Tularemia, a disease caused by the environmental bacterium Francisella tularensis, is characterized by acute febrile illness. F. tularensis is highly infectious: as few as 10 organisms can cause human disease. Tularemia is not known to be spread from person to person.
KEYWORDS: Francisella tularensis, tularemia, aquatic environment, biofilms, long-term persistence
ABSTRACT
Francisella tularensis, the causative agent of the zoonotic disease tularemia, can cause seasonal outbreaks of acute febrile illness in humans with disease peaks in late summer to autumn. Interestingly, its mechanisms for environmental persistence between outbreaks are poorly understood. One hypothesis is that F. tularensis forms biofilms in aquatic environments. We utilized two fully virulent wild-type strains: FSC200 (Francisella tularensis subsp. holarctica) and Schu S4 (Francisella tularensis subsp. tularensis) and three control strains, the attenuated live vaccine strain (LVS; F. tularensis subsp. holarctica), a Schu S4 ΔwbtI mutant that is documented to form biofilms, and the low-virulence strain U112 of the closely related species Francisella novicida. Strains were incubated in saline solution (0.9% NaCl) microcosms for 24 weeks at both 4°C and 20°C, whereupon viability and biofilm formation were measured. These temperatures were selected to approximate winter and summer temperatures of fresh water in Scandinavia, respectively. U112 and Schu S4 ΔwbtI formed biofilms, but F. tularensis strains FSC200 and Schu S4 and the LVS did not. All strains exhibited prolonged viability at 4°C compared to 20°C. U112 and FSC200 displayed remarkable long-term persistence at 4°C, with only 1- and 2-fold log reductions, respectively, of viable cells after 24 weeks. Schu S4 exhibited lower survival, yielding no viable cells by week 20. At 24 weeks, cells from FSC200, but not from Schu S4, were still fully virulent in mice. Taken together, these results demonstrate biofilm-independent, long-term survival of pathogenic F. tularensis subsp. holarctica in conditions that mimic overwinter survival in aquatic environments.
IMPORTANCE Tularemia, a disease caused by the environmental bacterium Francisella tularensis, is characterized by acute febrile illness. F. tularensis is highly infectious: as few as 10 organisms can cause human disease. Tularemia is not known to be spread from person to person. Rather, all human infections are independently acquired from the environment via the bite of blood-feeding arthropods, ingestion of infected food or water, or inhalation of aerosolized bacteria. Despite the environmental origins of human disease events, the ecological factors governing the long-term persistence of F. tularensis in nature between seasonal human outbreaks are poorly understood. The significance of our research is in identifying conditions that promote long-term survival of fully virulent F. tularensis outside a mammalian host or insect vector. These conditions are similar to those found in natural aquatic environments in winter and provide important new insights on how F. tularensis may persist long-term in the environment.
INTRODUCTION
Tularemia is a widely distributed zoonotic disease in the Northern Hemisphere caused by the bacterium Francisella tularensis. Human disease is mainly associated with strains from two subspecies, which have different geographical distributions. Francisella tularensis subsp. holarctica is found throughout the Northern Hemisphere, whereas Francisella tularensis subsp. tularensis is found only in North America. In humans, infections with F. tularensis are acquired from the environment via the bite of blood-feeding arthropods, ingestion of infected food or water, direct contact with infected animals, or inhalation of aerosolized bacteria. Infection can lead to acute febrile illness, and arthropod-related transmission peaks in the summer and autumn of outbreak years. Francisella is a large and diverse genus that includes environmental species of minor clinical relevance, including opportunistic pathogens such as Francisella novicida, F. hispaniensis, and F. philomiragia, which cause disease only in immunocompromised humans (1–6). F. tularensis is one of the most infectious pathogenic bacteria known; as few as 10 organisms can cause human infection by inoculation of the skin or inhalation of aerosolized bacteria (7), and it is regarded as a potential biological weapon and bioterrorism agent (8, 9). Naturally occurring F. tularensis causes tularemia in mammals, and more than 250 species have been reported to be naturally infected by F. tularensis (10). All human cases are acquired directly from the environment, and disease events in humans are often associated with zoonotic events in the environment. Predicting outbreaks of tularemia is extremely complex because of the numerous species described as susceptible to this disease, lack of knowledge of the complete life cycle of the bacterium, and the unknown natural reservoir of the bacterium. However, the capacity of F. tularensis to remain highly pathogenic in mammals is likely important to its natural life cycle.
F. tularensis appears to persist in the environment outside infected mammals and arthropods but, despite more than 100 years of research, little is known about the specific mechanisms of this environmental persistence (11). Human tularemia is typically characterized by irregular outbreaks that can be separated by several years within a small geographical region (disease focus). Previous studies have revealed persistence of the bacterium outside mammalian hosts or arthropod vectors in water and sediment for at least 16 months (12). In an area of Sweden where tularemia is endemic, F. tularensis subsp. holarctica DNA was detected by PCR in sediment and water samples collected during both outbreak and nonoutbreak years (13). In addition, genomic studies have confirmed the early findings of environmental persistence in disease foci from the early and mid-1900s (14, 15) and also confirmed that these foci have persisted to the present in both Western Europe (16) and Ukraine (17).
Persistence of F. tularensis in nature outside a host would require the ability to survive periods of severe nutrient limitation and variable temperatures. The ability to survive extended periods of starvation or other forms of environmental stress may be potentially conferred by symbiotic or parasitic interactions with protozoa (18–22) and/or associations with arthropod species (23, 24). It has also been hypothesized that F. tularensis forms biofilms, which could enhance persistence in the aquatic environment (25), consistent with the environmental lifestyle of many other bacteria. In laboratory studies performed in rich nutrient medium and at close to body temperature, isolates of F. novicida, F. philomiragia, F. tularensis subsp. holarctica, and F. tularensis subsp. tularensis have all been induced to form biofilms on the wells of plastic culturing plates (26–32).
Lower temperatures and other environmental parameters may be favorable for increased survival in F. tularensis. Cold water contaminated by carcasses or excreta of infected animals can remain infectious for as long as 10 weeks (12, 33). It also has been suggested that oceanic salt sprays may promote viability of F. tularensis in water (34). Berrada and Telford (34) utilized sterilized fresh and brackish water samples from Martha’s Vineyard (Massachusetts, USA) that were incubated at 20°C and found that the longest survival times of both F. tularensis subsp. tularensis (32 days) and F. tularensis subsp. holarctica (live vaccine strain [LVS], 42 days) occurred in brackish water (3.6% NaCl), with an intermediate survival time in physiological saline solution (0.85% NaCl) and the lowest survival time in freshwater. Additionally, early studies on factors that enhance F. tularensis spp. growth in culture noted that optimal growth could be obtained at 1 to 2% NaCl in culture medium (35). Also, the pH for optimal growth of F. tularensis subsp. holarctica is in the range of 5.8 to 6.3 (36), but both F. tularensis subsp. tularensis and F. tularensis subsp. holarctica show relatively high survival following temporal acid treatment (37, 38), and low-nutrient preadaptation in natural water resulted in even greater acid resistance (38).
