Abstract
Cancer immunotherapy, which suppresses cancer progression by activating the anti-cancer immunity of patients, shows utility in treating multiple types of cancers. Immunogenic cell death (ICD) induced by most clinical treatment modalities plays a critical role in promoting cancer immunotherapy by releasing tumor-associated antigens and neoantigens and exposing “danger signals” to stimulate immune cells. This comment article presents the different roles of nanoparticles in various treatment modalities of cancers, including chemotherapy, radiotherapy, photodynamic and photothermal therapies, and therapy with radiated tumor cell-released nanoparticles, which often activate anti-cancer immunological effects by inducing ICD of cancer cells, and highlights the challenges and opportunities of ICD-related cancer immunotherapy in the clinic.
Keywords: Immunogenic cell death, Nanoparticle, Nanoformulation, Immunotherapy, Multimodal cancer therapy
Graphical abstract
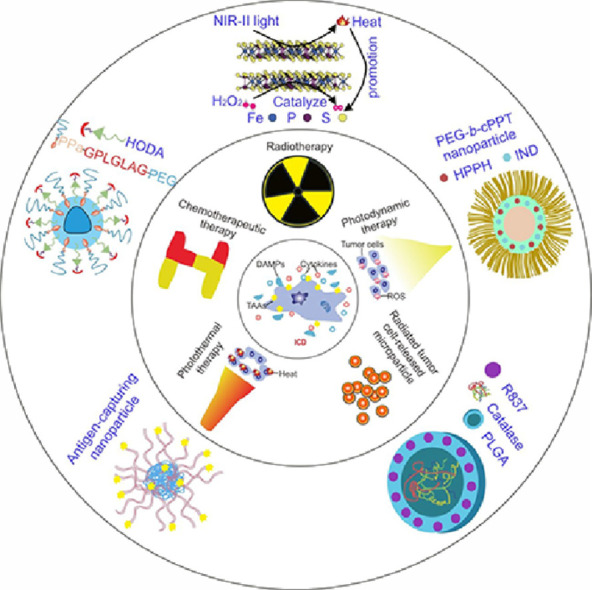
An essential concept of cancer immunotherapy is that immunogenic cell death (ICD), characterized by the release of tumor-associated antigens (TAAs) and tumor-specific antigens (TSAs) like neoantigens, danger-associated molecular patterns (DAMPs), and pro-inflammatory cytokines, facilitates the presentation of TAAs and TSAs to adaptive immune cells, eliciting an emerging or reinstating a pre-existing anti-cancer immune response. In many cancer types, accumulative clinical evidence indicates that ICD-related DAMPs, such as membrane-bound calreticulin expression and heat-shock proteins 70 and 90, not only correlate with the recruitment or activation of anti-cancer immune cells but are also positive prognostic biomarkers for cancer patients [1]. An ideal situation for cancer therapy is to activate systematic immunity while killing the cancer cells, and this might be facilitated by inducing a high level of ICD in the tumors. Nanoparticles are well-suited to deliver ICD-inducing drugs and antibodies to the tumors and improve the activity of reagents, regulating the tumor microenvironment (TME) and boosting immune response [2]. Nanoparticles can modulate the pharmacokinetics and biodistribution of ICD-inducing agents, thereby potentially offering clinical utility to ICD-related cancer immunotherapy.
1. Chemotherapy with nanoparticles to induce ICD for cancer immunotherapy
Chemotherapeutic drugs, such as anthracyclines (e.g., mitoxantrone, doxorubicin, daunorubicin, epirubicin, and idarubicin), taxanes (e.g., paclitaxel and docetaxel), oxaliplatin, cyclophosphamide, bleomycin, and bortezomib, all induce ICD reportedly [3,4]. Liposomes, polymer nanoparticles, inorganic nanoparticles, and tumor cell-derived nanoparticles are capable of delivering these immunogenic chemotherapeutic drugs to tumor sites. Furthermore, nanoparticles can be designed to assist with the combination of immunogenic chemotherapeutic drugs and anti-programmed cell death-1 (anti-PD-1), anti-programmed cell death-ligand 1 (anti-PD-L1), or anti-CD47 antibodies to propagate the anti-cancer immunity of ICD [5,6]. Research on the combination of nanoparticle-mediated cancer immunotherapy could also examine how nanoparticles release their payload, specifically within the TME. A folate-decorated liposome with a matrix metalloprotease 2-degradable shell of poly(ethylene glycol) (PEG) has been developed to deliver the ICD inducer doxorubicin for treatment of breast cancer [7].
