Highlights
-
•
This study examined changes in mental health and well-being in patients on MOUDs.
-
•
Initial decreases in depression and anxiety were observed.
-
•
No changes in mental health and well-being were maintained at 6 months.
-
•
Additional psychosocial treatment is needed to support patients on buprenorphine.
Keywords: Buprenorphine, Behavioral health, Depression, Anxiety, Life satisfaction, Substance use disorders
Abstract
Opioid use disorder (OUD) continues to be a significant problem in the United States, contributing to overdose and death. Recent efforts to expand access to treatment of OUD in primary care have increased the availability of medications for OUD (MOUDs). However, OUD is often accompanied by poor mental health and well-being, and it is not known if treatment with MOUDs alone is associated with improved psychological well-being. This study’s purpose was to examine changes in mental health and well-being in the first 6 months of treatment with MOUDs in a family medicine residency clinic. Patients (N = 126; M age = 34.6 years, SD = 10.6; 54.8% male; 71.4% white) completed validated screeners of mental health and well-being (depression, anxiety, anger, loneliness, perceived stress, meaning in life, and life satisfaction) at baseline (induction visit for buprenorphine), 1-month, and 6-months. Results indicated that the mental health and well-being indices did not significantly change over the first 6 months of treatment on MOUDs. There were initial decreases in depression and anxiety at 1-month; however, both increased and were equivalent to baseline levels at 6-months. These results suggest that MOUD treatment alone does not significantly impact mental health or well-being in patients with OUD. Additional treatments or supports are clearly needed to address the comorbid mental health and well-being challenges in this population, as these factors can be both antecedents and consequences of substance misuse.
1. Introduction
Opioid use disorder (OUD) impacts an estimated 2 million Americans annually (Substance Abuse and Mental Health Services Administration, 2019). Opioid misuse accounts for nearly 70% of overdose deaths in the United States, and over 46,800 Americans died of an opioid-related overdose in 2018 (National Institute on Drug Abuse, 2020). Medications for opioid use disorder (MOUDs), including methadone, buprenorphine, and naltrexone, have been tremendously successful in decreasing opioid-related mortality and morbidity rates (Wakeman et al., 2020) and improve quality of life among people with OUD (Raisch et al., 2012, Rhee and Rosenheck, 2019). Buprenorphine, a partial opioid agonist, is a commonly employed MOUD that can be prescribed by primary care clinicians during regular office visits.
More than half to two-thirds of patients living with OUD present to treatment in primary care with comorbid psychological health concerns, including but not limited to depression, anxiety, and post-traumatic stress disorder (Cole et al., 2019, Fareed et al., 2014, Li et al., 2019, Winstanley et al., 2020). The extent to which participation in stand-alone MOUD treatment is related to or contributes to improvements in these variables is unknown. Longitudinal evaluation of mental health and well-being in patients receiving MOUDs alone, without counseling, is lacking in the scientific literature (Streck, Ochalek, Badger, & Sigmon, 2018). Two studies have shown that patients taking buprenorphine experience decreases in psychiatric symptoms (depression and anxiety) in the first 3 months of treatment (Streck et al., 2018, Zheng et al., 2016). Another study with longer follow-up found that mental health (as measured by the Short Form-36) significantly improved from baseline to 12 months in patients enrolled in a study of extended-release buprenorphine injections (Ling et al., 2020). Further, all these studies demonstrated the biggest improvement in mental health symptoms in the first month of treatment. More research is needed to understand changes in mental health and well-being in patients receiving MOUDs in a primary care setting.
The purpose of the current research was to longitudinally track mental health and well-being in patients being treated in an office-based MOUD treatment program for 6 months after induction. Examination of changes over time in mental health and well-being is important in shaping our model of service delivery for patients living with OUD. Findings could suggest office-based MOUD can improve both substance misuse and mental health; however, lack of improvement over time may serve as an impetus for developing new treatment initiatives to positively impact the well-being of patients with OUD. Based on the limited available research, we hypothesized that mental health and well-being would improve during the 6 months of MOUD treatment.
2. Material and methods
2.1. Participants
Participants (N = 126) were patients receiving MOUDs at a university-affiliated family medicine residency clinic in the upper Midwest. The clinic is located in a socioeconomically depressed area of a large metropolitan city and predominantly serves patients who identify as Black (70%) and who are on state-funded insurance (70%). Patients were included if they were (a) at least 18 years old and (b) starting buprenorphine/naloxone between May 2018 and December 2019. Patients were excluded if their physician deemed them too unstable to participate.
