Social contacts estimated in the post-lockdown period in four large Chinese cities are not sufficient to sustain local SARS-CoV-2 transmission.
Abstract
Nonpharmaceutical interventions to control SARS-CoV-2 spread have been implemented with different intensity, timing, and impact on transmission. As a result, post-lockdown COVID-19 dynamics are heterogeneous and difficult to interpret. We describe a set of contact surveys performed in four Chinese cities (Wuhan, Shanghai, Shenzhen, and Changsha) during the pre-pandemic, lockdown and post-lockdown periods to quantify changes in contact patterns. In the post-lockdown period, the mean number of contacts increased by 5 to 17% as compared to the lockdown period. However, it remains three to seven times lower than its pre-pandemic level sufficient to control SARS-CoV-2 transmission. We find that the impact of school interventions depends nonlinearly on the intensity of other activities. When most community activities are halted, school closure leads to a 77% decrease in the reproduction number; in contrast, when social mixing outside of schools is at pre-pandemic level, school closure leads to a 5% reduction in transmission.
INTRODUCTION
The novel coronavirus disease 2019 (COVID-19) outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) began in Wuhan City, China in December 2019 and quickly became a global pandemic on 11 March 2020 (1). As of 30 July, a total of 84,292 cases of COVID-19, including 4634 deaths, have been reported in mainland China (2). The epidemic in Wuhan and in the rest of China subsided quickly after implementation of strict containment measures and travel restrictions. With the reduction of domestic cases in China and recent cases primarily originating from international travel (2), strict interventions have been gradually relaxed since February 2020.
In most of mainland China outside of Hubei Province, workplaces were allowed to resume operations after 10 February 2020 (3). Close community management (e.g., only one household member was allowed to purchase supplies every 3 days) and travel restrictions were lifted in March, and schools reopened at the end of April 2020. Similarly, the lockdown ended on 8 April 2020 in Wuhan. It has been widely argued that relaxing inventions increases the risk of resurgence as transmission may intensify, a prediction that has been borne out in southern United States and Europe (4–8). However, despite interventions being relaxed and continuous importation of new infections, a second wave in China has yet to materialize. Key questions remain about how relaxing interventions alters age-specific contact patterns and may, in turn, affect transmission. Quantifying the interaction between interventions and contacts is a key step to understand the post-lockdown SARS-CoV-2 transmission patterns.
This study aims to measure changes in mixing patterns as interventions are gradually relaxed to understand their impact on epidemic spread. To achieve this aim, we collected contact survey data in three different phases of the pandemic (before the pandemic, during the lockdown, and while interventions were being relaxed—post-lockdown phase) in four locations in China (Wuhan, Shanghai, Shenzhen, and Changsha). The post-lockdown phase was set at 1 month after the start of workplace reopening and relaxation of other measures (citywide close community management and mobility restrictions) at a time when there was no local transmission. The rationale for the definition of the post-lockdown period was to capture a time horizon when people were gradually coming out of a full lockdown. We aimed to investigate whether social interactions would increase relatively quickly over that horizon, leading to a putative resurgence of cases. On the basis of the collected data, we investigate changes in age-stratified contact patterns and provide a model-based evaluation of their impact on the SARS-CoV-2 transmission. Moreover, we leverage the calibrated model to project the impact of a hypothetical further increase in the number of contacts on the emergence of a second wave.
RESULTS
Contact surveys
We performed diary-based contact surveys (9–12) in four Chinese cities (Wuhan, Shanghai, Shenzhen, and Changsha) representing different epidemiological situations. Wuhan was the early epicenter of the outbreak. Shanghai is a highly connected international hub and, thus, has been experiencing continuous importations of COVID-19 cases. Shenzhen is a major hub in Guangdong Province, which reported the largest number of COVID-19 cases outside Hubei Province. Changsha is a city of Hunan Province adjacent to Hubei Province with a large number of commuters’ influx to and from Hubei.
The surveys were conducted from 1 to 20 March 2020 in Shanghai, Shenzhen, and Changsha, about 1 month after workplaces started to reopen on 10 February. In Wuhan, the survey was performed from 7 to 15 May 2020, about 1 month after the end of the lockdown (8 April). We collected information on weekday contact behavior for the pre–COVID-19 baseline period, the pandemic period when strict social distancing was in place, and during the post-lockdown survey period, as interventions were relaxed (Materials and Methods). At the time of the contact survey, schools had not reopened except for the final year of senior high school in Wuhan, but travel restrictions and community management had begun to relax (Fig. 1) (section S1).
Fig. 1. Number of COVID-19 reported cases, timing of the surveys, and the main interventions in place over time.
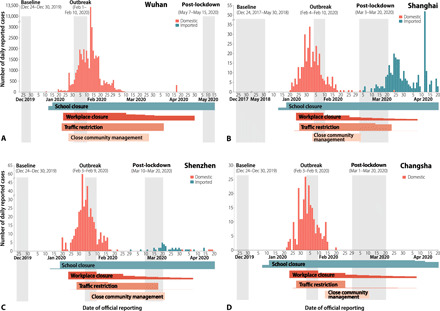
(A) Wuhan. (B) Shanghai. (C) Shenzhen. (D) Changsha. COVID-19 cases by local transmission and international importation are indicated in light red and blue. The contact surveys for Shanghai, Shenzhen, and Changsha were conducted from 1 to 20 March, corresponding to the period of relaxation of interventions, and 7 to 15 May for Wuhan. The contact diaries for the baseline and outbreak periods were derived from retrospective interviews or previous surveys. The horizontal bars at the bottom of each panel represent the intensity over time of the four main performed interventions, where the height of the bar refers to the relative share of population affected by the intervention with the exception of close community management. With relatively small number of cases, the close community management was limited to subcity areas where cases were identified. The detailed timeline of the interventions is reported in table S1. Note that the school and university closure starting in mid-January was the regular winter break before the Lunar New Year holiday. In the absence of the pandemic, schools were set to reopen around mid-February 2020, while universities were scheduled to reopen between 4 February and 1 March 2020. However, because of the pandemic, these closures were extended.
Characteristics of contact patterns
We analyzed a total of 54,324 contacts reported by 9206 study participants (Table 1). In Wuhan, the average daily number of contacts per participant significantly increased from 2.0 during the outbreak period (mean contacts weighted by age structure: 1.9) to 3.3 in the post-lockdown period (mean contacts weighted by age structure: 3.6) (P < 0.001). The increase in contacts was significantly different by sex, age, type of profession, and household size, with the exception of respondents under 20 years (Table 1). A smaller increase was observed in Shanghai, Shenzhen, and Changsha, where the average daily number of contacts increased by 0.1 to 0.4 contacts per day (0.2 to 0.8 for the mean number of contacts weighted by the age structure) starting from about 2.2 contacts during the lockdown period. The observed increase in the number of contacts (especially among adults) is statistically significant for Wuhan, Shanghai, and Shenzhen (Table 1). Participants in the four cities essentially reported the same number of contacts during the lockdown, but on average, individuals in Wuhan reported more contacts than individuals in the other cities in the post-lockdown period, possibly because of the different timing of the contact surveys in the four locations (section S3.2).