2. Radiotherapy with nanoparticles to trigger ICD for cancer immunotherapy
Radiation in radiotherapy, including X-ray, radioisotopes (γ-ray, α-particles, and β-particles), protons, heavy ions, and electron beams, can induce ICD by directly breaking deoxyribonucleic acid (DNA) structures or by generating reactive oxygen species (ROS), further damaging DNA. Following radiotherapy, released DAMPs recruit immune cells to activate the immune system [8]. However, the efficacy of anti-cancer immunity in response to radiotherapy alone is always limited, owing to the insufficient number of dendritic cells (DCs) and the existence of immunosuppressive cells or factors. To amplify the immune effect, Wang and co-workers developed antigen-capturing poly(lactic-co-glycolic acid) nanoparticles (PLGA NPs), modifying their surfaces to enable binding to tumor antigens through various mechanisms. For example, unmodified PLGA NPs bind to proteins through non-covalent hydrophobic interactions, while PLGA NPs coated with maleimide PEG bind to proteins via the formation of stable thioether bonds [9]. To counter immunosuppressive factors, Liu's group developed a core−shell PLGA nanoparticle by loading catalase inside the inner core and Toll-like receptor (TLR) 7 agonist in the shell, which enhanced the efficacy of radiotherapy by relieving hypoxia in the tumor [10].
3. Phototherapy with nanoparticles to induce ICD for cancer immunotherapy
Both photodynamic (PDT) and photothermal therapy (PTT) induce the ICD of cancer cells and generate anti-cancer immune effects, leading to high treatment efficacy with minimal side effects, owing to the accurate application of light to the tumors. Photothermal and photodynamic reagents can also be co-loaded with immunostimulators, immunogenic chemotherapeutic drugs, or anti-cancer peptides for effective combination treatments. For example, honey bee venom melittin peptides have been co-loaded with chlorin e6 (Ce6) into an organic−inorganic hybrid nanoparticle for enhanced Ce6 penetration and ICD level [11]. PDT has been approved clinically by numerous regulatory agents for the treatment of local tumors like esophageal cancer. However, this treatment causes sunlight sensitivity for several weeks, resulting in photo-sensitive dermatitis when exposed to sunlight. The use of aggregation-induced emission (AIE) agents, which fluoresce brightly in a dense, aggregated state as an emerging class of fluorescent reagents, have the potential for use in cancer immunotherapy. Some AIE agents are effective to produce intracellular ROS and cause strong ICD of tumor cells.
Additionally, hypoxia in TME limits PDT efficacy, which requires oxygen to generate ROS and kill cancer cells. Lan et al. established a unique nanoplatform consisting of Fe-TBP (TBP = 5,10,15,20-tetra (p-benzoate) porphyrin) and Fe3O clusters, that can decompose intracellular hydrogen peroxide (H2O2) to produce oxygen through a Fenton-like reaction under hypoxic conditions, causing more than 90% regression of the tumors when combined with anti-PD-L1 antibody [12]. ROS production is essential to instigate the intracellular danger signaling pathways that govern ICD [13]. For PTT, the main limitations are appropriate radiation dose and the high photothermal conversion efficiency of PTT agents with excellent biocompatibility and biodegradability. Combining PTT agents with imaging technology could assist in determining the best radiation dose and best time point of treatment. Chen et al. identified a highly efficient near-Infrared-II (NIR-II) PTT agent, based on liquid-exfoliated FePS3 nanosheet, with a photothermal conversion efficiency of up to 43%, among the highest reported levels in typical PTT agents [14]. Moreover, increasing the accumulation of PTT agents in the tumor is essential for improved PTT efficacy, which further increases the ICD of tumor cells.
4. Multifunctional nanoparticles to trigger ICD for cancer immunotherapy
In recent years, “all in one” multifunctional nanoparticles, which amplify anti-cancer effects from different aspects, such as inducing ICD of tumor cells, while recruiting immune cells or regulating inhibitory TME, to improve cancer immunotherapy efficacy have been established. Chen et al. designed a smart self-assembled nanovesicle from pH-responsive copolymer poly(ethylene glycol)-block-cationic polypeptide (PEG-b-cPPT) to encapsulate photosensitizer and inhibitor of indoleamine 2,3-dioxygenase (IDO), indoximod (IND), via hydrophobic interaction. After laser irradiation, this smart nanoparticle killed cancer cells by ROS, and recruited DCs and promoted their antigen presentation ability to T cells for immune activation. Moreover, the released IND modulated the TME to reverse the immunosuppressive microenvironments [15]. This smart nanoparticle is a promising tool for cancer immunotherapy and highlights the potential of rational nanoparticle design.
