Abstract
Background:
The reperfusion therapy using primary percutaneous coronary intervention (PPCI) in ST-segment elevation myocardial infarction (STEMI) is known to give a better result than fibrinolytic therapy. The fast access to PPCI will improve hospital outcome. We believe that patient access to PPCI facility would have improved due to enhanced public awareness and expanding evidenced-based health provision.
Methods:
This is a single-center retrospective study to analyze and compare data for STEMI patients. Patients were transferred to our hospital during the year 2010. Group l comprised 223 patients. Group 2 comprised 288 patients. Group 2 patients were those treated between August 2014 and August 2015. We compared their demographic and baseline characteristics, patients' access to the hospital, reasons for no access, and hospital mortality for the two groups.
Results:
Among the 288 patients in Group 2, 247 patients (85%) were males with an average age of 57 years, 49% were diabetics, 48% were hypertensive, 48% were smokers, and 27% were obese. These were not different in Group 1. In Group 2, 164 patients (57%) only had access to PPCI compared to 56% in Group 1 (P = 0.536-NS). In G2, the main reasons for no PPCI were late presentation in 47% versus 53% in Group 1; P = 0.34 NS. In Group 2, 27% were due to thrombolysis versus 17% in Group 1 (P = 0.11 NS). Hospital mortality in Group 2 was 4% in those treated with PPCI compared to 2.3% in Group 1 (P = 0.522-NS). Mortality in patients who did not receive PPCI in Group 2 was 8% compared to 11.3% in Group 1 (P = 0.49-NS). Females in Group 2 have about 3 times higher mortality. Patients treated for STEMI in the last 12 months at King Abdulaziz Cardiac Center still have relatively low access to PPCI due mainly to persistent pattern of late presentation and prior thrombolysis, which reflect apparent lack of direct access to hospitals with PPCI facilities.
Conclusion:
Comparing the two periods, there was no change in cardiology practice. The low access to PPCI was mainly due to late presentation and prior thrombolysis. Hospital mortality rate for patients treated with PPCI remained low during the two era. This seemingly relates to both lack of public awareness and health provision factors in PPCI organizations.
Keywords: Coronary artery disease, electrocardiogram, first medical contact, primary percutaneous coronary intervention, ST-elevation myocardial infarction
INTRODUCTION
The majority of patients with ST-segment elevation myocardial infarction (STEMI) diagnosis, who arrive in a facility with access to catheterization laboratory (Cath Lab), will achieve an excellent benefit from rapid reperfusion by the primary percutaneous coronary intervention (PPCI) than from fibrinolytic therapy.[1] At the same time, fibrinolysis is an equal alternative for patients with no access to a Cath Lab facility with percutaneous coronary intervention (PCI).[2] The American College of Cardiology/American Heart Association recommends a maximum delay of 90 min between first medical contact (FMC) and balloon inflation for PPCI.[3] The delays of fast coronary intervention were associated with re-hospitalization with heart failure and STEMI, and this may lead to more deaths.[4,5]
A timely access to reperfusion therapy and Cath lab facility seems to be more beneficial and significant than other treatment strategy. The initiation and development of an integrated system of care will permit timely access to Cath lab facilities. This will allow patients to have appropriate care within the required time.
During myocardial infarction, the timing of revascularization is very important. Delays do occur: (1) prehospital delay – the interval between FMC and arrival at a Cath Lab Facility and (2) door-to-balloon (D2B) interval.[6,7]
The following variables have been demonstrated to reduce D2B delay with respect to prehospital intervals: improvement of prehospital care protocols, with prehospital diagnosis of STEMI by electrocardiogram (ECG) recording and interpretation during ambulance transport; prehospital activation of cardiac catheterization laboratory; direct referral to PCI center without interhospital transfers; and emergency department (ED) bypass at the PCI center.[8,9,10]
By reducing prehospital system delays, new and integrative approaches to STEMI patient care can improve access to PCI in rural populations that would not otherwise have timely access.
The objective of our study is to evaluate whether or not any difference happened in the STEMI management between 2010 and 2015 regarding access to PPCI and awareness.[11,12,13]
METHODS
Study population
This study was a retrospective, single-center, observational study conducted at King Abdulaziz Cardiac Center (KACC). All patients who were admitted between August 2014 and August 2015 with a diagnosis of STEMI were included and classified according to their access to PPCI, and we compared the outcome with the patients who had STEMI in 2010.