Table 1. Number of contacts by respondent characteristics, location, and time period.
Note that reduced denominators indicate missing data. Percentages may not total 100 because of rounding. The 95% confidence interval (CI) on the mean is calculated by bootstrap sampling and are weighted by day type (i.e., weekday or weekend) for diaries during post-lockdown period. *P < 0.05, **P < 0.01, ***P < 0.001. P values are taken from a weighted negative binomial regression, with a single binary variable distinguishing the post-lockdown period from the outbreak period. The weight refers to day type (i.e., weekday and weekend).
| Characteristics | Wuhan, mean (95% CI) | Shanghai, mean (95% CI) | Shenzhen, mean (95% CI) | Changsha, mean (95% CI) | ||||||||
| Baseline | Outbreak |
Post- lockdown |
Baseline | Outbreak |
Post- lockdown |
Baseline | Outbreak |
Post- lockdown |
Baseline | Outbreak |
Post- lockdown |
|
| Total number of contacts (participants) |
9,114 (624) | 1,245 (627) | 2,751 (822) | 17,201 (965) | 1,296 (557) | 2,232 (814) | 5,846 (741) | 1,798 (836) | 2,130 (837) | 7,025 (738) | 1,756 (813) | 1,930 (832) |
| Overall | 14.6 (13, 16.3) |
2 (1.9, 2.1) | 3.3 (3, 3.6)*** | 18.8 (17.5, 20.1) | 2.3 (2, 2.8) | 2.7 (2.5, 3)*** | 7.9 (7.2, 8.6) | 2.2 (2.1, 2.3) | 2.5 (2.4, 2.7)*** | 9.5 (8.6, 10.4) | 2.2 (2.1, 2.3) | 2.3 (2.1, 2.6) |
| Sex | ||||||||||||
| Male | 14.5 (12.2, 16.9) |
1.8 (1.7, 2) | 3 (2.8, 3.2)*** | 19 (17.3, 20.8) | 2.1 (1.9, 2.4) | 2.7 (2.4, 3)*** | 8.6 (7.7, 9.6) | 2.2 (2, 2.4) | 2.5 (2.3, 2.8)** | 9.8 (8.5, 11.1) | 2.3 (2.1, 2.4) | 2.6 (2.2, 3.2)* |
| Female | 14.7 (12.5, 17.1) |
2.1 (2, 2.3) | 3.6 (3.1, 4.1)*** | 18.5 (16.8, 20.2) | 2.6 (2.1, 3.4) | 2.8 (2.4, 3.2) | 7.2 (6.4, 8.1) | 2.1 (2, 2.2) | 2.5 (2.3, 2.8)*** | 9.3 (8.1, 10.7) | 2.1 (1.9, 2.2) | 2 (1.9, 2.2) |
| Age group | ||||||||||||
| 0–6 years | 8.6 (3.3, 17.8) | 2.2 (1.8, 2.8) | 2.7 (2.5, 2.9) | 11.6 (9.1, 14.3) | 1.9 (1.6, 2.1) | 2.5 (2.3, 2.8) | 7.2 (5.2, 9.5) | 2.5 (2.3, 2.8) | 2.5 (2.2, 2.8) | 10.9 (8, 14.4) | 2.7 (2.4, 3) | 2.7 (2.4, 3) |
| 7–19 years | 16.2 (12.4, 19.9) |
2.1 (2, 2.2) | 2.5 (2.3, 2.7) | 27 (23.9, 30.2) | 2.6 (2, 3.4) | 2.2 (2.1, 2.4) | 11.6 (9.6, 13.5) | 2.5 (2.2, 2.8) | 2.3 (2, 2.6) | 16.4 (13.3, 19.6) |
2.2 (2.1, 2.4) | 2.1 (1.9, 2.2) |
| 20–39 years | 15.3 (12.8, 18) |
2.1 (1.9, 2.2) | 4.7 (3.8, 5.7)*** | 22.4 (19.4, 25.2) | 2.2 (2, 2.5) | 3.4 (2.8, 4.2)*** | 8 (7, 9.1) | 1.8 (1.6, 2) | 2.9 (2.4, 3.4)*** | 9.1 (7.4, 11) | 2.2 (1.9, 2.6) | 2.8 (2.1, 3.9) * |
| 40–59 years | 13.8 (11.2, 16.8) |
2 (1.9, 2.1) | 3.7 (3.2, 4.2)*** | 19.9 (17.4, 22.6) | 2.8 (2, 4.2) | 3.2 (2.6, 3.8) | 8.5 (7, 10.4) | 2 (1.8, 2.3) | 2.6 (2.3, 3.1)** | 9.4 (7.7, 11.2) | 2.1 (1.9, 2.3) | 2.4 (2.1, 2.7) |
| ≥60 years | 13.9 (8.1, 21) | 1.4 (1.2, 1.7) | 2.4 (2.2, 2.7)*** | 12.6 (10.8, 14.3) | 1.6 (1.3, 1.9) | 2 (1.8, 2.2)* | 5 (4.3, 5.8) | 2.3 (2.1, 2.5) | 2.3 (2, 2.6) | 5.5 (4.7, 6.4) | 2 (1.8, 2.2) | 1.8 (1.6, 2) |
| Type of profession | ||||||||||||
| Preschool | 8.6 (3.5, 17.2) | 2.2 (1.7, 2.8) | 2.7 (2.5, 2.9) | 10.4 (8, 13.2) | 1.9 (1.7, 2.1) | 2.6 (2.3, 2.9) | 5.2 (3.4, 7.8) | 2.6 (2.2, 2.9) | 2.4 (2.1, 2.8) | 8.3 (5.3, 12) | 2.7 (2.3, 3.1) | 2.7 (2.3, 3.1) |
| Student | 14.6 (11.6, 18) |
2.1 (2, 2.3) | 2.5 (2.3, 2.7) | 26.2 (23.3, 29.3) | 2.5 (2, 3.2) | 2.3 (2.1, 2.5) | 11.8 (10.1, 13.8) |
2.5 (2.3, 2.9) | 2.4 (2.2, 2.7) | 16.5 (14, 19.5) | 2.3 (2.2, 2.5) | 2.2 (2, 2.3) |
| Employed | 15.4 (13.4, 17.6) |
2.1 (1.9, 2.2) | 4.5 (3.9, 5.2)*** | 22.5 (20.4, 24.7) | 2.5 (2.1, 3.3) | 3.6 (3, 4.2)*** | 9.3 (8.3, 10.3) | 2 (1.8, 2.2) | 3 (2.6, 3.4)*** | 10.3 (8.8, 12.1) | 2.2 (2, 2.4) | 2.8 (2.3, 3.6)*** |
| Working age not in the labor force |
14.1 (6, 24.6) | 1.8 (1.3, 2.4) | 2.8 (2.3, 3.3)* | 14.5 (7.3, 24.2) | 1.8 (1.3, 2.3) | 2.3 (1.9, 2.9) | 5.9 (3.6, 9.4) | 1.8 (1.5, 2.1) | 1.8 (1.3, 2.3) | 5.5 (4.1, 7.3) | 2.1 (1.8, 2.4) | 1.9 (1.6, 2.2) |
| Retired | 12.1 (7.7, 17.2) |
1.5 (1.3, 1.7) | 2.4 (2.2, 2.6)*** | 11.8 (10.2, 13.3) | 1.6 (1.4, 1.8) | 2 (1.8, 2.1)* | 4.7 (4.2, 5.4) | 2.2 (2, 2.3) | 2.2 (2, 2.4) | 5.2 (4.5, 6) | 1.9 (1.7, 2.1) | 1.8 (1.6, 2) |
| Household size | ||||||||||||
| 1 | 10.5 (5, 17.6) | 0.6 (0.1, 1.4) | 2.2 (1.1, 3.7)** | 15.2 (10.5, 20.2) | 0.3 (0.2, 0.5) | 0.4 (0.2, 0.8) | 5.5 (4.1, 7.1) | 0.8 (0.6, 1.1) | 1 (0.6, 1.3) | 5.5 (3.8, 7.8) | 1 (0.4, 1.9) | 0.7 (0.3, 1.2) |