In this study, we investigated the survival of F. tularensis at low temperatures in low-nutrient water, and our findings lead us to challenge the hypothesis that fully virulent F. tularensis strains form biofilms under conditions that resemble environments where the bacteria may persist in nature. We documented that the combination of low temperature and physiological saline (0.9% NaCl) increased F. tularensis survival times substantially compared with earlier findings that examined only the effects of saline at higher temperatures.
RESULTS
F. tularensis strains do not form biofilms in low-nutrient water at either 20°C or 4°C.
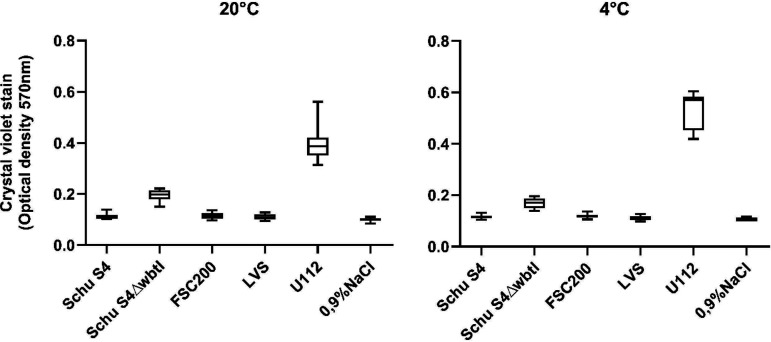
The only strains that developed biofilm during incubation in the saline solution (0.9% NaCl), as demonstrated by crystal violet staining, were F. novicida U112 and the Schu S4 ΔwbtI mutant (Fig. 1). These strains developed biofilms at the first sampling, performed at 2 weeks, which were quantified by measurement of optical density at 570 nm (OD570) as 0.57 ± 0.04 for U112 and 0.17 ± 0.02 for the Schu S4 ΔwbtI mutant in the 4°C incubations (Fig. 1). In a hierarchical linear mixed model (LMM), biofilm formation by U112 obtained a corresponding coefficient estimate of 0.43 (95% confidence interval [CI], 0.377 to 0.486; P < 1.0E−16) (see Fig. S1 in the supplemental material), whereas Schu S4 ΔwbtI resulted in an estimate of 0.059 (95% CI, 0.008 to 0.110; P = 0.038). Both comparisons were made relative to the negative control with saline solution (0.9% NaCl), suggesting that biofilm formation by the U112 strain is predicted to be 0.43 crystal violet stain assay unit above the negative control, on average.
FIG 1.
Biofilm formation of Francisella strains at 20°C (left) and 4°C (right) measured over time. Bacterial strains were incubated in a saline solution (0.9% NaCl), and biofilm formation was quantified using crystal violet stain and optical density measurement performed at 2, 3, 4, 6, 8, 10, 12, and 24 weeks incubation. Box plots present the median, quartile, minimum, and maximum of measurements. All data from the 2-, 3-, 4-, 6-, 8-, 10-, 12-, and 24-week measurements are presented in one whisker box plot per strain.
The amount of biofilm formed by the Schu S4 ΔwbtI strain was constant throughout the experiment, with no significant increase in crystal violet staining from sampling week 2 to week 24 (model estimate, 0.003; standard deviation, 0.006). For strain U112, the amount of biofilm decreased throughout the sampling period (estimate, −0.016; standard deviation, 0.006), suggesting that the biofilm would be reduced on average by 4% each week (if all other conditions were unchanged). At the 24-week sampling, the U112 biofilm in the 4°C incubation was at an optical density of 0.43 ± 0.09 in the crystal violet stain. There was no significant difference in the amount of biofilm formed by U112 and Schu S4 ΔwbtI at 4°C compared to the 20°C incubation (estimate, 0.0; 95% CI, −0.013 to 0.013; P = 1.0).
F. tularensis strains Schu S4 and FSC200 and the LVS displayed no biofilm formation at either 20°C or 4°C. The crystal violet stain assay results for these strains were not significantly different from that of the negative control with saline solution (0.9% NaCl) and no bacteria (estimate, 0; P = 1.0) (see Fig. S1).
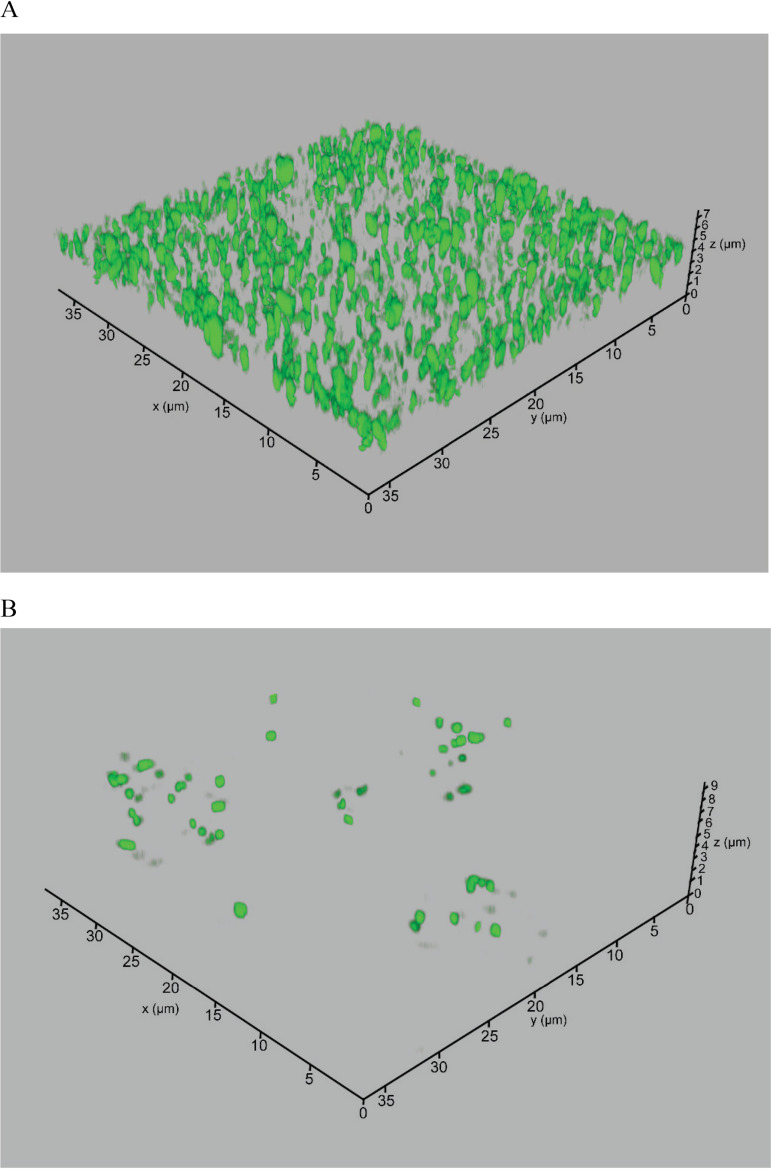
Furthermore, biofilm formation by green fluorescent protein (GFP)-labeled U112 was visualized with confocal microscopy (Fig. 2). Three-dimensional images of 1-week incubations detected the formation of biofilm in U112, with the thickness of attached cells ranging from 0.5 to 4 μm. However, the LVS did not form biofilm, as demonstrated by the crystal violet stain (Fig. 1), and confocal microscopy of a GFP-labeled LVS showed that very few cells were attached to the surface (Fig. 2).
