Abstract
The Building Healthy Children home visiting preventive intervention was designed to provide concrete support and evidence-based intervention to young mothers and their infants who were at heightened risk for child maltreatment and poor developmental outcomes. This paper presents two studies examining the short and long-term effectiveness of this program at promoting positive parenting and maternal mental health, while preventing child maltreatment and harsh parenting. It also examines the intervention’s sustained effect on child symptomatology and self-regulation. At baseline, young mothers and their infants were randomly assigned to receive BHC or Enhanced Community Standard. Families were assessed longitudinally across four time points. Data was also collected from the child’s teacher at follow-up. Mothers who received BHC evidenced significant reductions in depressive symptoms at mid-intervention, which was associated with improvements in parenting self-efficacy and stress as well as decreased child internalizing and externalizing symptoms at post-intervention. The follow-up study found that BHC mothers exhibited less harsh and inconsistent parenting, and marginally less psychological aggression. BHC children also exhibited less externalizing behavior and self-regulatory difficulties across parent and teacher report. Following the impactful legacy of Dr. Edward Zigler, these findings underline the importance of early, evidence-based prevention to promote well-being in disadvantaged families.
Keywords: Building Healthy Children, home visiting, preventive intervention, young mothers, child behavior
Introduction
Edward Zigler – ‘the Father of Head Start’ – was known for his steadfast commitment to bridging science and policy in service of children living in poverty (Zigler & Valentine, 1979). He highlighted for many, the impact of early experience on child development, and pioneered preventive intervention efforts for low-income families with young children. A staunch advocate of family and community collaboration, Zigler’s research and policy contributions drew attention to the importance of meaningful family involvement and the essential role of parents in the lives of their children (e.g. Luthar & Zigler, 1991). He spoke to the importance of a whole child approach, which emphasized the impact of family functioning and social-emotional needs on child development and education (Zigler, Taussig, & Black, 1992; Zigler & Trickett, 1978). The Building Healthy Children home visiting program (BHC; Paradis, Sandler, Manly, & Valentine, 2013) for young mothers and their infants was inspired by the work of Dr. Edward Zigler and other likeminded colleagues who emphasized the importance of early childhood intervention to mitigate risk factors associated with poverty and to foster healthy child development.
BHC was designed to provide concrete support and evidence-based intervention to young families at heightened risk for maladaptive parenting practices, child maltreatment, and poor developmental outcomes.
Child maltreatment is both a pervasive and significant public health concern. National data indicate that 1 in 4 children experience some form of child maltreatment in their lifetime (Barnett, Manly, & Cicchetti, 1993; CDC, 2014; Finkelhor, Turner, Shattuck, & Hamby, 2013; Vachon, Krueger, Rogosch, & Cicchetti, 2015). Youngest children (birth to 1 year) are often the most vulnerable (National Research Council, 2014; U.S.D.H.H.S., 2020). The impact of child maltreatment is widespread and enduring, and may initiate a negative cascade affecting multiple developmental domains. Trauma experienced at the hands of a caregiver is likely to fundamentally impact a child’s social, emotional, cognitive, and neurobiological development (Cicchetti & Toth, 2016; Cowell, Cicchetti, Rogosch, & Toth, 2015). The effects permeate various arenas of functioning, including mental and physical health, as well as education, employment and interpersonal relationships (National Research Council, 2014).
The cost of child maltreatment can be understood both monetarily and in terms of the suffering experienced by the victims and those that interact with them (e.g. family, peers, future romantic partner), the latter of which is impossible to fully quantify. Although human suffering should be enough to justify prevention efforts, quantifying the monetary cost is often necessary in advocating for policies that support prevention and treatment. Monetarily, the lifetime economic burden of first-time child maltreatment in the United States in 2014 was estimated to be $5.9 trillion in lifetime spending, and $2.7 trillion in lost gross domestic profit (Perryman Group, 2014). These estimates include spending in the areas of health care, social welfare, criminal justice, and education, as well as the reduction in earnings due to child maltreatment. A significant portion of the cost is due to out of home placement in foster care (Halfon, Berkowitz, & Klee, 1992). The monetary and human costs of child maltreatment make it critical for researchers, practitioners, and policymakers alike to focus efforts on prevention.
The precursors and sequela of child maltreatment can be best understood through a developmental psychopathology lens. Developmental psychopathology is an interdisciplinary scientific framework for conceptualizing and examining the links between normal and abnormal development (Cicchetti, 1984; Cicchetti & Toth, 2005). For decades, our understanding of child maltreatment and its causes and consequences, have been shaped by the theoretical underpinnings of this perspective (e.g. Cicchetti & Toth, 1995, 2016). Extant literature has identified a number of risk factors for child maltreatment and poor parenting, ranging from sociodemographic variables (e.g. income, parent age and race/ethnicity, parent education, unplanned pregnancy), to parent-child relationship quality (e.g. attachment, maternal sensitivity), to parenting practices (e.g. harsh, insensitive parenting), to a parent’s own depression, mental health and caregiving history (Dixon, Browne, & Hamilton‐Giachritsis, 2005; Hussey, Chang, & Kotch, 2006; Sidebotham, Heron, & Team, 2006; Stith et al., 2009). Recognizing that no single approach can address the multitude of risk factors, BHC was designed as a multicomponent preventive intervention that delivers a menu of evidence-based services to this high-risk population.
As highlighted above, various sociodemographic factors and adverse life experiences place young mothers at risk for child maltreatment and suboptimal parenting. One such factor is early and/or unplanned pregnancy (Russotti et al., 2020). Although there has been a marked decline in early pregnancy in recent decades, rates among adolescent girls in the United States remain higher than other developed countries. In the United States, estimates of the rate of pregnancy among 15 to19-year-old girls range from 22.3 to 57 per 1,000 (Martin, Hamilton, Osterman, Driscoll, & Mathews, 2017). African-American and Latina girls, as well as socioeconomically disadvantaged girls, and those involved with the child welfare system, are all at disproportionate risk for young pregnancy (CDC, 2017). In addition, meta-analyses have indicated a 2-fold increase risk for adolescent pregnancy among girls with a history of childhood sexual abuse, and a nearly 4-fold increased risk among girls with both physical and sexual abuse histories (Madigan, Wade, Tarabulsy, Jenkins, & Shouldice, 2014; Noll, Shenk, & Putnam, 2008). Young mothers are at-risk for a myriad of negative outcomes including maternal depression, suboptimal parenting practices, and compromised mother-child attachment relationships (Hodgkinson, Beers, Southammakosane, & Lewin, 2014; Szigethy & Ruiz, 2001; Flaherty & Sadler, 2011; Lewin, Mitchell, & Ronzio, 2013). In addition, children of young mothers are more likely to be maltreated, experience mental health challenges and become young parents themselves (Furstenberg, Levine, & Brooks-Gunn, 1990; Harden et al., 2007; Moore & Brooks-Gunn, 2002). Taken together, it is evident that this population is characterized by a number of risk factors, highlighting the importance of early prevention efforts.
BHC was designed as a preventive intervention program to directly address the enhanced risk of young and socioeconomically disadvantaged mothers and their children. Program participants were mothers who had their first child prior to 21 years of age, and who were eligible to receive Temporary Assistance for Needy Families (TANF), addressing both age and socioeconomic risk factors. Although not a selection criterion, the majority of the mothers who participated identified as part of racial and/or ethnic minorities groups. The intervention models incorporated into BHC address additional risk factors associated with child maltreatment, poor parenting practices and maladaptive outcomes in children. These factors, identified as targets of intervention in one or more of the BHC components, include parent-child insecure attachment, maternal insensitivity, maternal trauma history, maternal depression and low social support, and limited knowledge of appropriate developmental expectations.
Fostering a positive parent-child relationship has significant effects on child development and functioning (Cicchetti et al., 2006; Lieberman, Van Horn, & Ippen, 2005). Attachment insecurity is closely linked to child maltreatment; therefore, fostering a secure attachment relationship and increasing maternal sensitivity can reduce or prevent the occurrence of child maltreatment (Morton & Browne, 1998; Thomas & Zimmer‐Gembeck, 2011). Higher rates of maternal sensitivity and responsiveness have also been related to lower rates of child internalizing and externalizing behavior (e.g. Deater-Deckard, Ivy, & Petrill, 2006; DeKlyen & Greenberg, 2008; Shaw, Gilliom, Ingoldsby, & Nagin, 2003; Stams, Juffer, & van IJzendoorn, 2002). One systematic review found that parental sensitivity is lower in ethnic minority populations, often due to social and economic stress. However, increased sensitivity was also predictive of positive child outcomes in these populations, highlighting sensitivity as a target for interventions aiming to improve child well-being (Mesman, van IJzendoorn, & Bakermans‐Kranenburg, 2012). In addition, ample data has supported the link between attachment and emotion regulation in children, suggesting that a secure attachment relationship lends itself to the development of adaptive regulatory abilities (Sroufe, 2005). This is important given the ample evidence identifying emotion dysregulation as a “transdiagnostic feature” of many mental illnesses (Beauchaine & Cicchetti, 2019, pp. 799). Deficits in executive function, self-regulation, and emotion regulation in childhood and adolescence increase the likelihood of psychopathology in adulthood (Cole, Hall & Hajal, 2017).
BHC utilizes Child-Parent Psychotherapy (CPP; Lieberman & Van Horn, 2005) to foster maternal sensitivity and secure attachment, particularly with families who have a history of trauma and/or are exhibiting difficulties in the parent-child attachment relationship. Empirical research on CPP has demonstrated that this treatment is effective at improving attachment security, increasing mothers’ positive expectations of their child, and decreasing maternal and child mental health symptoms. This intervention in particularly effective for mothers with past histories of trauma (Lieberman, Ippen & Van Horn, 2015; Toth, Maughan, Manly, Spagnola, & Cicchetti, 2002; Toth, Rogosch, Manly, & Cicchetti, 2006). CPP was developed for mothers who had experienced trauma, and much of the research has been conducted with impoverished and racially/ethnically diverse samples. This is important to note as approximately half of mothers receiving BHC services had experienced maltreatment themselves during their childhood.
Extant research has also identified maternal depression as a risk factor for poor child outcomes. Offspring vulnerability associated with maternal depression has been documented throughout development, and as early as infancy (Teti & Gelfand, 1999). Even mild, yet chronic maternal depressive symptoms may negatively impact children (e.g., Hammen & Brennan, 2003). Maternal depression has also been linked with less warmth and responsivity, and more coercive and inconsistent parenting (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Approximately 16–44% of adolescent mothers experience depression (Hodgkinson et al., 2014) and estimates may be even higher for racial and ethnic minority girls (Szigethy & Ruiz, 2001). Among young mothers with a trauma history, there is a 4-fold increased risk of postpartum depression (Meltzer-Brody et al., 2013), suggesting a significant vulnerability for depression. Given the prevalence and detrimental impact of maternal depression on parenting and child development, it is imperative to address these symptoms early by decreasing stigma and increasing access to mental health services.
BHC’s flexible approach to service delivery and home visiting model helps to reduce this stigma and increase access to needed services. One component offered as part of the BHC program is Interpersonal Psychotherapy for Depressed Adolescents (IPT-A; Mufson, Dorta, Moreau, & Weissman, 2004), which specifically addresses maternal depression. Empirical support for IPT-A for adolescent depression has been demonstrated by a number of RCTs (Mufson, Weissman, Moreau, & Garfinkel, 1999; Young, Mufson, & Davies, 2006). Results indicate that IPT-A is as effective as CBT in reducing depressive symptoms (Horowitz, Garber, Ciesla, Young, & Mufson, 2007). In addition, mothers receiving IPT have shown significant improvement in mother-child relationship quality, perceived stress, parenting attitudes and self-efficacy, and social support (Beeber et al., 2013; Mulcahy et al., 2010; Toth et al., 2013; Handley, Michl-Petzing, Rogosch, Cicchetti, and Toth, 2017). Notably, IPT-A and IPT have demonstrated efficacy across racially/ethnically diverse samples from various socioeconomic backgrounds, and in women with histories of trauma and PTSD (Duberstein et al., 2018; Markowitz et al., 2015; Rossello & Bernal, 1999; Toth et al., 2013).