| 2 | 12.6 (7.9, 17.8) |
1.1 (0.9, 1.2) | 1.9 (1.6, 2.3)*** | 14.5 (12.5, 16.6) | 1.4 (1.1, 1.8) | 1.4 (1.2, 1.7) | 6.4 (4.8, 8.1) | 1.3 (1.2, 1.4) | 1.9 (1.5, 2.5)*** | 6.6 (5.4, 8) | 1.4 (1.2, 1.6) | 1.4 (1.2, 1.6) |
| 3 | 14.8 (12.5, 17.3) |
1.9 (1.8, 2) | 3.4 (2.9, 3.9)*** | 20.3 (18.5, 22.1) | 2.2 (2.1, 2.4) | 2.7 (2.4, 3.1)*** | 8.8 (7.9, 9.7) | 2.3 (2.1, 2.5) | 2.8 (2.6, 3.1)*** | 11.3 (9.6, 13) | 2.2 (2.1, 2.3) | 2.3 (2.1, 2.4) |
| 4 | 11.9 (9.2, 15.4) |
2.3 (2.2, 2.5) | 3.4 (3.2, 3.6)*** | 20.3 (16.6, 24.7) | 3 (2.8, 3.2) | 4.2 (3.5, 5.1)*** | 8.4 (7.2, 10) | 3.1 (2.9, 3.2) | 3.1 (2.9, 3.3) | 10.8 (8.5, 13.7) | 3 (2.8, 3.1) | 3.7 (2.7, 5.4)* |
| ≥5 | 21.5 (16.2, 27.5) |
3.2 (2.9, 3.5) | 5.7 (4.8, 6.8)*** | 21.4 (18.1, 25.4) | 5.9 (3.9, 9.2) | 5 (4.1, 6.7) | 10.2 (8.3, 12.3) | 4.3 (4.1, 4.5) | 4.3 (4, 4.6) | 11.3 (8.9, 14.2) | 3.9 (3.7, 4.1) | 4.2 (3.8, 4.6) |
In the four cities, the vast majority of contacts occurred at home in both periods, but workplace contacts increased in the post-lockdown period (sections S3.4 and S3.5). Moreover, a statistically significant increase in the number of physical (skin-to-skin) contacts was also observed in Wuhan only, but the increase was relatively small—from 1.2 to 1.4 physical contacts (section S3.3). Overall, the number of contacts increased over time from the outbreak period to the post-lockdown period (P < 0.001) (section S3.6).
When we consider the pre-pandemic (baseline) period, the typical features of age-mixing patterns (10, 11) emerge in all locations (Fig. 2, A to D). These features can be illustrated in the form of age-stratified contact matrices (provided as ready-to-use tables in section S3.7), where each cell represents the mean number of contacts that an individual of a certain age group has with other individuals of different ages. The bottom left corner of the matrix, corresponding to contacts between school-age children, is where the largest number of contacts is recorded. The contribution of contacts in the workplace is visible in the central part of the matrix, while the three diagonals (from bottom left to top right) represent contacts between household members.
Fig. 2. Contact matrices by age.
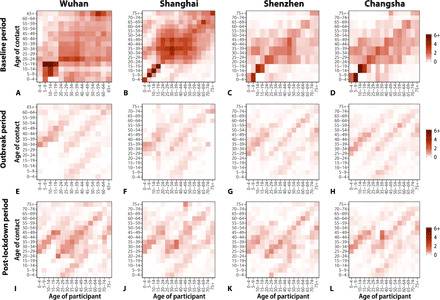
(A) Baseline period contact matrix for Wuhan (regular weekday only). Each cell of the matrix represents the mean number of contacts that an individual in a given age group has with other individuals, stratified by age groups. The color intensity represents the numbers of contacts. To construct the matrix, we performed bootstrap sampling with replacement of survey participants weighted by the age distribution of the actual population of Wuhan. Every cell of the matrix represents an average over 100 bootstrapped realizations. (B) Same as (A), but the contact matrix weighted by weekday and weekends for Shanghai. (C and D) Same as (A), but for Shenzhen and Changsha. (E to H) Same as (A), but for the outbreak contact matrices for Wuhan, Shanghai, Shenzhen, and Changsha. (I to L) Same as (A), but for the post-lockdown contact matrices weighted by weekday and weekends for Wuhan, Shanghai, Shenzhen, and Changsha.
During the COVID-19 outbreak period, when strict social distancing policies were in place, most of the abovementioned features disappear, essentially leaving the sole contribution of household mixing (Fig. 2, E to H). In particular, assortative contacts between school-age individuals fully vanish. Overall, contacts during the outbreak mostly occurred within household members (more than 90% in Shenzhen, Changsha, and Wuhan; 79% in Shanghai). If we compare the post-lockdown period with the outbreak period, more contacts were reinstated in the workplace and in community settings. Therefore, the fraction of contacts at home decreased to 63.0% in Wuhan, 72.5% in Shanghai, 70.2% in Shenzhen, and 78.8% in Changsha. Nevertheless, the three diagonals (from bottom left to top right) representing contacts between household members were still dominant. Note that while strict social distancing measures gradually relaxed in these four locations, a considerable share of workers had not yet resumed work or continued to work from home at the time of the survey (section S3.5).
