Abstract
Objective
To use quantitative and qualitative methods to characterize the work patients with type 2 diabetes mellitus (T2DM) enact and explore the interactions between illness, treatment, and life.
Patients and Methods
In this mixed-methods, descriptive study, adult patients with T2DM seen at the outpatient diabetes clinic at Mayo Clinic in Rochester, Minnesota, from February 1, 2016, through March 31, 2017, were invited to participate. The study had 3 phases. In phase 1, the Patient Experience with Treatment and Self-management (PETS) scale was used to quantify treatment burden. In phase 2, a convenience sample of patients used a smartphone application to describe, in real time, time spent completing diabetes self-management tasks and to upload descriptive digital photographs. In phase 3, these data were explored in qualitative interviews that were analyed by 2 investigators using deductive analysis.
Results
Of 162 participants recruited, 160 returned the survey (phase 1); of the 50 participants who used the smartphone application (phase 2), we interviewed 17 (phase 3). The areas in which patients reported highest treatment burden were difficulty with negotiating health services (eg, coordinating medical appointments), medical expenses, and mental/physical exhaustion with self-care. Participants reported that medical appointments required about 2.5 hours per day, and completing administrative tasks related to health care required about 45 minutes. Time spent on health behaviors varied widely—from 2 to 60 minutes in a given 3-hour period. Patients’ experience of a task’s burden did not always correlate with the time spent on that task.
Conclusion
The most burdensome tasks to patients with T2DM included negotiating health care services, affording medications, and completing administrative tasks even though they were not the most time-consuming activities. To be minimally disruptive, diabetes care should minimize the delegation of administrative tasks to patients.
Abbreviations and Acronyms: CuCoM, cumulative complexity model; HbA1c, hemoglobin A1c; PETS, Patient Experience with Treatment and Self-management; T2DM, type 2 diabetes mellitus
About 30 million Americans live with type 2 diabetes mellitus (T2DM). These patients must deal with the symptoms and functional limitations caused by the disease itself and with its treatment. Treatment competes with other life demands for patients’ time, energy, and attention, can be disruptive of existing routines, and may be difficult to enact.1 Yet to benefit from treatment, patients must embed these treatments in their daily routines with fidelity.2
Living with T2DM and its treatment may require considerable work on the part of patients, and their ability to do this work is limited by their capacity to enact it. This scenario is described in the cumulative complexity model (CuCoM). The capacity to do patient work is drawn from the same capacity to do the work of everyday life—eg, formal paid work, parenting and other caregiving, volunteering, and hobbies.3 When the workload of care exceeds the mobilizable capacity to shoulder it, it becomes burdensome and causes disease. This treatment burden is associated with both reductions in well-being and poor treatment fidelity.4, 5, 6
Despite its importance, how patients experience the dynamic interaction between treatment workload and capacity remains poorly understood.7 Some patients with seemingly limited capacity appear to handle patient work with ease, whereas asymptomatic and well-resourced patients facing a lighter workload struggle. A better understanding of patient work can help make health care services and treatments less disruptive and mitigate the suffering caused by the cumulative burden of treatment.
In this study, we describe the experience of living with T2DM and identify areas of high treatment burden. Using real-time data collection through a smartphone, we captured the time patients spent on health-related activities and photographs participants chose to take and share with us. We explored both data and photographs with participants during in-depth interviews designed to understand patient work and the sources of capacity from which patients drew to enact this work and minimize the disruption to their lives.
Patients and Methods
Study Design
This study had 3 phases. Phase 1 assessed the burden of treatment in patients with T2DM (paper survey). All phase 1 participants were invited to participate in phase 2, in which patients used a smartphone application to record estimates of the time they spent on diabetes management and to take photographs of that work. During phase 3, we conducted in-depth interviews with a convenience sample of participants from phase 2.
