Abstract
Out of hospital cardiac arrest (OHCA) remains a leading cause of mortality among adults in the United States. Environmental impact on incidence and outcomes of OHCA has not been fully investigated in recent years. Previous studies showed a possible increase in incidence and mortality in winter season and during seasons with temperature extremes. This study examines seasonal variation in incidence and outcomes of OHCA in the United States.
Retrospective study of adult OHCA using the Nationwide Emergency Department Sample was carried out. Monthly incidence rate per 100,000 ED presentations was calculated. Survival rates for each month of admission were examined by hospital region. Multivariate analyses were conducted to determine the effect of the season and month of admission on survival.
A total of 122,870 adult OHCA cases presented to emergency departments (EDs) in 2014 and were included. Average incidence of OHCA cases was 147 per 100,000 ED presentations. Overall survival rate in the study population was 5.6% (95% confidence intervals [CI] = 5.4%–5.9%). Patients had an average age of 65.5 (95% CI: 65.3–65.7) years and were mainly men (61.8%). Rates of OHCA presentations were highest during December and January (9.9% and 10.0%) while survival rates were lowest during December (4.6%) and highest in June (6.9%). Regional variation in OHCA outcomes was also noted with highest average survival rate in West (7.8%) and lowest in South (4.3%). After adjusting for confounders including region of hospital, Summer season (Ref: all other seasons), and more specifically month of June (Ref: all other months) were found to be positively associated with survival (OR 1.27, 95% CI [1.07–1.52], P-value = .008) and (OR 1.43, 95% CI [1.08–1.89], P-value = .012 respectively).
Incidence and outcomes of out of hospital cardiac arrest presentations to the emergency departments in the United States have seasonal variation. Both incidence and mortality of OHCA increase during colder months, and survival is significantly higher in summer season or in June. Exploring how to use this variation to improve outcomes through refresher training of medical providers or through other mitigation plans is needed.
Keywords: emergency department, incidence, out of hospital cardiac arrest, outcomes, seasonal variation
1. Introduction
Out of hospital cardiac arrest (OHCA) remains a leading cause of mortality among adults in the United States with an estimated incidence rate of OHCA ranging from 200,000 to 300,000 occurrences per year.[1–3] Overall survival rates to hospital discharge remain low with minimal impact on outcomes from in-hospital interventions.[1,2] Interventions to improve outcomes focus mainly on improving community involvement (early recognition, bystander cardiopulmonary resuscitation [CPR], public access defibrillation) and the emergency medical services’ response (dispatcher assister CPR, early high-quality CPR, and defibrillation by EMS providers).[4–6] Additionally, several patient related factors affect OHCA outcomes: these include characteristics such as sex, age, socioeconomic status, presence of chronic diseases, and family history.[1,2,7,8] Event related clinical variables such as witnessed status of cardiac arrest, occurrence and type of bystander CPR, EMS agency type, and use of automated defibrillators on scene are also associated with improved outcomes in OHCA.[4–6,9] Other interventions have also been associated with OHCA outcomes including airway management (intubation), time and type of medication administration, use of a cardiac assisted device such as a left ventricular assist device (LVAD), as well as initiation of hypothermia protocol.[5,6,10–13]
To date, few studies have examined environmental factors affecting outcomes in OHCA. Bagai et al[14] found temporal differences in hour of day, day of the week, and month of the year for both incidence and survival of OHCA in the United States between 2005 and 2010. The highest incidence occurred during daytime, from Friday to Monday, in December.[14] A direct association was also previously identified between cold weather in regions with mild winters in Europe and increased mortality.[15] A 1 °C decreases in temperature is associated with an increase of 1.72% in daily mortality with a greater effect observed in warmer cities.[16]
Other studies out of Asian countries have also previously examined the association between temperature change and OHCA. A significantly increased risk of OHCA was described with both cold and hot ambient temperatures in China.[17] A similar association between climate temperatures and outcomes of OHCA was also described in a nationwide cohort study in Japan.[18] The association between OHCA and temperature was stronger for mean temperature than either for day to day temperature change or diurnal temperature range.[19] To date, seasonal variation in incidence and outcomes of OHCA has not been evaluated across different regions in the United States. Understanding variation patterns in both OHCA occurrences and outcomes can help communities across the United States mitigate the impact of this disease and improve the healthcare system's readiness to respond better to OHCA.
This study examined seasonal variation of OHCA presentations to US emergency departments (EDs) and associated outcome (survival to hospital discharge) using the largest US national ED database.