Another way to foster positive parenting and child functioning is by increasing parent knowledge and appropriate expectations, while fostering social support. Zigler’s vision for a 21st Century school was born out of the recognition that recent societal changes have left many families isolated and alienated, with many parents raising children with little help or social support (Zigler & Finn-Stevenson, 2007). In addition, a large number of these families are living in poverty, creating a stressful environment for many children to grow-up. To counter this disadvantage, Zigler advocated for increased support services for families, including outreach and home visitation. One aspect of the 21st Century school model included parent support and outreach for at-risk families with infants and toddlers. This aspect of the program was modeled after the Parents as Teachers (PAT) curriculum, which emphasizes positive parenting behavior as the precipitant of developmental gains for children (Zigler & Finn-Stevenson, 2007). The major goals of PAT are to improve parents’ knowledge of normative child development, facilitate school readiness, and increase parents’ sense of competence and self-efficacy (Wagner & Clayton, 1999). Extant literature has linked parent knowledge and self-efficacy with a variety of positive parenting and child outcomes. Research suggests that parent education and home visiting programs are effective in reducing risk factors for child maltreatment and harsh parenting (e.g. Mikton & Butchart, 2009). In addition, parent self-efficacy is predictive of parenting behaviors as well as child adjustment (Jones & Prinz, 2005). Of particular relevance to this study, parent self-efficacy is a mechanism through which maternal history of childhood maltreatment predicts child behavior problems (Demeusy, Rogosch, Cicchetti, & Toth, 2018).
In order to enhance maternal knowledge of child development and foster self-efficacy, the BHC program also incorporated the PAT model. Empirical support for PAT has been demonstrated across a number of studies. Overall, positive effects on parent knowledge, parenting attitudes and behaviors, and parent’s perceived social support have been demonstrated, albeit inconsistently, across evaluations (Owen & Mulvihill, 1994; Pfannenstiel & Seltzer, 1989; Wagner, Spiker, & Linn, 2002). In terms of child functioning, there is evidence for the beneficial effect of PAT on children’s cognitive, language, and socio-emotional development (Drotar, Robinson, Jeavons, & Lester Kirchner, 2009; Pfannenstiel & Seltzer, 1989; Wagner et al., 2002). There is also promising evidence to suggest that engagement in PAT services helps to reduce the likelihood of child abuse and neglect, although additional research is needed in order to replicate this finding (Pfannenstiel et al., 1996; Pfannenstiel et al., 1991; Wagner & Clayton, 1999).
BHC was designed to address these multiple determinants of maladaptive parenting, child maltreatment and child psychopathology, using the aforementioned intervention models in conjunction with continuous outreach support. The outreach component addresses socioeconomic determinants of health to help relieve the stress of poverty on the families being served. Familial poverty is one of the strongest predictors of child abuse and neglect. Therefore, providing concrete support to families, especially during times of crisis or intensified need, is an important strategy to prevent child maltreatment (Horton, 2003). Incorporating this strategy, BHC utilizes a consistent outreach worker to address any concrete needs and barriers to healthcare, community services, and program engagement, while providing social support.
BHC utilizes a home visiting framework to deliver these comprehensive services. Home visiting is one of the most widespread, proactive approaches to preventing child maltreatment and promoting healthy development, particularly prenatally and during infancy. The Mother, Infant, and Early Childhood Home Visiting Program (MIECHV), established through the Patient Protection and Affordable Care Act, provides home visiting services to at-risk pregnant women and their children from birth to five years old (Avellar & Supplee, 2013). This federal investment has increased funding for and accessibility to these services, specifically those that are evidence-based. Several independent studies and comprehensive reviews have provided evidentiary support for home visiting in preventing child maltreatment and harsh parenting, while promoting adaptive child development (e.g. Avellar & Supplee, 2013; Howard & Brooks-Gunn, 2009; Mikton & Butchart, 2009). However, relatively fewer studies have investigated the long-term impact of infant home visiting services on parenting and child outcomes (Lyons-Ruth & Melnick, 2004).
Ample research has documented Nurse Family Partnership (NFP), a widely implemented home visiting intervention that assists high-risk mothers during pregnancy and post-delivery, as effective at preventing maltreatment and improving child outcomes (e.g. Eckenrode et al., 2000; Olds, 2006; Olds et al., 1997). BHC differs from NFP by incorporating a focus on child social emotional development, maternal mental health, and parent-child attachment in order to prevent child maltreatment and foster healthy development. Interestingly, research on NFP has revealed that avoidance of Child Protective Services (CPS) was most notable for the intervention group during the follow-up period, between the children’s fourth and fifteenth birthday (Olds et al., 1997). This finding echoes other studies which demonstrate that effect sizes for proactive interventions are larger at follow-up than immediately following the completion of the intervention (MacLeod & Nelson, 2000). These results support the notion that proactive prevention efforts can break a maladaptive pattern that may result in child maltreatment by targeting various known risk factors (Rutter, 1987). Together, these results highlight the importance of conducting long-term follow-up studies to better understand the impact of home visiting interventions over time.
Extensive research has been conducted on what makes home visiting programs more, or less, effective. In one review, Howard and Brooks-Gunn (2009) found that home-visiting programs are especially effective in child maltreatment prevention for first-time adolescent mothers, suggesting that these mothers may be more receptive to intervention having never engaged in poor parenting or child maltreatment previously. In addition, duration and frequency of visits have been shown to impact program effectiveness, with longer programs (greater than six months), and those that provide more frequent visits resulting in more positive outcomes (MacLeod & Nelson, 2000; Nievar, Van Egeren, & Pollard, 2010). Finally, many home visiting evaluations have found greater benefits for families at higher risk (e.g. low-income, unmarried) (Olds, 2008; Wagner et al., 2002). This suggests that targeting home visiting services to families at-risk for child maltreatment may increase the likelihood that the family benefits and that program funding is utilized to its fullest extent. BHC integrated this knowledge into its program design by providing services to high-risk adolescent mothers with no past history of CPS involvement, and by engaging families from birth to three years old on a regular (weekly) basis.
Although home visiting programs have proliferated over the past decade, additional research is needed in order to help us better understand what works for whom, and why (Roth & Fonagy, 2013). Ultimately, the term home visitation only describes the mechanism of service delivery; therefore, the design and content of each program can vary significantly. Many home visiting programs include principles from evidence-based models, while not implementing the full model. This is concerning because the efficacy of individual models incorporated is based on the model’s implementation to fidelity. Therefore, more research is needed on home visiting programs that implement previously established, evidence-based treatment models (Sweet & Appelbaum, 2004). In addition, more comprehensive preventive interventions for high-risk families are needed, specifically those that address maternal mental health and the attachment relationship (Duggan, Berlin, Cassidy, Burrell, & Tandon, 2009; Robinson & Emde, 2004).
Researchers have highlighted the importance of continued evaluation of preventive interventions that have been tested in efficacy trials as they are disseminated into increasingly naturalistic conditions in the community through effectiveness trials (Cicchetti & Toth, 2016; Flay et al., 2005; Olds, Sadler, & Kitzman, 2007). BHC is an effectiveness trial as it incorporates multiple evidence-based interventions models that have been proven efficacious into one home visiting model, which is then delivered within existing community infrastructure. Although each intervention component has demonstrated efficacy independently, no study to date has examined the sustained impact of this comprehensive, multi-component intervention program on parenting and child outcomes. A preliminary analysis conducted by Paradis, Sandler, Manly, and Valentine (2013) found that families were actively engaging in BHC services, with an overall retention rate of 85% by age three. Results demonstrated that BHC was effective in connecting families with preventive care, with BHC families completing significantly more well-child visits by 24 months of age, compared to those in the comparison group. An initial screen of this subsample of families found high rates of CPS avoidance across the intervention and comparison groups.
The following two studies extend these preliminary results by evaluating the immediate and long-term effects of BHC on parenting and child functioning. Specifically, Study 1 examines maternal depression as a mechanism in the effects of BHC on parenting and offspring outcomes at post-intervention. Study 2 builds on Study 1 by examining the sustained effects of BHC (3–7 years following post-intervention) on negative and positive parenting practices, as well as child symptomatology and self-regulation, when the child is school-age. We anticipate that this adaptive, multi-component intervention will have immediate and sustained impacts on each of these constructs, in favor of the intervention group.
Study 1: Immediate intervention effects
Methods
Participants
Participants included 232 mothers (aged 15–23; mean age=19.08, SD=1.65; 66.4% African-American, 22.8% Caucasian, 4.7% biracial, 6.0% other race; and 17.8% Latina) with an infant. At Time 1 (baseline), the majority of mothers were not married or living with someone as though married (75.0%) and did not have a high school diploma, or equivalent degree (53.4%). Mean ages of children were as follows: M age at baseline = 5.22 months (SD = 4.24), M age at mid-intervention = 24.74 months (SD= 1.88), and M age at post-treatment = 34.31 months (SD = 3.96). There were approximately equal numbers of male and female children (males: 53.4%).
Procedures
All eligible families receiving care at collaborating pediatric and family medicine practices in Rochester, New York were offered participation in the program. Eligibility criteria included the following: resident of Monroe County, eligible for Temporary Assistance for Needy Families (TANF), mother under 21 years of age at the birth of her first child, a maximum of two children under the age of three, and no previous CPS indication with her child. Exclusionary criteria included severe maternal medical illness, severe maternal psychiatric conditions, IQ less than 70, and/or current incarceration. Families were randomly assigned to the Building Healthy Children intervention (BHC, n=132, 57%), or the Enhanced Community Standard (ECS, n=100, 43.1%).
Research was conducted in accord with the Institutional Review Board approval. Mothers provided informed consent, or if under age 18 and living with their parent, the parent of the adolescent mother signed consent. We had a waiver of consent if the mother was not yet 18 years and did not live with a parent. Assessments were conducted at baseline enrollment (birth to age 1), mid-intervention (child age 2 years), and post-intervention (child age 3 years). All assessments were conducted in the families’ home by trained interviewers who were blind to group assignment. Mothers were provided with monetary compensation for their participation in research visits.
Building Healthy Children (BHC) program
Intervention group.
The BHC intervention is an adaptive multi-component, home visiting program that combines three evidence-based interventions (Parents as Teachers (PAT; Parents as Teachers National Center, 1999), Interpersonal Psychotherapy for Depressed Adolescents (IPT-A; Mufson et al., 2004a), and Child-Parent Psychotherapy (CPP; Lieberman & Van Horn, 2005)) with outreach support. The program is integrated within the child’s medical home through communication via the electronic medical record. Past research has emphasized the importance of this partnership between home visiting programs and pediatricians in strengthening the impact of home visitation (Avellar & Supplee, 2013). Service delivery for the various components of the intervention varies in intensity and is based on family need. All families receive broad-based support via persistent outreach to address concrete needs. All mothers are also offered parenting support through the PAT curriculum. Intervention components that specifically target maternal mental health, trauma, and parent-child attachment (IPT-A and CPP) are more intensive and specialized, and therefore are delivered to families based on individual interest and need.
To ensure that young parents were not overwhelmed by the many services available as part of the BHC intervention, the treatment team established appropriate priorities for intervention components based on data collected and/or maternal report. All participants in the treatment condition were offered outreach services throughout treatment from their outreach worker, and additionally were referred to one or more of the evidence-based interventions. Unless the initial assessments revealed difficulties with maternal depression or the parent-child relationship, the PAT component was initiated first. In cases where the assessment indicated elevated depressive symptomatology, therapists provided IPT-A to mothers. Once IPT-A was completed, families were able to transition to receiving PAT services, or CPP services if warranted. When trauma or difficulties with parent-child attachment were noted and families were identified as needing intensive therapeutic support beyond major depression, they were referred for CPP services. Once CPP was completed, the family was transitioned to PAT services if needed. Although this was the ideal design of the intervention program, as with many effectiveness studies, modifications needed to be made at times based on family need and engagement. For this reason, it was particularly important for clinicians to be cross-trained in the evidence-based models implemented as part of BHC, in order to flexibly deliver the best care to families while maintaining continuity of the therapist.
Outreach.