Participants and Setting
Adult patients (≥18 years old) with T2DM visiting the diabetes clinic at Mayo Clinic in Rochester, Minnesota, were identified from clinic calendars and recruited from February 1, 2016, through March 31, 2017. Potential participants were approached while waiting for their medical appointment in an examination room or after their medical appointment. Study procedures took place in a designated unoccupied clinic room.
Phase 1
Enrolled participants reported demographic characteristics and completed the Medical Outcomes Study self-rated health item8 and the Patient Experience with Treatment and Self-management (PETS) questionnaire.6,9 The self-rated health item asks participants to rate their health as “excellent,” “very good,” “good,” “fair,” or “poor.” Worse self-rated health has been associated with higher mortality.10 The PETS scale has 9 subscales assessing treatment burden in the domains of (1) health care expenses, (2) health care services, (3) interpersonal challenges, (4) medications, (5) medical information, (6) medical appointments, (7) medical/physical toll/exhaustion, (8) monitoring health, and (9) role and social activities. Variables extracted from the electronic medical record included comorbidities (to estimate the Charlson comorbidity index score),11 number of medications, diabetes treatment regimen, race and ethnicity, and most recent hemoglobin A1c (HbA1c) level.
Phase 2
During a 1-week period, participants used the smartphone application Metricwire to answer questions in real time about how much time they allocated to managing diabetes and to take and upload photographs.12 Participants received help downloading the application, written instructions, and a contact number.
The questions addressed care recommendations from the American Diabetes Association,13 with input from members of our diabetes patient advisory group. This group also piloted and provided feedback on the smartphone application interface (Supplemental Figure 1, available online at http://mcpiqojournal.org), including the implementation of a user-selected schedule for receiving survey prompts (rather than receiving the prompts at random times) to improve study acceptability. Participants received 10 prompts within a 1-week period that asked about the time spent self-managing diabetes. At the end of day 1 (the day of their medical appointment and recruitment), participants were queried about time spent at health care appointments. On 3 days in the same week, twice per day, patients were asked about time spent on health behaviors in the 3 hours before receiving the prompt; these health behaviors included taking and managing medications, monitoring their health (eg, checking blood sugar level and feet), and enacting physical activity and other health behaviors (eg, exercising, cooking diabetes-friendly meals). End-of-day prompts on those 3 days asked about health behaviors in the previous 3 hours and asked about time spent on administrative tasks at any time during the day: dealing with insurance and pharmacy, filling prescriptions, obtaining medical supplies, communicating with a health care professional, or scheduling health care appointments. Participants selected the morning, afternoon, and evening prompt times from a set of 3 schedules. Participants were informed that surveys would be open for completion within 60 minutes of the scheduled prompt times. This approach was used to minimize hoarding and backfilling, a common problem in diary data collection.14 Supplemental Table 1 (available online at http://mcpiqojournal.org) provides an example of the smartphone application prompt schedule.
Participants were also asked to take and upload 5 or more photographs during the week of the study. Via the smartphone application, participants could engage in reflexive photography, taking multiple photographs before uploading and sharing with study staff. This feature enabled participants to control topics discussed with regard to their illness experience.15,16 They were asked to take pictures that could illustrate “how they manage diabetes in their day-to-day life,” a prompt adapted from Rich et al.17
Phase 3
All participants from phase 2 were invited to complete in-depth interviews, usually on a day when they had a scheduled follow-up appointment. To minimize patients’ preferences for giving reports that would be favorably perceived by the diabetes care team, the interviewer (G.S.-B.) explicitly stated that she was not part of that team. Interviews were performed in the clinic (eg, in a private office) or over the phone.
