Abstract
Background and aim
Understanding people's attitudes towards Covid-19 vaccination is crucial to the successful implementation of a vaccination program. Hence this research study seeks to identify critical factors influencing Indian people's attitudes and intentions to take up Covid-19 vaccinations.
Methods
An online questionnaire was administered to a sample (n = 254) drawn from Indian population, to assess the impact of perceived benefits, risk perceptions, social media exposure, social norms, and trust associated with Covid-19 vaccines on people's attitudes towards Covid-19 vaccines and their intentions to take up the Covid-19 vaccinations.
Results
The findings showed that the perceived benefits, social norms, and trust correlated significantly with people's attitudes towards Covid-19 vaccinations. In contrast, risk perceptions and social media exposure showed an insignificant influence on people's attitudes towards Covid-19 vaccinations. Social norms, trust, and people's attitudes towards the Covid-19 vaccinations are significantly correlated with their intentions to take up Covid-19 vaccinations. On the contrary, social media exposure was found to have an insignificant influence on people's intentions to take up Covid-19 vaccinations.
Conclusion
Participants' intentions to take up Covid-19 vaccinations was influenced mainly by their attitudes and perceptions of Covid-19 vaccines in general, which strongly confirms the importance of various dimensions (perceived benefits, trust, social norms) of Covid-19 vaccines in cultivating Covid-19 vaccination acceptance among participants’.
Keywords: Covid-19 vaccination, Statistical analysis, Structural equation modeling, Theory of planned behavior (TPB), Health belief model (HBM)
1. Introduction
In December 2019, the novel Corona-virus (Covid-19) first came to light in Wuhan, China and within one month only, it has been proclaimed as a public health emergency worldwide. The outbreak of corona virus-related disease was coined as Corona pandemic by World Health Organization [1]. This deadly virus has taken away so many lives throughout the world, till February 2021, around 106 million people were affected by Corona-virus infection, and more than 2.3 million people died due to Covid-19 virus, these confirmed cases and death rates were recorded globally [1,2]. As of January 30, 2020, the first confirmed case of Covid-19 infection came to light in Kerala, India [3]. Despite being imposing travel-related restrictions, social distancing, and other preventive measures to control corona related infection, India has witnessed a spike in Covid-19 cases. Till mid-march 2021, more than 2, 00 thousand active cases of corona and approximately 160 thousand corona-related deaths have already taken place since its outbreak in India.
High fever, dry cough, respiratory difficulties, chest pain, extreme shortness of breath, and bilateral pulmonary infiltration are all signs of Covid-19 virus-related infection [4,5]. A core strategy for curing and preventing this deadly virus is through vaccinations. As SARS-CoV-2 is an exceptionally infectious and communicable virus that affects communities worldwide hence,Covid-19 vaccination are the most effective treatment for this disease [6,7]. Thus, mass immunization is necessary to reduce the spread of infection; however, queries still exist regarding the degree and extent of protection from the vaccinations of Covid-19 [8].
However, anti-vaccination sentiment has grown, giving rise to the phenomenon of vaccine hesitancy [9]. Vaccine hesitancy is amongst the top ten risks of public health declared by the WHO, that have wrecked havoc on immunization programs worldwide, as it remains a significant roadblock in achieving optimal vaccination targets [10].
People all over the world are waiting and hoping for a vaccine since the virus first emerged. Understanding why people are reluctant to get the Covid-19 vaccination done is essential, as it can aid health officials in increasing vaccine awareness and limiting the disease's spread [7]. As a result, there is a pressing need for a more up-to-date and nuanced understanding of vaccine-related attitudes and the factors influencing people's intentions to take up Covid-19 vaccines.