2. Materials and methods
2.1. Study design and population
This retrospective population-based observational study used the 2014 public release dataset of the Nationwide Emergency Department Sample (NEDS) database. Adult patients (18 years or older) who presented to US emergency departments in 2014 with both a diagnosis of cardiac arrest and well-defined outcomes were included. NEDS is the largest US all-payer Emergency Department database by Healthcare Cost and Utilization Project (HCUP).[19] The 2014 NEDS data were released in December of 2016 and consisted of aggregated data from 945 hospital-owned EDs located across 33 States (AR, AZ, CA, CT, FL, GA, HI, IA, IN, KS, KY, IL, MA, MD, ME, MN, MO, MT, NC, ND, NE, NJ, NV, NY, OH, RI, SC, SD, TN, UT, VT, WI, and WY) and the District of Columbia, reflecting approximately 20% of all hospital-based EDs located in the United States.[20]
According to the US Census Bureau data, the population strata of NEDS accounts for 68.7% of the US population in 2014. The 2014 NEDS dataset contains information on weighted 137,807,901 ED visits. Out of the total weighted ED visits, 170,251 were visits to the ED for OHCA. Out of those 122,870 were adult visits and constituted the study sample after exclusion of 47,381 patients who had no clear outcomes and no recorded month of presentation (Fig. 1). No sample size was calculated because all eligible patients who met the inclusion criteria were extracted from the NEDS database and included in the study sample.
Figure 1.
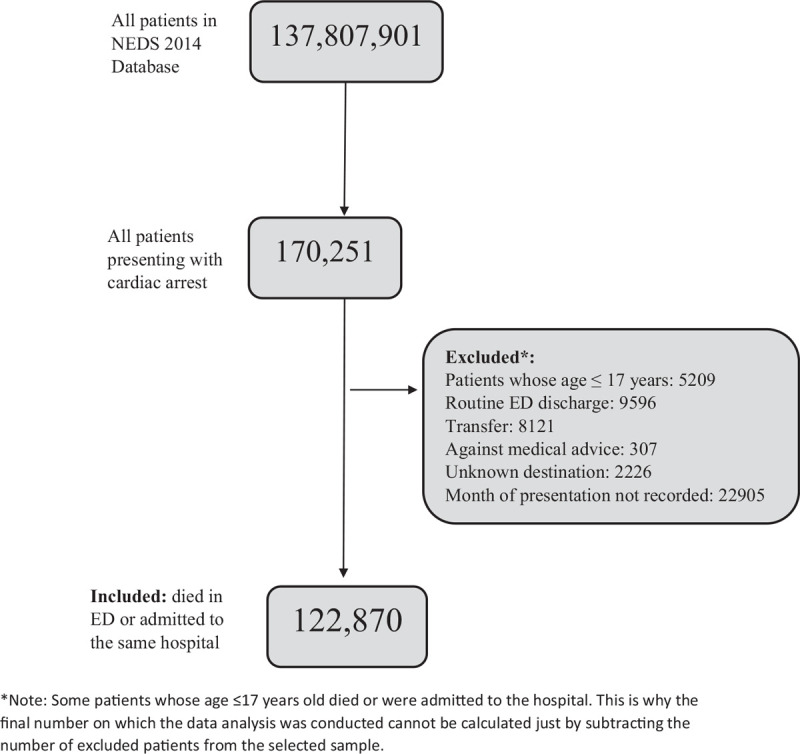
Inclusion and exclusion flowchart.
The institutional review board at the American University of Beirut approved the use of NEDS de-identified dataset for this study.
2.2. Data definitions
Data were weighted according to the following stratification variables as per HCUP specifications: US Census region, urban-rural location, ownership, and teaching status of the hospital and trauma center designation.[21] Additionally, publishing HCUP data requires that any data with size ≤10 must be excluded to safeguard patients’ privacy.
The NEDS database includes administrative and clinical data such as demographic patient information; admission and discharge status; procedure and diagnostic codes; payment source; healthcare expenses, and general hospital characteristics. International Classification of Diseases (ICD) coding system was used to select all patients with presenting with cardiac arrest. ICD coding system is a tool for designating patient diagnoses and procedures for billing and reimbursement uses. The following ICD-9 codes where used for cardiac arrest: 427.41, 427.42, 427.5. Only patients with a “primary diagnosis” of cardiac arrest under CCS 107 listed as “first listed diagnosis” (i.e., “the diagnosis, condition, problem or other reason for encounter/visit shown in the medical record to be chiefly responsible for the services provided”) were included in this study. The occurrence of any selection bias was minimized by including all patients who had CCS 107. Chronic diseases and procedures with frequencies <10% were removed from the analysis and were not displayed in the results. (Supplemental Digital Content Appendix 1)
Monthly incidence rate per 100,000 ED presentations was calculated by dividing the number of OHCA patients who presented during each month irrespective of their ED dispositions by all ED presentations of the same month in the United States in 2014.
In order to account for confounders related to clinical severity, a score of procedures used in the ED or in the hospital was calculated and included in the multivariate analysis. The northern meteorological seasons definition was used in this article, defined as the following: spring occurs from the months of March to May, summer occurs from June till August, fall (autumn) occurs from September till November, and lastly, winter occurs between the months of December to February.
