Abstract
The COVID-19 pandemic has awakened the need for telemedicine and teleconsultation to continue medical care while maintaining social distancing for safety against infection. The concept of the electronic intensive care unit (e-ICU) is evolving rapidly in developed nations. e-ICU in developing countries like India not only has great potential but also has many roadblocks. This article showcases the concept, advantages, and challenges of e-ICU in India, with a glimpse of the future.
KEY WORDS: COVID-19, electronic intensive care unit, remote consultation, teleintensive care unit, telemedicine
INTRODUCTION
The COVID-19 pandemic has spread to over 200 countries, thinning out medical resources everywhere. Even though mortality has been seen in only a small proportion of cases, for a populous country like India, with its very limited critical care services, the intensive care units (ICU) have been overwhelmed. Moreover, the availability of specialists and intensivists in distant and remote places is scarce. The burden imposed by COVID-19 calls for a reorganization of medical care teams and the expansion of hospital and ICU capacities. The creation of manpower, for example, critical care specialists, at all places in a short time interval may not be feasible. The alternate option could be to take the help of existing specialists for consulting from remote areas. This requires the reworking of existing infrastructure and the inclusion of telemedicine using electronic platforms.
ELECTRONIC INTENSIVE CARE UNIT
With the strain on traditional ICUs, electronic ICUs (e-ICU) are probably the best way ahead. e-ICU is a platform where all patient data, clinical profiles, investigations, and treatments can be stored and remotely accessed and monitored. It electronically links patients in ICUs and high dependency units, with their doctors, nurses, administrative staff, and even their kin. It allows for smart alarm systems with rapid troubleshooting protocols, teleconsultations with experts and specialists, and automated real-time monitoring of patient parameters. Continuous monitoring (24 × 7) of patients can be done remotely through e-monitoring.[1] Figure 1 represents the key aspects of a functioning e-ICU in a simplified pictorial representation.
Figure 1.
A pictorial representation of an electronic intensive care unit showing patient data being recorded (a) and relayed by a monitor (b) to a central monitoring desk (c) and accessed by a doctor in a remote location (d)
In India, electronic recording of ICU data is far from reality, making setting up an e-ICU a mammoth task. However, the COVID-19 pandemic has brought a realization of its urgent need. Karnataka was the first state in India to establish a dedicated command center for critical care support, by linking ICUs of COVID-19 hospitals onto a single platform. The entire unit was monitored by a centralized team of doctors. Cumulative data were monitored and analyzed by experts in real time.[2] The role of eNeuroIntensive care is not nascent, with references to such models dating back to a few years.[3] Hence, the present need mandates creation of such electronic hubs for better patient care, with the involvement of experts across the world connected through electronic means. Health-care workers who shall be working and coordinating together need to be trained in various aspects of an e-ICU. Training programs for this remain simple and can be done locally as well as through online mode. The IT infrastructure required for the creation of an eICU is available and may be useful. With the availability of financial resources, integration of electronic gadgets may further be integrated like the use of e-stethoscope, robots, e-otoscope, etc.
The e-ICU can be conceptualized into four basic components.[4] First is the patient's room, where a two-way audio-visual device, consisting of a microphone, a camera, a screen, and speakers, is required. Next, biomedical monitors and sensors to record information about a patient's condition are essential. Modern ventilators, infusion pumps, and patient beds can all be adjusted remotely from a central monitoring station. All these are existing technologies that are in use, at least partly, in traditional ICUs. At present, all this information is conveyed to a central monitoring station, where health-care professionals can monitor patient indices and vitals and adjust ventilator and other settings. In an e-ICU, this information needs to be communicated to remotely located intensivists and nonintensive care specialists. This is achieved by robust and secure internet connectivity, the likes of which are already being used in other sectors such as banking and monetary transactions. This always-on internet connection is the second and possibly the most important component. The third component includes doctors who are managing the patient. Intensivists, pulmonologists, cardiologists, radiologists, neurologists, neurosurgeons, etc., can all monitor their patients, alter treatment and machine settings, and review and advise investigations from a remote location and in real time. In addition, this also allows for multidisciplinary discussions to improve patient outcomes. The final component involves a technology that is currently rapidly growing. The entirety of patient data, from recordings obtained from sensors to patient investigation reports, from ventilator settings to pharmacotherapy, and much more can be recorded in a single digital case file. Data from the patient's admissions and visits in the past can also be accessed. With the help of computational intelligence and machine learning, this barrage of data can be converted into meaningful information.
PRACTICAL APPLICATION OF ELECTRONIC INTENSIVE CARE UNIT IN INDIA
Cardiology has already seen a benefit in the reduction of morbidity and mortality in STEMI patients using remote care.[5] Applying similar principles in critical care can easily help in multiple ways. A unique advantage of using telemedicine is that, in the e-ICU, even quarantined health–care providers, whose numbers are steadily increasing worldwide in the COVID-19 pandemic, can continue to provide teleconsultations. Detailed guidelines from central health authorities and telemedicine society in India have been released recently for the same.[6]
With personal distancing and shortage of personal protective equipment (PPE), face–to–face health–care encounters are increasingly becoming problematic even in a hospital setting. A different form of telemedicine, “distant monitoring within the premises,” can be easily brought into practice. Communication with an inpatient in an isolated area can be by audio or video aids including smartphones. All vitals can be evaluated from a central monitoring station.