Modeling the impact of relaxing interventions on SARS-CoV-2 transmission
We used the next-generation matrix approach to quantify changes in R0 during the post-lockdown period, as interventions were relaxed. In the early phases of COVID-19 spread in Wuhan, before control measures were put in place, R0 was estimated to range from 2.0 to 3.5 (13–19). In this study, we extended this range from 1 to 4 for the baseline period (i.e., before interventions). We found that the considerable changes of mixing patterns observed in Shenzhen and Changsha during the social distancing period led to a drastic decrease in R0 (Fig. 3). The reproductive number drops well below the epidemic threshold for all four locations.
Fig. 3. Effect of relaxing interventions on epidemic spread (assuming equal infectiousness by age).
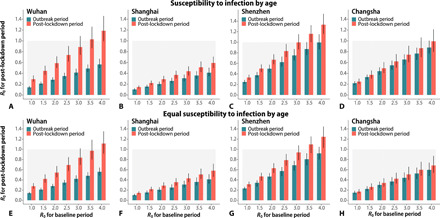
(A) Estimated R0 during the outbreak and post-lockdown periods [mean and 95% confidence interval (CI)] as a function of baseline R0 (i.e., that derived by using the contact matrix estimated from the baseline period). The distribution of the transmission rate is estimated through the next-generation matrix approach by using 100 bootstrapped contact matrices for the baseline period to obtain the desired R0 values. We then use the estimated distribution of the transmission rate and the bootstrapped outbreak and post-lockdown contact matrices to estimate R0 for the outbreak period and the post-lockdown period, respectively. The 95% CIs account for uncertainty in the distribution of the transmission rate, mixing patterns, and susceptibility to infection by age. (B to D) Same as (A), but for Shanghai, Shenzhen, and Changsha. The figure includes both the scenario accounting for susceptibility to infection by age and the scenario where we assume that all individuals are equally susceptible to infection. (A) to (D) refer to the first scenario, and (E) to (H) refer to the second scenario.
When we considered contacts in the post-lockdown period, while keeping the same baseline disease transmissibility as in the preintervention period at an average value of R0 = 2.5, the increase in the number of contacts was not high enough to bring R0 above 1 in any location. The reproductive number exceeded the epidemic threshold in Wuhan (Fig. 3A) and Shenzhen (Fig. 3C) for baseline R0 above 3.0, and in Changsha (Fig. 3D) for baseline R0 above 3.5. The reproductive number in Shanghai did not reach the threshold even for baseline R0 = 4 (Fig. 3B). These findings are robust to assumptions about age differences in susceptibility to infection in Wuhan, Shanghai, and Shenzhen (Fig. 3, E to G). Considering age differences in susceptibility to infection has a marked effect in predicted dynamics in Changsha, where transmission can be interrupted for baseline R0 at least up to four (Fig. 3H). We performed sensitivity analyses regarding age differences in infectiousness; an average individual aged 0 to 14 years was assumed to be twice less infectious than one aged above 14 years old. The results are consistent with those reported here (section S6.1). We also performed sensitivity analyses regarding possible compliance biases of self-reported contacts during the post-lockdown period. In this case, by assuming baseline R0 = 2.5 and by making the extreme assumption that only half of the actual nonhousehold contacts were reported by study participants, the reproduction number for post-lockdown period would still be below the threshold or slightly above it (section S6.2).
Impact of a possible return to pre-pandemic mixing patterns in schools, workplaces, and the community
We performed scenario analyses for Shanghai where we assume that contacts at school, in the workplace, and the community return to the levels reported during the pre-pandemic period. In this analysis, we set R0 = 2.5 to be in line with R0 measured in Wuhan before the start of the interventions (16) and age-specific susceptibility to infection as estimated in our previous study (9).
By assuming no contacts at school, we estimate that, in the absence of contact tracing and other control measures, 55% of workplace and 65% of community mixing could be resumed while keeping R0 below the epidemic threshold. In particular, a reduction of 80% of effective contacts in the community (corresponding to 1.2 contacts per day) would allow the work contacts to be resumed at 50% (Fig. 4A). Opening of senior high schools, even when considering as little as 10% of workplace and 10% of community contacts, could increase R0 above 1 (Fig. 4B). Broader school opening has a higher effect on R0 (Fig. 4C).
Fig. 4. Estimated R0 for Shanghai under different assumptions on the number of contacts in workplaces, community, and schools.
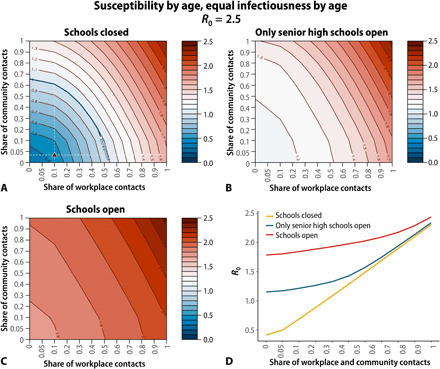
(A) Heatmap of the estimated mean value of R0 for a different combination of number of contacts in the workplaces and community under the assumption that all schools are closed. Share equal to 1 corresponds to the pre-pandemic contact pattern. The triangle corresponds to the measured share of contacts in the workplace and the community during the post-lockdown period. Baseline period R0 was set to 2.5, and we considered age-specific susceptibility to infection as in (9), and no differences in infectiousness by age. R0 values are estimated through the next-generation matrix approach. (B) Same as (A), but assuming that contacts in senior high schools are as in the pre-pandemic period. (C) Same as (A), but assuming that contacts in all schools (corresponding to the entire student population except for college students) are as in the pre-pandemic period. (D) Estimated mean value of R0 for different shares of workplace and community contacts under different levels of school closure.
It is important to highlight that the effect of school closure depends nonlinearly on the share of other activities being resumed (Fig. 4D). In particular, if we compare R0 in an extreme scenario when nearly all workplace and community activities are halted (i.e., only 5% workplace and community contacts included, which is about the same level observed during the lockdown period—about 4%), we can see that school closure corresponds to a decrease of R0 from 1.78 to 0.41. On the contrary, in a scenario where workplace and community contacts return to their pre-pandemic level (i.e., 100%), school closure corresponds to a decrease of R0 of about 0.13. In other words, social contacts in schools only truly matter if other social mixing opportunities are hindered. In this context of greatly reduced contact patterns at work and in the community, school closure becomes determinant in controlling disease spread. If contacts in other social settings are moderate or back to normal, then school closure is less relevant as the infection can spread through other chains of transmission. This effect is nonlinear and is captured by the change of the eigenvalues of the next-generation matrix.
When we consider relaxing interventions simultaneously (e.g., school reopening, workplace resumption, and resuming community activities), returning up to 34% of the pre-pandemic level of nonhousehold contacts (corresponding to a mean of 7.8 contacts per day) can lead R0 above the threshold in Shanghai, with slightly lower proportions (26 to 30%, corresponding to 3.4 to 5.5 contacts per day) in Shenzhen, Changsha, and Wuhan (section S9).