Definition
STEMI patient was defined as new onset of chest pain with ECG criteria of ST-segment elevation of at least >0.1 mV all leads, minimum of two consecutive leads, ≥0.2 mV for V1–V3, or new or presumably new left bundle branch block accompanying chest pain. Serum cardiac biomarkers used to assist in the diagnosis of myocardial injury were positive.
Statistical analysis
We used Student's t-test to compare continuous variables and Chi-square test to compare categorical variables to assess group differences. All tests were two-sided, with a 5% level of significance. Statistical analysis was done using IBM®SPSS® version 23.
RESULTS
A total number 288 patients (Group 2) were diagnosed with STEMI; 247 patients (85%) were males with average age of 57 years. Nearly 49% were diabetics, 48% hypertensive, 48% were smokers, and 27% were obese [Table 1].
Table 1.
Baseline characteristics of both groups
| Group 2 | Group 1 | |
|---|---|---|
| Number | 288 | 223 |
| Age(mean) | 57y | 56y |
| Sex(M) | 85% | 83% |
| DM | 49% | 52% |
| HTN | 48% | 46% |
| Smoker | 48% | 45% |
| Obesity | 27% | 26% |
| Hyperlipidemia | 52% | 52% |
These were not different in (Group 1) 223 patients. Of Group 2, 164 patients (57%) only had access to PPCI compared to 56% in Group 1 (P = 0.536-NS) [Figure 1].
Figure 1.
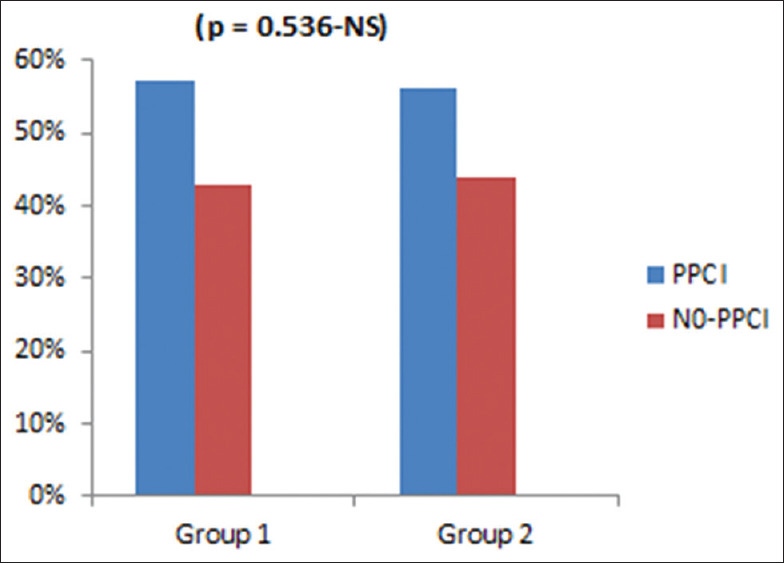
The difference in both groups for primary percutaneous coronary intervention versus non.primary percutaneous coronary intervention
In Group 2, the main reasons for no PPCI were late presentation in 47% versus 53% in Group 1; P = 0.34 NS and 27% due to thrombolysis versus 17% in Group 1 (P = 0.11 NS) [Figure 2].
Figure 2.
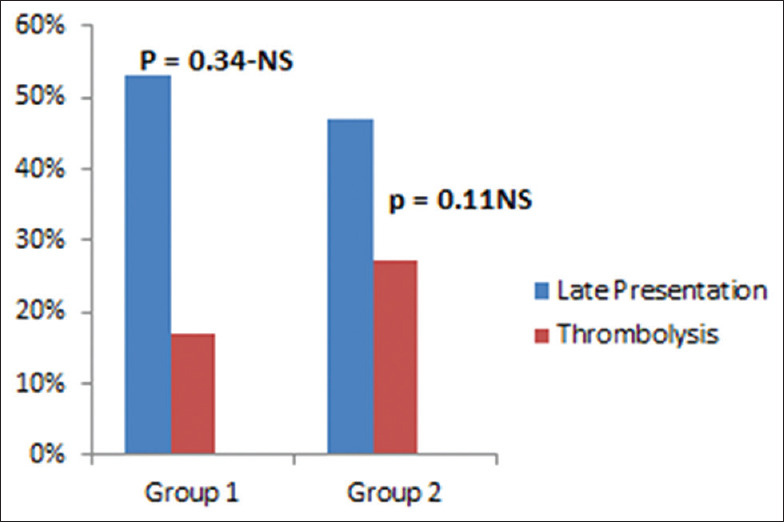
The difference in both groups for late presentation versus thrombolysis
Hospital mortality in Group 2 was 4% in those treated with PPCI compared to 2.3% in Group 1 (P = 0.522-NS). Mortality in patients who did not receive PPCI in Group 2 was 8% compared to 11.3% in Group 1 (P = 0.49-NS) [Figure 3].