Multiple ICU within a tertiary care hospital can be linked and managed through a common online portal with multiple access points. Besides, one intensivist can monitor a particular patient more vigilantly and continuously if required.
Similarly, a link between multiple quarantine centers for the suspect cases and isolation centers for mild patients can be made. The protocols for managing suspect cases with their reports and monitoring mild cases for deterioration can be followed through the e-platform.
PLAN AND STRATEGY REQUIRED
The commitment from central authorities, local health-care experts, and society is necessary to plan and implement e-ICU. Modern cameras, smartphones, and computers need to be available at multiple places throughout the health-care facility. Once the hardware is installed, software programs and platforms need to be developed with the help of information technology (IT) professionals. The training of all health-care workers (HCWs) on the use of these platforms has to be enforced. Real-time recording of patient details can be enabled in smartphones of HCW with appropriate alarm settings. These programs must be synchronized and carry necessary troubleshoot strategies that are immediately enforced.
The essence of an e-ICU is to offer real-time monitoring from a location that may not be in the proximity of the patient, without compromising the standards of care. Achieving this in the era of worldwide internet connectivity and state-of-the-art patient sensors, medication devices and ventilators may be easier than can be imagined.
TRAINING – THE FUEL TO ELECTRONIC INTENSIVE CARE UNIT
Infrastructure and workforce are useless if there is no training on the practical utility of the same. The various components of e-ICU need regular training and updating e-skills [Table 1]. Extensive and meticulous training of personnel is central for achieving the highest possible benefits of e-ICUs over traditional ones. The existing telemedicine education programs train doctors to effectively assess and manage their patients through e-consultations. These can be utilized even for the e-ICU. However, a large amount of real-time data and trends over time are available on screen for the remotely located doctor. Additional training may be required for learning ways to access and cross-referencing all of the data. Once put into practice, this aspect positively impacts the quality of care and outcomes. The on-site ICU staff needs to be trained not only in the workings and applications of sensors and devices but also to actively troubleshoot with additional technology that is not a part of traditional ICUs. Training for remote management of critically ill patients is being increasingly included in curricula in centers across the world.[7]
Table 1.
Preparation and planning of eintensive care unit
| Requirement | Components | Remarks |
|---|---|---|
| Infrastructure | ||
| ICU | High-speed network connectivity, integrated PACS | Needs government and authorities to setup. It is part of the basic |
| Integrated HMS | requirement | |
| CCTV | ||
| Command center | Monitors | These are available at tertiary care centers, but need to be setup in the |
| Audiovisual interaction | remotest of ICU | |
| High-speed network connectivity | ||
| Manpower | ||
| ICU | IT personnel backup | There is a need to augment the recruitment and training of these staff |
| Nursing staff | for the same | |
| Doctor | ||
| Command center | Critical care expert | There is a need to augment recruitment and training of these staff for |
| IT personnel backup | the same | |
| Training | ||
| ICU | Understanding and interpreting online data and its transmission to command center | Training of the staff required with regular updates |
| Command center | Understanding and interpreting online data and its transmission to ICU | Professional IT workforce needs to be involved |
ICU: Intensive care unit, IT: Information technology, CCTV: Closed-circuit television, PACS: Picture archiving and communication system, HMS: Hospital management software
ADVANTAGES AND LONG-TERM BENEFITS OF ELECTRONIC INTENSIVE CARE UNIT
There is a multitude of advantages with e-ICU that justifies the urgent need in the COVID-19 era. Cumulative data are monitored and analyzed by experts in real time. This can reduce the workforce of HCWs required, besides allowing the existing medical staff to work in rotation to ensure continued availability. It offers a safe face-to-face interaction with physical distancing. This will decrease the occupational transmission of the COVID-19 to doctors and save precious PPE, which are also limited in developing countries.
Conversely, quarantined and home-isolated doctors can continue to monitor their patients, without the risk of disease transmission to patients or other HCWs. Cost-cutting can be brought about by saving on the travel of doctors, requirements of PPE, and the required number of HCW.[8] Effective triage and risk stratification can be done easily.
Even patient outcomes have been found to improve with telemedicine applications. In a multicenter case–control study by Lily et al., significantly lower mortality was found in patients managed in an e-ICU.[9] Further, patients at peripheral and remote centers will get access to specialists and experts from other places.[10] The risks and cost of transfer of such patients through hundreds of kilometers across various terrains with limited health equipment can also be avoided. Thus, morbidity and mortality can be reduced to a large extent, especially in these COVID-19 pandemic times besides allowing for better bed and health-care resources utilization. It will allow for the prevention of overburdening of tertiary care centers which also cater to non-COVID patient care.