2.3. Statistical analysis
Statistical analysis for this study, done using IBM-SPSS 24, included descriptive analysis on the socio-demographic, clinical, and hospital characteristics including month of admission. Continuous variables were described as a mean with associated 95% confidence intervals (CI) and categorical variables were described as frequencies, percentages, and respective 95% CI. Survival rates for each month of admission were examined by hospital region. Multiple imputation was not used in this study since none of the assessed variables had >5% missing data. Analysis was verified using HCUPnet, a free on-line query system based on data from HCUP.[22] Logistic regression models were conducted to adjust for confounders and to determine the effect of months/seasons of admission on the survival of the OHCA patients. Only significant variables at the bivariate level were included in the multivariate analysis. The same multivariate analyses were performed when stratifying by hospital region. The CSDESCRIPTIVES, CSTABULATE, and CSLOGISTIC procedures were used to adjust for the NEDS survey design in developing estimates. Finally, a P-value of ≤.05 was used to indicate statistical significance.
3. Results
The study population included a total of 122,870 adult visits to ED hospitals in the United States in 2014. Patients had a mean age of 65.5 years (95% CI = 65.3–65.7) and were more commonly men 61.8% (95% CI = 61.3–62.3). The highest rates of presentations occurred in December (9.9%; 95% CI = 9.6–10.3) and January (10.0%; 95% CI = 9.7–10.3).
Overall average monthly incidence of OHCA cases was approximately 147 per 100,000 ED presentations. Figure 2 shows monthly rates of OHCA presentations with lowest incidence in September (126 per 100,000) and highest in January (175 per 100,000).
Figure 2.
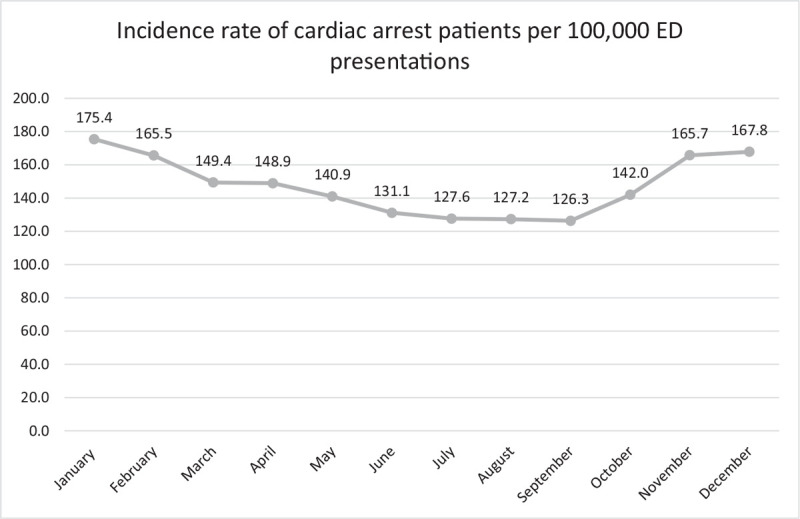
Incidence of OHCA at EDs in United States. EDs = emergency departments, OHCA = out of hospital cardiac arrest.
Outcomes of patients who presented with OHCA are also presented in Table 1. Overall survival for this study population is 5.6% (n = 6891; 95% CI = 5.4–5.9) ranging from 4.6% in December to 6.9% in June (Fig. 3). The highest reported overall survival was in western regions (7.8%; 95% CI = 7.2–8.5) while the lowest survival was in southern regions (4.3%; 95% CI = 3.9–4.7).
Table 1.
Characteristics of study population.