BHC utilized an outreach worker to address any concrete needs and barriers to healthcare, community services, or program participation. This assistance included but was not limited to: child care needs, housing assistance, emergency assistance, transportation to appointments, and advocacy. They also received support for education and employment goals. Throughout the intervention period mothers had regular and frequent contact with their assigned outreach worker. Initially, services would be more intense (e.g. weekly) until the family’s concrete needs were met. The outreach visits would then become less frequent (e.g. 2x per month) over time as the family became more self-sufficient. The outreach worker would remain with the family throughout the entirety of their participation in the program in order to develop a consistent and supportive relationship with the family.
Each mother was also assigned a clinician who was cross-trained in PAT, IPT-A, and CPP so that they could flexibly meet the needs of the family. At the initiation of treatment, the outreach worker and the mental health clinician conducted a needs assessment with the family to develop an initial service plan. Throughout the program, the outreach worker and clinician worked as a team to meet the needs of the family.
BHC evidence-based intervention components:
Parents as Teachers (PAT; Wagner & Clayton, 1999).
All mothers randomly assigned to BHC were eligible to receive weekly PAT. PAT included parenting education, developmental screening, general health screening, and activities to strengthen child development. Prior research on PAT demonstrates efficacy in improving parent knowledge, attitudes, and behaviors regarding parenting, and improving child social adjustment (Wagner et al., 2002).
Interpersonal Psychotherapy for Depressed Adolescents (IPT-A; Mufson et al., 2004a).
In cases of elevated maternal depressive symptoms, clinicians provided IPT-A in accordance with the manual (Mufson et al., 2004a). There is evidence for the efficacy of IPT-A for the treatment of depression among adolescents (e.g., Mufson et al., 2004b).
Child Parent Psychotherapy (CPP; Lieberman et al., 2015).
In cases of maternal or child traumatic experiences and/or difficulties in the parent-child relationship, CPP was offered. CPP included dyadic psychotherapy sessions, with both mother and child in accordance with the manual (Lieberman et al., 2015). CPP has demonstrated efficacy in improving attachment security and decreasing maternal and child mental health symptoms, (e.g., Lieberman, Ippen, & Van Horn, 2006).
Clinician Training and Fidelity:
Training for the interventions was completed as required by the developers of each intervention and implemented by certified trainers. Masters-level clinicians participated in weekly individual and group supervision to monitor fidelity. Clinicians completed fidelity questionnaires and supervisors reviewed these and audio-taped sessions.
Enhanced Community Standard (ECS).
Participants randomized to the ECS condition received screening and resource information at each assessment point, as deemed necessary. This could range from information on food pantries, housing, or educational opportunities, to community mental health referrals. In addition, if the participant reported any suicidal thoughts, project staff would assist in safety planning.
Measures
Demographic Interview (Cicchetti & Carlson, 1989).
Developed by Cicchetti and Carlson (1989), this measure has been used extensively in research with underprivileged, high-risk families. Information obtained from this measure included: date of birth, gender, race/ethnicity, family composition, parent’s education and current occupation, income, and use of public assistance. This information was collected during the baseline visit.
Childhood Trauma Questionnaire (CTQ; Bernstein et al., 2003).
The CTQ is a 25 item self-report measure assessing child maltreatment with excellent demonstrated psychometric properties (e.g., alphas range from .61–.95; Bernstein et al., 2003). In the present study, the presence of each subtype of maltreatment was calculated using established cut-off criteria (Walker et al., 1999). This measure was administered to mothers during the baseline (T1) visit.
Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996).
The BDI-II is a 21-item, maternal self-report measure of depression severity with good psychometric properties (Beck et al., 1996). At baseline, the mean total BDI-II score at baseline was 9.21 (SD=8.02), with 10.3% of mothers scoring above 19, indicative of clinical significance. This measure was administered to mothers at each time point of this study.
Maternal Efficacy Questionnaire (MEQ; Teti & Gelfand, 1991).
The MEQ is a 10-item questionnaire that assesses a mother’s feelings of self-efficacy. Internal consistency for the MEQ is 0.79–0.86 (Teti & Gelfand, 1991). The MEQ was administered to mothers during T1 and T3 of this study.
Parenting Stress Index (PSI-SF; Abidin, 1990).
The PSI-SF is a 36-item, parent-report measure that assesses mothers’ perception of parenting stress. The PSI-SF has well-established reliability and validity with reliability coefficients of .96 or greater (Abidin, 1990). The PSI-SF was administered to mothers during T1 and T3 of this study.
Child Behavior Checklist (CBCL; Achenbach, 2000).
The CBCL is a widely used, well validated and reliable parent-report instrument to assess child symptomatology (Achenbach, 2000). The CBCL version for 1.5 to 5 year old children (internalizing and externalizing subscales) was used in this study at T3.
Maltreatment Classification System (MCS; Barnett et al., 1993).
Obtained DHS records were independently coded by trained research coders using the the MCS. The MCS comprehensively classifies all forms of maltreatment that occur at the individual and family level. Other investigators have demonstrated that the MCS is reliable and valid way to comprehensively classify child maltreatment (Bolger, Patterson, &Kupersmidt, 1998; Dubowitz et al., 2005; Manly, 2005).
Results
Preliminary results
Table 1 presents the comparisons between the BHC and ECS groups at baseline. Overall, 10.3% of the mothers at baseline scored in the clinically elevated range of depressive symptoms. This did not vary by randomization status. There were more African American mothers in the BHC group compared to the ECS group. Maternal history of childhood maltreatment was prevalent for the mothers, with 56.5% reporting at least one subtype of maltreatment.
Table 1.
Comparison of BHC and ECS families on baseline demographic and study variables
| BHC (n=132) | ECS (n=100) | Statistic test (df) | |||
|---|---|---|---|---|---|
| n | % | n | % | χ2 | |
| Mother: Married | 33 | 25.0% | 25 | 25.0% | χ2 (1)=.00 |
| Mother: African-American | 95 | 72.0% | 59 | 59.0% | χ2 (1)=4.29* |
| Mother: high school diploma or GED | 58 | 43.9% | 50 | 50.0% | χ2 (1)=.84 |
| Mother: history of child maltreatment | 74 | 56.1% | 57 | 57.0% | χ2 (1)=.02 |
| Child: male gender | 75 | 56.8% | 49 | 49.0% | χ2 (1)=1.40 |
| M | SD | M | SD | t-test | |
| Mother: age (years) | 19.16 | 1.76 | 18.98 | 1.50 | t (230) = −.82 |
| Child: age (months) | 5.49 | 4.47 | 4.87 | 3.93 | t (230) = −1.11 |
| Baseline | |||||
| Depressive symptoms | 9.32 | 7.94 | 9.18 | 8.16 | t (230) = −.05 |
| Parenting efficacy | 3.48 | .32 | 3.54 | .26 | t (230) = 1.46 |
| Parenting stress | 1.95 | .46 | 1.94 | .49 | t (230) = −.17 |
Notes. BHC=Building Healthy Children; ECS=Enhanced Community Standard;
p<.05.
Primary analyses
Next, a structural equation model (SEM) was specified as shown in Figure 1. The SEM evidenced good fit to the data (χ2 (32) = 38.10, p=.21, CFI=.99, RMSEA=.03, SRMR=.04; Hu & Bentler, 1999). Mothers in the BHC group reported lower depressive symptoms at T2 compared to mothers in the ECS group. Mothers with fewer childhood maltreatment subtypes reported lower depressive symptoms at T2. Lower maternal depressive symptoms at T2 significantly predicted less child internalizing and externalizing behavior at T3. Lower maternal depressive symptoms at T2 predicted less parenting stress and greater parenting self-efficacy at T3.
Figure 1.
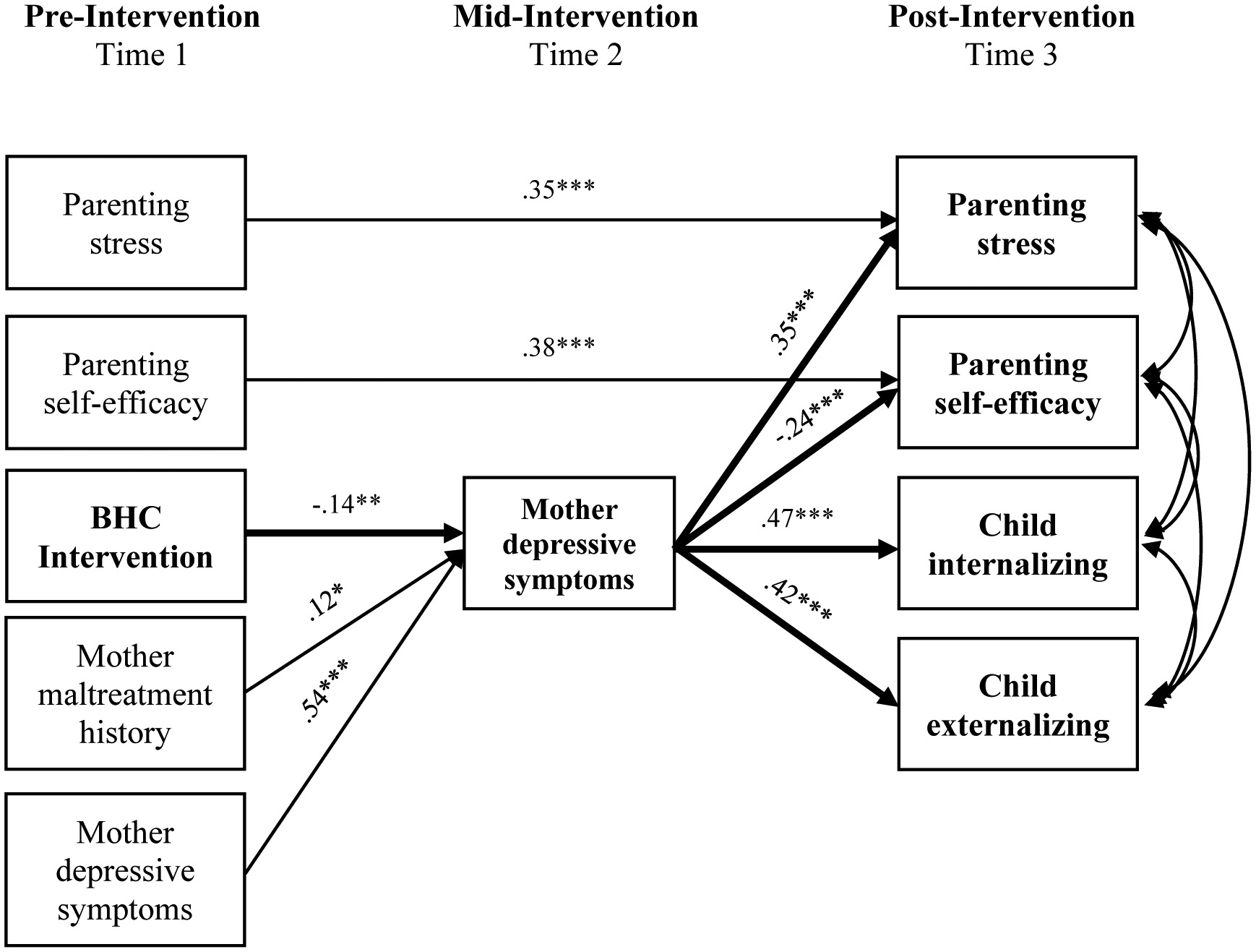
Results of Study 1 SEM
Notes: Standardized parameter estimates are displayed. Only significant paths are depicted. BHC Intervention is coded 0=community standard, 1=BHC. Maternal age and race and child age and gender were included as covariates predicting mother depressive symptoms at mid-intervention. These paths were non-significant and not depicted.*p<.05 **p<.01, ***p<.001.
Indirect effects were tested using 95% asymmetric confidence intervals (RMediation; Tofighi & MacKinnon, 2011). Reductions in maternal depressive symptoms at T2 was a significant mediator in the effect of BHC on the following T3 outcomes: 1) child internalizing symptoms (LCL=−2.727, UCL= −.358), 2) child externalizing symptoms (LCL=−2.517, UCL= −.322), 3) maternal parenting stress (LCL=−.085, UCL=−.01), and 4) maternal parenting self-efficacy (LCL=.004, UCL=.043).