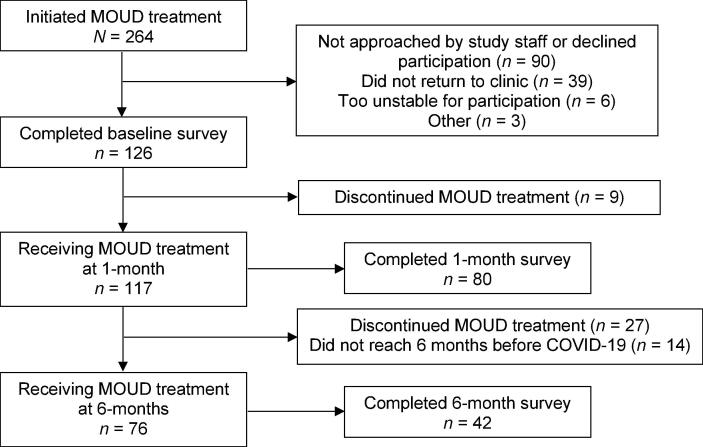
During the enrollment period, 264 patients initiated MOUDs. The 138 patients not included in this study did not participate for a variety of reasons (see Fig. 1). Some patients did not complete follow-up appointments within 1 month of initiation (n = 39). Patients who did return to the clinic within 1 month of initiation but did not enroll in the study (n = 90) often did not have an opportunity to meet with research staff during their clinic follow-up or declined participation due to time constraints. A few patients were too unstable or abusive to clinic staff to be appropriate for the study (n = 6) or met other exclusion criteria, such as being less than 18 years of age or starting naltrexone (n = 3).
Fig. 1.
Participant flow and survey completion. Note. MOUD = Medications for Opioid Use Disorder.
On average, participants were 34.6 years old (SD = 10.6 years). About half (n = 69, 54.8%) were male, 42.9% (n = 54) were female, and 2.4% (n = 3) identified as transgender or gender non-binary. The majority of participants identified as white (n = 90, 71.4%), followed by Black (n = 11, 8.7%), American Indian or Alaskan Native (n = 11, 8.7%), mixed race (n = 10, 7.9%), or other (n = 4, 3.2%). About half (n = 60, 48.4%) were single and never married, 25% (n = 31) were currently married, 21.8% were divorced (n = 27), 4% were currently separated (n = 5), and 0.8% were widowed (n = 1). The majority were unemployed (n = 65, 51.6%); only one-quarter (n = 31, 25%) were employed full- or part-time, with the remaining participants reporting that they were disabled (n = 16, 12.7%), students (n = 7, 5.6%), homemakers (n = 5, 4%), or retired (n = 2, 1.6%). Across the sample, income levels were low, with 50% reporting that they earned less than $10,000 annually (n = 62), 41.5% earning between $10,000 and $49,999 (n = 51), and 8.1% earning $50,000 or more per year (n = 10).
2.2. Procedure
This study used a longitudinal cohort study design. Clinic staff, including a licensed alcohol and drug counselor (LADC), a care coordinator, and project coordinators, approached patients during their MOUD induction clinic visit and asked if they would be willing to complete a survey with demographic and psychosocial variables. Staff emphasized that completing the surveys was completely voluntary, and their care would not be affected if they declined to participate. If participants were unable to complete the survey that day, they were invited to complete it at a subsequent clinic visit, usually within a week. At 1 and 6 months after completing baseline surveys, active participants were asked to again complete the surveys during a regularly scheduled clinic visit. Patients were offered $5 gift cards for completing each survey. This study was approved by the Institutional Review Board as program evaluation to better understand the mental health concerns of patients receiving MOUDs. Some 6-month follow-up surveys were not obtained because of service delivery changes due to COVID-19. As a result of safety practices, many clinic visits were switched to virtual visits which prevented us from being able to collect these surveys.
2.3. Measures
2.3.1. Demographics
Patients reported on demographic variables including gender, age, race/ethnicity, marital status, employment status, and income.
