and this study did not assess inter-rater and inter-equipment reliability. The full procedure was not well tolerated by most subjects due to the time-consuming of 21 nerve measurements and NCS. We did not include intra-rater reliability testing and information on this topic could not be provided. Finally, because all participants were Korean, and the study did not include subjects of different ethnicities, the reference values are difficult to apply across a broad population.
In conclusion, our study was a large-scale, prospective investigation of the HRUS CSA of multiple sites of the upper extremity nerves, including small sensory nerves in a healthy Asian population, after excluding subjects with subclinical neuropathy, identified by NCS. The results of our study can serve as a valuable resource to clinicians performing HRUS for the evaluation of peripheral nerve disorders in the Asian population.
Author contributions
Conceptualization: Dae Woong Bae, Jae Young An.
Data curation: Dae Woong Bae, Jae Young An.
Formal analysis: Dae Woong Bae.
Funding acquisition: Jae Young An.
Investigation: Jae Young An.
Methodology: Dae Woong Bae.
Project administration: Jae Young An.
Validation: Dae Woong Bae, Jae Young An.
Writing – original draft: Dae Woong Bae.
Writing – review & editing: Jae Young An.
Footnotes
Abbreviations: BMI = body mass index, CSA = cross-sectional area, HRUS = high-resolution ultrasonography, LACN = lateral antebrachial cutaneous nerve, MACN = medial antebrachial cutaneous nerve, ME = medial epicondyle, NCS = nerve conduction studies, PIN = posterior interosseous nerve, SG = spiral groove, SRS = superficial radial sensory, WFR = wrist-to-forearm median nerve CSA ratio.
How to cite this article: Bae DW, An JY. Cross-sectional area reference values for high-resolution ultrasonography of the upper extremity nerves in healthy Asian adults. Medicine. 2021;100:18(e25812).
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2018R1C1B5085469) and the statistical consultation was supported by a grant of the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI14C1731).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Walker FO, Cartwright MS, Wiesler ER, et al. Ultrasound of nerve and muscle. Clin Neurophysiol 2004;115:495–507. [DOI] [PubMed] [Google Scholar]
- [2].Cartwright MS, Passmore LV, Yoon JS, et al. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve 2008;37:566–71. [DOI] [PubMed] [Google Scholar]
- [3].Beekman R, van den Berg LH, Franssen H, et al. Ultrasonography shows extensive nerve enlargements in multifocal motor neuropathy. Neurology 2005;65:305–7. [DOI] [PubMed] [Google Scholar]
- [4].Imamura K, Tajiri Y, Kowa H, et al. Peripheral nerve hypertrophy in chronic inflammatory demyelinating polyradiculoneuropathy detected by ultrasonography. Intern Med 2009;48:581–2. [DOI] [PubMed] [Google Scholar]
- [5].Noto Y, Shiga K, Tsuji Y, et al. Nerve ultrasound depicts peripheral nerve enlargement in patients with genetically distinct Charcot-Marie-Tooth disease. J Neurol Neurosurg Psychiatry 2015;86:378–84. [DOI] [PubMed] [Google Scholar]
- [6].Scheidl E, Böhm J, Simó M, et al. Ultrasonography of MADSAM neuropathy: focal nerve enlargements at sites of existing and resolved conduction blocks. Neuromuscul Disord 2012;22:627–31. [DOI] [PubMed] [Google Scholar]
- [7].Zaidman CM, Al-Lozi M, Pestronk A. Peripheral nerve size in normals and patients with polyneuropathy: an ultrasound study. Muscle Nerve 2009;40:960–6. [DOI] [PubMed] [Google Scholar]
- [8].Babaei-Ghazani A, Roomizadeh P, Nouri E, et al. Ultrasonographic reference values for the median nerve at the level of pronator teres muscle. Surg Radiol Anat 2018;40:1019–24. [DOI] [PubMed] [Google Scholar]
- [9].Bathala L, Kumar P, Kumar K, et al. Normal values of median nerve cross-sectional area obtained by ultrasound along its course in the arm with electrophysiological correlations, in 100 Asian subjects. Muscle Nerve 2014;49:284–6. [DOI] [PubMed] [Google Scholar]
- [10].Bathala L, Kumar P, Kumar K, et al. Ultrasonographic cross-sectional area normal values of the ulnar nerve along its course in the arm with electrophysiological correlations in 100 Asian subjects. Muscle Nerve 2013;47:673–6. [DOI] [PubMed] [Google Scholar]