| Continuous variables | Frequency (N = 122,870) | Mean (95% CI) |
| Age, y | 122,870 | 65.5 (65.3–65.7) |
| Categorical variables | Frequency (N = 122,870) | Percentage (95% CI) |
| Gender (male) | ||
| Missing: 153 (0.1%) | 75,790 | 61.8 (61.2–62.3) |
| Month of admission | ||
| January | 12,272 | 10.0 (9.7–10.3) |
| February | 10,054 | 8.2 (7.9–8.5) |
| March | 10,241 | 8.3 (8.0–8.6) |
| April | 10,179 | 8.3 (8.0–8.6) |
| May | 9977 | 8.1 (7.8–8.4) |
| June | 9242 | 7.5 (7.2–7.8) |
| July | 9394 | 7.6 (7.4–7.9) |
| August | 9305 | 7.6 (7.3–7.9) |
| September | 9010 | 7.3 (7.1–7.6) |
| October | 10,100 | 8.2 (7.9–8.5) |
| November | 10,873 | 8.8 (8.5–9.2) |
| December | 12,223 | 9.9 (9.6–10.3) |
| Patient location: urban-rural code | ||
| Large central metropolitan | 28,322 | 23.2 (22.9–23.5) |
| Large fringe metropolitan | 27,743 | 22.7 (22.4–23.1) |
| Medium metropolitan | 28,379 | 23.3 (22.9–23.6) |
| Small metropolitan | 13,060 | 10.7 (10.4–11.0) |
| Micropolitan | 14,303 | 11.7 (11.5–11.9) |
| Not metropolitan or micropolitan | 10,163 | 8.3 (8.1–8.5) |
| Missing: 900 (0.7%) | ||
| Region of hospital | ||
| Northeast | 24,994 | 20.3 (20.3–20.3) |
| Midwest | 32,968 | 26.8 (26.8–26.8) |
| South | 42,028 | 34.2 (34.2–34.2) |
| West | 22,880 | 18.6 (18.6–18.6) |
| Patient underwent a procedure∗ | ||
| No procedure done | 86,473 | 70.4 (69.9–70.8) |
| 1 | 18,612 | 15.1 (14.8–15.5) |
| ≥2 | 17,785 | 14.5 (14.1–14.9) |
| Overall survival | 6891 | 5.6 (5.4–5.9) |
| Northeast | 1184 | 4.7 (4.3–5.3) |
| Midwest | 2122 | 6.4 (5.9–7.0) |
| South | 1800 | 4.3 (3.9–4.7) |
| West | 1785 | 7.8 (7.2–8.5) |
Procedures include the following: respiratory intubation and mechanical ventilation—diagnostic cardiac catheterization; coronary arteriography—other vascular catheterization; not heart—insertion; revision; replacement; removal of cardiac pacemaker or cardioverter/defibrillator—conversion of cardiac rhythm—percutaneous transluminal coronary angioplasty (PTCA)—blood transfusion—coronary artery bypass graft (CABG)—extracorporeal circulation auxiliary to open heart procedures—other therapeutic procedures—peritoneal dialysis.
Figure 3.

Overall survival rate of OHCA patients presenting to EDs in United States. EDs = emergency departments, OHCA = out of hospital cardiac arrest.
Table 2 shows total survival rates per month of presentation stratified by region. Survival rates were lowest in the South (3.4%–5.4%) and highest in the West (5.7%–9.6%). Table 3 shows crude and adjusted survival odds ratios for presentations with OHCA for season and month of admission. After adjusting for confounders including geographic region, summer season, and June were significantly associated with increased odds of survival (OR = 1.27, 95% CI 1.07–1.52, P = .008 and OR = 1.43, 95% CI 1.08–1.89, P = .012 respectively). When stratified by hospital region (Table 4), summer remained a significant positive predictor of survival in western region only (OR = 1.76, 95% CI: 1.25–2.48). More specifically, June remained significantly associated with increased odds of survival in Northeast and West regions but not in South or Midwest (Table 4).
Table 2.
Regional survival rate of OHCA patients presenting to EDs in United States.
| Northeast | Midwest | South | West | Total | ||||||
| N | Percent survived (95% CI) | N | Percent survived (95% CI) | N | Percent survived (95% CI) | N | Percent survived (95% CI) | N | Percent survived (95% CI) | |
| Month of admission | ||||||||||
| January | 95 | 3.9 (2.7–5.6) | 233 | 6.8 (5.2–8.7) | 148 | 3.5 (2.5–4.8) | 157 | 7.4 (5.5–9.8) | 633 | 5.2 (4.4–6.0) |
| February | 111 | 5.2 (3.6–7.3) | 173 | 6.4 (4.8–8.6) | 118 | 3.5 (2.5–4.9) | 122 | 6.6 (4.8–9.1) | 524 | 5.2 (4.4–6.1) |
| March | 91 | 4.6 (3.1–6.8) | 163 | 5.6 (4.1–7.5) | 159 | 4.7 (3.6–6.3) | 153 | 7.7 (5.8–10.2) | 566 | 5.5 (4.7–6.5) |
| April | 120 | 6.0 (4.3–8.4) | 197 | 7.6 (5.7–10.0) | 131 | 3.5 (2.6–4.7) | 160 | 8.7 (6.6–11.4) | 607 | 6.0 (5.1–6.9) |
| May | 117 | 5.7 (4.0–8.0) | 185 | 6.7 (5.1–8.8) | 132 | 4.0 (2.9–5.5) | 120 | 6.4 (4.6–8.8) | 554 | 5.6 (4.8–6.5) |
| June | 133 | 6.8 (5.0–9.2) | 168 | 7.2 (5.3–9.7) | 169 | 5.4 (4.0–7.2) | 166 | 9.2 (7.0–12.0) | 636 | 6.9 (5.9–8.0) |
| July | 91 | 4.9 (3.4–7.1) | 164 | 6.7 (4.9–9.1) | 165 | 5.0 (3.8–6.7) | 174 | 9.6 (7.4–12.3) | 594 | 6.3 (5.4–7.3) |
| August | 94 | 5.0 (3.4–7.2) | 159 | 6.7 (4.9–9.0) | 150 | 4.5 (3.3–6.1) | 151 | 8.9 (6.7–11.5) | 554 | 6.0 (5.1–6.9) |
| September | 65 | 3.5 (2.2–5.6) | 141 | 5.9 (4.2–8.1) | 154 | 5.2 (3.8–6.9) | 156 | 8.8 (6.6–11.6) | 516 | 5.7 (4.9–6.7) |
| October | 96 | 4.9 (3.3–7.0) | 159 | 5.7 (4.2–7.7) | 158 | 4.6 (3.5–6.2) | 111 | 5.7 (4.2–7.9) | 524 | 5.2 (4.4–6.1) |
| November | 92 | 4.0 (2.7–5.9) | 194 | 6.5 (4.9–8.6) | 172 | 4.7 (3.5–6.2) | 157 | 8.1 (6.2–10.5) | 615 | 5.7 (4.9–6.6) |
| December | 81 | 3.1 (2.1–4.7) | 186 | 5.8 (4.3–7.6) | 142 | 3.4 (2.5–4.5) | 157 | 7.2 (5.4–9.4) | 567 | 4.6 (4.0–5.4) |
EDs = emergency departments, OHCA = out of hospital cardiac arrest
Table 3.