2.3.2. Depressive symptoms
The 9-item Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2002) measures depressive symptoms. Participants rate the extent to which they are bothered by a series of nine symptoms (e.g., “little interest or pleasure in doing things”) over the past 2 weeks on a scale ranging from 0 (not at all) to 3 (nearly every day). Higher scores (possible range of 0–27) correspond to greater depressive symptoms. A cut-score of 10 or greater is used to indicate clinically significant depressive symptoms. Previous investigations have found that higher scores on the PHQ-9 were related to greater likelihood of being diagnosed with any depressive disorder (Kroenke & Spitzer, 2002). In this study the internal consistency was high at all three time points: baseline (α = 0.88), 1-month (α = 0.90), and 6-months (α = 0.91).
2.3.3. Anxious symptoms
The 7-item Generalized Anxiety Disorder-7 (GAD-7; Spitzer, Kroenke, Williams, & Lowe, 2006) questionnaire was used to measure anxious symptoms. Patients rate the extent to which they experienced the 7 symptoms (e.g., feeling nervous, anxious, or on edge) over the past two weeks on a scale from 0 (not at all) to 3 (nearly every day). Items are summed for a total score (possible range of 0–21), with higher scores corresponding to greater anxious symptoms. A cut-score of 10 or greater is used to indicate clinically significant anxiety. Internal consistency was very high at all three time points: baseline (α = 0.94), 1-month (α = 0.95), and 6-months (α = 0.90).
2.3.4. Loneliness
The 3-item version of the UCLA Loneliness Scale (Hughes, Waite, Hawkley, & Cacioppo, 2004) measures loneliness. Patients respond to each statement with one of three options (Hardly ever, Some of the time, or Often), scored 1, 2, or 3, respectively. Scores are summed with higher scores corresponding to more loneliness. Consistent with scoring from previous research, participants with scores ≥ 6 are categorized as significantly lonely (Steptoe et al., 2013). Previous research indicates that the three-item scale is positively associated with depression and is negatively associated with the number of social connections (Hughes et al., 2004). In the current study, internal consistency was good at baseline (α = 0.82), 1-month (α = 0.83), and 6-months (α = 0.91).
2.3.5. Life satisfaction
The Satisfaction with Life Scale (SWLS; Diener, Emmons, Larsen, & Griffin, 1985) measures life satisfaction. Patients rate their agreement with five statements on a 7-point Likert-type scale ranging from 1 (strongly disagree) to 7 (strongly agree). Responses are summed so that higher scores correspond with greater satisfaction with life (possible range of 5–35). In this study, the internal consistency was high: baseline (α = 0.89), 1-month (α = 0.86), and 6-months (α = 0.89).
2.3.6. Meaning in life
The 10-item Meaning in Life Questionnaire (Steger, Frazier, Oishi, & Kaler, 2006) measures presence of and searching for meaning in life. The presence subscale measures the extent to which persons perceive their lives as meaningful (e.g., “My life has a clear sense of purpose”), and the search subscale measures the extent to which patients are looking for meaning in their lives (e.g., “I am searching for meaning in life.”). Participants report the extent to which each statement is true for them on a 7-point Likert-type scale ranging from 1 (absolutely untrue) to 7 (absolutely true). Responses for each subscale are summed for a total score, with higher scores corresponding to greater presence of or searching for meaning (possible range = 5–35). Internal consistency was high for both presence (baseline, α = 0.88; 1-month, α = 0.90; 6-months, α = 0.88) and search (baseline, α = 0.87; 1-month, α = 0.89; 6-months, α = 0.84) at all three time points.
2.3.7. Perceived stress
The 10-item Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) measures the extent to which patients felt stressed in the past month. Patients rate the frequency to which they felt each symptom (e.g., felt nervous or “stressed”) on a scale from 0 (never) to 4 (very often). Four items are reversed scored, and the items are summed for a total perceived stress score. Higher scores (with a possible range of 0 to 40) correspond to greater perceived stress. Internal consistency was high at baseline (α = 0.85), 1-month (α = 0.84), and 6-months (α = 0.90).
2.3.8. Anger
The Dimensions of Anger Reactions-5 (DAR-5; Forbes et al., 2014) measures anger using 5 items. Patients rate the extent to which they experienced anger (e.g., “I found myself getting angry at people or situations”) over the past four weeks on a scale from 1 (none or almost none of the time) to 5 (all or almost all of the time). Items are summed for a total score (possible range of 5–25), with higher scores corresponding to greater anger. A cut-score of 12 or greater reflects high anger. Internal consistency was high at baseline (α = 0.86), 1-month (α = 0.88), and 6-months (α = 0.92).