FIG 2.
Confocal laser scanning microscopy of U112pKK289Kan-gfp (A) and LVSpKK289Kan-gfp (B), expressing GFP, after 1 week in 0.9% NaCl in 20°C.
All strains exhibited increased survival at 4°C compared to 20°C.
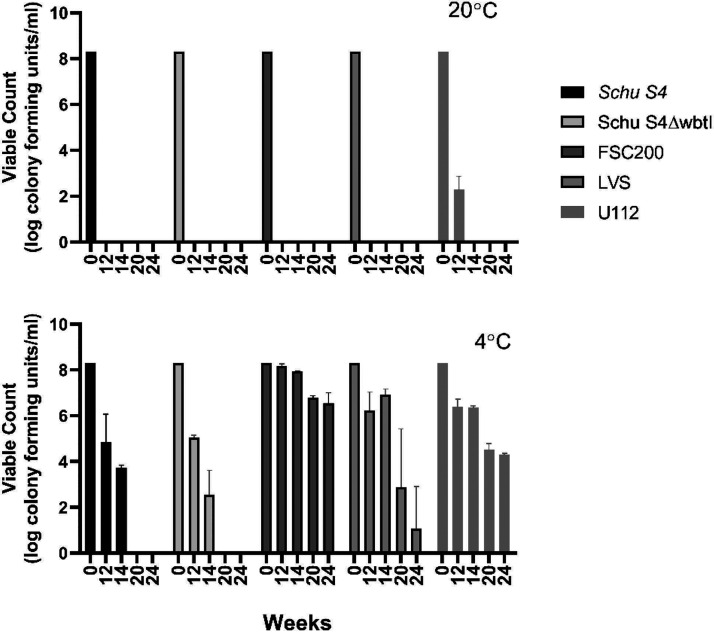
Viable-count analysis of planktonic cells in the biofilm incubation at 20°C showed a loss of viability by 12 weeks for all strains studied (Fig. 3), except for strain U112, which retained a population of viable cells at 2 × 102 CFU/ml after 12 weeks. After 14 weeks in 20°C, none of the bacterial strains were culturable.
FIG 3.
Viable counts of planktonic bacteria in the biofilm assay over time (0, 12, 14, 20, and 24 weeks). Francisella strains were incubated in 0.9% NaCl at 20°C and 4°C. Columns show means for six replicates (except those for FSC200 and the LVS at 24 weeks, which show means for three replicates), and error bars represent standard deviations. Absence of bars indicates no CFU.
In contrast, all strains retained viability for 14 weeks at 4°C (Fig. 3), irrespective of whether they formed biofilms. Interestingly, Schu S4 lost viability between 14 and 20 weeks, whereas FSC200, the LVS, and U112 were still viable after 24 weeks in the saline solution at 4°C. During the 6-month incubation period, FSC200 showed only a 2-fold log reduction in viable counts, from 1 × 108 CFU/ml to 1 × 106 CFU/ml (Fig. 3).
F. tularensis subsp. holarctica but not F. tularensis subsp. tularensis strains maintain virulence after 24 weeks in 4°C low-nutrient water.
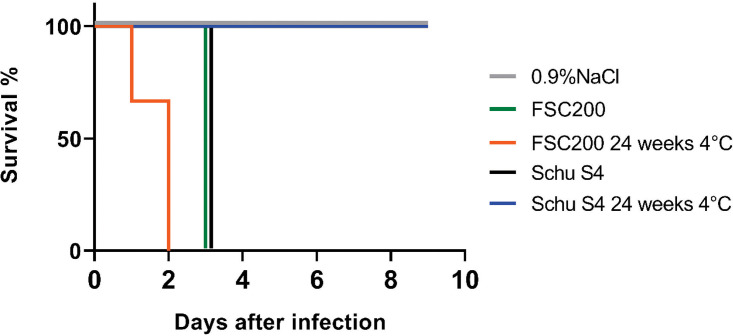
Mice infected with the FSC200 sample that had been incubated at 4°C for 24 weeks showed symptoms of disease at day 1 or 2 postinfection (Fig. 4). This confirms that the surviving FSC200 population remained highly virulent after incubation at 4°C for 24 weeks. Based on the viable-count analysis of FSC200 incubated at 4°C for 24 weeks (Fig. 3), the mice received an infectious dose of 1 × 105 CFU. In contrast, mice infected with the Schu S4 sample incubated in 4°C for 24 weeks did not show any symptoms of disease during the 10-day study, consistent with a lack of viability (no CFU) observed for these strains past 20 weeks (Fig. 3). Viable-count analysis confirmed the presence of F. tularensis in spleens from mice infected with FSC200 incubated in 4°C for 24 weeks but not in those from mice infected with Schu S4 incubated in 4°C for 24 weeks (data not shown). The control mice that were infected with ∼102 CFU of FSC200 and Schu S4 (grown overnight on supplemented GCII agar) showed symptoms of disease at day 3 postinfection (Fig. 4).
FIG 4.
Virulence of Francisella tularensis FSC200 (3 mice) and Schu S4 (3 mice) populations, incubated at 4°C for 24 weeks, in the C57BL/6J mouse model. FSC200 and Schu S4 from overnight cultures and an infectious dose of 102 CFU were used as a control (3 mice for each strain) and 0.9% NaCl was used as a negative control (2 mice).
DISCUSSION
We identified two key insights in the long-term survival of fully virulent strains of F. tularensis outside hosts in the type of nutrient-limited aquatic conditions they would be expected to encounter in nature. First, the long-term survival under these conditions of pathogenic F. tularensis strains known to cause disease in humans does not appear to be dependent on intrinsic biofilm formation. Of course, this does not exclude the possibility that in the environment, F. tularensis survival is potentially enhanced by biofilms produced by other organisms. Second, survival of planktonic Francisella cells in nutrient-limited aquatic conditions is greatly extended at lower temperatures. In particular, the planktonic survival of F. tularensis subsp. tularensis for over 3 months and F. tularensis subsp. holarctica for over 6 months at lower temperatures suggests a critical factor which could allow viable F. tularensis, in general, to overwinter in nutrient-limited aquatic environments. The differences observed between the two subspecies lend support to an idea originally developed by Jellison (39) that F. tularensis subsp. holarctica might be more adapted to survival in aquatic environments, such as streams, ponds, lakes, and rivers, whereas F. tularensis subsp. tularensis may be less adapted to long-term survival in aquatic conditions.