5. Autologous tumor cell-derived nanoparticles to induce ICD for cancer immunotherapy
In addition to the design of synthetic nanoparticles, some nanoparticles are secreted by cancer cells themselves under special circumstances and exhibit effective anti-cancer properties. Yang et al. reported that radiated tumor cell-released microparticle (RT-MP) showed a broad anti-cancer effect and caused ICD mainly through the ferroptosis pathway. In the investigation, the diameter of RT-MP was about 500 nm, an appropriate size to be taken up by macrophages. After intrapleural administration, RT-MP polarized microenvironmental M2 tumor-associated macrophage (M2-TAM) to M1-TAM in a malignant pleural effusion (MPE) mouse model, conferring an ablative effect against MPE [16]. However, the exact substances involved in inducing ICD of cancer cells and reprogramming TAM remain unknown. For nanoparticles that just cause ICD of tumor cells, it is necessary to avoid being uptaken by phagocytic myeloid cells as far as possible to make sure more nanoparticles reach the tumor site. If nanoparticles can regulate or reprogram phagocytes after being swallowed and also cause ICD of tumor cells after going inside of tumor cells, they will provoke anti-cancer immunity and inhibit tumor growth. Our group showed that RT-MP had effects on both tumor cells and macrophages, and such nanoparticles are worthy of further exploration.
6. Barriers to clinical translation of nanoparticles for cancer immunotherapy
AbraxaneⓇ (paclitaxel), DoxilⓇ (doxorubicin), Ferumoxytol (iron oxide nanoparticle), Onivyde (irinotecan), and many other nanoformulations have seen clinical and commercial success in treating multiple types of cancers. Still, promising preclinical results do not always translate to the clinic. A thermo-sensitive liposome formulation that showed excellent efficacy in mouse models and was tested for its effectiveness in phase III clinical trial was less effective in the clinic. The optimal conditions found in animal studies are not usually effective for clinical application. Improved in vitro and animal models, which can provide accurate predictions on the efficacy of nanoparticles in humans, are required. For clinical translation, the treatment choice should be considered more comprehensively. For example, when using chemotherapeutic drugs, we should consider not only the killing effect on tumor cells but also the effect on other stromal and immune cells, or consider whether the combination use of drugs that help activate immunity or regulate inhibitory TME can amplify the anti-cancer effect. There is, therefore, still a long way for more nanoparticles to go from the “bench to the bedside”.
7. Conclusions and prospects
ICD plays an essential role in nanoparticle-mediated cancer immunotherapy. More cell death forms, such as anoikis, autophagy, pyroptosis, ferroptosis, necroptosis, parthanatos, and NETosis, have been detected during the last decades, and more efforts are needed to identify compounds or modalities that induce ICD. An ideal ICD inducer is supposed to be an efficient instigator of cell death, capable of inducing the release of multiple types of DAMPs (high mobility group protein B1, calreticulin (CRT), adenosine triphosphate (ATP), etc.), TLR agonists (mitochondrial DNA, ribonucleoproteins, histones, etc.), and immunogenic signals (interleukin-1α (IL-1α), interleukin-33 (IL-33), etc.), and capable of inducing endoplasmic reticulum (ER) stress and ROS production, which would make it possible to improve DAMPs trafficking and to increase their release.
ICD inducers are expected to be considered for the design of anti-cancer nanoparticles. There should, hence, be diverse nanoplatforms for different cancers based on the understanding of the limitation of different treatment modalities and the complexity of TME, to select the best combinational approach. Effort must still be made to fully exploit nanoparticle platforms that are suitable for clinical translation with high accumulation in the tumors and manufacturing scalability that can enhance tissue localization, cell permeability, and anti-cancer immune response after systemic administration.
When used reasonably, the intratumoral injection can cause direct contact with tumor cells and lead to their ICD more effectively and efficiently, provoking a more robust immune response than intravenous delivery. In some cases, the intratumoral injection can not only effectively cause ICD against local tumors but also activate systemic anti-cancer immunity against distant metastases. Intratumoral injections suffer from variability, however, and achieving homogenous distribution of the injected compound throughout the tumor is not possible. For intravenous delivery, nanoparticles go to tumors through blood circulation and have an effect on metastatic tumors, but the percentage of the administered drug reaching the tumors is low, and intravenous delivery has more side effects than intratumoral injection. Systemic administration is the approach used in clinical practice.
Since cancer is considered as a chronic inflammatory disease, designing highly effective targeted nanoplatforms for ICD will not only reduce the incidence rate of drug resistance and adverse side effects but also activate immune cells to destroy cancer cells further and produce more pro-inflammatory cytokines in TME; this guarantees patient's safety and therapy efficiency and remarkably promotes the development of clinical cancer immunotherapy in the foreseeable future.
Conflicts of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgment
The work was financially supported by the National Natural Science Foundation of China (Nos. 81874233 and 51873207) and the Natural Science Foundation of Hubei Province (No. 2019CFB465).
Contributor Information
Honglin Jin, Email: jin@hust.edu.cn.
Jianxun Ding, Email: jxding@ciac.ac.cn.