2.4. Data analysis
Data were analyzed using SAS 9.4. Descriptive statistics, including means, standard deviations, skewness, and kurtosis, and graphical methods were used to examine the distributions of mental health and well-being measures at each of the three time points (baseline, 1 month, 6 months). To examine missing data patterns, baseline differences in mental health and well-being between (a) those retained at 1- and 6-months and those who were no longer receiving treatment and between (b) survey completers and non-completers at 1- and 6-months were examined using independent samples t-tests.
Changes in mental health and well-being over time were examined using hierarchical linear models (SAS PROC MIXED), with time nested within participants, restricted maximum likelihood estimation, and unstructured covariance matrices. One benefit of using this approach is that all available data were used to estimate change over time.
3. Results
Of the 126 patients at baseline, 117 (96.6%) were still receiving treatment (i.e. had an active prescription for buprenorphine) at the 1-month time period (see Fig. 1). As noted above, data collection abruptly ceased in mid-March 2020 due to our clinic’s discontinuation of most in-person visits due to COVID-19; at that time, 103 patients had been in treatment for 6 months (and were therefore eligible to complete the 6-month follow up survey). Of those, 76 (73.7%) were still receiving treatment (i.e., had an active prescription) at 6 months.
Of patients who were actively engaged in MOUD treatment, 80 (68.4%) completed surveys at 1 month and 42 (55.3%) completed surveys at 6 months. At treatment initiation, there were no differences in mental health or well-being between patients who were retained in treatment at 1- and 6-months (all ps > 0.10). Further, there were no differences in baseline mental health or well-being between survey completers and non-completers at 1- or 6-months (all ps > 0.10).
Descriptive statistics of mental health and well-being measures at baseline, 1-month, and 6-months are presented in Table 1. At baseline, many reported clinically significant levels of distress, including nearly half (n = 62, 49.2%) reported high loneliness, 38% (n = 48) reported clinically significant anxiety, 31% (n = 39) reported high anger, and 28% (n = 35) reported clinically significant depressive symptoms. Further, average scores for life satisfaction were in the “slightly below average” range, and perceived stress was in the moderate range. Mean scores for presence of meaning in life and search for meaning in life were slightly below and slightly above, respectively, previously reported means in a college student sample (Steger, Frazier, Oishi, & Kaler, 2006).
Table 1.
Descriptive statistics of mental health and well-being over time in patients with OUD receiving MOUDs.