The only strain that produced significant levels of biofilm under the conditions utilized in this study (i.e., cold and low-nutrient water) was strain U112, which corroborates previous studies that suggest that biofilm formation is an environmental survival mechanism for F. novicida (32). Originally, F. novicida was isolated from a turbid water sample (1), and it has since been detected in brackish and saltwater sources, but no association with arthropod vectors or animals has been demonstrated in nature (1, 23, 40–42). Compared with F. tularensis, the genome of F. novicida is larger and more complex; it shows a higher degree of metabolic competence, higher levels of recombination, and dN/dS ratios (ratios of nonsynonymous to synonymous substitutions) consistent with a free-living environmental niche (43, 44). Several studies have contributed to the characterization of F. novicida biofilm formation and composition, revealing that the biofilm matrix consist of nucleic acids, proteins, exopolysaccharides (including cellulose), and polymeric β-1,4-linked N-acetylglucosamine (26, 27, 29, 31, 32). A gene cluster present in F. novicida but absent in F. tularensis is involved in the synthesis and degradation of the secondary messenger molecule c-di-GMP, which regulates the switch from a free-living planktonic lifestyle to a biofilm-associated lifestyle (45). High c-di-GMP levels program F. novicida to produce biofilm and inhibit virulence (45), thus promoting survival outside the host. This c-di-GMP signaling cascade is missing in F. tularensis, which is consistent with the concept that F. tularensis is a highly niche-restricted pathogen (43). In F. tularensis, loss of the ability to produce a functional lipopolysaccharide (LPS) O-antigen due to a mutation in the wbt locus results in enhanced biofilm formation in culture medium at 37°C (31). Accordingly, the only F. tularensis strain where biofilm formation could be detected under the conditions used in this experiment was the Schu S4 ΔwbtI mutant, which has a dysfunctional LPS O-antigen; however, this mutant is completely avirulent (46, 47).
F. tularensis is well known for its persistence in water. Parker et al. (12) showed persistence in water and sediment for at least 16 months in the Gird Creek area (Montana, USA). However, a high level of variation exists in the length of time that F. tularensis persists under laboratory conditions. In a sample of naturally contaminated water from Gird Creek stored at 7°C, the pathogen survived for a shorter time, at least 23 days but not more than 35 days (12). Naturally contaminated mud samples originating from Cattail Creek (Montana, USA) were stored under the same conditions but gave varying results, with persistence lasting throughout a 4- to 10-week period (12). Dearmon et al. (48) investigated survival in F. tularensis liquid cultures after storage at constant temperatures (37, 26, 15, 3, and 0°C) for 1 to 111 days and found that long-term survival through the entire time period occurred only at the lowest temperatures (3°C and 0°C), with the highest proportions of culturable cells at 3°C. However, it should be noted that both studies (12, 48) were performed before the division of F. tularensis into subspecies came into practice, and it is not clear if F. tularensis subsp. holarctica and/or F. tularensis subsp. tularensis was under investigation in these studies. More recent studies have documented that F. tularensis subsp. holarctica remains viable for 21 to 70 days at 8°C in sterile tap water (49, 50) and 28 days in low-nutrient sterilized lake water incubated at 20°C (20). Other physical water parameters, such as salinity and pH, may also influence survival of the bacterium. In our experimental setup, we chose to use intermediate conditions for both salinity and pH (0.9% NaCl and pH 6.0).
Carcasses of wild animals deceased from tularemia and with high bacterial burdens, such as voles and beavers, can contaminate local surface waters (12, 15, 51–54). In line with this, F. tularensis subsp. holarctica has recently been shown to be equipped with a mechanosensitive channel that protects it from osmotic variations in its life cycle, such as that encountered when transitioning from a mammalian host to freshwater or drinking water (55). It is not known whether F. tularensis subsp. tularensis possesses this ability, but if it does not, this difference may account for the greater association of F. tularensis subsp. holarctica strains with water (56). In Turkey, oropharyngeal waterborne tularemia caused by contamination of water by small rodents deceased from infections with F. tularensis subsp. holarctica is frequently reported. The greater part of these outbreaks have occurred in late fall, winter, or early spring (57–59), which suggests that survival in lower water temperatures is significant for the epidemiology of F. tularensis subsp. holarctica. In Sweden, where humans predominantly develop ulceroglandular tularemia from bites of mosquitoes infected with F. tularensis subsp. holarctica (60–62), it is hypothesized that mosquitos may acquire the bacterium from the ephemeral waters that constitute the habitat of mosquito larvae. These temporary water pools occur in early spring during snowmelt and later in the year during periods of heavy rainfall and are prone to alternate between dilution by rain and an increase in salinity due to evaporation. Field-collected mosquito larvae reared in such temporary waters, as well as mosquito larvae experimentally exposed to F. tularensis subsp. holarctica during development in a laboratory setting, have been documented to harbor the bacteria as adults (63–65). Thus, F. tularensis (F. tularensis subsp. holarctica in particular) seems well adapted to survive the transition from mammalian hosts to cold-water conditions found in the environment that are prone to large variation in osmolarity.
It is important to note that this study considered only axenic conditions for bacterial biofilm formation and survival and that conditions in natural waters with a high background of competing and predatory microorganisms are bound to play an important role in bacterial persistence in water. Interestingly, Buse et al. (66) observed growth of F. tularensis subsp. tularensis (strain Schu S4) but not F. tularensis subsp. holarctica (the LVS and strain IN99) among a high background of competing microorganisms in well water storage experiments when shifted to a 37°C incubation. This suggest that in these complex environments, F. tularensis subsp. holarctica remains nonactive in response to a temperature shift, whereas F. tularensis subsp. tularensis is more opportunistic or competitive and prone to induce growth. As shown for several species of aquatic bacteria, there is a competitive advantage in inactivity (or entering a quiescent state) (67, 68). Quiescent bacteria in cold-water conditions have been shown to experience lower biological competition than actively growing cells (69).
Our findings suggest that the planktonic survival of F. tularensis subsp. holarctica for over 6 months in cold water may be a critical mechanism by which viable and fully virulent cells overwinter. This suggests the possibility of survival of F. tularensis in the environment between host-associated replication events. The maximum density point of freshwater is at approximately 4°C, and this property of freshwater ensures that the bottom of a body of water will remain at low temperature, yet unfrozen, during the winter period. This type of thermal stratification is usually seasonal in the Northern Hemisphere, where F. tularensis occurs. Mixing of the water layers during spring turnover would then lead to contact of the bacteria with susceptible animals, either directly by intake of water or indirectly through bridging vectors associated with water. These results are compatible with a decay model of survival in the environment in which, after a certain time has passed (time lapse varying with ecosystem and environmental conditions as well as presence of hosts, vectors, and reservoirs), the bacteria will go extinct unless a susceptible host can be infected.
MATERIALS AND METHODS
Bacterial strains and growth conditions.
All Francisella strains used in this study (Table 1) were cultured on GCII agar (chocolate agar) containing 1% hemoglobin and 1% IsoVitaleX (70). The cultures were incubated at 37°C in 5% CO2 if not stated otherwise. Laboratory work involving virulent strains was performed in a biosafety level 3 (BSL3) laboratory.