1.1. Proposed conceptual framework and development of hypotheses
1.1.1. Perceived benefits
Perceived benefits regarding Covid-19 vaccines are explained as a belief that vaccinations will reduce the risk of this severe infection which causes various diseases and threats to human life [11]. The patients who were tested positive even after the vaccinations also required lesser hospitalization and medical care than those who were not vaccinated [1]. Vaccinations provide social benefits by reducing Corona-virus infection spread, which ultimately protects society from a pandemic [12]. Majority of the respondents agreed that to protect themselves from Corona-virus infection, it is better to take up the vaccinations [13].
H1
Perceived benefits influence participants' attitude towards Covid-19 vaccination
1.1.2. Risk perception
Risk perceptions include emotional elements like fear, anxiety, and worry [7]. Risk perception in context of vaccines can be defined as the doubts about vaccines' effectiveness and fear of side effects of these vaccines [14]. Risk perception plays a crucial role in the intentions to get vaccinated [15]. People are not ready to take up Covid-19 vaccinations due toits adverse side effects; despite having high benefit-to-risk ratio of these vaccines [16].
H2
Risk perception influences participants' attitude towards Covid-19 vaccination
1.1.3. Social norms
Social norms are defined as individuals' views and decisions influenced by external elements [17]. In the context of Corona-virus pandemic, social norms are concerned with people's behavior [18] which is influenced by societal values and choices, which includes various elements like family members, relatives, friends, etc., who are responsible for changes in people's viewpoints and perceptions [19]. The intentions for getting the Corona-virus vaccinations done was positively correlated with the subjective norms [20].
H3
Social norms influence participants' attitudes towards Covid-19 vaccinations
H4
Social norms influence participants' intentions towards Covid-19 vaccinations
1.1.4. Social media exposure
Social media is an internet-based technology or application that facilitates sharing ideas, information, and thoughts over multiple platforms through the building of virtual networks and communities [21]. Social media is a robust platforms for sharing and acquiring information on various states of affairs, especially during such a prevailing pandemic situation of Covid-19 [22] Social media platform helps in assessing public confidence related to Covid-19 vaccinations [23].
H5
Social media influences participants' attitudes towards Covid-19 vaccinations
H6
Social media influences participants' intentions towards Covid-19 vaccinations
1.1.5. Trust
Trust means the character, strength, or truth of something or someone [24]. Individuals recommended by medical professionals are more likely to take up Covid-19 vaccinations [25]. Trust plays an important role in vaccine decisions [26]. Majority of people accepting Covid-19 vaccinations are likely to be those nations that hold trust in their governments, like South Korea and China [27].
H7
Trust influences participants' attitudes towards Covid-19 vaccinations
H8
Trust influences participants' intentions towards Covid-19 vaccinations
1.1.6. Attitudes and intentions
Attitude refers to how an individual views something or tends to behave towards it, usually in an evaluative way [28]. Understanding people's attitudes towards Covid-19 vaccination is crucial to the successful implementation of a vaccination program and to tailor public health massaging as usually, public attitudes towards vaccine safety and efficacy are consistently associated with vaccine uptake [24,29].
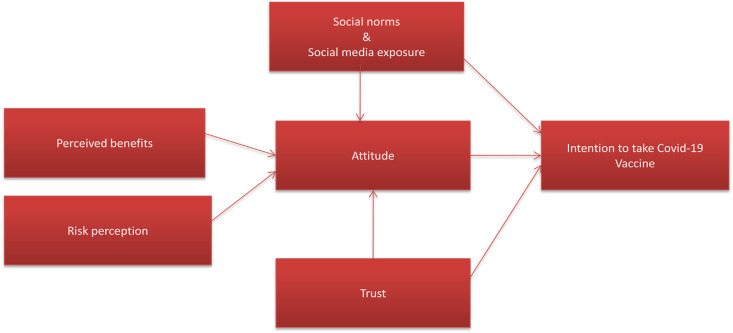
H9
There is a positive relationship between people's attitude and intention towards Covid-19 vaccination. The proposed conceptual framework is shown in Fig. 1 .
Fig. 1.
Proposed conceptual framework.