Multiple specialties of doctors including intensivists, anesthetists, infection control, microbiologists, pulmonologists, and internists can have peer support, common decisions, and academic discussions to improve patient care and outcome. This can stimulate and promote research and data analysis on a large scale.[11]
Eventually, the system can evolve to include teaching and resident training, which will again be real time and patient oriented with a reduction in bedside teaching.
ROADBLOCKS AND CHALLENGES
Even in the tertiary care center ICU in India, there are no electronic records of any patients. There is no existing database and all clinical profiles, investigations, and treatments are maintained in pen-paper format. There is a highly backward system of interdepartmental referral, which eventually is often nonexistent.
There is no record keeping, data analysis, and seldom audits to improve hospital treatment protocols. The HCW including doctors has no training in IT and thus avoids using the e-tools and platforms. The health infrastructure expenditure is a minuscule part of the Gross domestic product (GDP), the doctor: patient ratio is highly skewed, and the poor patients and their kin are often illiterate and oblivious of any technological advancements.
A high cost of setting up and running the whole framework is a hindrance. State-of-the-art hardware and updated and secure software are expensive investments that resource-limited countries may not be able to afford on a large scale. In the long run, however, the ability to deliver a high quality of care would make e-ICUs more valuable than at the time of setting up.[7]
CONCLUSION
e-ICU has undisputed benefits and is the need of the hour [Figure 2]. COVID-19 pandemic should serve as a wake-up call to remove roadblocks and promote the concept and application through joint efforts of the government, hospital authorities, and HCW to reduce critical and sick patients' morbidity and mortality.
Figure 2.
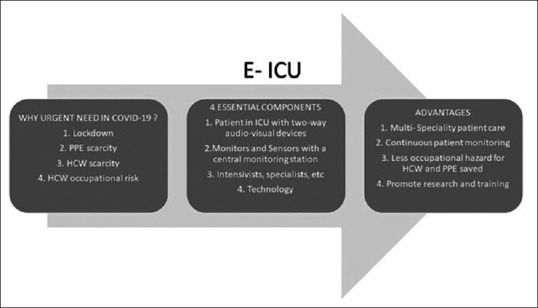
The need, components, and advantages of electronic intensive care unit in the COVID-19 pandemic
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Celi LA, Hassan E, Marquardt C, Breslow M, Rosenfeld B. The eICU: It's not just telemedicine. Crit Care Med. 2001;29(Suppl 8):N183–9. doi: 10.1097/00003246-200108001-00007. [DOI] [PubMed] [Google Scholar]
- 2.Karnataka Sets up Critical Care Support Unit by Linking COVID Hospitals Across State. Press Trust of India. [Last accessed on 2020 Jun 05]. Available from: https://www.businessstandard.com/article/ptistories/karnatakasetsupcriticalcare-supportunitbylinkingcovidhospitalsacrossstate120041500931_1.html .
- 3.Ganapathy K. Telemedicine and neurosciences. Neurol India. 2018;66:642–51. doi: 10.4103/0028-3886.232346. [DOI] [PubMed] [Google Scholar]
- 4.Udeh C, Udeh B, Rahman N, Canfield C, Campbell J, Hata JS. Telemedicine/virtual ICU: Where are we and where are we going? Methodist Debakey Cardiovasc J. 2018;14:126–33. doi: 10.14797/mdcj-14-2-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta S, Dewan S, Kaushal A, Seth A, Narula J, Varma A. eICU reduces mortality in STEMI patients in resource-limited areas. Glob Heart. 2014;9:425–7. doi: 10.1016/j.gheart.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Telemedicine Practice Guidelines Enabling Registered Medical Practitioners to Provide Healthcare Using Telemedicine. Board of governors, in Supersession with Medical Council of India. [Last accessed on 2020 Mar 26]. Available from: https://www.mohfw.gov.in/pdf/Telemedicine.pdf .
- 7.Becker CD, Fusaro MV, Scurlock C. Telemedicine in the ICU: Clinical outcomes, economic aspects, and trainee education. Curr Opin Anaesthesiol. 2019;32:129–35. doi: 10.1097/ACO.0000000000000704. [DOI] [PubMed] [Google Scholar]
- 8.Lilly CM, Mickelson JT. Evolution of the intensive care unit telemedicine value proposition. Crit Care Clin. 2019;35:463–77. doi: 10.1016/j.ccc.2019.02.010. [DOI] [PubMed] [Google Scholar]
- 9.Lilly CM, McLaughlin JM, Zhao H, Baker SP, Cody S, Irwin RS, et al. A multicenter study of ICU telemedicine reengineering of adult critical care. Chest. 2014;145:500–7. doi: 10.1378/chest.13-1973. [DOI] [PubMed] [Google Scholar]
- 10.Iyengar K, Vaish A, Toh E, Vaishya R. COVID-19 and remote consulting strategies in managing trauma and orthopaedics. Postgrad Med J. 2020;96:438–9. doi: 10.1136/postgradmedj-2020-137917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollard TJ, Johnson AE, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU collaborative research database, a freely available multi-center database for critical care research. Sci Data. 2018;5:180178. doi: 10.1038/sdata.2018.178. [DOI] [PMC free article] [PubMed] [Google Scholar]