Crude and adjusted odds ratios of seasons and months of admission for survived cardiac arrest patients.
| Crude | Adjusted∗ | |||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Season of admission | ||||||
| Winter (vs all other seasons) | 0.85 | 0.76–0.94 | .002 | 0.85 | 0.71–1.00 | .05 |
| Spring (vs all other seasons) | 1.02 | 0.92–1.14 | .73 | 1.03 | 0.86–1.23 | .77 |
| Summer (vs all other seasons) | 1.2 | 1.08–1.34 | .001 | 1.27 | 1.07–1.52 | .008 |
| Autumn (vs all other seasons) | 0.98 | 0.88–1.09 | .69 | 0.91 | 0.76–1.10 | .34 |
| Month of admission | ||||||
| January (vs all other months) | 0.91 | 0.77–1.07 | .25 | 1.04 | 0.80–1.36 | .78 |
| February (vs all other months) | 0.92 | 0.77–1.10 | .36 | 0.78 | 0.59–1.03 | .08 |
| March (vs all other months) | 0.98 | 0.83–1.17 | .85 | 1.15 | 0.89–1.50 | .28 |
| April (vs all other months) | 1.08 | 0.91–1.27 | .39 | 0.97 | 0.73–1.30 | .83 |
| May (vs all other months) | 0.99 | 0.83 – 1.18 | .90 | 0.95 | 0.72–1.26 | .74 |
| June (vs all other months) | 1.27 | 1.08–1.50 | .005 | 1.43 | 1.08–1.89 | .01 |
| July (vs. all other months) | 1.15 | 0.97–1.36 | .11 | 1.14 | 0.86–1.51 | .36 |
| August (vs. all other months) | 1.07 | 0.90–1.27 | .42 | 1.11 | 0.84–1.47 | .46 |
| September (vs. all other months) | 1.02 | 0.86–1.23 | .79 | 1.08 | 0.81–1.45 | .59 |
| October (vs. all other months) | 0.91 | 0.77–1.09 | .32 | 0.91 | 0.69–1.22 | .54 |
| November (vs. all other months) | 1.01 | 0.86–1.19 | .91 | 0.83 | 0.61–1.12 | .21 |
| December (vs. all other months) | 0.80 | 0.68–0.95 | .01 | 0.81 | 0.63–1.04 | .10 |
Adjusted for: age; sex; admission day is a weekend; factors influencing health status and contact with health services; endocrine, nutritional, and metabolic diseases and immunity disorders; diseases of the respiratory system; symptoms, signs, and ill-defined conditions; mental disorders; diseases of the genitourinary system; diseases of the nervous system and sense organs; injury diagnosis reported on records; primary expected payer; patient location: NCHS urban-rural code; median household income national quartile for patient ZIP code; region of hospital; diagnosis (Ventricular fibrillation and ventricular flutter); Procedures. (0, 1, ≥2).
Table 4.
Adjusted∗ odds ratios of seasons and months of admission for survived cardiac arrest patients stratified by hospital region.