TABLE 1.
Francisella strains and constructs used in the study
| Strain/construct | Subspecies | Description | Source and/or reference |
|---|---|---|---|
| U112 | F. novicida | Identified as FSC040 here and in previous publications | Water, 1950, Utah (1) |
| FSC200 | F. tularensis subsp. holarctica | Wild-type strain | Human ulcer, 1998, Sweden (76) |
| LVS | F. tularensis subsp. holarctica | Live vaccine strain; identified as FSC155 here and in previous publications | USAMRIID |
| Schu S4 | F. tularensis subsp. tularensis | Wild type strain. Identified as FSC237 here and in previous publications | Human ulcer, 1941, Ohio (77) |
| Schu S4 ΔwbtI | F. tularensis subsp. tularensis | Mutant of FSC237 characterized by loss of the long-chain O-polysaccharide | 47 |
| LVSpKK289Kan-gfp | F. tularensis subsp. holarctica | FSC155 expressing GFP in trans | This study |
| U112pKK289Kan-gfp | F. novicida | FSC040 expressing GFP in trans | This study |
| pKK289Kan-gfp | groELS promoter; Ft ori; p15A ori; GFP; Kanr | 71 |
Construction of a F. novicida strain expressing GFP.
The pKK289Kan-gfp plasmid (71) was introduced into U112 and the LVS by electroporation as previously described (72). The resulting strains, U112pKK289Kan-gfp and LVSpKK289Kan-gfp, expressing GFP in trans, were verified by selection on GCII agar plates supplemented with kanamycin.
Microtiter plate biofilm quantification assay and viable count.
Bacterial strains were grown overnight as described above. The bacteria were then harvested from the surface of GCII agar plates and suspended in saline solution (0.9% NaCl, pH 6) at a concentration of 108 CFU/ml, as determined by measurement of optical density at 540 nm (OD540). Six replicate aliquots of 200 μl from each concentrated inoculum were placed in standard 96-well plates and sealed. One 96-well plate was prepared for each sampling time point and duplicated for the two incubation temperatures, 20°C and 4°C. Planktonic growth at different temperatures was assessed with viable counts at weeks 0, 12, 14, 20, and 24 by plating 100 μl onto supplemented GCII agar plates from 10-fold serial dilutions in 1× phosphate-buffered saline (1× PBS).
To measure biofilm formation, planktonic bacteria (at weeks 2, 3, 4, 6, 8, 10, 12, and 24) were aspirated and wells were washed three times with 1× PBS to remove all remaining nonadherent cells. Plates were incubated for 1 h at 37°C, stained with 200 μl of 0.2% (wt/vol) crystal violet/well for 15 min, and washed 4 or 5 times with PBS. Plates were air dried, after which the dye bound to the adherent cells was resolubilized by the addition of 200 μl of 95% ethanol. The optical density of each well was measured at 570 nm using a microtiter plate reader.
Confocal microscopy.
Biofilm presence and thickness were evaluated using two GFP-expressing strains (U112pKK289Kan-gfp and LVSpKK289Kan-gfp) (Table 1). Bacteria were grown on solid agar as described above and suspended in 0.9% NaCl at a concentration of 109 CFU/ml, as determined by optical density (OD540). Bacterial suspensions of 150 μl were incubated on 8-well chamber slides (ibidi, Germany). After 1 week of incubation at room temperature, wells were washed three times with 1× PBS. Confocal microscopy was performed on a Leica SP8 inverted confocal system (Leica Microsystems) equipped with a HC PL APO 63×/1.40 numerical aperture oil immersion lens. Scanning was performed in line-by-line sequential mode. Images were captured and processed using LasX (Leica Microsystems) software.
Virulence in mice.
C57BL/6J female mice, aged 7 to 10 weeks (Scanbur), were used for virulence studies. Mice were housed under conventional conditions, given food and water ad libitum, and allowed to acclimatize before infection. The study was approved by the Local Ethical Committee on Laboratory Animals in Umeå, Sweden (A43-2018). Mice were injected intraperitoneally (i.p.) with 100 μl of the FSC200 and Schu S4 cells stored for 24 weeks at 4°C (in replicates of three mice per bacterial strain). As a positive control, mice were injected via the i.p. route with FSC200 (n = 2; 600 CFU each) and Schu S4 (n = 3; 100 CFU each) cells grown on GCII agar containing 1% hemoglobin and 1% IsoVitaleX, as described above. For negative controls, two mice were injected with 100 μl of 0.9% NaCl. Mice were observed for the weight reduction that precedes the visible symptoms of murine tularemia (i.e., >1.2 g of weight reduction within a single 24-h period). Moribund mice were euthanized immediately, and all remaining mice were euthanized after 10 days. All virulence tests in mice were performed under BSL3 conditions. The presence of Francisella in euthanized mice was confirmed by serial dilutions of homogenized spleens plated on agar plates (as described above).
Statistical analysis.
To assess the differences in biofilm production, a hierarchical linear mixed model (LMM) was fitted to the biofilm measurements, with crystal violet stain measurements as the response variable and temperature and strain as fixed effects. The weekly effect for each strain was included as random slope in the model to account for deviations across the sampling period (i.e., a linear growth or decay in biofilm production of each strain), while the “interaction week × strain” effect was included as a random intercept in the model to account for replicate dependencies. The R package lme4 (73) was used to fit the LMM to the data. Default values of the parameters controlling convergence of the glmer function in the lme4 package were used. P values of fixed effect estimates were calculated via a t test using Satterthwaite's degrees-of-freedom method implemented in the R package lmerTest (74). Confidence intervals (CI) were calculated using the Wald method. The coefficient estimates plot was created using the R package sjPlot (75).
Supplementary Material
ACKNOWLEDGMENTS
We thank Karin Wallgren and Anna-Lena Johansson for excellent technical assistance in virulence studies, Athar Alam for excellent support with confocal microscopy, and Jon Ahlinder for valuable contributions to the statistical evaluation of data.
This study was supported by funding by the U.S. Department of Defense’s Defense Threat Reduction Agency (DTRA, HDTRA1-18-1-0037) and the Swedish Ministry of Defence (A4042).
Footnotes
Supplemental material is available online only.