Figure 3.
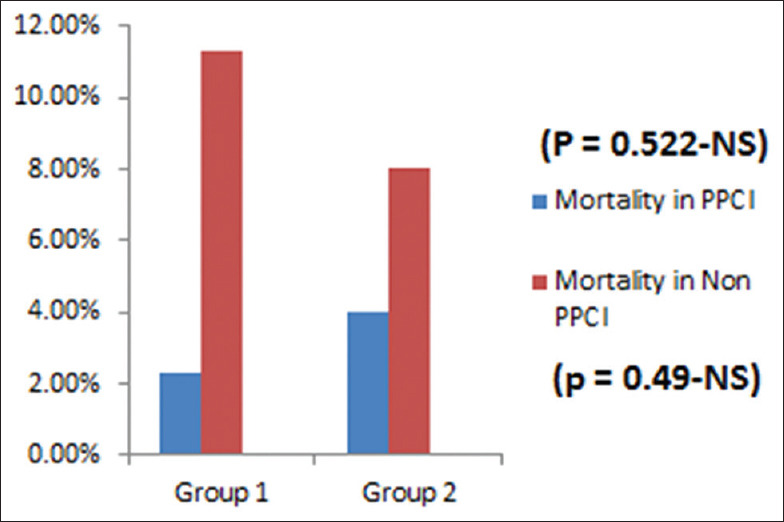
The difference in mortality in both groups for primary percutaneous coronary intervention versus nonprimary percutaneous coronary intervention
Females in Group 2 have about three times higher mortality. Compared to 2010, patients treated for STEMI in the past 12 months at KACC still have same, relatively low access to PPCI due mainly to persistent pattern of late presentation and prior thrombolysis, which reflect apparent lack of direct access to hospitals with PPCI facilities.
CONCLUSION
Data from 2010 at KACC showed relatively low access to PPCI for STEMI patients primarily due to late presentation and initial thrombolysis. We believe that patient access to PPCI would have improved over the past 5 years due to improved public awareness and expanding evidenced-based health provision.
DISCUSSION
Our study showed in big difference occurred in the practice of STEMI management, in the period between 2010 and 2015, regarding the access to PPCI. In North American rural communities, long transport times create challenges in access to PCI for STEMI patients. Nevertheless, the studies showed that patient access to PCI within a 60-min prehospital standard is possible in a regionalized PCI system and should be encouraged.[14,15]
The ground ambulance transport for patients located over 110 km from a PCI center achieved timely access. In the province of Quebec in Canada, helicopter transfer is not available. Implementation of several evidence-based strategies helped reach that goal including multiple prehospital ECGs, rerouting patients to the closest PCI center without interhospital transfer, activation of catheterization laboratory during ambulance transport, and ED bypass at PCI centers.[13,16] The regional STEMI system was designed to achieve the benchmark of a 90-min interval between STEMI diagnosis and balloon inflation; this interval allows for 60-min ambulance transport and 30 min for D2B inflation. Cheskes et al. defined FMC as the moment that paramedics arrived at the scene.[16,17] Using this definition, their system achieved a (median) 70-min interval between FMC and balloon inflation, for a median travel distance of 16.1 kmand a maximum distance of 49.2 km. Other studies have used a more conservative operational definition, defining FMC as the moment that the 911 call was received.[18,19] A Danish study reported that median FMC to balloon interval was 93 min in a rural region for a maximum 100 km transport distance.[19]
Terkelsen et al. proposed a nomenclature of delays that would track STEMI patients from symptom onset to balloon inflation: patient delay, followed by prehospital system delay, followed by D2B delay.[4,16,20,21]
Time to reperfusion therapy found in our study and others was above that recommended by national and international guidelines.[22,23] In general, patients do not seek medical care until 1.5–2 h after the onset of pain. This reality has not changed significantly in the past 10 years, despite the implementation of specific public policies.[24]
Previous studies have identified reasons for the increase in patient's delay time. The main component of patient delay time: the perception that the symptom is self-limiting, attributing the symptoms to other conditions, fear of disturbing others, fear that the symptoms are a false alarm, lack of knowledge of the importance of quick action and lack of awareness that one should call the EMS.[25,26]
CONCLUSION
Comparing the two periods, there was no change in the cardiology practice. The low access to PPCI was mainly due to late presentation, and prior thrombolysis, hospital mortality rate for patients treated with PPCI remained low during the two era, relating to lack of public awareness and health provision factors in PPCI organizations.