DISCUSSION
We have provided measures of the changes in mixing patterns linked to gradual relaxation of interventions in the Chinese cities of Wuhan, Shanghai, Shenzhen, and Changsha and their impact on the spread of SARS-CoV-2. We find that although the number of contacts has increased in the post-lockdown period in China, social behavior has only partially and slowly changed and mixing patterns have not returned to normal, including among adults. We estimate that the increase in mixing patterns 1 month after the Wuhan lockdown was lifted and after work resumed in the other three cities was not enough to sustain local transmission. The mixing patterns measured in this study were far from the pre-pandemic ones. We also estimate that the importance of school closure/reopening on SARS-CoV-2 control increases in a nonlinear fashion as contacts in the other settings decrease. In particular, our findings support that closing schools was essential to keep the epidemic under control during the lockdown.
Several studies have shown a very marked decrease in the number of contacts between the pre-pandemic and lockdown periods (9, 20–24), in agreement with what we found here, which parallels a decrease in mobility patterns (9, 25). However, our study shows that the post-lockdown increase in mobility patterns is not a good proxy of the daily number of in contacts in the four study locations (section S4). The intracity mobility in the analyzed cities has also been rebounding to pre-pandemic levels, while contacts in the same period are still very close to the ones estimated during the lockdown period. Several studies for different countries have shown a rebound in mobility after the lockdown (26–29). However, the much slower increase in the number of daily contacts that we estimated here could be location-specific. A similar pattern has been found in the United States where mobility measured by mobile phone data has rebounded to pre-pandemic levels, but the number of contacts quantified by co-proximity is still at 50% or less of pre-pandemic levels (30). Whether these results can be generalized to other countries remains unclear.
To estimate how changes in contact patterns affect SARS-CoV-2 spread, we performed a model-based analysis. In particular, we estimated that the level of contacts recorded during the post-lockdown period in spring 2020 is sufficient to keep the reproduction number below the epidemic threshold. On the contrary, in a purely theoretical scenario where all schools were open but parents could agree to stay at home, social distancing among adults would not be sufficient to prevent a COVID-19 outbreak. This highlights the need for considering additional case- and population-based interventions such as those in place in China since the end of the lockdown (e.g., 14-day quarantine in designated places for medical observation and testing for imported cases and use of face masks). However, it is important to stress that the population may spontaneously adjust its behavior, including avoidance of gatherings and adherence to hygiene measures, to limit their risk of SARS-CoV-2 infection while the pandemic is still spreading worldwide. These behavioral adaptations may partially explain why the number of contacts measured in this study in the post-lockdown period is still remarkably lower than before the pandemic.
This study is prone to the limitations pertaining to social contact surveys. The definition of contact relevant for SARS-CoV-2 transmission is still unclear. We used the classic definition of having a conversation or direct physical contact (9), which does not include contacts with surfaces (fomite transmission) that may have been possibly contaminated by infectious individuals. However, contacts with surfaces are hard to quantify, irrespective of the adopted methodology, and their contribution on SARS-CoV-2 transmission has yet to be clarified. The contact survey presented in this study is based on self-reported contacts. It can thus be affected by various biases, including recall bias and self-reporting bias. In particular, reported contacts for the baseline period in Wuhan, Shenzhen, and Changsha may be prone to recall bias as contacts were recorded retrospectively with delays up to 1 month in Wuhan and up to 2 to 3 months in Shenzhen and Changsha (table S2). This may explain why we observed a larger number of contacts during that period in Shanghai with respect to the other three locations and less marked typical features of contact matrices by age (such as the presence of three main diagonals representing contacts among household members, a bottom-left corner showing contacts among students, and a central area showing contacts between workers) in these three locations with respect to Shanghai. Nonetheless, it is important to stress that the mean number of daily contacts estimated for the four locations during the pre-pandemic period is comparable to that obtained in other countries (10, 31, 32), ranging from 4.5 contacts per day in Japan (32) to 27 contacts per day in the United Kingdom (33). Moreover, the age-stratified contact matrices presented in those studies share the same features as those presented here. Another possible bias is that survey participants may have felt pressure to minimize reported contacts that occurred during the post-lockdown period, given that social distancing policy has not been totally relaxed, even if the anonymity and confidentiality of the survey were emphasized. However, results are robust to inflating reported contacts outside of the home severalfold, suggesting that possible compliance and social acceptability biases linked to the post-lockdown period do not affect our main findings (section S6.2).
Our modeling analysis contains several approximations. The model does not consider explicitly symptomatic and asymptomatic individuals and possible differences in their infectiousness and/or mixing patterns. Explicit modeling of symptomatic/asymptomatic individuals would require assumptions on contact patterns for symptomatic/asymptomatic individuals, as this information was not collected in our surveys. In particular, it is possible that the difference in mixing patterns observed in the pre-pandemic, outbreak, and post-lockdown phase would be less marked for symptomatic individuals (especially for severe ones). Therefore, our estimates of SARS-CoV-2 transmission in the post-lockdown phase may be slightly underestimated. On the other hand, the model assumes a homogeneous network of contacts (i.e., it does not account for the typical clustering of human contacts), and thus, our results can be considered an upper bound of SARS-CoV-2 transmissibility. The adopted transmission scheme is simple and does not explicitly account for different levels of the severity pyramid, such as hospitalizations or deaths. Estimates of incidence and disease burden are beyond the scope of the paper; our model was designed to provide a general view of the effect of age-mixing patterns on SARS-CoV-2 transmission rather than direct projections of the pandemic on the healthcare system.
We would like to stress that here we do not necessarily endorse relaxing or reinstating social distancing policies in the context of COVID-19, but rather merely describe their impact on SARS-CoV-2 transmission based on the data collected in four Chinese cities. Our contact surveys were conducted about 1 month after social distancing measures started to be relaxed in China and cover a period of 1 to 3 weeks in each study location. Whether these findings can be generalized to other locations or how and to what extent mixing patterns have evolved over time warrants further research. It remains unclear how long people would be able to sustain a reduced level of social restrictions, as observed right after the lockdown. Additional and more recent contact surveys should be conducted in the pandemic and post-pandemic period in a number of countries. Understanding compliance to interventions and long-term changes in contact patterns because of COVID-19 will be a rich area for future research.
From 1 June to 12 December 2020, China has experienced four local outbreaks with more than 50 cases: An outbreak of 335 cases was reported in Beijing, one of 826 cases in Urumqi in Xinjiang Uygur Autonomous Region, one of 92 cases in Dalian in Liaoning Province, and one of 78 cases in Kashgar Prefecture in Xinjiang Uygur Autonomous Region (34). This supports our modeling results indicating that the reproduction number may easily cross the epidemic threshold when schools are open. However, none of these outbreaks escalated to a nationwide level as prompt and strict interventions were put in place in reaction to these flare-ups. Moving forward, to prevent the resurgence of the epidemic, it will be particularly important to strengthen sanitization activities (e.g., washing hands and disinfection) and proactive social distancing measures (e.g., increased distance between individuals while in contact or use of a face mask), along with large-scale testing and contact tracing (35–38). This is particularly important when schools are open (39) and during festivities, when an increase of intercity mobility, inbound travelers, and more social mixing between people and households can be anticipated. Researches should continue to focus on refining age-specific estimates of susceptibility to infection, infectiousness, and risk of severe disease, in conjunction with changes in mixing patterns, as these are instrumental to evaluate the impact of control strategies on SARS-CoV-2 transmission.