|
Baseline |
1-month |
6-month |
|||||
|---|---|---|---|---|---|---|---|
| Possible Range | M | SD | M | SD | M | SD | |
| Depressive symptoms | 0–27 | 7.8 | 5.8 | 6.4 | 6.2 | 7.9 | 6.7 |
| Anxiety symptoms | 0–21 | 8.3 | 6.1 | 6.8 | 6.3 | 7.9 | 5.5 |
| Perceived stress | 0–40 | 20.7 | 7.2 | 19.0 | 6.8 | 18.0 | 8.1 |
| Anger | 5–25 | 9.8 | 4.2 | 9.0 | 4.3 | 8.9 | 4.4 |
| Life satisfaction | 5–35 | 15.5 | 7.7 | 16.6 | 7.1 | 15.9 | 7.9 |
| Presence of meaning | 5–35 | 21.8 | 7.3 | 21.6 | 7.4 | 21.5 | 7.3 |
| Searching for meaning | 5–35 | 24.7 | 6.7 | 25.0 | 7.4 | 24.2 | 6.4 |
| Loneliness | 0–9 | 5.7 | 2.0 | 5.2 | 1.9 | 5.4 | 2.3 |
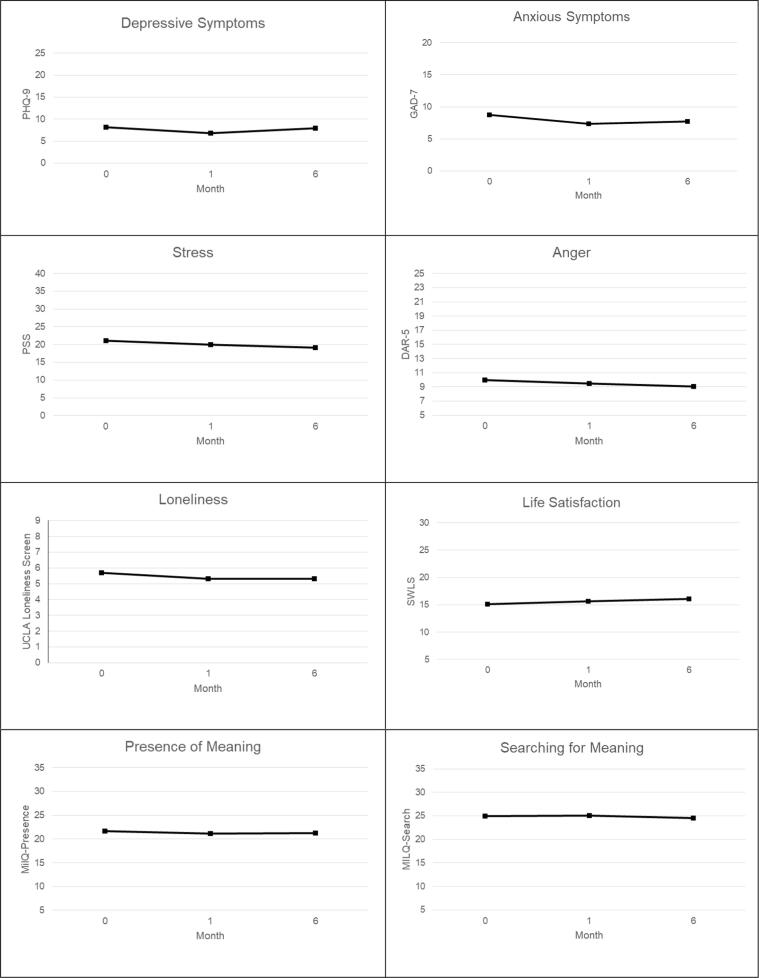
Overall, there were minimal changes in variables across the study period (see Fig. 2). There were no significant changes in stress, F (2, 146) = 2.44, p = .09, life satisfaction, F (2, 146) = 0.68, p = .51, presence of meaning, F (2, 145) = 0.51, p = .60, searching for meaning, F (2, 145) = 0.16, p = .85, anger, F (2, 145) = 1.73, p = .18, or loneliness, F (2, 124) = 1.79, p = .17, over time.
Fig. 2.
Changes in mental health and well-being over the first 6 months of buprenorphine treatment.
There was a significant change in depressive symptoms over time, F (2, 146) = 4.03, p = .02, namely a significant and small decrease in depressive symptoms from baseline to 1-month, b = -1.28, SE = 0.45, t (146) = -2.83, p = .005, followed by a non-significant increase in depressive symptoms from 1-month to 6-months, b = 1.05, SE = 1.03, t (146) = 1.02, p = .31. However, there was no difference in depressive symptoms between baseline and 6-months, b = -0.23, SE = 1.01, t (146) = -0.22, p = .82.
A similar pattern emerged for anxious symptoms, with an overall significant change in anxious symptoms over time, F (2, 146) = 4.65, p = .01. There was a significant and small decrease in anxious symptoms from baseline to 1-month, b = -1.38, SE = 0.47, t (146) = -2.93, p = .004. There was a small, non-significant increase in anxious symptoms from 1- to 6-months, b = 0.40, SE = 0.84, t (146) = 0.47, p = .64, but there were no differences between baseline and 6 month anxiety levels, b = -0.99, SE = 0.77, t (146) = -1.29, p = .20.
4. Discussion
This unique study utilized validated brief screeners of numerous mental health and well-being variables and followed 126 patients across a 6-month period in an office-based MOUD program. Our findings are consistent with previous research showing significant co-morbidity of mental health problems with OUD, including loneliness, anxiety, depression, anger, and stress, thus highlighting the considerable distress experienced by many people living with OUD (Cole et al., 2019, Fareed et al., 2014, Li et al., 2019, Winstanley et al., 2020).