Given the paucity of knowledge about treatment burden and the disruption it can cause for patients with T2DM, both of which are issues fundamentally rooted in each person’s experience, we deemed data-prompted interviewing as appropriate to explore the meaning and discuss implications of the data collected with participants.18 Supplemental Table 2 (available online at http://mcpiqojournal.org) provides the interview guide used to inform the qualitative interviews. The quantitative data (PETS scale response and time-use responses) and uploaded photographs were used to elicit interview topics, jog a participant’s memory when answering open-ended questions, or prompt questions the investigators may not have thought to ask.18,19
Statistical Analyses
We performed a mixed-methods study with a sequential explanatory design. Statistical analyses were conducted using JMP Pro, version 10.0.0 (SAS Institute). We dichotomized the sample by the patient’s level of glycemic control (HbA1c <8% vs ≥8%).20 We prorated the scores of PETS subscales in which at least 50% of items were available.6 Each scale score was then transformed to a 0 to 100 scale. We performed exploratory analyses comparing mean PETS subscales scores across glycemic control groups using a 2-sided Student t test with α level set at .05.
We recruited participants to meet a phase 2 goal of 50 patients to account for a previously described smartphone application survey completion rate of 50% at 3 days.21 This method provided enough participants to apply the central limit theorem to descriptive statistics. Qualitative data, elicited from the quantitative results and photographs, were used to add depth to the quantitative findings; they helped explain the aspects of health care that patients found most burdensome as well as positive aspects of diabetes self-management. Coders (C.G., G.S.-B., V.S.) used deductive analyses to classify participant statements into the 9 PETS domains. A codebook with calibrated examples was generated using 2 interviews. New codes were generated when data were not able to be coded in the 9 PETS domains and were discussed by the coders.
Results
Patient Characteristics and Treatment Burden
Of 184 eligible patients invited, 162 agreed to participate in our study and 160 returned the survey (phase 1), 116 of whom had smartphones. Of these 116, 50 agreed to enroll in the smartphone portion of the study, and 45 provided data through the application (Supplemental Figure 2, available online at http://mcpiqojournal.org). The Table describes the characteristics of the 162 patients who agreed to participate in phase 1. Participants were similar across glycemic control categories except that fewer patients with HbA1c levels of less than 8% were receiving insulin therapy (39% [37 of 95] vs 72% [48 of 67]). Supplemental Table 3 (available online at http://mcpiqojournal.org) describes the characteristics of the participants enrolled in phase 2. There were no important differences between the characteristics of the whole cohort and the patients who participated in phase 2.
Table.
| Variable | HbA1c <8% (n=95) | HbA1c ≥8% (n=67) |
|---|---|---|
| Age (y) | 62 (56-71) | 65 (54-70) |
| Women | 36 (38) | 25 (37) |
| Diabetes duration (y) | 9 (3-16) | 12.5 (6-20.75) |
| HbA1c | 6.8% (6.2%-7.3%) | 9.5% (8.4%-10.6%) |
| No. of medications | 12 (8-16) | 11 (7-5.25) |
| Prescribed insulin | 37 (39) | 48 (72) |
| Charlson comorbidity index score | 5 (4-7) | 5 (4-6) |
| Race and ethnicity | ||
| Asian | 0 | 1 (1.5) |
| Black | 1 (1) | 3 (5) |
| Native American | 1 (1) | 0 |
| Other/unknown | 6 (6) | 7 (11) |
| White, Latino/a | 3 (3) | 1 (1.5) |
| White, non-Latino/a | 84 (87) | 55 (82) |
| Marital status | ||
| Divorced | 6/93 (6) | 5/66 (8) |
| Married | 71/93 (76) | 48/66 (73) |
| Member of unmarried couple | 4/93 (4) | 2/66 (3) |
| Never been married | 6/93 (6) | 7/66 (11) |
| Widowed | 6/93 (6) | 4/66 (6) |
| Employment status | ||
| Homemaker | 2 (2) | 3 (5) |
| Employed | 51 (55) | 29 (44) |
| Out of work | 3 (3) | 1 (1.5) |
| Student | 0 | 2 (3) |
| Unable to work | 7 (8) | 7 (11) |
| Retired | 30 (32) | 24 (36) |
| Annual household income | ||
| <$20,000 | 5 (6) | 4 (7) |
| $20,000-$34,999 | 9 (10) | 11 (19) |
| $35,000-$49,999 | 5 (6) | 7 (12) |
| $50,000-$74,999 | 13 (15) | 11 (19) |
| $75,000-$99,999 | 10 (11) | 5 (9) |
| $100,000-$149,999 | 20 (23) | 10 (17)) |
| $150,000-$199,999 | 9 (10) | 5 (9) |
| ≥$200,000 | 17 (19) | 5 (9) |
| Self-rated health | ||
| Excellent | 4 (4) | 3 (5) |
| Very good | 24 (26) | 15 (23) |
| Good | 34 (37) | 27 (41) |
| Fair | 23 (25) | 15 (23) |
| Poor | 8 (9) | 6 (9) |
HbA1c, hemoglobin A1c; IQR, interquartile range.