MATERIALS AND METHODS
Design of the contact survey
To estimate changes in age-mixing patterns associated with relaxation of interventions against SARS-CoV-2, we conducted contact surveys in four cities. The design of the survey was similar to that of our previous work (9–11). Participants in Shenzhen and Changsha were asked to complete a questionnaire describing their contact behavior (9, 12) on three different days: (i) a regular weekday between 24 and 30 December 2019, before the COVID-19 outbreak was officially declared (baseline period); (ii) a day between 3 and 9 February 2020 when the COVID-19 epidemic peaked across China and stringent interventions were in place (outbreak period); and (iii) the day before the telephone interview took place, corresponding to a period when interventions were being relaxed across China (post-lockdown period). A contact was defined as either a two-way conversation involving three or more words in the physical presence of another person or a direct physical contact (e.g., a handshake). Participants in Wuhan and Shanghai were asked to complete the same questionnaire used for Shenzhen and Changsha, but to report only the contacts during the post-lockdown period. For the baseline and outbreak period in Wuhan and Shanghai, we relied on a survey conducted in 2017–2018 and another survey conducted in 2020 during the pandemic that followed the same design (9, 10). A more detailed description of the methodology is given in the Supplementary Materials (sections S1 and S2).
Estimation of contact patterns
The number of daily contacts (including physical and conversational contacts) was compared between the post-lockdown period and the outbreak period for each location using a weighted negative binomial regression, where the weight refers to the day type of contact diary (i.e., weekdays or weekends) (9). The same comparison was performed among four cities for the outbreak period and the post-lockdown period, respectively.
We defined 16 age groups (0 to 4 years, 5 to 9 years, 10 to 14 years, 15 to 19 years, 20 to 24 years, 25 to 29 years, 30 to 34 years, 35 to 39 years, 40 to 44 years, 45 to 49 years, 50 to 54 years, 55 to 59 years, 60 to 64 years, 65 to 69 years, 70 to 74 years, and 75 years and over) to build age-specific contact matrices. Contact matrices representing mixing patterns during a baseline pre-pandemic day (referred to as “baseline period contact matrix”), during the COVID-19 outbreak (referred to as “outbreak contact matrix”), and during the period of relaxation of interventions (referred to as “post-lockdown contact matrix”) were estimated for the four cities. Because of the sample size, for baseline and outbreak contact matrices in Wuhan, we used 14 age groups (last age group being 65+ years). To account for the uncertainty of the contact matrices and sample representativeness of contact matrix, we performed bootstrap sampling with replacement of survey participants weighted by the age distribution of the actual population in each location. For the post-lockdown period, we adjusted for weekdays and weekends (weight of 2/7 for diaries referring to Saturdays/Sundays, weight of 5/7 for diaries referring to Monday to Friday) (9).
SARS-CoV-2 natural history and transmission
To explore how our empirical data can inform how to relax COVID-19 control strategies, we performed a modeling exercise. A key parameter regulating the dynamics of an epidemic is the basic reproduction number (R0), which corresponds to the average number of secondary cases generated by an index case in a fully susceptible population. We estimated the impact of relaxing interventions on R0, relying on the empirically estimated mixing patterns. We also considered age-specific estimates of susceptibility to infection presented in (9) and no differential infectiousness by age (40). We also consider scenarios where all age groups are equally susceptible by age and where children are twice less infectious than adults (section S6.1). The mean time interval between two consecutive generations of cases was set to be 5.1 days, aligning with the mean of the serial interval reported by Zhang et al. (41). Last, we used the next-generation matrix approach to quantify estimate R0 (section S5) (42).
Simulation of hypothetical scenarios with alternative mixing patterns
We project how increasing school, workplace, and community contacts can affect COVID-19 spread in Shanghai. We considered several different scenarios, on the basis of the baseline contact matrix and gradual implementation of interventions by social setting (i.e., household, school, workplace, and community). A similar analysis was performed for Shenzhen and Changsha (section S8). No simulations were performed for Wuhan, as for this location we did not collect data by social setting for the baseline period (9). We finally used the same next-generation matrix approach to project what degree of return to pre-pandemic contact could lead R0 above the epidemic threshold if the contacts outside the household are resumed simultaneously (section S9).
Acknowledgments
We would like to acknowledge Y. Chen and H. Gong from the Fudan University for help on the data cleaning and N. Samay for assistance in preparing the figures. Funding: H.Y. acknowledges financial support from the National Science Fund for Distinguished Young Scholars (no. 81525023), Key Emergency Project of Shanghai Science and Technology Committee (no. 20411950100), and National Science and Technology Major Project of China (nos. 2018ZX10201001-010, 2018ZX10713001-007, and 2017ZX10103009-005). J.Z. acknowledges financial support from China Postdoctoral Science Foundation (no. 2020T130014ZX). M.L., A.V., and M.A. acknowledge financial support from Cooperative Agreement no. NU38OT000297 from the Centers for Disease Control and Prevention (CDC) and the Council of State and Territorial Epidemiologists (CSTE). The study does not necessarily represent the views of CDC and CSTE. Ethics statement: Ethics approval was obtained from the institutional review board of the School of Public Health, Fudan University (IRB no. 2020-01-0801-S2). Verbal informed consent was obtained from all subjects (or from a parent/guardian if participant was below 18 years of age). Author contributions: H.Y. and M.A. designed the experiments. J.Z., Y.L., W.Z., and H.S. collected and cleaned the data. J.Z., M.L., Y.L., W.Z., and H.S. analyzed the data. J.Z., M.L., A.V., C.V., M.A., and H.Y. interpreted the results. J.Z., M.L., M.A., and H.Y. wrote the manuscript. A.V. and C.V. edited the manuscript. Competing interests: A.V. reports a grant from Metabiota Inc. M.A. has received research funding from Seqirus. H.Y. has received research funding from Sanofi Pasteur, GlaxoSmithKline, Yichang HEC Changjiang Pharmaceutical Company, and Shanghai Roche Pharmaceutical Company. None of this funding is related to COVID-19. The authors declare no other competing interests. Data and materials availability: All data needed to evaluate the conclusions in the paper are present in the paper and/or the Supplementary Materials. All information needed to reproduce the results of this study are available in the Supplementary Materials. Data and code are available on Zenodo at DOI: 10.5281/zenodo.3754582 and DOI: 10.5281/zenodo.4312245.