Disappointingly, we found no significant changes in any of the variables across the 6-month study period. Although there were small but significant decreases in levels of depression and anxiety at the 1-month period, these improvements were not maintained at 6 months; there were no statistically significant differences in any variable between baseline and the 6-month time period. Although the improvements in depression and anxiety symptoms were statistically significant, the clinical significance is unknown but doubtful. Initial decreases in depression and anxiety are consistent with previous research (Ling et al., 2020, Streck et al., 2018, Zheng et al., 2016); however, previous research demonstrated that these improvements in mental health were largely maintained. One major difference between this study and previous research is that patients in those studies were enrolled in a research study; patients in this study were receiving treatment in an outpatient primary care clinic. Thus, simply providing MOUD in primary care does not appear to improve mental health or well-being in an outpatient primary care setting.
MOUDs predominantly address brain chemistry related to opiate addiction, and the treatment may not have positive ripple effects on broader well-being. In an analogous fashion, metformin addresses levels of insulin in patients with diabetes but is not intended to treat comorbid depression or anxiety. Our null findings highlight the need for intentional mental health support beyond just MOUDs, which could include psychotherapy, peer support, organized substance use recovery treatment or meetings, religion, or family/friend support. As comorbid mental health and poor well-being could have contributed to the development and maintenance of OUD, failing to intentionally address them can increase a patient’s risk for relapse. Thus, it is incumbent for providers to empower their patients to engage in and stick with treatments that address these comorbid issues.
Limitations of this study include data from a single site study, a relatively small sample, and reliance on self-report measures. Further, there was no comparison group, as it would be unethical to withhold MOUD treatment from patients with OUD. Although we used validated screening questionnaires, they are imperfect proxies for formal individualized evaluation and diagnosis. In addition, survey completion rates were less than ideal, including 68% at 1-month and 55% at the 6-month time period. Although a small proportion of patients were no longer receiving treatment at follow-up time (and therefore were not contacted to complete surveys), data collection in a busy residency clinic where many patients come as walk-ins (rather than scheduled appointments) is challenging. Additionally, project staffing changes adversely affected our ability to always connect with patients when they were in clinic. Further, patients who are in treatment for 6 months or longer have fewer appointments (often only coming in once per month), which makes it more difficult to catch them in clinic for survey completion. Collection of data at the 6-month time point was also limited due to clinic changes associated with the COVID-19 pandemic. Given the ongoing pandemic disproportionately affects persons with substance use disorders in terms of access to medical care and behavioral health services, safe and stable housing, employment opportunities, and social connections (Parshley, 2020), the urgency of this work cannot be understated. It is possible that incomplete survey capture may skew results, in that patients who do not complete surveys have better or poorer mental health and well-being; however, there were no difference between completers and non-completers at baseline. Future research should also examine the course of these psychosocial variables beyond the first 6 months of treatment. Despite these limitations, our use of validated measures in a longitudinal design in a natural setting is a considerable advance in the literature, and our findings have important clinical implications.
4.1. Conclusions
Providing MOUDs to patients is clearly a significant advance in the treatment of OUD, but it is not enough. Failure to address these mental health and well-being issues means continued poor quality of life for patients and likely increased risk for relapse. To provide holistic, comprehensive care for OUD patient population, MOUD providers should collaborate with their on-site and community-based mental health providers who can assess and offer evidence-based services for the many comorbid conditions that appear to persist in patients in the early months of MOUD treatment.
Role of the funding sources
This work was supported by the Substance Abuse and Mental Health Administration State Opioid Response Grant through the Minnesota Department of Human Services (H79TI080248). The Minnesota Department of Human Services and the Substance Abuse Mental Health Administration had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Contributors
Stephanie A. Hooker, Michelle D. Sherman, Robert Levy, and Tanner Nissly designed the study. Mary Lonergan-Cullum conducted literature searches, provided summaries of previous research studies, and assisted with data collection. Stephanie A. Hooker conducted statistical analysis. All authors contributed to manuscript writing and have approved the final manuscript.