Limitation of the study
This study was a single-center study, and patient numbers and samples are small sized compared with international centers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The author's special thanks to catheterization laboratory staff including consultants, residents, nurses, technicians, and to all who entered data into computers at KACC.
REFERENCES
- 1.de Boer SP, Barnes EH, Westerhout CM, Simes RJ, Granger CB, Kastrati A, et al. High-risk patients with ST-elevation myocardial infarction derive greatest absolute benefit from primary percutaneous coronary intervention: Results from the primary coronary angioplasty trialist versus thrombolysis (PCAT)-2 collaboration. Am Heart J. 2010;161:500–7e1. doi: 10.1016/j.ahj.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 2.Lambert L, Brown K, Segal E, Brophy J, Rodes-Cabau J, Bogaty P. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. JAMA. 2010;303:2148–55. doi: 10.1001/jama.2010.712. [DOI] [PubMed] [Google Scholar]
- 3.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 4.Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–71. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 5.Terkelsen CJ, Jensen LO, Tilsted HH, Trautner S, Johnsen SP, Vach W, et al. Health care system delay and heart failure in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention: Follow-up of population-based medical registry data. Ann Intern Med. 2011;155:361–7. doi: 10.7326/0003-4819-155-6-201109200-00004. [DOI] [PubMed] [Google Scholar]
- 6.Diercks DB, Kontos MC, Chen AY, Pollack Jr CV, Wiviott SD, Rumsfeld JS, et al. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: Data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol. 2009;53:161–6. doi: 10.1016/j.jacc.2008.09.030. [DOI] [PubMed] [Google Scholar]
- 7.Ong ME, Wong AS, Seet CM, Teo SG, Lim BL, Ong PJ, et al. Nationwide improvement of door-to-balloon times in patients with acute ST-segment elevation myocardial infarction requiring primary percutaneous coronary intervention with out-of-hospital 12-lead ECG recording and transmission. Ann Emerg Med. 2013;61:339–47. doi: 10.1016/j.annemergmed.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 8.Rezaee ME, Conley SM, Anderson TA, Brown JR, Yanofsky NN, Niles NW. Primary percutaneous coronary intervention for patients presenting with ST-elevation myocardial infarction: Process improvements in rural prehospital care delivered by emergency medical services. Prog Cardiovasc Dis. 2010;53:210–8. doi: 10.1016/j.pcad.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Camp-Rogers T, Dante S, Kontos MC, Roberts CS, Kreisa L, Kurz MC. The impact of prehospital activation of the cardiac catheterization team on time to treatment for patients presenting with ST-segment-elevation myocardial infarction. Am J Emerg Med. 2011;29:1117–24. doi: 10.1016/j.ajem.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Kontos MC, Kurz MC, Roberts CS, Joyner SE, Kreisa L, Ornato JP, et al. Emergency physician-initiated cath lab activation reduces door to balloon times in ST-segment elevation myocardial infarction patients. Am J Emerg Med. 2011;29:868–74. doi: 10.1016/j.ajem.2010.03.025. [DOI] [PubMed] [Google Scholar]
- 11.Fosbol EL, Granger CB, Jollis JG, Monk L, Lin L, Lytle BL, et al. The impact of a statewide pre-hospital STEMI strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation. 2013;127:604–12. doi: 10.1161/CIRCULATIONAHA.112.118463. [DOI] [PubMed] [Google Scholar]
- 12.Le May MR, So DY, Dionne R, Glover CA, Froeschl MP, Wells GA, et al. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2008;358:231–40. doi: 10.1056/NEJMoa073102. [DOI] [PubMed] [Google Scholar]