SUPPLEMENTARY MATERIALS
Supplementary material for this article is available at http://advances.sciencemag.org/cgi/content/full/7/19/eabe2584/DC1
REFERENCES AND NOTES
- 1.World Health Organization, WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 (2020); www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [accessed 9 July 2020].
- 2.National Health Commission of the People’s Republic of China, Update on COVID-19 as of 24:00 on July 30, 2020 (2020); www.nhc.gov.cn/xcs/yqtb/202007/f81f2c2e757240a88bbc0a265f4249de.shtml [accessed 31 July 2020].
- 3.“Workplaces resume operations from February 10,” Tencent News, 2020; https://new.qq.com/omn/20200131/20200131A0L4GF00.html [accessed 9 July 2020].
- 4.“COVID-19 resurgence threatens South Korea’s success story,” The Diplomat, 2020; https://thediplomat.com/2020/06/covid-19-resurgence-threatens-south-koreas-success-story/ [accessed 12 June 2020].
- 5.University of Minnesota, US posts largest single-day jump in new COVID-19 cases (2020); www.cidrap.umn.edu/news-perspective/2020/07/us-posts-largest-single-day-jump-new-covid-19-cases [accessed 9 July 2020].
- 6.University of Minnesota, US daily COVID-19 cases near 50,000 as 19 states pause reopening (2020); www.cidrap.umn.edu/news-perspective/2020/07/us-daily-covid-19-cases-near-50000-19-states-pause-reopening [accessed 9 July 2020].
- 7. News at a glance. Science 368, 1164–1165 (2020). [DOI] [PubMed] [Google Scholar]
- 8.Hao X., Cheng S., Wu D., Wu T., Lin X., Wang C., Reconstruction of the full transmission dynamics of COVID-19 in Wuhan. Nature 584, 420–424 (2020). [DOI] [PubMed] [Google Scholar]
- 9.Zhang J., Litvinova M., Liang Y., Wang Y., Wang W., Zhao S., Wu Q., Merler S., Viboud C., Vespignani A., Ajelli M., Yu H., Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 368, 1481–1486 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang J., Klepac P., Read J. M., Rosello A., Wang X., Lai S., Li M., Song Y., Wei Q., Jiang H., Yang J., Lynn H., Flasche S., Jit M., Yu H., Patterns of human social contact and contact with animals in Shanghai, China. Sci. Rep. 9, 15141 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Litvinova M., Liu Q.-H., Kulikov E. S., Ajelli M., Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc. Natl. Acad. Sci. U.S.A. 116, 13174–13181 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mossong J., Hens N., Jit M., Beutels P., Auranen K., Mikolajczyk R., Massari M., Salmaso S., Tomba G. S., Wallinga J., Heijne J., Sadkowska-Todys M., Rosinska M., Edmunds W. J., Social contacts and mixing patterns relevant to the spread of infectious diseases. PLOS Med. 5, e74 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu J. T., Leung K., Leung G. M., Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet 395, 689–697 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Read J. M., Bridgen J. R. E., Cummings D. A. T., Ho A., Jewell C. P., Novel coronavirus 2019-nCoV: Early estimation of epidemiological parameters and epidemic predictions. medRxiv 2020.01.23.20018549 , (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K. S. M., Lau E. H. Y., Wong J. Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Liu M., Tu W., Chen C., Jin L., Yang R., Wang Q., Zhou S., Wang R., Liu H., Luo Y., Liu Y., Shao G., Li H., Tao Z., Yang Y., Deng Z., Liu B., Ma Z., Zhang Y., Shi G., Lam T. T. Y., Wu J. T., Gao G. F., Cowling B. J., Yang B., Leung G. M., Feng Z., Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 382, 1199–1207 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abbott S., Hellewell J., Munday J.; CMMID nCoV Working Group, Funk S., The transmissibility of novel Coronavirus in the early stages of the 2019-20 outbreak in Wuhan: Exploring initial point-source exposure sizes and durations using scenario analysis. Wellcome Open Res. 5, 17 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chinazzi M., Davis J. T., Ajelli M., Gioannini C., Litvinova M., Merler S., Pastore y Piontti A., Mu K., Rossi L., Sun K., Viboud C., Xiong X., Yu H., Halloran M. E., Longini I. M. Jr., Vespignani A., The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 368, 395–400 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.N. Imai, A. Cori, I. Dorigatti, M. Baguelin, C. A. Donnelly, S. Riley, N. M. Ferguson, Transmissibility of 2019-nCoV (Imperial College London, 2020).
- 19.World Health Organization, Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) (2020); www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf [accessed 11 March 2020].
- 20.Del Fava E., Cimentada J., Perrotta D., Grow A., Rampazzo F., Gil-Clavel S., Zagheni E., The differential impact of physical distancing strategies on social contacts relevant for the spread of COVID-19: Evidence from a multi-country survey. medRxiv 2020.05.15.20102657, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perrotta D., Grow A., Rampazzo F., Cimentada J., Fava E. D., Gil-Clavel S., Zagheni E., Behaviors and attitudes in response to the COVID-19 pandemic: Insights from a cross-national Facebook survey. medRxiv 2020.05.09.20096388, (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jarvis C. I., Van Zandvoort K., Gimma A., Prem K.; CMMID COVID-19 working group, Klepac P., Rubin G. J., Edmunds W. J., Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 18, 124 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quaife M., van Zandvoort K., Gimma A., Shah K., Creesh N. M., Prem K., Barasa E., Mwanga D., Kangwana B., Pinchoff J.; CMMID COVID-19 Working Group, Edmunds W. J., Jarvis C. I., Austrian K., The impact of COVID-19 control measures on social contacts and transmission in Kenyan informal settlements. BMC Med. 18, 316 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feehan D., Mahmud A., Quantifying interpersonal contact in the United States during the spread of COVID-19: First results from the Berkeley Interpersonal Contact Study. medRxiv 2020.04.13.20064014, (2020). [Google Scholar]
- 25.Lai S., Ruktanonchai N. W., Zhou L., Prosper O., Luo W., Floyd J. R., Wesolowski A., Santillana M., Zhang C., Du X., Yu H., Tatem A. J., Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 585, 410–413 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Badr H. S., Du H., Marshall M., Dong E., Squire M. M., Gardner L. M., Association between mobility patterns and COVID-19 transmission in the USA: A mathematical modelling study. Lancet Infect. Dis. 20, 1247–1254 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.P. Cintia, D. Fadda, F. Giannotti, L. Pappalardo, G. Rossetti, D. Pedreschi, S. Rinzivillo, P. Bonato, F. Fabbri, F. Penone, M. Savarese, D. Checchi, F. Chiaromonte, P. Vineis, G. Guzzetta, F. Riccardo, V. Marziano, P. Poletti, F. Trentini, A. Bella, X. Andrianou, M. Del Manso, M. Fabiani, S. Bellino, S. Boros, A. Mateo Urdiales, M. Fenicia Vescio, S. Brusaferro, G. Rezza, P. Pezzotti, M. Ajelli, S. Merler, The relationship between human mobility and viral transmissibility during the COVID-19 epidemics in Italy. arXiv:2006.03141 [cs.SI] (2020).