2. Methods
2.1. Data collection
To approve the proposed conceptual framework and examine the proposed research hypotheses; a questionnaire was developed and administered through the internet to collect required data from people in India. For this study, 300 questionnaires were administered to obtain responses from Indian people regarding their views and perceptions about various Covid-19 vaccines available in India. However, out of 300 respondents, only 254 duly filled questionnaires were received from the respondents. All items were modified using a Likert scale in five points ranging from strongly disagree (1) to strongly agree (5). A pilot study was carried out with 30 participants to ensure that the questions and response formats were understood. The majority of respondents indicated that the language used was simple, and the questionnaire's length was also suitable.
2.2. Statistical analysis
The data collected were processed and analyzed using two statistical software's, SPSS 20.0 and AMOS 21.0. To understand the structure of the sample, demographic analysis of the respondents was done in the first stage. Responses of 46 participants were discarded during the pre-processing of data due to missing data points. As a result, this study examined the responses of only 254 participants, and the results are summarized below in Table 1 . The results indicate that approx. 56% of the participants were males, and the remaining 44% were females. The majority of participants, which is approx. 38%, were between 18 -30 years of age. The majority of the participants were postgraduates, and this counts approx. 53%.
Table 1.
Demographic profile.
| N | Percentage | ||
|---|---|---|---|
| Gender | Male | 143 | 56 |
| Female | 111 | 44 | |
| Age (year) | 18-30 | 97 | 38 |
| 31-42 | 89 | 35 | |
| 43-55 | 56 | 22 | |
| Above 55 | 12 | 5 | |
| Nationality | Indian | 254 | 100 |
| Foreign Nationals | – | – | |
| Educational Qualification | Bachelor | 99 | 39 |
| Master degree | 134 | 53 | |
| Ph.D | 21 | 8 | |
| Other | – | ||
The Cronbach alpha, reliability, and validity of the constructs were assessed. To compute the internal accuracy of survey items, the Cronbach alpha was calculated (see Table 2 ). All values were greater than 0.70 suggested by Ref. [30]. The measurement model (CFA) was put under test to ensure an adequate model fitness level and constructs validity and reliability. Absolute fit indices which include “χ2/df (Chi-square to degree of freedom ratio) and RMSEA (root mean-square error of approximation), Incremental fit indices comprised CFI (comparative fit index) and TLI (Tucker-Lewis Index) and also, parsimony fit was examined using AGFI (adjusted goodness-of-fit index)”. The model fit is good when “χ2/df < 3.0, with the values of CFI, TLI ≥ 0.90, RMSEA ≤ 0.08, and AGFI ≥ 0.80” [30].The resultant fit statistics “(χ2 = 270.393,df = 209, p < .01; χ2/df = 1.294; CFI = .982; TLI = .979; RMSEA = .034; GFI= .920; AGFI = .895)” were all higher than the minimum acceptable limit [31,32].
Table 2.
Factor loading &Chronbach's alpha.
| Constructs | Item | Factor Loading | Chronbach's Alpha |
|---|---|---|---|
| Perceived Benefits | PB1 | 0.825 | 0.819 |
| PB2 | 0.801 | ||
| PB3 | 0.797 | ||
| Risk Perception | RP1 | 0.919 | 0.908 |
| RP2 | 0.917 | ||
| RP3 | 0.904 | ||
| Media Exposure | ME1 | 0.874 | 0.882 |
| ME2 | 0.861 | ||
| ME3 | 0.838 | ||
| Social Norms | SN1 | 0.876 | 0.883 |
| SE2 | 0.873 | ||
| SE3 | 0.824 | ||
| Trust | TR1 | 0.861 | 0.856 |
| TR2 | 0.807 | ||
| TR3 | 0.796 | ||
| Attitude | AT1 | 0.808 | 0.880 |
| AT2 | 0.802 | ||
| AT3 | 0.775 | ||
| AT4 | 0.731 | ||
| Intention | INT1 | 0.838 | 0.895 |
| INT2 | 0.768 | ||
| INT3 | 0.750 | ||
| INT4 | 0.744 | ||
Reliability measurements such as Composite Reliability and Average Variance Extracted were computed to assess constructs' internal consistency. For all constructs, the CR values were higher than 0.70 33, indicating that the proposed conceptual framework has reasonably good internal consistency. Similarly, for all constructs, the AVE values were higher than 0.50 33. Furthermore, CR is greater than AVE, the average variance derived, and composite reliability verified the entire constructs' convergent validity.