Data are presented as No. (percentage) of participants or median (IQR).
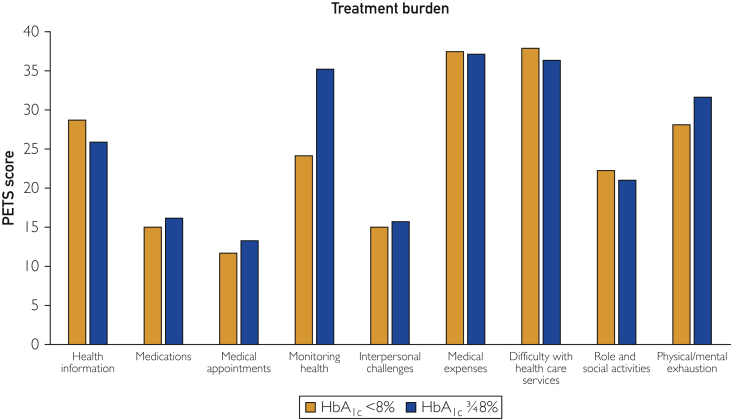
Patients reported the highest treatment burden in the domains of medical expenses, difficulty with health services, and physical and mental exhaustion related to self-care (Figure) (n=162). We found no differences in PETS scores between glycemic control groups, except in the “monitoring health” domain, which was 11 points more burdensome for patients with higher HbA1c levels (P=.001).
Figure.
Treatment burden stratified by Patient Experience with Treatment and Self-management domains. HbA1c, hemoglobin A1c; PETS, Patient Experience with Treatment and Self-management.
Phase 1 participants reported visiting their “diabetes doctor” a median of twice per year (n=160). Phase 2 participants reported spending a median of 2.5 hours per visit traveling, waiting, and participating in a medical appointment (n=50). When patients reported completing administrative tasks such as dealing with insurance and pharmacy, filling prescriptions, and obtaining medical supplies, these tasks took a median of 45 minutes (n=50). In a 3-hour period, participants reported spending 2 to 60 minutes on health behaviors: a median of 9 minutes dealing with medications, 5 minutes monitoring their health, and 30 minutes on other health activities (eg, exercising, shopping for diabetes-friendly foods) (n=160).
In-depth Interviews
Seventeen patients participated in the in-depth interviews exploring how participants construct self-care activities as burdensome.
Medical Expenses
Participants reporting high treatment burden due to medical expenses described ways in which they had to adjust their self-care to be able to enact their physician’s recommendations. One participant described the transition to living with a diabetes management regimen and how it required physical space and financial resources that must be intentionally allocated to diabetes care (Supplemental Figure 3, Supplemental Table 4 [part A], available online at http://mcpiqojournal.org). Notably, participants in this study seldom mentioned foregoing diabetes self-care activities altogether because of their cost. Instead, participants deliberately modified self-care independent of physician input to comply with their financial realities. For one patient, this meant rationing and reusing diabetes monitoring supplies (Supplemental Table 4 [part B]).