Ad-hoc analyses
Additional analyses were conducted with the subset of families for whom we had access to DHS records (n=180, BHC=95, EC=85). Results indicated a significant difference between BHC and ES families on rates of indicated child maltreatment via CPS record data at post-intervention. Specifically, 10.6% of ES families had an indicated maltreatment incident compared to 3.2% of BHC families (χ2 (1) = 3.98, p=.07).
Study 2: Long-term follow-up
Methods
Participants
A subset of the families who had participated in the BHC program were selected for long-term follow-up. Specifically, families who were still enrolled in the study at the conclusion of the intervention phase (T3), and whose target child was 6–10 years old at the follow-up visit were contacted. School-age was chosen for a number of reasons. Adaptation to the school environment is an important stage-salient developmental task that can either provide buffering to early adversity or set the stage for subsequent challenges, making it an important developmental period to examine. Teachers can also provide an alternative perspective of child functioning. In addition, normative externalizing behavior typically decreases by school entry; therefore, examining children after this developmental period allows for the differentiation between normative and clinically-elevated behavior problems (Hill, Degnan, Calkins, and Keane, 2006).
Project staff recruited families over the phone using a variety of sources for contact information, including information collected during Study 1, as well as, updated contact information through the university medical center’s electronic medical record system. The project coordinator and all research assistants remained blind to intervention status throughout this study. Due to the time lapse between the conclusion of the intervention and recruitment for this study (3–7 years), a number of families were unable to be reached or were uninterested in the study. Overall, 87 families completed the follow-up visit.1 Fifty-nine percent of the sample had been randomly assigned to receive the BHC intervention, while 41% had been randomized to receive Enhanced Community Standard (ECS). At the time of follow-up, maternal age ranged from 22–32 years old (M=27), and child age ranged from 6–10 years old (M=7.5). Child gender was split nearly even (42 girls, 45 boys). The racial and ethnic composition of caregivers and mothers was similar to that of the original sample described in Study 1. Attrition analyses were conducted on the recruitment sample to compare families who completed the follow-up visit versus those that did not. These groups did not differ based on maternal age, race, ethnicity, marital status, education, baseline depression, or intervention status. Nor did they differ based on child gender, age, race, or ethnicity.
In addition, data were collected from the child’s current primary teacher. Teacher data was collected for 69/87 children. Demographic information was not collected from teachers due to the method of data collection (online), and to minimize personal information collected due to the waiver of documentation of consent that was utilized. This waiver was requested in order to minimize barriers to teacher completion.
Procedures
Study 2 included a one-time research visit conducted with the mother. Research was conducted in accord with the Institutional Review Board approval. Mothers signed a new informed consent form specifically for the follow-up study. They met individually with trained research staff in a private interview room. During the follow-up visit a number of questionnaires were completed to assess life stressors, child symptomatology and self-regulation, and parenting practices. At the completion of the visit, mothers received monetary compensation for completing the study. Mothers were also asked to sign a release form for study staff to contact the child’s teacher. With their consent, the child’s teacher was contacted via email to complete questionnaires regarding the child’s functioning in school. Teachers were blind to the child’s intervention condition. Teachers received monetary compensation for their participation.
Measures
Demographic Update Interview- Enhanced.
Demographic Interview (Cicchetti & Carlson, 1989) was amended and re-administered at follow-up. This version of the questionnaire collected the same information as the original version; however, it additionally asked whether certain life stressors had occurred between post-intervention and the follow-up visit. These questions were adapted from the Adverse Childhood Experiences (ACE) questionnaire (Felitti, 1998), and assessed the following domains: parental separation/divorce, substance use, incarceration, loss, homelessness, domestic violence, and community violence.
Conflict Tactics Scales: Parent–Child Version (CTSPC; Straus, Hamby, & Warren, 2003).
The CTSPC consists of 35 items that identify abuse, neglect, and discipline practices in families. The items focus on parent/caregiver behavior towards the child. Mothers rated the frequency an item occurred within the past year on an 8-point Likert scale (0=None to 6=More than 20 times). This measure yielded three subscales of interest to this study: Nonviolent Discipline, Psychological Aggression, and Physical Assault. Straus, Hamby, and Warren’s (2003) recommendations for scoring were followed by summing the midpoints for the response categories chosen by the mother. Higher scores indicate increased frequency of behavior. Internal consistency was acceptable (α > .70) in the current sample for the Nonviolent Discipline and Psychological Aggression subscales. However, the Physical Assault subscale demonstrated unacceptable internal consistency (α = .47), therefore rendering it invalid.
Parenting Practices Interview (Webster-Stratton, 1998).
The PPI is a 73-item parent-report measure assessing positive and negative parenting strategies. This measure yields seven summary scales which assess Appropriate Discipline, Harsh and Inconsistent Discipline, Positive Verbal Discipline, Monitoring, Physical Punishment, Praise and Incentives, and Clear expectations. Two summary scores were created, one for Positive Parenting (Appropriate Discipline, Positive Verbal Discipline, Clear Expectations, Praise and Incentives) and one for Harsh and Inconsistent Parenting (Harsh and Inconsistent Discipline, Physical Punishment). Higher scores indicate increased frequency of the parenting behavior. These two summary scales demonstrated good internal consistency (α > .78).
Behavior Rating Inventory of Executive Functioning, Second edition (BRIEF-2; Gioia, Isquith, Guy, & Kenworthy, 2016).
The BRIEF-2 is an 86-item other-report questionnaire that was completed by caregivers and teachers to assess children’s executive functioning at home and school. Respondents rated the child on a 3-point scale based on the child’s behaviors over the previous 2 months. This measure yields nine non-overlapping clinical scales that form a General Executive Composite score, and three index scores: Behavior Regulation (Inhibition, Self-Monitor), Emotion Regulation (Shift, Emotional Control), and Cognitive Regulation (Initiate, Working Memory, Plan/Organize, Organization of Materials, and Task-Monitor). All three indices demonstrated good internal consistency in this sample (α > .75). This measure produces T-scores for each of the indices which are normed based on age and gender. Higher scores indicate greater difficulty with regulation (referred to as dysregulation in this paper) in that domain.
Emotion Regulation Checklist (ERC; Shields & Cicchetti, 1997).
The ERC is a 24-item other-report measure, which targets processes central to emotionality and regulation, including affective lability, intensity, valence, flexibility, and situational appropriateness of emotional expression (Shields & Cicchetti, 1998). Caregivers and teachers rated children on a 4-point Likert scale as to how characteristic each item is of the child. Two subscales were derived from this data. The first, Lability/Negativity, assesses for mood swings, angry reactivity, emotional intensity, and dysregulated positive emotions. The second, Emotion Regulation, assess for processes central to adaptive regulation, including equanimity, emotion understanding, and empathy (Shields & Cicchetti, 1997). The Lability/Negativity subscale demonstrated good internal consistency amongst caregivers and teachers (α= .87–.93). The Emotion Regulation subscale demonstrated questionable internal consistency amongst caregiver data (α= .67) but good internal consistency for teacher data (α= .85).
Child Behavior Checklist/Teacher Report Form 6–18 (CBCL/TRF; Achenbach & Rescorla, 2001).
This measure is the same as that used in Study 1; however, the 6–18 year old version was utilized for both caregivers and teachers. These are widely-used, well validated and reliable measures (Achenbach, 2001). For the purpose of this study, the T-scores for the internalizing and externalizing behavior dimensions were analyzed, which are normed based on age and gender. Higher scores indicate greater difficulty in these domains.
Results
Preliminary Analyses
To assess for comparability on baseline characteristics between intervention and ECS families, comparisons were made on a number of maternal (age, race, ethnicity, education, and marital status) and child (age, gender, race, ethnicity) demographic variables using chi-square and t-test analyses. Groups did not differ based on maternal or child factors at follow-up. In addition, groups were compared on presence of adverse life events between conclusion of the intervention and the follow-up visit. Groups did not differ based on the presence or absence of these events. It is notable that the sample experienced high rates of adverse life events overall during this period. Based on maternal report, 67% of families experienced the death of someone close to them, 15% experienced homelessness, and 12% had been evicted. 35% and 16% of families or someone close to them had experienced incarceration or had difficulty with substance use. 21% of mothers were the victim of domestic violence, 12% were victims of or witnessed community violence, and 24% separated or divorced from their partner.
Preliminary analyses were conducted to determine the appropriateness of covariate inclusion. Child gender and age were not significantly predictive of any outcome variables. However, child gender was marginally predictive (p=.07) of parental psychological aggression; therefore, this was included as a statistical control in the regression model.
Primary analyses
Mothers in the BHC group reported using significantly less harsh and inconsistent parenting at follow-up (M=3.73) compared to mothers in the ECS group (M=4.36), t(83)= 2.948, p=.004. In addition, intervention status was a marginally significant predictor of psychological aggression. The overall model was significant, F(2,82)= 4.077, p=.021. Above and beyond the effect of child gender, BHC mothers reported using marginally less psychological aggression towards their children at follow-up (M=12.98) compared to ECS mothers (M=21.03), b= −.202, p = .059. There were no significant effects of the intervention on positive parenting or non-violent discipline.
In order to assess the impact of BHC on child outcomes, both parent and teacher data were analyzed. According to parent report (Table 2), results indicated that children in the BHC group had fewer externalizing (t(58.68)= 2.219, p=.030) and internalizing (t(85)= 2.048, p=.044) problems at follow-up than those in the comparison group. Additional analyses were conducted to examine the effect of the intervention on these two outcomes, while controlling for their post-intervention (T3) values. The pattern and significance of these results remained the same. ECS children’s externalizing behavior fell in the Clinically Significant range (T-score ≥ 64) at a significantly higher rate (36%) than BHC children (12%), χ2 (1)=8.90, p=.003. This result was marginally significant for internalizing behavior, χ2 (1)=3.670, p=.055.
Table 2.
Intervention Effects on Main Outcome Variables – parent report
| Parent Data | BHC Mean (SD) | ECS Mean (SD) | Test Statistic | P Value |
|---|---|---|---|---|
| Parenting Outcomes | ||||
| Positive Parenting | 19.61 (2.42) | 19.75 (2.52) | t(83)= .251 | .803 |
| HI Parenting | 3.73 (0.88) | 4.36 (1.07) | t(83)= 2.948 | .004** |
| Non-violent Discipline | 43.14 (27.74) | 47.09 (31.92) | t(82)= .603 | .548 |
| Psychological Aggression | 12.98 (15.70) | 21.03 (20.84) | F(2,82)= 3.671 | .059† |
| Child Outcomes | ||||
| Externalizing Behavior | 51.06 (9.95) | 57.14 (14.15) | t(58.68)= 2.219 | .030* |
| Internalizing Behavior | 48.98 (10.15) | 53.72 (11.30) | t(85)= 2.048 | .044* |
| Global Executive Function | 50.51 (10.06) | 55.42 (13.52) | t(61.14)= 1.847 | .070† |
| Behavior Dysregulation | 51.00 (10.67) | 54.86 (14.92) | t(85)= 1.331 | .188 |
| Emotion Dysregulation | 50.02 (9.48) | 56.72 (14.31) | t(56.28)= 2.456 | .017* |
| Cognitive Dysregulation | 49.53 (10.14) | 53.14 (11.70) | t(85)= 1.534 | .129 |
| Negativity/Lability | 27.02 (6.19) | 29.86 (9.77) | t(54.56)= 1.540 | .129 |
| Emotion Regulation | 27.14 (3.06) | 27.69 (3.81) | t(85)= .756 | .452 |
Notes. HI Parenting = Harsh & Inconsistent Parenting. An F statistic is reported for Psychological Aggression due to the inclusion of gender in a regression model to control for the effect of this covariate.
p < .01,
p <.05,
p <.10.
In terms of self-regulation, parents reported that children in the BHC group exhibited marginally significantly less difficulties with self-regulation at follow-up, as measured by the Global Executive Composite of the BRIEF-2, t(61.14)= 1.847, p=.070. Specifically, BHC children exhibited significantly less emotion regulation difficulties than those in the comparison group t(56.28)= 2.456, p=.017. There were no significant group differences on measures of behavior and cognitive dysregulation. Results indicated that ECS children’s emotion dysregulation fell in the Potentially Clinically Elevated/Clinically Elevated range (T score ≥ 65) at a significantly higher rate (28%) than BHC children (8%), χ2 (1)=6.211, p=.013. This result was marginally significant for global executive functioning, χ2 (1)=3.605, p=.058. There were also no significant differences between groups on the two subscales of the ERC, including negativity/lability and emotion regulation ability.