Furthermore, discriminant validity is always an essential measurement to assess constructs' validity [33]. According to this approach, the AVE of each construct must be greater than the squared correlation between the build and remaining constructs. As shown in Table 3 , the discriminant validity is satisfying, demonstrated by the measurement model. Squared multiple correlations among the variables are shown in the diagonal elements. As shown in Table 3, values of AVE range from 0.603 to 0.767. Diagonal value also ranges from 0.776 to 0.876, which indicates that the diagonal variable is greater than other AVE values, which means high adequacy of discriminant validity for all constructs.
Table 3.
Reliability, Validity Statistics, and Correlations.
| CR | AVE | MSV | MaxR(H) | TR | INT | ATT | RP | ME | SN | PB | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| TR | 0.858 | 0.669 | 0.328 | 0.860 | 0.818∗ | ||||||
| INT | 0.899 | 0.689 | 0.417 | 0.911 | 0.573 | 0.830∗ | |||||
| ATT | 0.882 | 0.651 | 0.417 | 0.887 | 0.475 | 0.646 | 0.807∗ | ||||
| RP | 0.908 | 0.767 | 0.032 | 0.909 | 0.037 | 0.103 | 0.158 | 0.876∗ | |||
| ME | 0.882 | 0.713 | 0.188 | 0.884 | 0.434 | 0.409 | 0.405 | 0.178 | 0.845∗ | ||
| SN | 0.885 | 0.719 | 0.217 | 0.885 | 0.338 | 0.466 | 0.427 | 0.093 | 0.289 | 0.848∗ | |
| PB | 0.820 | 0.603 | 0.285 | 0.823 | 0.303 | 0.512 | 0.534 | 0.082 | 0.342 | 0.382 | 0.776∗ |
Note: “CR = composite reliability; AVE = average variance extracted; MSV = maximum shared variance; MaxR(H) = maximum reliability; (∗) = square root of AVE”.
3. Results
Structural equation modeling was deployed to test the main research hypotheses between the proposed constructs. All fit indices of the structural model were found to be within appropriate ranges, similar to the measurement model: “GFI = 0.918; AGFI = 0.893; NFI = 0.926; CFI = 0.981; and RMSEA = 0.035” [31,32]. These indices show a good fitting model representing 55% of the variation in participants’ intentions to take up Covid-19 vaccines. Path coefficient analyses were used to test the major causal paths, as shown in Table 4 . The main factors of the proposed conceptual framework namely, perceived benefits (β = .344, t = 4.878, p < .001) on attitudes towards Covid-19 vaccines were found significant. Therefore, H1 were supported. Whilst, risk perception (β = .054, t = 1.462, p > .05) on attitudes towards Covid-19 vaccines were found insignificant therefore, H2 were not supported. Social norms on attitudes (β = .115, t = 2.441, p < 0.05) and intentions (β = .157, t = 2.916, p < .01), were found significant so, hypothesis H3 and H4 were supported. In contrast to media exposure on attitudes (β = .083, t = 1.570, p > .05) and on intentions (β = .066, t = 1.107, p > .05) were found having insignificant influence so, it is concluded that H5 and H6 were supported. Trust on attitudes (β = .202, t = 3.641, p < 0.001) and intentions (β = .286, t = 4.301, p < .001), were found significant. Thus hypothesis H7 and H8 were supported.
Table 4.