Patients negotiated the boundaries of conventional medical recommendations and innovated outside them to afford their medications and supplies. For a patient, the work of affording diabetes management medications meant searching across formal and informal sources for affordable insulin, daring encounters with strangers to obtain these essential medicines, and prioritizing glycemic control over pain management (Supplemental Table 4 [part C]). This patient endorsed that her cost savings allowed her to provide for her family. When her adult children discovered her strategy, however, it created substantial tension in their interpersonal relationships.
Difficulty With Health Services
Participants described burden from health services in situations that required frequent interaction with health care staff, especially when visits could have been consolidated. For one patient, lack of consolidation represented a nuisance (Supplemental Table 4 [part D]). For another patient, who was recently hospitalized and was experiencing substantial burden of illness, health care fragmentation hindered her ability to coordinate her own care. This patient later described how her inability to enact the physician’s instructions to schedule an urgent medical procedure created tension in the patient-physician relationship (Supplemental Table 4 [part E]).
Mental Exhaustion Related to Self-care. Many Patients Described Exhaustion Indirectly
A patient living with multiple chronic conditions reflected on the mental toll of dealing with intensive treatment regimens (Supplemental Figure 4 [available online at http://mcpiqojournal.org], Supplemental Table 4 [part F]). She described the work of health care and its effect on her mental well-being as private, something she actively minimizes and does not mention even to her clinicians.
New Theme: Activities That Boost Capacity
Although lifestyle changes (diet and exercise) are not part of the PETS survey, these activities often appeared in patients’ uploaded photographs. Patients, even those who asserted that they were not enacting lifestyle changes, discussed these activities positively, never as burdensome. Patients often described finding pleasure and meaning in adopting healthy habits such as spending time with pets, restarting old hobbies, or taking up new activities such as swimming or gardening (Supplemental Figure 5 [available online at http://mcpiqojournal.org], Supplemental Table 4 [part G]).
Discussion
Summary of Findings
In this sample of patients with T2DM receiving specialty care, we found that the areas of highest treatment burden were difficulty negotiating access to health care services, affording medical expenses, mental and physical exhaustion from self-care, and—particularly for patients with HbA1c levels of 8% or higher, many of whom used insulin—monitoring their health. Administrative tasks and attending medical appointments were the most time-consuming activities, requiring a median of 45 minutes and 2.5 hours, respectively, on days when they were performed. Although the infrequent activities that required greatest time investments—administrative tasks and medical appointments—were also the most burdensome, time alone does not appear to fully explain their contribution to treatment burden. For instance, in qualitative interviews, patients did not describe lifestyle changes requiring greater time investments every day as burdensome. Activities with high administrative complexity may be burdensome in part because they allow for minimal discretion in the ways patients allocate time and energy. Also, our findings placing administrative chores and healthy lifestyle activities at opposite ends of the burden spectrum suggest that tasks patients value more may be perceived as less burdensome.
Also consistent with the CuCoM, we found that patients with poor glycemic control and more likely to be using insulin, ie, sicker patients with less capacity and facing more work, were more likely to feel burdened by self-monitoring tasks. Similarly, our qualitative data provided examples of treatment burden interactions with scarcity and illness burden—both factors that in the CuCoM reduce patient capacity. Although health care activities such as affording and coordinating health care can be a nuisance to a relatively healthier patient, for a sicker one these activities become impracticable or demand precarious trade-offs. Connections between the different domains of treatment burden arose in interviews; financial and health care coordination challenges could lead to interpersonal conflict with family members or health care personnel. Negotiating through and working to resolve these conflicts increases the treatment workload, further taxing the patient’s capacity and increasing the burden of treatment.
Comparison With Previous Studies
Similar to previous qualitative studies, we found that patients preferred terms other than burden to describe difficulties with health care and self-care.22 Patients instead used terms like frustrating or a pain and described “running from” activities they found burdensome.