| Northeast | Midwest | South | West | |||||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Season of admission† | ||||||||||||
| Winter | 0.75 | 0.48–1.17 | .20 | 0.91 | 0.66–1.27 | .58 | 0.82 | 0.60–1.12 | .21 | 0.77 | 0.55–1.09 | .15 |
| Spring | 0.96 | 0.61–1.49 | .84 | 1.05 | 0.76–1.47 | .76 | 1.09 | 0.79–1.51 | .61 | 0.97 | 0.67–1.40 | .87 |
| Summer | 1.50 | 0.94–2.39 | .09 | 1.13 | 0.78–1.64 | .51 | 1.06 | 0.77–1.47 | .72 | 1.76 | 1.25–2.48 | .001 |
| Autumn | 0.95 | 0.58–1.56 | .83 | 0.93 | 0.65–1.34 | .70 | 1.05 | 0.77–1.45 | .75 | 0.77 | 0.54–1.10 | .15 |
| Month of admission‡ | ||||||||||||
| January | 0.89 | 0.46–1.71 | .72 | 1.24 | 0.76–2.01 | .39 | 1.02 | 0.64–1.62 | .94 | 0.90 | 0.49–1.63 | .72 |
| February | 0.76 | 0.35–1.65 | .49 | 0.90 | 0.54–1.50 | .69 | 0.63 | 0.38–1.03 | .07 | 0.68 | 0.39–1.20 | .18 |
| March | 1.82 | 0.98–3.40 | .06 | 0.89 | 0.52–1.51 | .65 | 1.67 | 1.12–2.50 | .01 | 0.81 | 0.47–1.42 | .47 |
| April | 0.79 | 0.39–1.62 | .52 | 1.08 | 0.61–1.92 | .79 | 0.66 | 0.37–1.17 | .15 | 1.46 | 0.90–2.36 | .13 |
| May | 0.72 | 0.38–1.35 | .30 | 1.19 | 0.75–1.88 | .47 | 1.05 | 0.63–1.76 | .85 | 0.74 | 0.36–1.52 | .41 |
| June | 2.25 | 1.18–4.27 | .01 | 1.31 | 0.74–2.32 | .35 | 0.84 | 0.50–1.42 | .52 | 2.26 | 1.38–3.71 | .001 |
| July | 0.77 | 0.33–1.79 | .55 | 1.02 | 0.56–1.86 | .95 | 1.43 | 0.91–2.26 | .13 | 1.26 | 0.71–2.23 | .43 |
| August | 1.45 | 0.68–3.07 | .34 | 1.00 | 0.57–1.77 | .99 | 0.97 | 0.56–1.69 | .91 | 1.39 | 0.89–2.17 | .15 |
| September | 1.52 | 0.70–3.31 | .29 | 1.07 | 0.65–1.75 | .81 | 1.39 | 0.87–2.23 | .17 | 0.74 | 0.40–1.34 | .31 |
| October | 1.60 | 0.86–2.96 | .14 | 0.60 | 0.34–1.07 | .08 | 1.14 | 0.67–1.94 | .63 | 0.78 | 0.47–1.29 | .33 |
| November | 0.41 | 0.18–0.96 | .04 | 1.31 | 0.71–2.43 | .39 | 0.74 | 0.45–1.21 | .23 | 0.90 | 0.52–1.56 | .71 |
| December | 0.74 | 0.41–1.31 | .30 | 0.70 | 0.41–1.18 | .18 | 0.93 | 0.59–1.45 | .74 | 0.86 | 0.53–1.39 | .53 |
Adjusted for the same variables listed under the table, expect for the hospital region that was used to stratify the data set into 4 groups.
Reference for each season is all other seasons.
Reference for each month is all other months.
4. Discussion
This study is the first to use a large nationwide database to examine seasonal variation in out of hospital cardiac arrest presentations and outcomes in the United States. To date, few studies originating from outside the United States have examined the impact of seasonal variation on OHCA presentations and outcomes using emergency department population-based databases. Understanding the environmental association with incidence and outcomes of a specific disease, mainly OHCA, is needed for tailored interventions since OHCA management requires a specific system of care in place. Public education, community initiatives (bystander CPR and AED use), OHCA awareness campaigns targeting the community, EMS and ED providers, and potential refresher training of medical providers might be needed.
In this study, adult OHCA presentations to the ED had an approximate incidence of 147 out of every 100,000 ED presentations and an overall survival rate to hospital discharge of 5.6%. This survival rate falls within the range of OHCA survival to hospital discharge rates reported from a previous EMS based study out of sites in North America[23] (1.1%–8.4%) and is slightly lower than rates reported from a study out of England (7.9%).[24] Variation in OHCA survival rates may be related to different inclusion/exclusion criteria in terms of arrest etiology and to type of databases used for conducting other studies.
This study also shows that the overall incidence of out of hospital cardiac arrest tends peaks during the early winter months (December and January) and that summer season is associated with increased survival from OHCA when compared with all other seasons. Deshmukh et al[25] showed a similar seasonal trend in OHCA hospitalizations using a large national inpatient database from 2000 till 2011. Previous studies have also reported an increase in OHCA incidence with colder temperatures.[15,16,19] Potential factors contributing to this increase in incidence of acute cardiac events may be related to physiologic changes associated with cold weather such as vasoconstriction, increased systolic and diastolic blood pressure, blood viscosity plasma cholesterol, and fibrinogen levels.[26] A previous study out of Texas showed that cold weather is associated with increased mortality risk and that this association is strongest for specific diseases mainly myocardial infarction, respiratory diseases, and ischemic heart diseases.[27] These diseases are usually responsible for the majority of OHCA cases especially in older adults. Other potential contributing factors to increased incidence of OHCA during winter months may include overexertion, cold exposure, missed prescriptions, and changes in eating or exercise habits. Further research is needed to assess the impact of these factors on OHCA incidence and outcomes.