Hypotheses testing.
| Estimates | SE. | CR. | P | Decision | |
|---|---|---|---|---|---|
| PB → ATT | 0.344 | 0.071 | 4.878 | ∗∗∗ | Supported |
| RP → ATT | 0.054 | 0.037 | 1.462 | 0.144 | Not Supported |
| SN → ATT | 0.115 | 0.047 | 2.441 | ∗ | Supported |
| ME → ATT | 0.083 | 0.053 | 1.570 | 0.116 | Not Supported |
| TR → ATT | 0.202 | 0.055 | 3.641 | ∗∗∗ | Supported |
| SN → INT | 0.157 | 0.054 | 2.916 | ∗∗ | Supported |
| ME → INT | 0.066 | 0.060 | 1.107 | 0.269 | Not Supported |
| TR → INT | 0.286 | 0.066 | 4.301 | ∗∗∗ | Supported |
| ATT → INT | 0.526 | 0.088 | 5.977 | ∗∗∗ | Supported |
Note: “P < 0.05 ∗, P < 0.01 ∗∗, P < 0.001 ∗∗∗”.
Notably, attitudes towards Covid-19 vaccines exerted a strong positive impact on participant's intentions to take up Covid-19 vaccinations (β = .526, t = 5.977, p < .001) consequently, H9 was supported.
4. Discussion
This research study seeks to identify critical factors influencing Indian people's attitudes and intentions to take up Covid-19 vaccinations. To operational the research objectives a conceptual framework was proposed by integrating the Theory of planned behavior (TPB) and health belief model (HBM) along with social media exposures. The research findings showed that perceived benefits are supported to have a significant impact on participants' attitudes towards Covid-19 vaccine uptake. These results are similar with the previous studies [7,34]. Participants agreed to take up Covid-19 vaccinations, if they found higher levels of perceived benefits regarding Covid-19 vaccines. Risk perception shows an insignificant relationship with attitudes. These results are similar to other studies [7,16]. Participants generally viewed Covid-19 as a severe health risk, hence they tend not to feel very vulnerable or fear the vaccine.
Furthermore, the social norms and trust were supported to have a significant impact on the attitudes and intentions towards Covid-19 vaccine uptake. These results are comparable to previous research studies for trust [35,36] and social norms [34]. Basically, trust of participants regarding Covid-19 vaccines mainly consists of vaccine development, clinical trials, and approval of these vaccines from government and medical authorities. Social norms consist of family, friends, and doctors with whom participants enjoy a close relationship and consider them as trusted.
Social media exposure showed an insignificant relationship on attitudes and Intentions towards Covid-19 vaccine uptake. These results are also supported by previous studies [21,[37], [38], [39]]. A strong relationship was also supported between participants’ attitudes and intentions towards Covid-19 vaccination and these results support earlier research work [17,40].
Findings from this research study have several implications for public health campaigns and educational programs aimed at promoting wider acceptance of the Covid-19 vaccines. First and foremost, the public health system needs to emphasize the actual impact of the Covid-19 disease and its severity on public health. Second, the benefits derived from the Covid-19 vaccine must be conveyed to the public through various effective means of communications that should increase understanding of the public's knowledge and positive perceptions regarding Covid-19 vaccines. Thirdly, the governments should conduct campaigns, public rallies, and educational programs to positively influence people's attitudes and intentions towards the uptake of the Covid-19 vaccines.
This research study had some limitations. First, this study did not analyze the moderating effects of demographic characteristics. Sub-analysis of the current data and future studies might address this issue and provide a better and more detailed interpretation of participants intentions by incorporating demographic variables not included in this report. Second this research study's results did not exhibit respondents' actual behavior future studies might focus on actual behavior regarding Covid-19 vaccinations.
Ethical approval
No ethical approval was required for this research study, as this research focused on attitude and intentions not an actual behavior.
Funding
No funding was received to support the writing of this research paper.
Declaration of competing interest
The authors have no Competing or conflicting interests.