As exhibited in Table 3, results from teacher report echo many of the parent report findings. According to teachers, BHC children had fewer externalizing (t(67)=2.015, p=.048) problems at follow-up than those in the comparison group (ECS). ECS children’s externalizing behavior fell in the Clinically Significant range at a marginally, significantly higher rate (39%) than BHC children (24%), χ2 (1)=3.793, p=.051. However, no significant group difference in internalizing behavior was found. Children in the BHC group exhibited marginally, significantly less difficulties with self-regulation, across measures of global executive composite (t(67)= 1.867, p=.066), behavior dysregulation (t(67)= 1.792, p= .078), and emotion dysregulation (t(67)= 1.845, p= .070). ECS children’s global executive functioning fell in the Potentially Clinically Elevated/Clinically Elevated range at a significantly higher rate (42%) than BHC children (26%), χ2 (1)=4.126, p=.042. ECS children’s emotion dysregulation also fell in the Potentially Clinically Elevated/Clinically Elevated range at a significantly higher rate (44%) than BHC children (28%), χ2 (1)=4.495, p=.034. There was no significant difference in clinical significance rates for behavior dysregulation. In addition, there were no significant differences on the cognitive dysregulation subscale of the BRIEF-2, or the two subscales of the ERC, including negativity/lability and emotion regulation ability.
Table 3.
Intervention Effects on Main Outcome Variables – teacher report
| Teacher Data | BHC Mean (SD) | ECS Mean (SD) | Test Statistic | P Value |
|---|---|---|---|---|
| Externalizing Behavior | 59.10 (9.80) | 64.37 (11.78) | t(67)=2.015 | .048* |
| Internalizing Behavior | 53.17 (11.31) | 56.44 (10.18) | t(67)=1.220 | .227 |
| Global Executive Functioning | 59.81 (12.64) | 65.67 (12.83) | t(67)= 1.867 | .066† |
| Behavior Dysregulation | 58.71 (11.88) | 64.37 (14.11) | t(67)= 1.792 | .078† |
| Emotion Dysregulation | 59.24 (15.27) | 66.30 (15.88) | t(67)= 1.845 | .070t |
| Cognitive Dysregulation | 58.00 (11.95) | 62.56 (11.48) | t(67)= 1.569 | .121 |
| Negativity/Lability | 27.98 (9.40) | 31.33 (9.42) | t(67)= 1.447 | .152 |
| Emotion Regulation | 23.40 (4.57) | 23.67 (4.62) | t(67)= .231 | .818 |
Notes.
p < .01,
p <.05,
p <.10
Discussion
Recognizing that no single approach can meet the multi-dimensional needs of impoverished, high-risk families, the Building Healthy Children preventive intervention was designed to provide concrete support and evidence-based intervention to young mothers and their infants who are at heightened risk for child maltreatment and poor developmental outcomes. BHC supports these families by flexibly delivering three evidence-based treatment models in conjunction with outreach support. The studies presented above utilize a longitudinal mixed-method, multi-informant design to evaluate the immediate and long-term effectiveness of this program on parenting and child functioning.
Impact on parenting
Results from both Study 1 and Study 2 indicate that BHC had significant short and long-term effects on parenting. Although Study 1 did not reveal a direct effect of the intervention on parenting attitudes at child age 3, mothers who participated in BHC experienced reductions in depressive symptoms at mid-intervention, when their children were 2 years old. This alleviation of maternal depressive symptoms predicted positive benefits for parenting stress and self-efficacy when the children were 3 years old. Alleviating mothers’ depressive symptoms represents a mechanism of the effects of BHC on family wellbeing, highlighting the criticality of addressing the mental health needs of young mothers. This is consistent with research demonstrating that remission of maternal depressive symptoms fosters positive outcomes for children and families (e.g., Cuijpers, Weitz, Karyotaki, Garber, & Andersson, 2015).
Importantly, using Child Protective Service record data, findings provide preliminary support that this adaptive home visiting program is effective at preventing child maltreatment. Given the detrimental, long-term effects that maltreatment can have on a child and family, these results suggest that BHC, a tailored evidence-based prevention model delivered in home, in combination with a community health worker, may prevent child maltreatment.
Although data on CPS avoidance was not available for Study 2, results from this study demonstrate the sustained positive benefits of BHC on the family environment into the school-aged years. Mothers who participated in the BHC intervention exhibited significantly less harsh and inconsistent parenting (including harsh and inconsistent discipline and physical punishment) toward their child at follow-up, compared to those that did not. Although harsh parenting (including corporal punishment) does not necessarily equate to child maltreatment, previous literature has found that it is related to child abuse potential (Rodriguez, 2010). Not surprisingly, abusive parents typically administer excessively harsh discipline (Veltkamp & Miller, 1994). In addition, harsh parenting is similarly associated with many of the same adverse outcomes as child maltreatment, including externalizing behavior problems. In fact, harsh parenting is one of the strongest correlates for childhood aggression and disruptive behavior (Erath, El‐Sheikh, & Mark Cummings, 2009; Gershoff, 2002).
In addition, there was a marginally significant effect of the intervention on psychological aggression, in favor of the intervention group. In Study 2, psychological aggression was defined as “verbal and symbolic acts by the parent intended to cause psychological pain or fear on the part of the child (e.g. threatening to hit your child, or send them away) (Straus & Field, 2003). This construct would most likely be subsumed under the more comprehensive construct of psychological maltreatment (also referred to as mental, emotional, or psychological abuse and neglect) (Binggeli, Hart, & Brassard, 2001; APSAC Taskforce, 2019). Psychological aggression has been significantly associated with greater child abuse potential (Rodriguez, 2010). It has also been linked to a number of detrimental outcomes in childhood and beyond (Liu & Wang, 2015; Straus & Field, 2003). In fact, one study found that when considering physical abuse, corporal punishment and psychological aggression simultaneously, psychological aggression emerged as the strongest predictor of negative psychological outcomes (Miller-Perrin, Perrin, & Kocur, 2009). Findings from a large, nationally representative study revealed a robust association between psychological maltreatment and a wide range of clinician-rated diagnostic symptoms and risk indicators in adolescence (e.g. depression, anxiety, self-injurious behavior, behavior problems, academic problems). This study found that psychological maltreatment was as, if not more, potent of a predictor for childhood maladjustment as sexual abuse, physical abuse, and the combination of the two, across a range of outcomes (Spinazzola et al., 2014). Despite the prevalence and clear detriment of psychological maltreatment, it is often not a target of intervention (Hart & Brassard, 1987; Spinazzola et al., 2014). The results of this study, while only marginally significant, suggest the effectiveness of a comprehensive home visiting program in preventing the use of this detrimental parenting practice.
Taken together, the results from Study 1 and 2 demonstrate the effectiveness of BHC at promoting positive parenting and maternal mental health and preventing child maltreatment and harsh parenting. In addition, the findings highlight the ability of home visiting programs to foster maternal self-efficacy and decrease parenting stress- two important predictors of positive parent and child outcomes. Overall, these findings suggest that an adaptive, evidence-based multi-component home visiting program that addresses concrete needs as well as parenting and maternal psychopathology, is effective in fostering positive parenting attitudes and preventing the use of negative parenting strategies.
Impact on child functioning
In addition, results from Study 1 and 2 both indicate that the BHC intervention has a sustained impact on child functioning. BHC was found to initiate a cascade of positive adaption throughout the family, beginning with the reduction in maternal depressive symptoms, which then led to improvements in child mental health by age 3. Furthermore, results of Study 2 demonstrate the sustained benefit into school age. Specifically, children who received the BHC intervention in infancy and early childhood exhibited significantly less internalizing and externalizing behavior problems in elementary school, as rated by their caregiver. In addition, teachers also reported that these children exhibited significant less externalizing behavior than their peers. Finding from Study 2 also revealed marginally significant to significant intervention effects across different domains of self-regulation, in favor of the intervention group. These results were echoed by both parents and teachers.
According to parents, intervention children exhibited significantly less difficulty with emotion regulation, compared to the ECS group. However, this effect was only evident in one measure (BRIEF-2) and not the other (ERC). This may be due to the fact that while these two measures are significantly correlated and do overlap, they are ultimately tapping different capabilities. One measures emotion regulation through the lens of executive function (BRIEF-2), while the other measures emotion dysregulation more broadly, including aspects of lability and negativity (ERC). Therefore, it is clear that while on the surface these two constructs look highly similar, they differ conceptually.
Examining the intervention effects on child externalizing behavior and dysregulation, we see that parent and teachers’ report of these difficulties were more likely to fall in the Clinically Significant/Elevated or Potentially Clinically Elevated range for children in the ECS condition across a number of constructs, while those in the intervention group were more likely to fall within the normative range. In addition, teachers’ reports of these difficulties were often rated more problematic than parents’ reports. While the pattern of results was the same across parents and teachers, and parent and teacher data was significantly correlated, it may be that children’s externalizing behavior and difficulties with self-regulation are more disruptive and therefore more noticeable in the school setting. Additionally, parents may be biased in reporting their own child’s behavior.
In addition, it should be noted that for some of the subscales of the CBCL/TRF and the BRIEF-2, the standard deviations of the T-scores were slightly larger than expected (greater than 10). The large standard deviations indicate that the scores on some of these subscales varied greatly among study families, according to both parent and teacher data. In addition, large standard deviations can make it more difficult to detect a significant effect, particularly in smaller samples.
Overall, the findings from Study 1 and Study 2 highlight the positive and sustained effect of BHC on child functioning. Children who were enrolled in the BHC intervention during infancy and early childhood exhibited significantly less internalizing and externalizing behavior at age three, and several years later during elementary school. This powerful preventative effect is further highlighted by the significant life stressors that many of these children experienced between post-intervention and follow-up. Despite the fact that these stressors are often associated with internalizing and externalizing behavior problems and difficulties with self-regulation, those that received the BHC intervention continued to function in the normative range compared to their same-age and same-gender peers.
These results can be further understood through an ecological theory lens (Bronfenbrenner, 1994). Even though a majority of the intervention contact was with mothers (for some families all of the contact), we see a ripple effect on other people within the family system- the child. As advocated by Zigler throughout his career, these findings emphasize the importance of fostering healthy family functioning to promote resilience among disadvantaged children (Luthar & Zigler, 1991). One way to do so is by providing concreate support and access to mental health services for caregivers, as modeled by the BHC program. Our findings support a recent consensus by experts that one of the best ways to promote wellbeing among at-risk children is to address the wellbeing of the caregiver (Luthar & Eisenberg, 2017).
Strengths and limitations
Both studies are characterized by several notable strengths. Overall, these findings were derived from a multi-informant, multi-method longitudinal design. Due to its design, we were able to capture the temporal precedence necessary to examine prevention effects and potential mechanisms of change. Having official CPS records of child maltreatment and both parent and teacher report of child behavior also strengthened the results of this study. In addition, Study 2 provides a long-term follow-up of a prevention program, which is quite rare in the literature. Researchers and policy makers alike have emphasized the importance of longer-term follow-up studies in order to examine sustainability of program effects and the prevention of psychological disorders (Gillham, Shatté, & Reivich, 2001; Kellam & Langevin, 2003). Examining child functioning across a span of multiple years allows us to better differentiate normative developmental fluctuations (e.g. externalizing behavior during preschool years; Hill, Degnan, Calkins, & Keane, 2006) from more long-term, sustained behavior problems.
Additionally, the samples from these two studies are representative of minority populations (African American, Hispanic/Latinx) in Rochester and across the country. This is especially important since these groups have typically been underrepresented in intervention evaluations. This makes these results generalizable to other similar, underrepresented populations. While there is often stigma surrounding mental health and service utilization within these populations, BHC’s flexible delivery approach helps to reduce this stigma. By recruiting families from their established medical home and by delivering services in their physical homes, tailored to their individual interests and needs, BHC’s model of service delivery actively works to reduce the stigma associated with traditional outpatient service delivery and partner with parents and children to support healthy development.