Survival rates differed between different regions in the United States. Most notably, lower survival rates were noted in the southern region when compared with other regions. Nichol et al[23] found a similar trend in North America where the southern region sites had both an increased incidence as well as an increased case-fatality rate. This finding could be related to unmeasured factors such as differences in socioeconomic and racial characteristics, in availability of emergency cardiac care, and in OHCA event related characteristics.[23] Additionally Southern US region includes several states that are considered popular retirement areas with higher concentration of older Americans with potentially higher prevalence of comorbidities such as cardiovascular heart disease. Temporary seasonal migration of elderly population during winter months (Snowbirds) to Southern States is also well described in the literature and might be a contributing factor to the observed lower survival rates in the southern region during winter months.[28]
Limitations of this study are related to its retrospective nature and to characteristics of the database used. NEDS is the largest ED database in the United States however collects limited clinical data elements that are disease specific and lacks pre-hospital information such as pre-hospital bystander interventions, witnessed status, duration of cardiopulmonary resuscitation (CPR), or EMS level of care. Regional differences in community and EMS practice standards of OHCA care and their impact on outcomes were therefore not examined. In-hospital procedures and OHCA specific diagnosis (ventricular fibrillation and ventricular flutter) were however part of the data collected and were included as confounders in order to adjust for clinical severity and characteristics of included cases. The study also included only patients who presented to the ED with OHCA. This may have resulted in excluding patients who were declared dead on scene and were not transported to ED in communities where EMS protocols allow for this which may have resulted in underestimating incidence of OHCA. Another limitation is related to lack of specific climate or weather data elements. More detailed information about ambient temperature and weather conditions would allow for more targeted interventions. Lastly, NEDS dataset is released several years after data collection and the data used for this study are gathered from 2014 population data. Climate changes are not usually drastic in successive years and with similar patterns identified in other studies from previous years it is unlikely that the study findings be different if a more recent dataset is used. Studies examining data collected over several years might however reveal different trends in incidence and outcomes of OHCA.
5. Conclusion
Incidence and outcomes of out of hospital cardiac arrest presentations to the emergency departments in the United States have seasonal variation. Both incidence and mortality of OHCA increase during colder months, and survival is significantly higher in summer season or in June. Exploring how to use this variation to improve outcomes through refresher training of medical providers or through other mitigation plans is needed.
Author contributions
Conceptualization: Mazen J. El Sayed.
Data curation: Rana H. Bachir.
Formal analysis: Rana H. Bachir.
Investigation: Rayan H. El Sibai, Mazen J. El Sayed.
Methodology: Mazen J. El Sayed.
Project administration: Mazen J. El Sayed.
Resources: Rayan H. El Sibai.
Software: Rana H. Bachir.
Supervision: Mazen J. El Sayed.
Validation: Rana H. Bachir.
Visualization: Rana H. Bachir.
Writing – original draft: Rayan H. El Sibai.
Writing – review & editing: Mazen J. El Sayed.
Supplementary Material
Footnotes
Abbreviations: AHRQ = Agency for Healthcare Research and Quality, CI = confidence intervals, HCUP = healthcare cost and utilization project, ICD = International Classification of Diseases, LVAD = left ventricular assist device, NEDS = Nationwide Emergency Department Sample, OHCA = out of hospital cardiac arrest, OR = odds ratios.
How to cite this article: El Sibai RH, Bachir RH, El Sayed MJ. Seasonal variation in incidence and outcomes of out of hospital cardiac arrest: A retrospective national observational study in the United States. Medicine. 2021;100:18(e25643).
Ethics approval and consent to participate: An exemption for the use of this de-identified dataset was obtained from the institutional review board (IRB) office. This database is de-identified prior to use and is defined as limited data set under the HIPAA Privacy.
Consent for publication: Not applicable.
The authors declare that they have no competing interests.
There are no reported sources of funding for the research.
The datasets generated during and/or analyzed during the current study are publicly available.
Supplemental digital content is available for this article.