- 28.B. Klein, T. LaRock, S. McCabe, L. Torres, F. Privitera, B. Lake, M. U. G. Kraemer, J. S. Brownstein, D. Lazer, T. Eliassi-Rad, S. V. Scarpino, M. Chinazzi, A. Vespignani, Assessing changes in commuting and individual mobility in major metropolitan areas in the United States during the COVID-19 outbreak. MOBS Lab Technical Report (2020); www.networkscienceinstitute.org/publications/assessing-changes-in-commuting-and-individual-mobility-in-major-metropolitan-areas-in-the-united-states-during-the-covid-19-outbreak [accessed 10 December 2020].
- 29.Miller A. C., Foti N. J., Lewnard J. A., Jewell N. P., Guestrin C., Fox E. B., Mobility trends provide a leading indicator of changes in SARS-CoV-2 transmission. medRxiv 2020.05.07.20094441, (2020). [Google Scholar]
- 30.Mobility, commuting, and contact patterns across the United States during the COVID-19 outbreak (2020); https://covid19.gleamproject.org/mobility.
- 31.Hoang T., Coletti P., Melegaro A., Wallinga J., Grijalva C. G., Edmunds J. W., Beutels P., Hens N., A systematic review of social contact surveys to inform transmission models of close-contact infections. Epidemiology 30, 723–736 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Munasinghe L., Asai Y., Nishiura H., Quantifying heterogeneous contact patterns in Japan: A social contact survey. Theor. Biol. Med. Model. 16, 6 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Danon L., House T. A., Read J. M., Keeling M. J., Social encounter networks: Collective properties and disease transmission. J. R. Soc. Interface 9, 2826–2833 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chinese Center for Disease Control and Prevention, Update on COVID-19 in China (2020); http://2019ncov.chinacdc.cn/2019-nCoV/ [accessed 10 December 2020].
- 35.Prem K., Liu Y., Russell T. W., Kucharski A. J., Eggo R. M., Davies N.; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group, Jit M., Klepac P., The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. Lancet Public Health 5, e261–e270 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heymann D. L., Shindo N.; WHO Scientific and Technical Advisory Group for Infectious Hazards , COVID-19: What is next for public health? Lancet 395, 542–545 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Riley S., Fraser C., Donnelly C. A., Ghani A. C., Abu-Raddad L. J., Hedley A. J., Leung G. M., Ho L.-M., Lam T.-H., Thach T. Q., Chau P., Chan K.-P., Lo S.-V., Leung P.-Y., Tsang T., Ho W., Lee K.-H., Lau E. M. C., Ferguson N. M., Anderson R. M., Transmission dynamics of the etiological agent of SARS in Hong Kong: Impact of public health interventions. Science 300, 1961–1966 (2003). [DOI] [PubMed] [Google Scholar]
- 38.Brooks J. T., Butler J. C., Redfield R. R., Universal masking to prevent SARS-CoV-2 transmission—The time is now. JAMA 324, 635–637 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levinson M., Cevik M., Lipsitch M., Reopening primary schools during the pandemic. N. Engl. J. Med. 383, 981–985 (2020). [DOI] [PubMed] [Google Scholar]
- 40.Hu S., Wang W., Wang Y., Litvinova M., Luo K., Ren L., Sun Q., Chen X., Zeng G., Li J., Liang L., Deng Z., Zheng W., Li M., Yang H., Guo J., Wang K., Chen X., Liu Z., Yan H., Shi H., Chen Z., Zhou Y., Sun K., Vespignani A., Viboud C., Gao L., Ajelli M., Yu H., Infectivity, susceptibility, and risk factors associated with SARS-CoV-2 transmission under intensive contact tracing in Hunan, China. Nat. Commun. 12, 1533 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang J., Litvinova M., Wang W., Wang Y., Deng X., Chen X., Li M., Zheng W., Yi L., Chen X., Wu Q., Liang Y., Wang X., Yang J., Sun K., Longini I. M. Jr., Halloran M. E., Wu P., Cowling B. J., Merler S., Viboud C., Vespignani A., Ajelli M., Yu H., Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: A descriptive and modelling study. Lancet Infect. Dis. 20, 793–802 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Diekmann O., Heesterbeek J. A. P., Metz J. A. J., On the definition and the computation of the basic reproduction ratio R0 in models for infectious diseases in heterogeneous populations. J. Math. Biol. 28, 365–382 (1990). [DOI] [PubMed] [Google Scholar]
- 43.Wang L., Cowling B. J., Wu P., Yu J., Li F., Zeng L., Wu J. T., Li Z., Leung G. M., Yu H., Human exposure to live poultry and psychological and behavioral responses to influenza A(H7N9), China. Emerg. Infect. Dis. 20, 1296–1305 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.H. Liu, Tabulation on the Population Census of Hubei Province (China Statistics Press, 2012). [Google Scholar]
- 45.Shanghai Municipal Bureau of Statistics, Sample Survey of 1% Population in Shanghai City (China Statistics Press, 2017). [Google Scholar]
- 46.Guangdong Provincial Bureau of Statistics, Sample Survey of 1% Population in Guangdong Province (China Statistics Press, 2017). [Google Scholar]
- 47.Hunan Provincial Bureau of Statistics, Sample Survey of 1% Population in Hunan Province (China Statistics Press, 2017). [Google Scholar]
- 48.M. J. Keeling, P. Rohani, in Modeling Infectious Diseases in Humans and Animals (Princeton Univ. Press, 2011). [Google Scholar]
- 49.Lai S., Zhou H., Xiong W., Yu H., Huang Z., Yu J., Yin W., Wang L., Chen Q., Li Y., Mu D., Zeng L., Ren X., Geng M., Zhang Z., Cui B., Li T., Wang D., Sun Q., Wardrop N. A., Tatem A. J., Wei S., Changing epidemiology of human brucellosis, China, 1955–2014. Emerg. Infect. Dis. 23, 184–194 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leung K., Wu J. T., Liu D., Leung G. M., First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: A modelling impact assessment. Lancet 395, 1382–1393 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.R. Anderson, R. May, Infectious Diseases of Humans: Dynamics and Control (Oxford Univ. Press, 1991). [Google Scholar]
- 52.National Bureau of Statistics, China census data (2020); www.stats.gov.cn/ [accessed 1 March 2020].
- 53.Liu Q.-H., Ajelli M., Aleta A., Merler S., Moreno Y., Vespignani A., Measurability of the epidemic reproduction number in data-driven contact networks. Proc. Natl. Acad. Sci. U.S.A. 115, 12680–12685 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material for this article is available at http://advances.sciencemag.org/cgi/content/full/7/19/eabe2584/DC1