A main strength of the BHC intervention is the flexible design and real-world application. Researchers have stressed the importance of continued evaluation of preventive interventions along the continuum from efficacy trials to effectiveness studies, in order to better understand the utility of our interventions in the real world (Cicchetti & Toth, 2016; Flay et al., 2005; Olds, Sadler, et al., 2007; Weisz & Jensen, 1999). The BHC home visitation program was specifically developed with this in mind, balancing fidelity to evidence-based models (PAT, IPT-A, CPP) with adaptation to the demands of widespread community implementation and individual family need. Home visitation has been described as a “desperately needed public health approach to prevent the intergenerational transfer of toxic stress and disparities in health, education, and economic productivity” (Garner, 2013, pp. S71). Similar to other home-visiting programs, BHC addresses the concrete needs of the family, supports connections with medical providers, and fosters positive child development. However, what differentiates BHC is that it also addresses the relational and mental health needs of the mothers and their infants. By offering not only parent skills training, but also an attachment-based intervention and a depression treatment, BHC provides an adaptive model of home-based preventive intervention. Our findings suggest that this comprehensive and flexible approach leads to widespread benefits.
This approach is also aligned with the burgeoning field of precision medicine. As Supplee and Duggan (2019) highlight, precision public health uses this approach on a larger scale to match communities’ specific needs with the most efficient and cost-effective investment. Doing so means offering those with less risk factors less intensive (and less costly) interventions, and those at higher risk more intensive (and more costly) interventions. Recently, the field of prevention science has supported the precision approach, calling for interventions that are more tailored to specific client needs (August & Gewirtz, 2019). As part of this call, the field of home visiting has begun actively conducting research on precision home visiting (e.g. Home Visiting Applied Research Collaborative).
Although these studies have several notable strengths, it is important to acknowledge their limitations as well. Across both studies, many of the parenting constructs were measured using maternal report. While self-report is the most widely available and feasible option, responses may be biased due to social desirability and fear of repercussions. Substituting or supplementing self-report measures with behavioral observation and/or official records would be advantageous. We found preliminary evidence of the effectiveness of BHC at reducing child maltreatment incidents with the subsample of families for whom CPS records were available. Although these results are promising, access to records for the entire sample at post-intervention and follow-up will be necessary to substantiate these findings. Another limitation to consider is sample bias. Given the length of time between the intervention period and the follow-up visit (3–7 years) and the transience of this population, we only recruited families that were still enrolled at the conclusion of the intervention (T3). While this improved recruitment feasibility, it does introduce potential bias, which is important to consider when thinking about the generalizability of these results.
Finally, our findings speak to the impact of the BHC intervention as an entire intervention package. There was natural variability not only in which of the evidence-based interventions mothers received, but also the dosage, sequencing and timing. Future research utilizing novel designs such as Sequential, Multiple Assignment, Randomized Trial (SMART; Lei, Nahum-Shani, Oslin, & Murphy, 2012) would be useful to determine the optimal sequencing of intervention components and effective treatment pathways tailored to individual needs.
Conclusion
In conclusion, these studies demonstrate the short and long-term effectiveness of a multi-component preventive intervention that offers outreach support and a menu of evidence-based models tailored to the individual needs of high-risk young families. When delivered during infancy and early childhood, this program is effective at preventing negative parenting practices, while fostering parental self-efficacy and reducing parenting stress. It also shows promise at preventing child maltreatment. In addition, BHC has a sustained and favorable effect on child functioning in early and middle childhood. These findings highlight the importance of an adaptive model of home visiting that flexibly addresses the complex needs of these young families, by supporting maternal mental health, mother-child attachment, parenting skills, and families’ basic needs.
Due to the stigma towards mental health and the social and economic burdens many of these families face, it is likely that many of these problematic parent and child behaviors would not have been identified until school-age or later. Rather than waiting for problems to develop, BHC utilized a preventative approach by reaching a non-treatment seeking population within their medical home and providing a flexible, evidence-based approach to service delivery. BHC moves us away from a “one size fits all” approach to intervention and towards a better understanding of “what works for whom and why (Roth & Fonagy, 2013),” in order to increase efficiency and cost-effectiveness for families, providers, and community stakeholders.
While BHC may at first require more training, time, and resources than treatment as usual (Shonkoff & Fisher, 2013; Toth & Manly, 2011), the preventive effects demonstrated above can ultimately decrease the economic burden and associated negative outcomes (e.g. child maltreatment, mental illness). Policies that increase access to more efficacious intervention programs for impoverished and minority youth may also help to decrease future health disparities often evident in these populations; thereby improving the lives of children in the long-term (Chen, Martin, & Matthews, 2006). Edward Zigler was a champion of evidence-based prevention efforts for disadvantaged young children and families – supporting programs such as these is one way to carry on his legacy.
Acknowledgments
We are grateful to the Monroe County Department of Human Services, the United Way of Greater Rochester, Administration of Children and Families (90CA1772/01), the Society for Research in Child Development, and the American Psychological Association Division 29 for their support of this work.
Footnotes
Conflicts of Interest: None
85 of the participants were the child’s biological mother who also participated in the intervention. The 2 other participants were alternative primary caregivers (1 father and 1 grandmother). Alternative caregivers completed all measures except for the parenting questionnaires. Because they did not participate in the intervention, we did not expect their parenting practices to be impacted. Hereinafter, all caregivers will be referred to as mothers for clarity and consistency.
References
- Abidin RR (1990). Parenting stress index-short form: Pediatric Psychology Press; Charlottesville, VA. 10.1037/t02445-000 [DOI] [Google Scholar]
- Achenbach TM, & Rescorla LA (2000). Manual for the ASEBA preschool forms & profiles: An integrated system of multi-informant assessment; Child behavior checklist for ages 1 1/2–5; Language development survey; Caregiver-teacher report form: Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms & profiles: an integrated system of multi-informant assessment Burlington, VT: University of Vermont. Research Center for Children, Youth, & Families. [Google Scholar]
- Taskforce APSAC (2019). The investigation and determination of suspected psychological maltreatment in children and adolescents. The American Professional Society on the Abuseof Children (APSAC). Retrieved from https://www.apsac.org/guidelines. [Google Scholar]
- August GJ, & Gewirtz A (2019). Moving toward a precision-based, personalized framework for prevention science: Introduction to the special issue. Prevention Science, 20(1), 1–9. 10.1007/s11121-018-0955-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avellar SA, & Supplee LH (2013). Effectiveness of home visiting in improving child health and reducing child maltreatment. Pediatrics, 132(Supplement 2), S90–S99. 10.1542/peds.2013-1021g [DOI] [PubMed] [Google Scholar]
- Barnett D, Manly JT, & Cicchetti D (1993). Defining child maltreatment: The interface between policy and research. Child Abuse, Child Development, and Social Policy,8,7–73. 10.1017/cbo9780511665707.014 [DOI] [Google Scholar]
- Beauchaine T & Cicchetti D (2019). Emotion Dysregulation and Emerging Psychopathology: A transdiagnostic, transdisciplinary perspective. Development and Psychopathology. 31(3). 799–804. 10.1017/s0954579419000671 [DOI] [PubMed] [Google Scholar]
- Beeber LS, Schwartz TA, Holditch-Davis D, Canuso R, Lewis V, & Hall HW (2013). Parenting enhancement, interpersonal psychotherapy to reduce depression in low-income mothers of infants and toddlers: A randomized trial. Nursing Research, 62(2), 82. 10.1097/nnr.0b013e31828324c2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory-II (BDI-II). San Antonio, TX: Psychological Corporation. 10.1037/t00742-000 [DOI] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … & Zule W (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse & Neglect, 27(2), 169–190. 10.1016/s0145-2134(02)00541-0 [DOI] [PubMed] [Google Scholar]
- Binggeli NJ, Hart SN, & Brassard MR (2001). Psychological maltreatment of children: Sage. [Google Scholar]
- Bronfenbrenner U (1994). Ecological models of human development. Readings on the Development of Children, 2(1), 37–43. [Google Scholar]
- Centers for Disease Control and Prevention. (2014). Child maltreatment: Facts at a glance. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- Centers for Disease Control and Prevention. (2017). About Teen Pregnancy. Retrieved from https://www.cdc.gov/teenpregnancy/about/. [Google Scholar]
- Chen E, Martin AD, & Matthews KA (2006). Understanding health disparities: the role of race and socioeconomic statusin children’s health. American Journal of Public Health, 96(4), 702–708. 10.2105/ajph.2004.048124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D (1984). The emergence of developmental psychopathology. Child Development,1–7. 10.2307/1129830 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Carlson V (1989). Child maltreatment: Theory and research on the causes and consequences of child abuse and neglect: Cambridge University Press. 10.1017/cbo9780511665707 [DOI] [Google Scholar]
- Cicchetti D, & Toth SL (1995). A developmental psychopathology perspective on child abuse and neglect. Journal of the American Academy of Child & Adolescent Psychiatry, 34(5), 541–565. 10.1097/00004583-199505000-00008 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2005). Child maltreatment. Annual Review of Clinical Psychology, 1, 409–438. 10.1146/annurev.clinpsy.1.102803.144029 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2016). Child maltreatment and developmental psychopathology: A multilevel perspective. Developmental Psychopathology, Maladaptation and Psychopathology, 3, 457. 10.1002/9781119125556.devpsy311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, & Toth SL (2006). Fostering secure attachment in infants in maltreating families through preventive interventions. Development and Psychopathology, 18(03), 623–649. 10.1017/s0954579406060329 [DOI] [PubMed] [Google Scholar]
- Cole PM, Hall SE, & Hajal N (2017). Emotion dysregulation as a vulnerability to psychopathology. In Beauchaine TP& Hinshaw SP (Eds.), Child and adolescent psychopathology (3rd ed., pp. 346–386). Hoboken, NJ: Wiley. [Google Scholar]
- Cowell RA, Cicchetti D, Rogosch FA, & Toth SL (2015). Childhood maltreatment and its effect on neurocognitive functioning: Timing and chronicity matter. Development and Psychopathology, 27(2), 521–533. 10.1017/s0954579415000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Weitz E, Karyotaki E, Garber J, & Andersson G (2015). The effects of psychological treatment of maternal depression on children and parental functioning: a meta-analysis. European Child & Adolescent Psychiatry, 24(2), 237–245. 10.1007/s00787-014-0660-6 [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K, Ivy L, & Petrill SA (2006). Maternal warmth moderates the link between physical punishment and child externalizing problems: A parent-offspring behavior genetic analysis. Parenting: Science and Practice, 6(1), 59–78. 10.1207/s15327922par0601_3 [DOI] [Google Scholar]