REFERENCES
- 1.Larson C, Wicht W, Jellison W. 1955. A new organism resembling P. tularensis isolated from water. Public Health Rep 70:253–258. doi: 10.2307/4589039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olsufjev NG, Emelyanova OS, Dunaeva TN. 1959. Comparative study of strains of B. tularense in the Old and New World and their taxonomy. Hyg Epidemiol Microbiol Immunol 3:138–149. [PubMed] [Google Scholar]
- 3.Hollis DG, Weaver RE, Steigerwalt AG, Wenger JD, Moss CW, Brenner DJ. 1989. Francisella philomiragia comb. nov. (formerly Yersinia philomiragia) and Francisella tularensis biogroup novicida (formerly Francisella novicida) associated with human disease. J Clin Microbiol 27:1601–1608. doi: 10.1128/JCM.27.7.1601-1608.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huber B, Escudero R, Busse H-J, Seibold E, Scholz HC, Anda P, Kampfer P, Splettstoesser WD. 2010. Description of Francisella hispaniensis sp. nov., isolated from human blood, reclassification of Francisella novicida (Larson et al. 1955) Olsufiev et al. 1959 as Francisella tularensis subsp. novicida comb. nov. and emended description of the genus Franc. Int J Syst Evol Microbiol 60:1887–1896. doi: 10.1099/ijs.0.015941-0. [DOI] [PubMed] [Google Scholar]
- 5.Penn R. 2010. Francisella tularensis (Tularemia), p 2927–2937. In Mandell GL, Bennet JE, Doblin R (ed), Mandell, Douglas and Bennett's principles and practice of infectious diseases, 6th ed. Elsevier Churchill, Livingstone, Philadelphia, PA. [Google Scholar]
- 6.Aravena-Román M, Merritt A, Inglis TJJ. 2015. First case of Francisella bacteraemia in Western Australia. New Microbes New Infect 8:75–77. doi: 10.1016/j.nmni.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. 1961. Tularemia vaccine study. I. Intracutaneous challenge. Arch Intern Med 107:689–701. doi: 10.1001/archinte.1961.03620050055006. [DOI] [PubMed] [Google Scholar]
- 8.Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, Mcdade JE, Osterholm MT, Toole TO, Parker G, Perl TM, Russell PK, Tonat K, O’Toole T, Parker G, Perl TM, Russell PK, Tonat K, Working Group on Civilian Biodefense. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763–2773. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- 9.Maurin M. 2015. Francisella tularensis as a potential agent of bioterrorism? Expert Rev Anti Infect Ther 13:141–144. doi: 10.1586/14787210.2015.986463. [DOI] [PubMed] [Google Scholar]
- 10.Olsufjev NG. 1974. Tularemia, p 1–28. In World Health Organization Inter-regional Travelling Seminar on Natural Foci of Zoonoses. USSR Ministry of Public Health Central Institute for Advanced Medical Training, Moscow, Russia. [Google Scholar]
- 11.Telford SR, Goethert HK. 2010. Toward an understanding of the perpetuation of the agent of tularemia. Front Microbiol 1:150. doi: 10.3389/fmicb.2010.00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker RR, Steinhaus EA, Kohls GM, Jellison WL. 1951. Contamination of natural waters and mud with Pasteurella tularensis and tularemia in beavers and muskrats in the northwestern United States. Bull Natl Inst Health 193:1–161. [PubMed] [Google Scholar]
- 13.Broman T, Thelaus J, Andersson A-C, Bäckman S, Wikström P, Larsson E, Granberg M, Karlsson L, Bäck E, Eliasson H, Mattsson R, Sjöstedt A, Forsman M. 2011. Molecular detection of persistent Francisella tularensis subspecies holarctica in natural waters. Int J Microbiol 2011:1–26. doi: 10.1155/2011/851946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jusatz HJ. 1952. Zweiter Bericht über das Vordringen der Tularämie nach Mittel-und Westeuropa in der Gegenwart. Z Hyg Infektionskr 134:350–374. [PubMed] [Google Scholar]
- 15.Pollitzer R. 1967. History and incidence of tularaemia in the Soviet Union: a review. Fordham University, Bronx, NY. [Google Scholar]
- 16.Dwibedi C, Birdsell D, Lärkeryd A, Myrtennäs K, Öhrman C, Nilsson E, Karlsson E, Hochhalter C, Rivera A, Maltinsky S, Bayer B, Keim P, Scholz HC, Tomaso H, Wittwer M, Beuret C, Schuerch N, Pilo P, Pérez MH, Rodriguez D, Escudero R, Anda P, Forsman M, Wagner DM, Larsson P, Johansson A. 2016. Long-range dispersal moved Francisella tularensis into Western Europe from the East. Microb Genom 2:e000100. doi: 10.1099/mgen.0.000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hightower J, Kracalik IT, Vydayko N, Goodin D, Glass G, Blackburn JK. 2014. Historical distribution and host-vector diversity of Francisella tularensis, the causative agent of tularemia, in Ukraine. Parasit Vectors 7:453. doi: 10.1186/s13071-014-0453-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berdal BP, Mehl R, Meidell NK, Lorentzen-Styr AM, Scheel O. 1996. Field investigations of tularemia in Norway. FEMS Immunol Med Microbiol 13:191–195. doi: 10.1111/j.1574-695X.1996.tb00235.x. [DOI] [PubMed] [Google Scholar]
- 19.Abd H, Johansson T, Golovliov I, Sandström G, Forsman M. 2003. Survival and growth of Francisella tularensis in Acanthamoeba castellanii. Appl Environ Microbiol 69:600–606. doi: 10.1128/aem.69.1.600-606.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thelaus J, Andersson A, Mathisen P, Forslund A-L, Noppa L, Forsman M. 2009. Influence of nutrient status and grazing pressure on the fate of Francisella tularensis in lake water. FEMS Microbiol Ecol 67:69–80. doi: 10.1111/j.1574-6941.2008.00612.x. [DOI] [PubMed] [Google Scholar]
- 21.El-Etr SH, Margolis JJ, Monack D, Robison RA, Cohen M, Moore E, Rasley A. 2009. Francisella tularensis type A strains cause the rapid encystment of Acanthamoeba castellanii and survive in amoebal cysts for three weeks postinfection. Appl Environ Microbiol 75:7488–7500. doi: 10.1128/AEM.01829-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buse HY, Schaefer FW, III, Rice EW. 2017. Enhanced survival but not amplification of Francisella spp. in the presence of free-living amoebae. Acta Microbiol Immunol Hung 64:17–36. doi: 10.1556/030.63.2016.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petersen JM, Mead PS, Schriefer ME. 2009. Francisella tularensis: an arthropod-borne pathogen. Vet Res 40:7. doi: 10.1051/vetres:2008045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zellner B, Huntley JF. 2019. Ticks and tularemia: do we know what we don’t know? Front Cell Infect Microbiol 9:146. doi: 10.3389/fcimb.2019.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Hoek ML. 2013. Biofilms: an advancement in our understanding of Francisella species. Virulence 4:833–846. doi: 10.4161/viru.27023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dean RE, Ireland PM, Jordan JE, Titball RW, Oyston PCF. 2009. RelA regulates virulence and intracellular survival of Francisella novicida. Microbiology (Reading) 155:4104–4113. doi: 10.1099/mic.0.031021-0. [DOI] [PubMed] [Google Scholar]