Appendix.
| Constructs | Items | |
|---|---|---|
| Perceived benefits | I believe vaccines for Covid-19 will reduce my chances of becoming infected with the disease. | (All items are Self constructed) |
| I believe vaccines for Covid-19 will help our community to control the Covid-19 disease. | ||
| I believe vaccines for Covid-19 will be effective in preventing the Covid-19 disease. | ||
| Risk Perception | I believe vaccines for Covid-19 will have adverse side effects. | |
| I fear that after getting Covid-19 vaccines, I could fall prey to infectious diseases. | ||
| I fear taking up Covid-19 vaccines as it is still under in its trial stage. | ||
| Social Media | I believe social media provides relevant information about Covid-19 vaccines | |
| I believe social media inspire me to take the Covid-19 vaccines | ||
| I believe the comprehensive information on Covid-19 vaccines on social media was helpful to me. | ||
| Social Norms | My family recommends me to take-up Covid-19 vaccines. | |
| People who are important to me influence my decision to take up Covid-19 vaccines | ||
| My friends and colleagues influence my decision to take up Covid-19 vaccines. | ||
| Trust | I feel assured that Covid-19 vaccines are effective against the Covid-19 virus. | |
| I believe that Covid-19 vaccines are an effective solution to cure and prevent the Covid-19 pandemic. | ||
| I trust Covid-19 vaccines as it is recommended and approved by medical professionals and government authorities. | ||
| Attitude | In my opinion, Covid-19 vaccine is an effective response to the corona pandemic | |
| I have surely decided to take up Covid-19 vaccines. | ||
| I would never refuse a dose of Covid-19 vaccines. | ||
| I think Covid-19 vaccines are a necessity for all people. | ||
| Intention | I intend to take up Covid-19 vaccines soon. | |
| I would recommend my family members to take up Covid-19 vaccines. | ||
| I intend to take up Covid-19 vaccines if it is recommended by a doctor. | ||
| I intend to take up Covid-19 vaccines as it boosts my immune system. |
References
- 1.Conlon A., Ms C.A., Washer L., Eagle K.A., Bowman M.A.H. Impact of the influenza vaccine on COVID-19 infection rates and severity. AJIC Am J Infect Control. 2021 doi: 10.1016/j.ajic.2021.02.012. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong E., Du H., Gardner L. The Lancet Infectious Diseases. vol. 20. Lancet Publishing Group; 2020. An interactive web-based dashboard to track COVID-19 in real time.https://www.who.int/china/news/ [Internet] [cited 2021 Mar 2]. p. 533–4. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foy B.H., Wahl B., Mehta K., Shet A., Menon G.I., Britto C. Comparing COVID-19 vaccine allocation strategies in India: a mathematical modelling study. Int J Infect Dis. 2021;103:431–438. doi: 10.1016/j.ijid.2020.12.075. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li T., Zhang T., Gu Y., Li S., Xia N. Current progress and challenges in the design and development of a successful COVID-19 vaccine. Fundam Res. 2021 doi: 10.1016/j.fmre.2021.01.011. [Internet] 0–56. Available from: [DOI] [Google Scholar]
- 5.Deng S.-Q., Peng H.-J. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. 2020 Feb 20;9(2):575. doi: 10.3390/jcm9020575. https://pubmed.ncbi.nlm.nih.gov/32093211/ [Internet] [cited 2021 Mar 2] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saiful Islam M., Siddique A.B., Akter R., Tasnim R., Safaet M., Sujan H. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. medRxiv. 2021 Feb 19 doi: 10.1101/2021.02.16.21251802. [Internet] [cited 2021 Mar 11];2021.02.16.21251802. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karlsson L.C., Soveri A., Lewandowsky S., Karlsson L., Karlsson H., Nolvi S. Fearing the disease or the vaccine: the case of COVID-19. Pers Indiv Differ. 2021 Apr 1;172:110590. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Altmann D.M., Douek D.C., Boyton R.J. The Lancet. vol. 395. Lancet Publishing Group; 2020. What policy makers need to know about COVID-19 protective immunity; pp. 1527–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Publ Health. 2021 Feb doi: 10.1016/S2468-2667. [Internet] [cited 2021 Mar 15];0(0). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sonawane K., Troisi C.L., Deshmukh A.A. COVID-19 vaccination in the UK: addressing vaccine hesitancy. Lancet Regul Health Eur. 2021;1:100016. doi: 10.1016/j.lanepe.2020.100016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zampetakis L.A., Melas C. The health belief model predicts vaccination intentions against COVID-19: a survey experiment approach. Appl Psychol Heal Well-Being. 2021 Feb 26 doi: 10.1111/aphw.12262. https://onlinelibrary.wiley.com/doi/10.1111/aphw.12262 [Internet] [cited 2021 Mar 2];aphw.12262. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jung H., Albarracín D. Concerns for others increases the likelihood of vaccination against influenza and COVID-19 more in sparsely rather than densely populated areas. Proc Natl Acad Sci U S A. 2020;118(1) doi: 10.1073/pnas.2007538118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seale H., Heywood A.E., Leask J., Sheel M., Durrheim D.N., Bolsewicz K. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect Dis. 2021 Dec 1;21(1) doi: 10.1186/s12879-021-05833-1. http://pmc/articles/PMC7840792/ [Internet] [cited 2021 Apr 12] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lehmann B.A., Ruiter R.A.C., Chapman G., Kok G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine. 2014;32(51) doi: 10.1016/j.vaccine.2014.10.034. [Internet] [cited 2021 Mar 15], 6986–91. Available from: [DOI] [PubMed] [Google Scholar]
- 15.Caserotti M., Girardi P., Rubaltelli E., Tasso A., Lotto L., Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. 2021;272 doi: 10.1016/j.socscimed.2021.113688. (December 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Echoru I., Ajambo P.D., Bukenya E.M. 2020. Acceptance and risk perception of COVID-19 vaccine in Uganda: a Cross Sectional study in Western Uganda; pp. 1–11. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chu H., Liu S. Patient education and counseling integrating health behavior theories to predict American ’ s intention to receive a COVID-19 vaccine. Patient Educ Couns. 2021 doi: 10.1016/j.pec.2021.02.031. [Internet] (xxxx). Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maqbool A., Khan N.Z. Analyzing barriers for implementation of public health and social measures to prevent the transmission of COVID-19 disease using DEMATEL method. Diabetes Metab Syndr Clin Res Rev. 2020 Sep;14(5):887–892. doi: 10.1016/j.dsx.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The importance of new social norms in a COVID-19 outbreak. https://policyoptions.irpp.org/magazines/march-2020/the-importance-of-new-social-norms-in-a-covid-19-outbreak/ [Internet], [cited 2021 Mar 17]. Available from:
- 20.Guidry J.P.D., Laestadius L.I., Vraga E.K., Miller C.A., Perrin P.B., Burton C.W. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Contr. 2021 Feb 1;49(2) http://pmc/articles/PMC7677682/ [Internet] [cited 2021 Mar 3] 137–42. Available from: [Google Scholar]
- 21.Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccines Immunother. 2020:1–8. doi: 10.1080/21645515.2020.1780846. [Internet] 00(00), Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.González-Padilla D.A., Tortolero-Blanco L. Social media influence in the COVID-19 pandemic. Int Braz J Urol. Braz Soc Urol. 2020;vol. 46 doi: 10.1590/S1677-5538.IBJU.2020.S121. http://orcid.org/0000-0002-5853-8845 [Internet] [cited 2021 Apr 12]. p. 120–4. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hussain A., Sheikh A. Opportunities for Artificial Intelligence–Enabled social media analysis of public attitudes toward Covid-19 vaccines. Nejm Catal Innov Care Deliv. 2021 [Internet] [cited 2021 Mar 3]; Available from::/pmc/articles/PMC7864479/ [Google Scholar]