- DeKlyen M, & Greenberg MT (2008). Attachment and psychopathology in childhood. Handbook of attachment: Theory, research, and clinical applications, 2, 637–665. [Google Scholar]
- Demeusy E, Rogosch F, Cicchetti D, Toth S (2018, November). The effect of maternal history of childhood maltreatment on future parenting and child behavior. Poster presented at the International Society for Traumatic Stress Studies 34th Annual Meeting, Washington, DC. [Google Scholar]
- Dixon L, Browne K, & Hamilton‐Giachritsis C (2005). Risk factors of parents abused as children: a mediational analysis of the intergenerational continuity of child maltreatment (Part I). Journal of Child Psychology and Psychiatry, 46(1), 47–57. 10.1111/j.1469-7610.2004.00339.x [DOI] [PubMed] [Google Scholar]
- Drotar D, Robinson J, Jeavons L, & Lester Kirchner H (2009). A randomized, controlled evaluation of early intervention: The Born to Learn curriculum. Child: Care, Health and Development, 35(5), 643–649. 10.1111/j.1365-2214.2008.00915.x [DOI] [PubMed] [Google Scholar]
- Duberstein PR, Ward EA, Chaudron LH, He H, Toth SL, Wang W, … & Talbot NL, (2018). Effectiveness of interpersonal psychotherapy-trauma for depressed women with childhood abuse histories. Journal of Consulting and Clinical Psychology, 86(10), 868. 10.1037/ccp0000335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan AK, Berlin LJ, Cassidy J, Burrell L, & Tandon SD (2009). Examining maternal depression and attachment insecurity as moderators of the impacts of home visiting for at-risk mothers and infants. Journal of Consulting and Clinical Psychology, 77(4), 788. 10.1037/a0015709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckenrode J, Ganzel B, Henderson CR Jr, Smith E, Olds DL, Powers J, … Sidora K (2000). Preventing child abuse and neglect with a program of nurse home visitation: The limiting effects of domestic violence. Jama, 284(11), 1385–1391. 10.1001/jama.284.11.1385 [DOI] [PubMed] [Google Scholar]
- Erath SA, El‐Sheikh M, & Mark Cummings E (2009). Harsh parenting and child externalizing behavior: Skin conductance level reactivity as a moderator. Child Development, 80(2), 578–592. 10.1111/j.1467-8624.2009.01280.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Marks JS . (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2013). Violence, crime, and abuse exposure in a national sample of children and youth: an update. JAMA Pediatrics, 167(7), 614–621. 10.1001/jamapediatrics.2013.42 [DOI] [PubMed] [Google Scholar]
- Flaherty SC, & Sadler LS (2011). A review of attachment theory in the context of adolescent parenting. Journal of Pediatric Health Care, 25(2), 114–121. 10.1016/j.pedhc.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flay BR, Biglan A, Boruch RF, Castro FG, Gottfredson D, Kellam S, … Ji P (2005). Standards of evidence: Criteria for efficacy, effectiveness and dissemination. Prevention Science, 6(3), 151–175. 10.1007/s11121-005-5553-y [DOI] [PubMed] [Google Scholar]
- Furstenberg FF Jr, Levine JA, & Brooks-Gunn J (1990). The children of teenage mothers: patterns of early childbearing in two generations. Family Planning Perspectives, 54–61. 10.2307/2135509 [DOI] [PubMed] [Google Scholar]
- Garner AS (2013). Home visiting and the biology of toxic stress: opportunities to address early childhood adversity. Pediatrics, 132(Supplement 2), S65–S73. 10.1542/peds.2013-1021d [DOI] [PubMed] [Google Scholar]
- Gershoff ET (2002). Corporal punishment by parents and associated child behaviors and experiences: a meta-analytic and theoretical review. Psychological Bulletin, 128(4), 539. 10.1037/0033-2909.128.4.539 [DOI] [PubMed] [Google Scholar]
- Gillham JE, Shatté AJ, & Reivich K (2001). Needed for prevention research: Long-term follow up and the Evaluation of mediators, moderators, and lay providers. Prevention & Treatment, 4(1), Article 9c. 10.1037/1522-3736.4.1.49c [DOI] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, & Kenworthy L (2016). Behavior rating inventory of executive function, (BRIEF-2): Lutz, FL: Psychological Assessment Resource. 10.4324/9781003076391-76 [DOI] [Google Scholar]
- Gioia GA, Isquith PK, Retzlaff PD, & Espy KA (2002). Confirmatory factor analysis of the Behavior Rating Inventory of Executive Function (BRIEF) in a clinical sample. Child Neuropsychology, 8(4), 249–257. 10.1076/chin.8.4.249.13513 [DOI] [PubMed] [Google Scholar]
- Halfon N, Berkowitz G, & Klee L (1992). Mental health service utilization by children in foster care in California. Pediatrics, 89(6), 1238–1244. [PubMed] [Google Scholar]
- Hammen C, & Brennan PA (2003). Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry, 60(3), 253–258. 10.1001/archpsyc.60.3.253 [DOI] [PubMed] [Google Scholar]
- Handley ED, Michl-Petzing LC, Rogosch FA, Cicchetti D, & Toth SL (2017). Developmental cascade effects of interpersonal psychotherapy for depressed mothers: Longitudinal associations with toddler attachment, temperament, and maternal parenting efficacy. Development and Psychopathology, 29(2), 601–615. 10.1017/s0954579417000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden KP, Lynch SK, Turkheimer E, Emery RE, D’onofrio BM, Slutske WS, … & Martin NG, (2007). A behavior genetic investigation of adolescent motherhood and offspring mental health problems. Journal of Abnormal Psychology, 116(4), 667. 10.1037/0021-843x.116.4.667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart SN, & Brassard MR (1987). A major threat to children’s mental health: Psychological maltreatment. American Psychologist, 42(2), 160. 10.1037/0003-066x.42.2.160 [DOI] [PubMed] [Google Scholar]
- Hill A, Degnan KA, Calkins SD, & Keane SP (2006). Profiles of externalizing behavior problems for boys and girls across preschool: the roles of emotion regulation and inattention. Developmental Psychology, 42(5), 913. 10.1037/0012-1649.42.5.913 [DOI] [PubMed] [Google Scholar]
- Hodgkinson S, Beers L, Southammakosane C, & Lewin A (2014). Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics, peds-2013. 10.1542/peds.2013-0927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JL, Garber J, Ciesla JA, Young JF, & Mufson L (2007). Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs. Journal of Consulting and Clinical Psychology, 75(5), 693. 10.1037/0022-006x.75.5.693 [DOI] [PubMed] [Google Scholar]
- Horton C (2003). Protective factors literature review: Early care and education programs and the prevention of child abuse and neglect: Center for the Study of Social Policy. [Google Scholar]
- Howard KS, & Brooks-Gunn J (2009). The role of home-visiting programs in preventing child abuse and neglect. The Future of Children, 19(2), 119–146. 10.1353/foc.0.0032 [DOI] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: prevalence, risk factors, and adolescent health consequences. Pediatrics, 118(3),933–942. 10.1542/peds.2005-2452 [DOI] [PubMed] [Google Scholar]
- Jones TL, & Prinz RJ (2005). Potential roles of parental self-efficacy in parent and child adjustment: A review. Clinical Psychology Review, 25(3), 341–363. 10.1016/j.cpr.2004.12.004 [DOI] [PubMed] [Google Scholar]
- Kellam SG, & Langevin DJ (2003). A framework for understanding “evidence” in prevention research and programs. Prevention Science, 4(3), 137–153. [DOI] [PubMed] [Google Scholar]
- Lei H, Nahum-Shani I, Lynch K, Oslin D, & Murphy SA (2012). A” SMART” design for building individualized treatment sequences. Annual Review of Clinical Psychology, 8, 21–48. 10.1146/annurev-clinpsy-032511-143152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin A, Mitchell SJ, & Ronzio CR (2013). Developmental differences in parenting behavior: Comparing adolescent, emerging adult, and adult mothers. Merrill-Palmer Quarterly, 59(1), 23–49. 10.1353/mpq.2013.0003 [DOI] [Google Scholar]
- Lieberman AF, Ippen CG, & Van Horn P (2015). Don’t hit my mommy: A manual for Child-Parent Psychotherapy with young children exposed to violence and other trauma, Second Edition. Washington, DC: Zero to Three. 10.1002/imhj.21816 [DOI] [Google Scholar]
- Lieberman AF, Ippen CG, & Van Horn P (2006). Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 45(8), 913–918. 10.1097/01.chi.0000222784.03735.92 [DOI] [PubMed] [Google Scholar]
- Lieberman AF, & Van Horn P (2005). Don’t hit my mommy!: A manual for child-parent psychotherapy with young witnesses of family violence: Zero to Three. 10.33212/att.v13n1.2019.127 [DOI] [Google Scholar]
- Lieberman AF, Van Horn P, & Ippen CG (2005). Toward evidence-based treatment: Child-parent psychotherapy with preschoolers exposed to marital violence. Journal of the American Academy of Child & Adolescent Psychiatry, 44(12), 1241–1248. 10.1097/01.chi.0000181047.59702.58 [DOI] [PubMed] [Google Scholar]
- Liu L, & Wang M (2015). Parenting stress and children’s problem behavior in China: The mediating role of parental psychological aggression. Journal of Family Psychology, 29(1), 20. 10.1037/fam0000047 [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, & Neuman G (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20(5), 561–592. 10.1016/s0272-7358(98)00100-7 [DOI] [PubMed] [Google Scholar]
- Luthar SS, & Eisenberg N (2017). Resilient Adaptation Among At‐Risk Children: Harnessing Science Toward Maximizing Salutary Environments. Child Development, 88(2), 337–349. 10.1111/cdev.12737 [DOI] [PubMed] [Google Scholar]
- Luthar SS, & Zigler E (1991). Vulnerability and competence: A review of research on resilience in childhood. American Journal of Orthopsychiatry, 61(1), 6–22. 10.1037/h0079218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons-Ruth K, & Melnick S (2004). Dose–response effect of mother–infant clinical home visiting on aggressive behavior problems in kindergarten. Journal of the American Academy of Child & Adolescent Psychiatry, 43(6), 699–707. 10.1097/01.chi.0000122730.72597.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madigan S, Wade M, Tarabulsy G, Jenkins JM, & Shouldice M (2014). Association between abuse history and adolescent pregnancy: a meta-analysis. Journal of Adolescent Health, 55(2), 151–159. 10.1016/j.jadohealth.2014.05.002 [DOI] [PubMed] [Google Scholar]
- MacLeod J, & Nelson G (2000). Programs for the promotion of family wellness and the prevention of child maltreatment: A meta-analytic review. Child Abuse & Neglect, 24(9), 1127–1149. 10.1016/s0145-2134(00)00178-2 [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, & Mathews TJ (2017). Births: Final data for 2015. National vital statistics report; vol 66, no 1. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Markowitz JC, Petkova E, Neria Y, Van Meter PE, Zhao Y, Hembree E, … Marshall RD (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry, 172(5), 430–440. 10.1176/appi.ajp.2014.14070908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer-Brody S, Bledsoe-Mansori SE, Johnson N, Killian C, Hamer RM, Jackson C, … & Thorp J, (2013). A prospective study of perinatal depression and trauma history in pregnant minority adolescents. American Journal of Obstetrics and Gynecology, 208(3), 211–e1. 10.1016/j.ajog.2012.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesman J, van IJzendoorn MH, & Bakermans‐Kranenburg MJ (2012). Unequal in opportunity, equal in process: Parental sensitivity promotes positive child development in ethnic minority families. Child Development Perspectives, 6(3), 239–250. 10.1111/j.1750-8606.2011.00223.x [DOI] [Google Scholar]
- Mikton C, & Butchart A (2009). Child maltreatment prevention: a systematic review of reviews. Bulletin of the World Health Organization, 87, 353–361. 10.2471/blt.08.057075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Perrin CL, Perrin RD, & Kocur JL (2009). Parental physical and psychological aggression: Psychological symptoms in young adults. Child Abuse & Neglect, 33(1),1–11. 10.1016/j.chiabu.2008.12.001 [DOI] [PubMed] [Google Scholar]
- Moore MR, & Brooks-Gunn J (2002). Adolescent parenthood. Handbook of Parenting, 3, 173–214. [Google Scholar]
- Morton N, & Browne KD (1998). Theory and observation of attachment and its relation to child maltreatment: A review. Child Abuse & Neglect, 22(11), 1093–1104. 10.1016/s0145-2134(98)00088-x [DOI] [PubMed] [Google Scholar]
- Mulcahy R, Reay RE, Wilkinson RB, & Owen C (2010). A randomised control trial for the effectiveness of group interpersonal psychotherapy for postnatal depression. Archives of Women’s Mental Health, 13(2), 125–139. 10.1007/s00737-009-0101-6 [DOI] [PubMed] [Google Scholar]