Our findings on treatment burden and time use are consistent with those of previous studies. The PETS scale validation data (when assessed in patients with any chronic condition) revealed the highest treatment burden in the domains of difficulty with health services delivery, medical expenses, and mental and physical exhaustion from self-care.6 A subsequent validation in primary care cohorts reported scores similar to those in our cohort of patients and was able to document higher burden in unmarried patients and those with less education, lower income, and worse health status.23 Estimates of diabetes care time requirements have ranged from 25 minutes per day to 122 minutes per day for health behaviors and approximately 2.2 hours per month for activities related to accessing and using health care services.13,24, 25, 26 It has been estimated that patients with 3 chronic conditions would have to spend 50 to 70 hours per month on health-related activities, with these time requirements increasing with additional comorbidities.26 We report similar estimates here: some patients may be spending over 2 hours per day on self-care without including time spent addressing administrative tasks and health care appointments.
Study Limitations and Strengths
We may have underestimated the burden of treatment because participants in this study had access to specialty care, were mostly either employed or retired, had access to a smartphone, and were willing and able to take part in the study (ie, overwhelmed patients may have been more likely to opt out). Furthermore, our findings may not generalize well to patients not referred to a specialty diabetes clinic, although the distribution of our PETS scores are consistent with those of a recently published population-based cohort from our clinic’s catchment area.23 We did not document material deprivation, health insurance, or literacy challenges in our participants, limiting our collection to self-reported highest education completed and income. Although the interviewer explicitly stated that she was not a part of the clinical care team during phase 3 interviews, patients may have provided desirable anecdotes. Similarly, given the proximity of the data collection period to the medical appointment, patients may have experienced higher motivation to participate in self-care and spent more time on these activities than usual. Strengths of this study were the implementation of methods to reduce the burden of participation and the application of a novel method of real-time data collection with an acceptable response rate to decrease recall bias in time estimates and better characterize patients’ day-to-day experience with diabetes management with real-time photographs. We used methodological triangulation to support the validity of our qualitative findings.27 The main strength of this study, however, lies in the depth of the data rather than their breadth, with our findings providing useful insights for improving patient care.
Implications
Our findings are widely consistent with the CuCoM and identify practical areas to support the practice of minimally disruptive medicine.1 This practice seeks to advance patient goals while minimizing the burden of treatment. Consistent with this practice, we have assessed the burden of treatment and identified areas such as health care services delivery and medical expenses as capable of overwhelming patients with T2DM. Although multimorbidity and trouble with medical expenses have been associated with higher treatment burden in all domains,28,29 patients with financial resources and in seemingly good health (or able to control indicators, such as HbA1c level) are also at risk of being overwhelmed by health care. This situation occurs because overwhelmed patients, to reconcile being unable to accomplish the recommended self-care work, may sacrifice safety or attempt to achieve health goals at the expense of other fulfilling activities. Therefore, clinicians may need to inquire about the steps required to enact self-care and whether they are feasible in patients’ lives, including the exploration of commonly reported areas of treatment burden such as medical expenses. Tools, such as the ICAN (Instrument for Patient Capacity Assessment) discussion aid, may uncover sources of burden and pleasure.30
Capacity coaching, a novel approach to health and wellness coaching rooted in the CuCoM and designed to help patients decrease the burdens of illness and treatment, bolster capacity, and adapt to life with illness and treatment may be integrated into primary care to help patients with T2DM and high treatment burden.31
Reducing the workload of treatment may result in improvements in other areas of patients’ lives such as mental well-being and interpersonal relationships, which, in turn, may reduce burden by improving capacity. Future interventions to improve the well-being of patients with T2DM should target medical expenses, the organization of health services, and the prevention and treatment of exhaustion with self-care.
Conclusion
Patients with T2DM spend substantial time doing patient work. Although patients with T2DM in our study spent about 2 hours per day in patient work, the most burdensome tasks were not necessarily those that took more time and included negotiating health care services, affording medications, and completing administrative tasks. Lack of control and meaning made some tasks more burdensome, particularly when faced by patients with limited capacity to enact them. Patients with T2DM experience substantial burden of treatment that reduces their well-being, much of which results from the way health care is organized and delivered and could be improved by implementing minimally disruptive medicine.