References
- 1.Fucikova J, Moserova I, Urbanova L, Bezu L, Kepp O, Cremer I. Prognostic and predictive value of DAMPs and DAMP-associated processes in cancer. Front Immunol. 2015;6:402. doi: 10.3389/fimmu.2015.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feng X, Xu W, Li Z, Song W, Ding J, Chen X. Immunomodulatory nanosystems. Adv Sci. 2019;6(17) doi: 10.1002/advs.201900101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garg AD, More S, Rufo N, Mece O, Sassano ML, Agostinis P. Trial watch: Immunogenic cell death induction by anti-cancer chemotherapeutics. Oncoimmunology. 2017;6(12) doi: 10.1080/2162402X.2017.1386829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Q, Chen MC, Liu Z. Local biomaterials-assisted cancer immunotherapy to trigger systemic anti-tumor responses. Chem Soc Rev. 2019;48(22):5506–5526. doi: 10.1039/c9cs00271e. [DOI] [PubMed] [Google Scholar]
- 5.Zhou FY, Feng B, Yu HJ, Wang DG, Wang TT, Ma YT. Tumor microenvironment-activatable prodrug vesicles for nanoenabled cancer chemoimmunotherapy combining immunogenic cell death induction and CD47 blockade. Adv Mater. 2019;31(14) doi: 10.1002/adma.201805888. [DOI] [PubMed] [Google Scholar]
- 6.Li L, Li YC, Yang CH, Radford C, Wang JW, Janat-Amsbury M. Inhibition of immunosuppressive tumors by polymer-assisted inductions of immunogenic cell death and multivalent PD-L1 crosslinking. Adv Funct Mater. 2020;30(13) doi: 10.1002/adfm.201908961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deng CF, Zhang Q, Jia MD, Zhao J, Sun X, Gong T. Tumors and their microenvironment dual-targeting chemotherapy with local immune adjuvant therapy for effective antitumor immunity against breast cancer. Adv Sci. 2019;6(6) doi: 10.1002/advs.201801868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Li Z, Wang Z, Yu Y, Li D, Li B. Nanomaterials for combinational radio-immuno oncotherapy. Adv Funct Mater. 2020 [Google Scholar]
- 9.Min YZ, Roche KC, Tian SM, Eblan MJ, McKinnon KP, Caster JM. Antigen-capturing nanoparticles improve the abscopal effect and cancer immunotherapy. Nat Nanotechnol. 2017;12(9):877–884. doi: 10.1038/nnano.2017.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Q, Chen JW, Yang ZJ, Xu J, Xu LG, Liang C. Nanoparticle-enhanced radiotherapy to trigger robust cancer immunotherapy. Adv Mater. 2019;31(10) doi: 10.1002/adma.201802228. [DOI] [PubMed] [Google Scholar]
- 11.Liu HJ, Hu Y, Sun YJ, Wan C, Zhang ZJ, Dai XM. Co-delivery of bee venom melittin and a photosensitizer with an organic-inorganic hybrid nanocarrier for photodynamic therapy and immunotherapy. ACS Nano. 2019;13(11):12638–12652. doi: 10.1021/acsnano.9b04181. [DOI] [PubMed] [Google Scholar]
- 12.Lan GX, Ni KY, Xu ZW, Veroneau SS, Song Y, Lin WB. Nanoscale metal-organic framework overcomes hypoxia for photodynamic therapy primed cancer immunotherapy. J Am Chem Soc. 2018;140(17):5670–5673. doi: 10.1021/jacs.8b01072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krysko DV, Garg AD, Kaczmarek A, Krysko O, Agostinis P, Vandenabeele P. Immunogenic cell death and DAMPs in cancer therapy. Nat Rev Cancer. 2012;12(12):860–875. doi: 10.1038/nrc3380. [DOI] [PubMed] [Google Scholar]
- 14.Zhang QH, Guo QB, Chen Q, Zhao XX, Pennycook SJ, Chen HR. Highly efficient 2D NIR-II photothermal agent with Fenton catalytic activity for cancer synergistic photothermal chemodynamic therapy. Adv Sci. 2020;7(7) doi: 10.1002/advs.201902576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang WJ, Zhang FW, Deng HZ, Lin LS, Wang S, Kang F. Smart nanovesicle-mediated immunogenic cell death through tumor microenvironment modulation for effective photodynamic immunotherapy. ACS Nano. 2020;14(1):620–631. doi: 10.1021/acsnano.9b07212. [DOI] [PubMed] [Google Scholar]
- 16.Wan C, Sun Y, Tian Y, Lu L, Dai X, Meng J. Irradiated tumor cell-derived microparticles mediate tumor eradication via cell killing and immune reprogramming. Sci Adv. 2020;6(13) doi: 10.1126/sciadv.aay9789. eaay9789. [DOI] [PMC free article] [PubMed] [Google Scholar]