- Mufson L, Dorta KP, Moreau D, & Weissman MM (2004a). Interpersonal psychotherapy for depressed adolescents (second ed.). New York: Guilford Press. 10.1093/sw/40.5.713 [DOI] [Google Scholar]
- Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, & Weissman MM (2004b). A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry, 61(6), 577–584. 10.1001/archpsyc.61.6.577 [DOI] [PubMed] [Google Scholar]
- Mufson L, Weissman MM, Moreau D, & Garfinkel R (1999). Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry, 56(6), 573–579. 10.1001/archpsyc.56.6.573 [DOI] [PubMed] [Google Scholar]
- National Research Council (2014). New directions in child abuse and neglect research: National Academies Press. [PubMed] [Google Scholar]
- Nievar MA, Van Egeren LA, & Pollard S (2010). A meta‐analysis of home visiting programs: Moderators of improvements in maternal behavior. Infant Mental Health Journal, 31(5), 499–520. 10.1002/imhj.20269 [DOI] [PubMed] [Google Scholar]
- Noll JG, Shenk CE, & Putnam KT (2008). Childhood sexual abuse and adolescent pregnancy: A meta-analytic update. Journal of Pediatric Psychology, 34(4), 366–378. 10.1093/jpepsy/jsn098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL (2006). The nurse–family partnership: An evidence‐based preventive intervention. Infant Mental Health Journal, 27(1), 5–25. 10.1002/imhj.20077 [DOI] [PubMed] [Google Scholar]
- Olds DL (2008). Preventing child maltreatment and crime with prenatal and infancy support of parents: The nurse‐family partnership. Journal of Scandinavian Studies in Criminology and Crime Prevention, 9(S1), 2–24. 10.1080/14043850802450096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Eckenrode J, Henderson CR, Kitzman H, Powers J, Cole R, … Luckey D (1997). Long-term effects of home visitation on maternal life course and child abuse and neglect: Fifteen-year follow-up of a randomized trial. Jama, 278(8), 637–643. 10.1001/jama.1997.03550080047038 [DOI] [PubMed] [Google Scholar]
- Olds DL, Sadler L, & Kitzman H (2007). Programs for parents of infants and toddlers: recent evidence from randomized trials. Journal of Child Psychology and Psychiatry, 48(3‐4), 355–391. 10.1111/j.1469-7610.2006.01702.x [DOI] [PubMed] [Google Scholar]
- Owen MT, & Mulvihill BA (1994). Benefits of a parent education and support program in the first three years. Family Relations, 206–212. 10.2307/585324 [DOI] [Google Scholar]
- Parents as Teachers National Center (1999). Born to Learn curriculum (prenatal to 3 years). St. Louis, MO: Author. [Google Scholar]
- Paradis HA, Sandler M, Manly JT, & Valentine L (2013). Building healthy children: Evidence-based home visitation integrated with pediatric medical homes. Pediatrics, 132(Supplement 2), S174–S179. 10.1542/peds.2013-1021r [DOI] [PubMed] [Google Scholar]
- Pfannenstiel J, Lambson T, & Yarnell V (1996). The Parents as Teachers program: Longitudinal follow up to the Second Wave Study. Overland Park, KS: Research & Training Associates. [Google Scholar]
- Pfannenstiel J, Lambson T, Yarnell V, Research, Inc., T. A., & America, U. S. o. (1991). Second wave study of the Parents as Teachers program: Executive summary. St. Louis, MO: Parents as Teachers National Center. [Google Scholar]
- Pfannenstiel J, & Seltzer D (1989). New parents as teachers: Evaluation of an early parent education program. Early Childhood Research Quarterly, 4(1), 1–18. 10.1016/s0885-2006(89)90025-2 [DOI] [Google Scholar]
- Group Perryman (2014). Suffer the Little Children: An Assessment of the Economic Cost of Child Maltreatment. The Perryman Group. Retrieved from: https://www.perrymangroup.com/media/uploads/reports/perryman-suffer-the-little-children-11-2014.pdf. [Google Scholar]
- Robinson JL, & Emde RN (2004). Mental health moderators of Early Head Start on parenting and child development: Maternal depression and relationship attitudes. Parenting: Science and Practice, 4(1), 73–97. 10.1207/s15327922par0401_4 [DOI] [Google Scholar]
- Rodriguez C (2010). Parent–child aggression: Association with child abuse potential and parenting styles. Violence and Victims, 25(6), 728–741. 10.1891/0886-6708.25.6.728 [DOI] [PubMed] [Google Scholar]
- Rossello J, & Bernal G (1999). The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of consulting and clinical psychology, 67(5), 734. 10.1037/0022-006x.67.5.734 [DOI] [PubMed] [Google Scholar]
- Roth A, & Fonagy P (2013). What works for whom?: a critical review of psychotherapy research: Guilford Publications. [Google Scholar]
- Russotti J, Rogosch FA, Handley ED, Douthit KZ, Marquis A, & Cicchetti D (2020). Teen childbearing and offspring internalizing symptoms: the mediating role of child maltreatment. Development and Psychopathology, 1–13. 10.1017/s0954579420000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M (1987). Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry, 57(3), 316. 10.1111/j.1939-0025.1987.tb03541.x [DOI] [PubMed] [Google Scholar]
- Shaw DS, Gilliom M, Ingoldsby EM, & Nagin DS (2003). Trajectories leading to school-age conduct problems. Developmental Psychology, 39(2), 189. 10.1037/0012-1649.39.2.189 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33(6), 906. 10.1037/0012-1649.33.6.906 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (1998). Reactive aggression among maltreated children: The contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology, 27(4), 381–395. 10.1207/s15374424jccp2704_2 [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, & Fisher PA (2013). Rethinking evidence-based practice and two-generation programs to create the future of early childhood policy. Development and Psychopathology, 25(4pt2), 1635–1653. 10.1017/s0954579413000813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidebotham P, Heron J, & Team AS (2006). Child maltreatment in the “children of the nineties”: A cohort study of risk factors. Child Abuse & Neglect, 30(5), 497–522. 10.1016/j.chiabu.2005.11.005 [DOI] [PubMed] [Google Scholar]
- Spinazzola J, Hodgdon H, Liang L-J, Ford JD, Layne CM, Pynoos R, … Kisiel C (2014). Unseen wounds: The contribution of psychological maltreatment to child and adolescent mental health and risk outcomes. Psychological Trauma: Theory, Research, Practice, and Policy 6(S1), S18. 10.1037/a0037766 [DOI] [Google Scholar]
- Sroufe LA (2005). Attachment and development: A prospective, longitudinal study from birth to adulthood. Attachment & Human Development, 7(4), 349–367. 10.1080/14616730500365928 [DOI] [PubMed] [Google Scholar]
- Stams G-JJ, Juffer F, & van IJzendoorn MH (2002). Maternal sensitivity, infant attachment, and temperament in early childhood predict adjustment in middle childhood: The case of adopted children and their biologically unrelated parents. Developmental Psychology, 38(5), 806 10.1037/0012-1649.38.5.806 [DOI] [PubMed] [Google Scholar]
- Straus MA, & Field CJ (2003). Psychological aggression by American parents: National data on prevalence, chronicity, and severity. Journal of Marriage and Family, 65(4), 795–808. 10.1111/j.1741-3737.2003.00795.x [DOI] [Google Scholar]
- Stith SM, Liu T, Davies LC, Boykin EL, Alder MC, Harris JM, … Dees J (2009). Risk factors in child maltreatment: A meta-analytic review of the literature. Aggression and Violent Behavior, 14(1), 13–29. 10.1016/j.avb.2006.03.006 [DOI] [Google Scholar]
- Supplee LH, & Duggan A (2019). Innovative research methods to advance precision in home visiting for more efficient and effective programs. Child Development Perspectives, 13(3), 173–179. 10.1111/cdep.12334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet MA, & Appelbaum MI (2004). Is home visiting an effective strategy? A meta‐analytic review of home visiting programs for families with young children. Child Development, 75(5), 1435–1456. 10.1111/j.1467-8624.2004.00750.x [DOI] [PubMed] [Google Scholar]
- Szigethy EM, & Ruiz P (2001). Depression among pregnant adolescents: an integrated treatment approach. American Journal of Psychiatry, 158(1), 22–27. 10.1176/appi.ajp.158.1.22 [DOI] [PubMed] [Google Scholar]
- Teti DM, & Gelfand DM (1991). Behavioral competence among mothers of infants in the first year: The mediational role of maternal self‐efficacy. Child Development, 62(5), 918–929. 10.2307/1131143 [DOI] [PubMed] [Google Scholar]
- Teti DM, Nakagawa M, Das R, & Wirth O (1991). Security of attachment between preschoolers and their mothers: Relations among social interaction, parenting stress, and mother’s sorts of the Attachment Q-Set. Developmental Psychology, 27(3), 440. 10.1037/0012-1649.27.3.440 [DOI] [Google Scholar]
- Thomas R, & Zimmer‐Gembeck MJ (2011). Accumulating evidence for parent–child interaction therapy in the prevention of child maltreatment. Child Development, 82(1), 177–192. 10.1111/j.1467-8624.2010.01548.x [DOI] [PubMed] [Google Scholar]
- Tofighi D, & MacKinnon DP (2011). RMediation: An R package for mediation analysis confidence intervals. Behavior Research Methods, 43(3), 692–700. 10.3758/s13428-011-0076-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth SL, & Manly JT (2011). Bridging research and practice: Challenges and successes in implementing evidence-based preventive intervention strategies for child maltreatment. Child Abuse & Neglect, 35(8), 633–636. 10.1016/j.chiabu.2011.05.003 [DOI] [PubMed] [Google Scholar]
- Toth SL, Maughan A, Manly JT, Spagnola M, & Cicchetti D (2002). The relative efficacy of two interventions in altering maltreated preschool children’s representational models: Implications for attachment theory. Development and Psychopathology, 14(4), 877–908. 10.1017/s095457940200411x [DOI] [PubMed] [Google Scholar]
- Toth SL, Rogosch FA, Manly JT, & Cicchetti D (2006). The efficacy of toddler-parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: a randomized preventive trial. Journal of Consulting and Clinical Psychology, 74(6), 1006. 10.1037/0022-006x.74.6.1006 [DOI] [PubMed] [Google Scholar]
- Toth SL, Rogosch FA, Oshri A, Gravener-Davis J, Sturm R, & Morgan-López AA (2013). The efficacy of interpersonal psychotherapy for depression among economically disadvantaged mothers. Development and Psychopathology, 25(4pt1), 1065–1078. 10.1017/s0954579413000370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. (2020). Child Maltreatment 2018. 10.1037/e303422003-014 [DOI] [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, & Cicchetti D (2015). Different forms of child maltreatment have comparable consequences among children from low-income families. JAMA Psychiatry, 72(11), 1135. 10.1001/jamapsychiatry.2015.1792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veltkamp LJ, & Miller TW (1994). Clinical handbook of child abuse and neglect: International Universities Press, Inc. [Google Scholar]
- Wagner M, & Clayton S (1999). The Parents as Teachers program: Results from two demonstrations. The Future of Children, 91–115. 10.2307/1602723 [DOI] [PubMed] [Google Scholar]
- Wagner M, Spiker D, & Linn MI (2002). The effectiveness of the Parents as Teachers program with low-income parents and children. Topics in Early Childhood Special Education, 22(2), 67–81. 10.1177/02711214020220020101 [DOI] [Google Scholar]
- Webster-Stratton C (1998). Preventing conduct problems in Head Start children: strengthening parenting competencies. Journal of Consulting and Clinical Psychology, 66(5), 715. 10.1037/0022-006x.66.5.715 [DOI] [PubMed] [Google Scholar]
- Weisz JR, & Jensen PS (1999). Efficacy and effectiveness of child and adolescent psychotherapy and pharmacotherapy. Mental Health Services Research, 1(3), 125–157. [DOI] [PubMed] [Google Scholar]
- Young JF, Mufson L, & Davies M (2006). Efficacy of Interpersonal Psychotherapy‐Adolescent Skills Training: an indicated preventive intervention for depression. Journal of Child Psychology and Psychiatry, 47(12), 1254–1262. 10.1111/j.1469-7610.2006.01667.x [DOI] [PubMed] [Google Scholar]
- Zigler E, & Trickett PK (1978). IQ, social competence, and evaluation of early childhood intervention programs. American Psychologist, 33(9), 789. 10.1037/0003-066x.33.9.789 [DOI] [Google Scholar]
- Zigler E & Valentine J (1979). Project Head Start: A Legacy of the War on Poverty. The Free Press, A Division of Macmillan Publishing Co., Inc. [Google Scholar]
- Zigler E, Taussig C, & Black K (1992). Early childhood intervention: a promising preventative for juvenile delinquency. American Psychologist, 47(8), 997. 10.1037/0003-066x.47.8.997 [DOI] [PubMed] [Google Scholar]
- Zigler E, & Finn‐Stevenson M (2007). From research to policy and practice: The school of the 21st century. American Journal of Orthopsychiatry, 77(2), 175–181. 10.1037/0002-9432.77.2.175 [DOI] [PubMed] [Google Scholar]