- 27.Margolis JJ, El-Etr S, Joubert LM, Moore E, Robison R, Rasley A, Spormann AM, Monack DM. 2010. Contributions of Francisella tularensis subsp. novicida chitinases and sec secretion system to biofilm formation on chitin. Appl Environ Microbiol 76:596–608. doi: 10.1128/AEM.02037-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verhoeven AB, Durham-Colleran MW, Pierson T, Boswell WT, Van Hoek ML. 2010. Francisella philomiragia biofilm formation and interaction with the aquatic protist Acanthamoeba castellanii. Biol Bull 219:178–188. doi: 10.1086/BBLv219n2p178. [DOI] [PubMed] [Google Scholar]
- 29.Durham-Colleran MW, Verhoeven AB, van Hoek ML. 2010. Francisella novicida forms in vitro biofilms mediated by an orphan response regulator. Microb Ecol 59:457–465. doi: 10.1007/s00248-009-9586-9. [DOI] [PubMed] [Google Scholar]
- 30.Mahajan UV, Gravgaard J, Turnbull M, Jacobs DB, McNealy TL. 2011. Larval exposure to Francisella tularensis LVS affects fitness of the mosquito Culex quinquefasciatus. FEMS Microbiol Ecol 78:520–530. doi: 10.1111/j.1574-6941.2011.01182.x. [DOI] [PubMed] [Google Scholar]
- 31.Champion AE, Catanzaro KCF, Bandara AB, Inzana TJ. 2019. Formation of the Francisella tularensis biofilm is affected by cell surface glycosylation, growth medium, and a glucan exopolysaccharide. Sci Rep 9:12252. doi: 10.1038/s41598-019-48697-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siebert C, Villers C, Pavlou G, Touquet B, Yakandawala N, Tardieux I, Renesto P. 2020. Francisella novicida and F. philomiragia biofilm features conditionning fitness in spring water and in presence of antibiotics. PLoS One 15:e0228591. doi: 10.1371/journal.pone.0228591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jellison WLW, Kohls GGM, Butler WJ, Weaver JA. 1942. Epizootic tularemia in the beaver, Castor canadensis, and the contamination of stream water with Pasteurella tularensis. Am J Epidemiol 36:168–182. doi: 10.1093/oxfordjournals.aje.a118815. [DOI] [Google Scholar]
- 34.Berrada ZL, Telford SR. 2011. Survival of Francisella tularensis type A in brackish-water. Arch Microbiol 193:223–226. doi: 10.1007/s00203-010-0655-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tamura JT, Gibby IW. 1943. Cultivation of Bacterium tularense in simplified liquid media. J Bacteriol 45:361–371. doi: 10.1128/JB.45.4.361-371.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klimentova J, Pavkova I, Horcickova L, Bavlovic J, Kofronova O, Benada O, Stulik J. 2019. Francisella tularensis subsp. holarctica releases differentially loaded outer membrane vesicles under various stress conditions. Front Microbiol 10:2304. doi: 10.3389/fmicb.2019.02304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Humrighouse BW, Adcock NJ, Rice EW. 2011. Use of acid treatment and a selective medium to enhance the recovery of Francisella tularensis from water. Appl Environ Microbiol 77:6729–6732. doi: 10.1128/AEM.05226-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adcock NJ, Morris BJ, Rice EW. 2014. Acid resistance in Francisella tularensis. Microbiologyopen 3:133–138. doi: 10.1002/mbo3.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jellison W. 1974. Tularemia in North America, 1930–1974. University of Montana, Missoula, MT. [Google Scholar]
- 40.Berrada ZL, Telford SR. 2010. Diversity of Francisella species in environmental samples from Martha’s Vineyard, Massachusetts. Microb Ecol 59:277–283. doi: 10.1007/s00248-009-9568-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brett M, Doppalapudi A, Respicio-Kingry LB, Myers D, Husband B, Pollard K, Mead P, Petersen JM, Whitener CJ. 2012. Francisella novicida bacteremia after a near-drowning accident. J Clin Microbiol 50:2826–2829. doi: 10.1128/JCM.00995-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kingry LC, Petersen JM. 2014. Comparative review of Francisella tularensis and Francisella novicida. Front Cell Infect Microbiol 4:35. doi: 10.3389/fcimb.2014.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Larsson P, Elfsmark D, Svensson K, Wikström P, Forsman M, Brettin T, Keim P, Johansson A. 2009. Molecular evolutionary consequences of niche restriction in Francisella tularensis, a facultative intracellular pathogen. PLoS Pathog 5:e1000472. doi: 10.1371/journal.ppat.1000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sjödin A, Svensson K, Ohrman C, Ahlinder J, Lindgren P, Duodu S, Johansson A, Colquhoun DJ, Larsson P, Forsman M. 2012. Genome characterisation of the genus Francisella reveals insight into similar evolutionary paths in pathogens of mammals and fish. BMC Genomics 13:268. doi: 10.1186/1471-2164-13-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zogaj X, Wyatt GC, Klose KE. 2012. Cyclic di-GMP stimulates biofilm formation and inhibits virulence of Francisella novicida. Infect Immun 80:4239–4247. doi: 10.1128/IAI.00702-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kadzhaev K, Zingmark C, Golovliov I, Bolanowski M, Shen H, Conlan W, Sjöstedt A. 2009. Identification of genes contributing to the virulence of Francisella tularensis SCHU S4 in a mouse intradermal infection model. PLoS One 4:e5463. doi: 10.1371/journal.pone.0005463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Twine SM, Vinogradov E, Lindgren H, Sjostedt A, Conlan JW. 2012. Roles for wbtC, wbtI, and kdtA genes in lipopolysaccharide biosynthesis, protein glycosylation, virulence, and immunogenicity in Francisella tularensis strain SCHU S4. Pathogens 1:12–29. doi: 10.3390/pathogens1010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dearmon IA, Orlando MD, Rosenwald AJ, Klein F, Fernelius AL, Lincoln RE, Middaugh PR. 1962. Viability and estimation of shelf-life of bacterial populations. Appl Microbiol 10:422–427. doi: 10.1128/AM.10.5.422-427.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Forsman M, Henningson EW, Larsson E, Johansson T, Sandstrom G. 2000. Francisella tularensis does not manifest virulence in viable but non-culturable state. FEMS Microbiol Ecol 31:217–224. doi: 10.1111/j.1574-6941.2000.tb00686.x. [DOI] [PubMed] [Google Scholar]
- 50.Gilbert SE, Rose LJ. 2012. Survival and persistence of nonspore-forming biothreat agents in water. Lett Appl Microbiol 55:189–194. doi: 10.1111/j.1472-765X.2012.03277.x. [DOI] [PubMed] [Google Scholar]