- 24.Merhi M., Hone K., Tarhini A. A cross-cultural study of the intention to use mobile banking between Lebanese and British consumers: extending UTAUT2 with security, privacy and trust. Technol Soc. 2019;59 (June) [Google Scholar]
- 25.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020 Sep 29;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Majid U., Ahmad M. The factors that promote vaccine hesitancy, rejection, or delay in parents. Qual Health Res. 2020 Sep 1;30(11) doi: 10.1177/1049732320933863. http://journals.sagepub.com/doi/10.1177/1049732320933863 [Internet] [cited 2021 Mar 4] 1762–76. Available from: [DOI] [PubMed] [Google Scholar]
- 27.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2020 Oct 20;27(2) doi: 10.1038/s41591-020-1124-9. [Internet] [cited 2021 Mar 4], 225–8. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buchari I., Rafiki A., Qassab MAH Al. Awareness and attitudes of employees towards islamic banking products in Bahrain. Procedia Econ Financ. 2015;30:68–78. www.sciencedirect.com [Internet] [cited 2021 Mar 16] Available from: [Google Scholar]
- 29.Habersaat K.B., Betsch C., Danchin M., Sunstein C.R., Böhm R., Falk A. Ten considerations for effectively managing the COVID-19 transition. Nat Hum Behav. 2020 Jul 1;4(7) doi: 10.1038/s41562-020-0906-x. [Internet] [cited 2021 Mar 15], 677–87. Available from: [DOI] [PubMed] [Google Scholar]
- 30.Hu L.T., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. http://record/1998-03102-001 [Internet] [cited 2021 Feb 22] Available from: [Google Scholar]
- 31.Hair J.F., Black W., University L.S., Babin B.J., University L.T., Anderson R.E. 2010. Multivariate data analysis: a global Perspective | request PDF.https://www.researchgate.net/publication/237009923_Multivariate_Data_Analysis_A_Global_Perspective [Internet]. Person. [cited 2021 Feb 22]. Available from: [Google Scholar]
- 32.Tabachnick B.G., Fidell Linda S. fifth ed. PsycNET; 2007. Using multivariate statistics.https://psycnet.apa.org/record/2006-03883-000 [Internet] [cited 2021 Feb 22]. Available from: [Google Scholar]
- 33.Fornell C., Larcker D.F. Evaluating structural equation models with unobservable variables and measurement error. J Market Res. 1981 Feb 28;18(1):39–50. http://journals.sagepub.com/doi/10.1177/002224378101800104 [Internet] [cited 2021 Apr 10] Available from: [Google Scholar]
- 34.Wong M.C.S., Wong E.L.Y., Huang J., Cheung A.W.L., Law K., Chong M.K.C. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–1156. doi: 10.1016/j.vaccine.2020.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodram B. Trust in a COVID-19 vaccine in the U.S.: a social-ecological perspective. Soc Sci Med. 2021;270(January):113684. doi: 10.1016/j.socscimed.2021.113684. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdul K., Mursheda K. 2021. Munich Personal RePEc Archive knowledge , attitude and acceptance of a COVID-19 Vaccine: a global Cross-Sectional study. (105236) [Google Scholar]
- 37.Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021 Feb 12;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health. 2020 Oct 23;5(10):4206. doi: 10.1136/bmjgh-2020-004206. http://gh.bmj.com/ [Internet] [cited 2021 Mar 10] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang J., Featherstone J.D., Calabrese C., Wojcieszak M. Effects of fact-checking social media vaccine misinformation on attitudes toward vaccines. Prev Med. 2021 Apr 1;145:106408. doi: 10.1016/j.ypmed.2020.106408. [DOI] [PubMed] [Google Scholar]
- 40.Kwok K.O., Li K.K., Wei W.I., Tang A., Wong S.Y.S., Lee S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int J Nurs Stud. 2021:114. doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]