References
- [1].Adrie C, Cariou A, Mourvillier B, et al. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: the OHCA score. Eur Heart J 2006;27:2840–5. [DOI] [PubMed] [Google Scholar]
- [2].McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. MMWR Surveill Summ 2011;60:01–19. [PubMed] [Google Scholar]
- [3].Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women--2011 update: a guideline from the american heart association. Circulation 2011;123:1243–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sanghavi P, Jena AB, Newhouse JP, et al. Outcomes after out-of-hospital cardiac arrest treated by basic vs advanced life support. JAMA Intern Med 2015;175:196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Fouche PF, Simpson PM, Bendall J, et al. Airways in out-of-hospital cardiac arrest: systematic review and meta-analysis. Prehospital Emerg Care 2014;18:244–56. [DOI] [PubMed] [Google Scholar]
- [6].Sasson C, Rogers MAM, Dahl J, et al. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63–81. [DOI] [PubMed] [Google Scholar]
- [7].Bunch TJ, White RD, Khan AH, et al. Impact of age on long-term survival and quality of life following out-of-hospital cardiac arrest. Crit Care Med 2004;32:963–7. [DOI] [PubMed] [Google Scholar]
- [8].Clarke SO, Schellenbaum GD, Rea TD. Socioeconomic status and survival from out-of-hospital cardiac arrest. Acad Emerg Med 2005;12:941–7. [DOI] [PubMed] [Google Scholar]
- [9].Eisenberg M, White RD. The unacceptable disparity in cardiac arrest survival among American communities. Ann Emerg Med 2009;54:258–60. [DOI] [PubMed] [Google Scholar]
- [10].Holzer M, Bernard SA, Hachimi-Idrissi S, et al. Hypothermia for neuroprotection after cardiac arrest: systematic review and individual patient data meta-analysis. Crit Care Med 2005;33:414–8. [DOI] [PubMed] [Google Scholar]
- [11].Lecky F, Bryden D, Little R, et al. Emergency intubation for acutely ill and injured patients. Cochrane Database Syst Rev 2008;CD001429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Koscik C, Pinawin A, McGovern H, et al. Rapid epinephrine administration improves early outcomes in out-of-hospital cardiac arrest. Resuscitation 2013;84:915–20. [DOI] [PubMed] [Google Scholar]
- [13].Hung SW, Chu CM, Su CF, et al. Effect of preceding medications on resuscitation outcome of out-of-hospital cardiac arrest. J Investig Med 2017;65:689–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bagai A, McNally BF, Al-Khatib SM, et al. Temporal differences in out-of-hospital cardiac arrest incidence and survival. Circulation 2013;128:2595–602. [DOI] [PubMed] [Google Scholar]
- [15].The Eurowinter Group. Cold exposure, winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, all causes in warm, cold regions of Europe. Lancet Lond Engl 1997;349:1341–6. [PubMed] [Google Scholar]
- [16].Analitis A, Katsouyanni K, Biggeri A, et al. Effects of cold weather on mortality: results from 15 European cities within the PHEWE project. Am J Epidemiol 2008;168:1397–408. [DOI] [PubMed] [Google Scholar]
- [17].Niu Y, Chen R, Liu C, et al. The association between ambient temperature and out-of-hospital cardiac arrest in Guangzhou, China. Sci Total Environ 2016;572:114–8. [DOI] [PubMed] [Google Scholar]
- [18].Fukuda T, Ohashi N, Doi K, et al. Impact of seasonal temperature environment on the neurologic prognosis of out-of-hospital cardiac arrest: a nationwide, population-based cohort study. J Crit Care 2014;29:840–7. [DOI] [PubMed] [Google Scholar]
- [19].Onozuka D, Hagihara A. Associations of day-to-day temperature change and diurnal temperature range with out-of-hospital cardiac arrest. Eur J Prev Cardiol 2017;24:204–12. [DOI] [PubMed] [Google Scholar]
- [20].Overview of the nationwide emergency department sample (NEDS). HCUP website. Available at: https://www.hcup-us.ahrq.gov/nedsoverview.jsp. Accessed November 13, 2018. [Google Scholar]
- [21].HCUP methods series. Population denominator data for use with the HCUP databases (updated with 2014 population data). Report # 2015-07. Available at: https://www.hcup-us.ahrq.gov/reports/methods/2015-07.pdf. Accessed November 13, 2018. [Google Scholar]
- [22].HCUPnet [Internet]. HCUPnet. Available at: https://hcupnet.ahrq.gov. Accessed November 13, 2018. [Google Scholar]
- [23].Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA J Am Med Assoc 2008;300:1423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hawkes C, Booth S, Ji C, et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation 2017;110:133–40. [DOI] [PubMed] [Google Scholar]
- [25].Deshmukh A, Patel NJ, Deshmukh A, et al. Abstract 51: seasonal variation in out-of-hospital cardiac arrest. Circulation 2014;130: suppl: A51–151. [Google Scholar]
- [26].Giang PN, Dung do V, Bao Giang K, et al. The effect of temperature on cardiovascular disease hospital admissions among elderly people in Thai Nguyen Province, Vietnam. Glob Health Action 2014;7:23649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Chen TH, Li X, Zhao J, et al. Impacts of cold weather on all-cause and cause-specific mortality in Texas, 1990-2011. Environ Pollut 2017;225:244–51. [DOI] [PubMed] [Google Scholar]
- [28].Smith SK, House M. Snowbirds, sunbirds, and stayers: seasonal migration of elderly adults in Florida. J Gerontol B Psychol Sci Soc Sci 2006;61:S232–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