- 51.Janse I, van der Plaats RQJ, de Roda Husman AM, van Passel MWJ. 2018. Environmental surveillance of zoonotic Francisella tularensis in the Netherlands. Front Cell Infect Microbiol 8:140. doi: 10.3389/fcimb.2018.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bell JF, Stewart SJ. 1975. Chronic shedding tularemia nephritis in rodents: possible relation to occurrence of Francisella tularensis in lotic waters. J Wildl Dis 11:421–430. doi: 10.7589/0090-3558-11.3.421. [DOI] [PubMed] [Google Scholar]
- 53.Rossow H, Forbes KM, Tarkka E, Kinnunen PM, Hemmilä H, Huitu O, Nikkari S, Henttonen H, Kipar A, Vapalahti O. 2014. Experimental infection of voles with Francisella tularensis indicates their amplification role in tularemia outbreaks. PLoS One 9:e108864. doi: 10.1371/journal.pone.0108864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schulze C, Heuner K, Myrtennäs K, Karlsson E, Jacob D, Kutzer P, Große K, Forsman M, Grunow R. 2016. High and novel genetic diversity of Francisella tularensis in Germany and indication of environmental persistence. Epidemiol Infect 144:3025–3036. doi: 10.1017/S0950268816001175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Williamson DR, Dewan KK, Patel T, Wastella CM, Ning G, Kirimanjeswara GS. 2018. A single mechanosensitive channel protects Francisella tularensis subsp. holarctica from hypoosmotic shock and promotes survival in the aquatic environment. Appl Environ Microbiol 84:e02203-17. doi: 10.1128/AEM.02203-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hennebique A, Boisset S, Maurin M. 2019. Tularemia as a waterborne disease: a review. Emerg Microbes Infect 8:1027–1042. doi: 10.1080/22221751.2019.1638734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gürcan S, Otkun MT, Otkun M, Arikan OK, Ozer B. 2004. An outbreak of tularemia in Western Black Sea region of Turkey. Yonsei Med J 45:17–22. doi: 10.3349/ymj.2004.45.1.17. [DOI] [PubMed] [Google Scholar]
- 58.Gürcan S, Eskiocak M, Varol G, Uzun C, Tatman-Otkun M, Sakru N, Karadenizli A, Karagöl C, Otkun M. 2006. Tularemia re-emerging in European part of Turkey after 60 years. Jpn J Infect Dis 59:391–393. [PubMed] [Google Scholar]
- 59.Gürcan S. 2007. Francisella tularensis and tularemia in Turkey. Mikrobiyol Bul 41:621–636. [PubMed] [Google Scholar]
- 60.Eliasson H, Broman T, Forsman M, Bäck E. 2006. Tularemia: current epidemiology and disease management. Infect Dis Clin North Am 20:289–311. doi: 10.1016/j.idc.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 61.Eliasson H, Bäck E. 2007. Tularaemia in an emergent area in Sweden: an analysis of 234 cases in five years. Scand J Infect Dis 39:880–889. doi: 10.1080/00365540701402970. [DOI] [PubMed] [Google Scholar]
- 62.Eliasson H, Lindbäck J, Nuorti JP, Arneborn M, Giesecke J, Tegnell A. 2002. The 2000 tularemia outbreak: a case-control study of risk factors in disease-endemic and emergent areas, Sweden. Emerg Infect Dis 8:956–960. doi: 10.3201/eid0809.020051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lundstrom JO, Andersson ACC, Backman S, Schafer ML, Forsman M, Thelaus J. 2011. Transstadial transmission of Francisella tularensis holarctica in mosquitoes, Sweden. Emerg Infect Dis 17:794–799. doi: 10.3201/eid1705.100426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Thelaus J, Andersson A, Broman T, Bäckman S, Granberg M, Karlsson L, Kuoppa K, Larsson E, Lundmark E, Lundström JO, Mathisen P, Näslund J, Schäfer M, Wahab T, Forsman M. 2014. Francisella tularensis subspecies holarctica occurs in Swedish mosquitoes, persists through the developmental stages of laboratory-infected mosquitoes and is transmissible during blood feeding. Microb Ecol 67:96–107. doi: 10.1007/s00248-013-0285-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bäckman S, Näslund J, Forsman M, Thelaus J. 2015. Transmission of tularemia from a water source by transstadial maintenance in a mosquito vector. Sci Rep 5:7793. doi: 10.1038/srep07793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Buse HY, Morris BJ, Rice EW. 2020. Early detection of viable Francisella tularensis in environmental matrices by culture-based PCR. BMC Microbiol 20:66. doi: 10.1186/s12866-020-01748-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cole JJ. 1999. Aquatic microbiology for ecosystem scientists: new and recycled paradigms in ecological microbiology. Ecosystems 2:215–225. doi: 10.1007/s100219900069. [DOI] [Google Scholar]
- 68.Lennon JT, Jones SE. 2011. Microbial seed banks: the ecological and evolutionary implications of dormancy. Nat Rev Microbiol 9:119–130. doi: 10.1038/nrmicro2504. [DOI] [PubMed] [Google Scholar]
- 69.Chrzanowski TH, Šimek K. 1990. Prey-size selection by freshwater flagellated protozoa. Limnol Oceanogr 35:1429–1436. doi: 10.4319/lo.1990.35.7.1429. [DOI] [Google Scholar]
- 70.World Health Organization. 2007. WHO guidelines on tularaemia. WHO Press, Geneva, Switzerland. [Google Scholar]
- 71.Bönquist L, Lindgren H, Golovliov I, Guina T, Sjöstedt A. 2008. MglA and Igl proteins contribute to the modulation of Francisella tularensis live vaccine strain-containing phagosomes in murine macrophages. Infect Immun 76:3502–3510. doi: 10.1128/IAI.00226-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Maier TM, Havig A, Casey M, Nano FE, Frank DW, Zahrt TC. 2004. Construction and characterization of a highly efficient Francisella shuttle plasmid. Appl Environ Microbiol 70:7511–7519. doi: 10.1128/AEM.70.12.7511-7519.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bates D, Mächler M, Bolker BM, Walker SC. 2015. Fitting linear mixed-effects models using lme4. J Stat Softw 67:1–48. [Google Scholar]
- 74.Kuznetsova A, Brockhoff PB, Christensen RHB. 2017. lmerTest package: tests in linear mixed effects models. J Stat Softw 82:1–26. [Google Scholar]
- 75.Ludecke D. 2020. Package “sjPlot”: data visualization for statistics in social science. R Package version 285.
- 76.Svensson K, Sjödin A, Byström M, Granberg M, Brittnacher MJ, Rohmer L, Jacobs MA, Sims-Day EH, Levy R, Zhou Y, Hayden HS, Lim R, Chang J, Guenthener D, Kang A, Haugen E, Gillett W, Kaul R, Forsman M, Larsson P, Johansson A. 2012. Genome sequence of Francisella tularensis subspecies holarctica strain FSC200, isolated from a child with tularemia. J Bacteriol 194:6965–6966. doi: 10.1128/JB.01040-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Larsson P, Oyston PCF, Chain P, Chu MC, Duffield M, Fuxelius H-H, Garcia E, Hälltorp G, Johansson D, Isherwood KE, Karp PD, Larsson E, Liu Y, Michell S, Prior J, Prior R, Malfatti S, Sjöstedt A, Svensson K, Thompson N, Vergez L, Wagg JK, Wren BW, Lindler LE, Andersson SGE, Forsman M, Titball RW. 2005. The complete genome sequence of Francisella tularensis, the causative agent of tularemia. Nat Genet 37:153–159. doi: 10.1038/ng1499. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.