- 13.Bagai A, Jollis JG, Dauerman HL, Peng SA, Rokos IC, Bates ER, et al. Emergency department bypass for ST-Segment-elevation myocardial infarction patients identified with a prehospital electrocardiogram: A report from the American Heart Association Mission: Lifeline program. Circulation. 2013;128:352–9. doi: 10.1161/CIRCULATIONAHA.113.002339. [DOI] [PubMed] [Google Scholar]
- 14.Plourde G, Abdelaal E, Bataille Y, MacHaalany J, Dery JP, Dery Y, et al. Effect on door-to-balloon time of immediate transradial percutaneous coronary intervention on culprit lesion in ST-elevation myocardial infarction compared to diagnostic angiography followed by primary percutaneous coronary intervention. Am J Cardiol. 2013;111:836–40. doi: 10.1016/j.amjcard.2012.11.059. [DOI] [PubMed] [Google Scholar]
- 15.Aguirre FV, Varghese JJ, Kelley MP, Lam W, Lucore CL, Gill JB, et al. Rural interhospital transfer of ST-elevation myocardial infarction patients for percutaneous coronary revascularization: The Stat Heart Program, Circulation. 2008;117:1145–52. doi: 10.1161/CIRCULATIONAHA.107.728519. [DOI] [PubMed] [Google Scholar]
- 16.Blankenship JC, Scott TD, Skelding KA, Haldis TA, Tompkins-Weber K, Sledgen MY, et al. Door-to-balloon times under 90 min can be routinely achieved for patients transferred for ST-segment elevation myocardial infarction percutaneous coronary intervention in a rural setting. J Am Coll Cardiol. 2011;57:272–9. doi: 10.1016/j.jacc.2010.06.056. [DOI] [PubMed] [Google Scholar]
- 17.Cheskes S, Turner L, Foggett R, Huiskamp M, Popov D, Thomson S, et al. Paramedic contact to balloon in less than 90 minutes: A successful strategy for ST-segment elevation myocardial infarction bypass to primary percutaneous coronary intervention in a Canadian emergency medical system. Prehosp Emerg Care. 2011;15:490–8. doi: 10.3109/10903127.2011.598613. [DOI] [PubMed] [Google Scholar]
- 18.Studnek JR, Garvey L, Blackwell T, Vandeventer S, Ward SR. Association between prehospital time intervals and ST-elevation myocardial infarction system performance. Circulation. 2010;122:1464–9. doi: 10.1161/CIRCULATIONAHA.109.931154. [DOI] [PubMed] [Google Scholar]
- 19.Sorensen JT, Terkelsen CJ, Norgaard BL, Trautner S, Hansen TM, Botker HE, et al. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur Heart J. 2011;32:430–6. doi: 10.1093/eurheartj/ehq437. [DOI] [PubMed] [Google Scholar]
- 20.Lassen JF, Botker HE, Terkelsen CJ. Timely and optimal treatment of patients with STEMI. Nat Rev Cardiol. 2013;10:41–8. doi: 10.1038/nrcardio.2012.156. [DOI] [PubMed] [Google Scholar]
- 21.Henry TD, Sharkey SW, Burke MN, Chavez IJ, Graham KJ, Henry CR, et al. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–8. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 22.Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006;27:789–95. doi: 10.1093/eurheartj/ehi774. [DOI] [PubMed] [Google Scholar]
- 23.Lambrew CT, Bowlby LJ, Rogers WJ, Chandra NC, Weaver WD. Factors influencing the time to thrombolysis in acute myocardial infarction. Time to Thrombolysis Substudy of the National Registry of Myocardial Infarction-1. Arch Intern Med. 1997;157:2577–82. [PubMed] [Google Scholar]
- 24.Davis C. Prehospital delay in patients with acute coronary syndromes (from the global registry of acute coronary events [GRACE]) J Emerg Med. 2009;37:347. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 25.Leslie WS, Urie A, Hooper J, Morrison CE. Delay in calling for help during myocardial infarction: Reasons for the delay and subsequent pattern of accessing care. Heart. 2000;84:137–41. doi: 10.1136/heart.84.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKinley S, Moser DK, Dracup K. Treatment-seeking behavior for acute myocardial infarction symptoms in North America and Australia. Heart Lung. 2000;29:237–47. doi: 10.1067/mhl.2000.106940. [DOI] [PubMed] [Google Scholar]