Ackowledgments
We thank Megan E. Branda, MS, for her insightful feedback on this project.
The content of this work is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Grant Support: Dr Spencer-Bonilla was supported by Clinical and Translational Science Awards grant TL1TR000137 from the National Center for Advancing Translational Sciences and grant 3R01HL131535-01S1 from the National Heart, Lung, and Blood Institute. Dr Montori was partially supported by grant UL1TR000135 from the National Center for Advancing Translational Sciences.
Potential Competing Interests: The authors report no competing interests.
Supplemental material can be found online at http://mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.May C., Montori V.M., Mair F.S. We need minimally disruptive medicine. BMJ. 2009;339:b2803. doi: 10.1136/bmj.b2803. [DOI] [PubMed] [Google Scholar]
- 2.Corbin J., Strauss A. Managing chronic illness at home: three lines of work. Qual Sociol. 1985;8:224–247. [Google Scholar]
- 3.Shippee N.D., Shah N.D., May C.R., Mair F.S., Montori V.M. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. J Clin Epidemiol. 2012;65(10):1041–1051. doi: 10.1016/j.jclinepi.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 4.Vijan S., Hayward R.A., Ronis D.L., Hofer T.P. Brief report: the burden of diabetes therapy; implications for the design of effective patient-centered treatment regimens. J Gen Intern Med. 2005;20(5):479–482. doi: 10.1111/j.1525-1497.2005.0117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tran V.-T., Harrington M., Montori V.M., Barnes C., Wicks P., Ravaud P. Adaptation and validation of the Treatment Burden Questionnaire (TBQ) in English using an internet platform. BMC Med. 2014;12:109. doi: 10.1186/1741-7015-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eton D.T., Yost K.J., Lai J.-S., et al. Development and validation of the Patient Experience with Treatment and Self-management (PETS): a patient-reported measure of treatment burden. Qual Life Res. 2017;26(2):489–503. doi: 10.1007/s11136-016-1397-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bohlen K., Scoville E., Shippee N.D., May C.R., Montori V.M. Overwhelmed patients: a videographic analysis of how patients with type 2 diabetes and clinicians articulate and address treatment burden during clinical encounters. Diabetes Care. 2012;35(1):47–49. doi: 10.2337/dc11-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ware J.E., Jr., Sherbourne C.D. The MOS 36-item short-form health survey (SF-36), I: Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 9.Spencer-Bonilla G., Quiñones A.R., Montori V.M., International Minimally Disruptive Medicine Workgroup Assessing the burden of treatment. J Gen Intern Med. 2017;32(10):1141–1145. doi: 10.1007/s11606-017-4117-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeSalvo K.B., Fan V.S., McDonell M.B., Fihn S.D. Predicting mortality and healthcare utilization with a single question. Health Serv Res. 2005;40(4):1234–1246. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sundararajan V., Henderson T., Perry C., Muggivan A., Quan H., Ghali W.A. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–1294. doi: 10.1016/j.jclinepi.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 12.Metricwire Breakthrough Research Metricwire Inc website. https://metricwire.com/
- 13.Russell L.B., Suh D.-C., Safford M.A. Time requirements for diabetes self-management: too much for many? J Fam Pract. 2005;54(1):52–56. [PubMed] [Google Scholar]
- 14.Shiffman S., Stone A.A., Hufford M.R. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 15.Asiedu G.B., Carroll K., Griffin J.M., Hurt R.T., Mundi M. Home enteral nutrition: use of photo-elicitation to capture patient and caregiver experiences. Health Sci Rep. 2018;1(8):e56. doi: 10.1002/hsr2.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clark C.D. The autodriven interview: a photographic viewfinder into children's experience. Visual Sociol. 1999;14(1):39–50. [Google Scholar]