- [11].Seok JI, Lee SB, Bae CB. Ultrasonographic findings of the normal nerves in common entrapment site; cross-sectional area reference value and normal variant. J Korean Neurol Assoc 2015;33:08–12. [Google Scholar]
- [12].Sugimoto T, Ochi K, Hosomi N, et al. Ultrasonographic reference sizes of the median and ulnar nerves and the cervical nerve roots in healthy Japanese adults. Ultrasound Med Biol 2013;39:1560–70. [DOI] [PubMed] [Google Scholar]
- [13].Niu J, Li Y, Zhang L, et al. Cross-sectional area reference values for sonography of nerves in the upper extremities. Muscle Nerve 2020;61:338–46. [DOI] [PubMed] [Google Scholar]
- [14].Won SJ, Kim BJ, Park KS, et al. Reference values for nerve ultrasonography in the upper extremity. Muscle Nerve 2013;47:864–71. [DOI] [PubMed] [Google Scholar]
- [15].Won SJ, Kim BJ, Park KS, et al. Measurement of cross-sectional area of cervical roots and brachial plexus trunks. Muscle Nerve 2012;46:711–6. [DOI] [PubMed] [Google Scholar]
- [16].Seok HY, Jang JH, Won SJ, et al. Cross-sectional area reference values of nerves in the lower extremities using ultrasonography. Muscle Nerve 2014;50:564–70. [DOI] [PubMed] [Google Scholar]
- [17].Boehm J, Scheidl E, Bereczki D, et al. High-resolution ultrasonography of peripheral nerves: measurements on 14 nerve segments in 56 healthy subjects and reliability assessments. Ultraschall Med 2014;35:459–67. [DOI] [PubMed] [Google Scholar]
- [18].Cartwright MS, Shin HW, Passmore LV, et al. Ultrasonographic findings of the normal ulnar nerve in adults. Arch Phys Med Rehabil 2007;88:394–6. [DOI] [PubMed] [Google Scholar]
- [19].Cartwright MS, Shin HW, Passmore LV, et al. Ultrasonographic reference values for assessing the normal median nerve in adults. J Neuroimaging 2009;19:47–51. [DOI] [PubMed] [Google Scholar]
- [20].Kerasnoudis A, Pitarokoili K, Behrendt V, et al. Cross sectional area reference values for sonography of peripheral nerves and brachial plexus. Clin Neurophysiol 2013;124:1881–8. [DOI] [PubMed] [Google Scholar]
- [21].Marciniak C, Caldera F, Welty L, et al. High-resolution median nerve sonographic measurements: correlations with median nerve conduction studies in healthy adults. J Ultrasound Med 2013;32:2091–8. [DOI] [PubMed] [Google Scholar]
- [22].Qrimli M, Ebadi H, Breiner A, et al. Reference values for ultrasonography of peripheral nerves. Muscle Nerve 2016;53:538–44. [DOI] [PubMed] [Google Scholar]
- [23].Tagliafico A, Martinoli C. Reliability of side-to-side sonographic cross-sectional area measurements of upper extremity nerves in healthy volunteers. J Ultrasound Med 2013;32:457–62. [DOI] [PubMed] [Google Scholar]
- [24].Yalcin E, Onder B, Akyuz M. Ulnar nerve measurements in healthy individuals to obtain reference values. Rheumatol Int 2013;33:1143–7. [DOI] [PubMed] [Google Scholar]
- [25].Burg EW, Bathala L, Visser LH. Difference in normal values of median nerve cross-sectional area between Dutch and Indian subjects. Muscle Nerve 2014;50:129–32. [DOI] [PubMed] [Google Scholar]
- [26].Chiavaras MM, Jacobson JA, Billone L, et al. Sonography of the lateral antebrachial cutaneous nerve with magnetic resonance imaging and anatomic correlation. J Ultrasound Med 2014;33:1475–83. [DOI] [PubMed] [Google Scholar]
- [27].Raeburn K, Burns D, Hage R, et al. Cross-sectional sonographic assessment of the posterior interosseous nerve. Surg Radiol Anat 2015;37:1155–60. [DOI] [PubMed] [Google Scholar]
- [28].Hobson-Webb LD, Massey JM, Juel VC, et al. The ultrasonographic wrist-to-forearm median nerve area ratio in carpal tunnel syndrome. Clin Neurophysiol 2008;119:1353–7. [DOI] [PubMed] [Google Scholar]
- [29].Hunderfund AN, Boon AJ, Mandrekar JN, et al. Sonography in carpal tunnel syndrome. Muscle Nerve 2011;44:485–91. [DOI] [PubMed] [Google Scholar]
- [30].Werner RA, Jacobson JA, Jamadar DA. Influence of body mass index on median nerve function, carpal canal pressure, and cross-sectional area of the median nerve. Muscle Nerve 2004;30:481–5. [DOI] [PubMed] [Google Scholar]