CRediT authorship contribution statement
Stephanie A. Hooker: Conceptualization, Formal analysis, Methodology, Writing - original draft. Mary Lonergan-Cullum: Data curation, Project administration, Writing - original draft. Robert Levy: Conceptualization, Methodology, Supervision, Writing - review & editing. Tanner Nissly: Conceptualization, Writing - original draft. Michelle D. Sherman: Conceptualization, Methodology, Supervision, Writing - original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983:385–396. [PubMed] [Google Scholar]
- Cole E.S., DiDomenico E., Cochran G., Gordon A.J., Gellad W.F., Pringle J.…Donohue J.M. The role of primary care in improving access to medication-assisted treatment for rural Medicaid enrollees with opioid use disorder. Journal of General Internal Medicine. 2019;34(6):936–943. doi: 10.1007/s11606-019-04943-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E., Emmons R., Larsen R., Griffin S. The Satisfaction with Life Scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Fareed A., Eilender P., Ketchen B., Buchanan-Cummings A.M., Scheinberg K., Crampton K.…Drexler K. Factors affecting noncompliance with buprenorphine maintenance treatment. Journal of Addiction Medicine. 2014;8(5):345–350. doi: 10.1097/ADM.0000000000000057. [DOI] [PubMed] [Google Scholar]
- Forbes D., Alkemade N., Mitchell D., Elhai J.D., McHugh T., Bates G.…Lewis V. Utility of the dimensions of anger reactions-5 scale as a brief anger measure. Depression and Anxiety. 2014;31:166–173. doi: 10.1002/da.22148. [DOI] [PubMed] [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Li K.J., Smedberg B.S., DeLisi L.E. A retrospective 4-year outcome study of veterans admitted to an acute inpatient detoxification unit for opioid use disorder. The American Journal on Addictions. 2019;28(4):318–323. doi: 10.1111/ajad.12893. [DOI] [PubMed] [Google Scholar]
- Ling W., Nadipelli V.R., Solem C.T., Ronquest N.A., Yeh Y.C., Learned S.M.…Heidbreder C. Effects of monthly buprenorphine extended-release injections on patient-centered outcomes: A long-term study. Journal of Substance Abuse Treatment. 2020;110:1–8. doi: 10.1016/j.jsat.2019.11.004. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. (2020, March 10). Overdose death rates. https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates.
- Parshley, L. (2020, April 21). The pandemic may fuel the next wave of the opioid crisis. National Geographic. https://www.nationalgeographic.com/science/2020/04/coronavirus-pandemic-may-fuel-the-next-wave-of-the-opioid-crisis/.
- Raisch D.W., Campbell H.M., Garnand D.A., Jones M.A., Sather M.R., Naik R., Ling W. Health-related quality of life changes associated with buprenorphine treatment for opioid dependence. Quality of Life Research. 2012;21(7):1177–1183. doi: 10.1007/s11136-011-0027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee T.G., Rosenheck R.A. Association of current and past opioid use disorders with health-related quality of life and employment among US adults. Drug and Alcohol Dependence. 2019;199:122–128. doi: 10.1016/j.drugalcdep.2019.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Lowe B. A brief measure for assessing generalized anxiety disorder. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Steger M.F., Frazier P., Oishi S., Kaler M. The Meaning in Life Questionnaire: Assessing the presence of and search for meaning in life. Journal of Counseling Psychology. 2006;53:80–93. doi: 10.1037/0022-0167.53.1.80. [DOI] [Google Scholar]
- Streck J.M., Ochalek T.A., Badger G.J., Sigmon S.C. Interim buprenorphine treatment during delays to comprehensive treatment: Changes in psychiatric symptoms. Experimental and Clinical Psychopharmacology. 2018;26(4):403. doi: 10.1037/pha0000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A., Shankar A., Demakakos P., Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proceedings of the National Academy of Sciences. 2013;110(15):5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2019, August 20). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf.
- Wakeman S.E., Larochelle M.R., Ameli O., Chaisson C.E., McPheeters J.T., Crown W.H.…Sanghavi D.M. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Network Open. 2020;3(2) doi: 10.1001/jamanetworkopen.2019.20622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley E.L., Lander L.R., Berry J.H., Mahoney J.J., Zheng W., Herschler J.…Haut M.W. West Virginia’s model of buprenorphine expansion: Preliminary results. Journal of Substance Abuse Treatment. 2020;108:40–47. doi: 10.1016/j.jsat.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng W.H., Wakim R.J., Geary R.C., Lander L.R., Wen S.J., Xiao M.C., Sullivan C.R. Self-reported sleep improvement in buprenorphine MAT (medication assisted treatment) population. Austin Journal of Drug Abuse and Addiction. 2016;3(1) [PMC free article] [PubMed] [Google Scholar]