- 17.Rich M., Lamola S., Gordon J., Chalfen R. Video intervention/prevention assessment: a patient-centered methodology for understanding the adolescent illness experience. J Adolesc Health. 2000;27(3):155–165. doi: 10.1016/s1054-139x(00)00114-2. [DOI] [PubMed] [Google Scholar]
- 18.Kwasnicka D., Dombrowski S.U., White M., Sniehotta F.F. Data-prompted interviews: using individual ecological data to stimulate narratives and explore meanings. Health Psychol. 2015;34(12):1191–1194. doi: 10.1037/hea0000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thompson M., Oelker A. Use of participant-generated photographs versus time use diaries as a method of qualitative data collection. Int J Qual Methods. 2013;12:624–637. [Google Scholar]
- 20.Inzucchi S.E., Bergenstal R.M., Buse J.B., et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach; update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–149. doi: 10.2337/dc14-2441. [DOI] [PubMed] [Google Scholar]
- 21.Spook J.E., Paulussen T., Kok G., Van Empelen P. Monitoring dietary intake and physical activity electronically: feasibility, usability, and ecological validity of a mobile-based Ecological Momentary Assessment tool. J Med Internet Res. 2013;15(9):e214. doi: 10.2196/jmir.2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montori V. 2017. Why We Revolt: A Patient Revolution for Careful and Kind Care. The Patient Revolution. [Google Scholar]
- 23.Eton D.T., Linzer M., Boehm D.H., et al. Deriving and validating a brief measure of treatment burden to assess person-centered healthcare quality in primary care: a multi-method study. BMC Fam Pract. 2020;21(1):221. doi: 10.1186/s12875-020-01291-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Safford M.M., Russell L., Suh D.-C., Roman S., Pogach L. How much time do patients with diabetes spend on self-care? J Am Board Fam Pract. 2005;18(4):262–270. doi: 10.3122/jabfm.18.4.262. [DOI] [PubMed] [Google Scholar]
- 25.Yen L.E., McRae I.S., Jowsey T., Bagheri N. Time spent on health related activity by older Australians with diabetes. J Diabetes Metab Disord. 2013;12:33. doi: 10.1186/2251-6581-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buffel du Vaure C., Ravaud P., Baron G., Barnes C., Gilberg S., Boutron I. Potential workload in applying clinical practice guidelines for patients with chronic conditions and multimorbidity: a systematic analysis. BMJ Open. 2016;6(3):e010119. doi: 10.1136/bmjopen-2015-010119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bekhet A.K., Zauszniewski J.A. Methodological triangulation: an approach to understanding data. Nurse Res. 2012;20(2):40–43. doi: 10.7748/nr2012.11.20.2.40.c9442. [DOI] [PubMed] [Google Scholar]
- 28.Rosbach M., Andersen J.S. Patient-experienced burden of treatment in patients with multimorbidity - a systematic review of qualitative data. PLoS One. 2017;12(6):e0179916. doi: 10.1371/journal.pone.0179916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheng C., Inder K., Chan S.W.-C. Patients' experiences of coping with multiple chronic conditions: a meta-ethnography of qualitative work. Int J Ment Health Nurs. 2019;28(1):54–70. doi: 10.1111/inm.12544. [DOI] [PubMed] [Google Scholar]
- 30.Boehmer K.R., Hargraves I.G., Allen S.V., Matthews M.R., Maher C., Montori V.M. Meaningful conversations in living with and treating chronic conditions: development of the ICAN Discussion Aid. BMC Health Serv Res. 2016;16(1):514. doi: 10.1186/s12913-016-1742-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Boehmer K.R., Guerton N.M., Soyring J., Hargraves I., Dick S., Montori V.M. Capacity coaching: a new strategy for coaching patients living with multimorbidity and organizing their care. Mayo Clin Proc. 2019;94(2):278–286. doi: 10.1016/j.mayocp.2018.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.