Abstract
The outbreak of COVID-19, caused by SARS-CoV-2, has spread across many countries globally. Greatly, there are limited studies concerned with the effect of airborne pollutants on COVID-19 infection, while exposure to airborne pollutants may harm human health. This paper aimed to examine the associations of acute exposure to ambient atmospheric pollutants to daily newly COVID-19 confirmed cases in 41 Chinese cities. Using a generalized additive model with Poisson distribution controlling for temperature and relative humidity, we evaluated the association between pollutant concentrations and daily COVID-19 confirmation at single-city level and multicity levels. We observed a 10-μg/m3 rise in levels of PM2.5 (lag 0−14), O3 (lag 0−1), SO2 (lag 0), and NO2 (lag 0−14) were positively associated with relative risks of 1.050 (95% CI: 1.028, 1.073), 1.011 (1.007, 1.015), 1.052 (1.022, 1.083), and 1.094 (1.028, 1.164) of daily newly confirmed cases, respectively. Further adjustment for other pollutants did not change the associations materially (excepting in the model for SO2). Our results indicated that COVID-19 incidence may be susceptible to airborne pollutants such as PM2.5, O3, SO2, and NO2, and mitigation strategies of environmental factors are required to prevent spreading.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11356-021-14159-z.
Keywords: Air pollution, COVID-19, Novel coronavirus pneumonia, Generalized additive model
Introduction
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spread across the world and many countries are experiencing ongoing local transmission (Ghinai et al. 2020; Götzinger et al. 2020). The World Health Organization (WHO) reported the novel coronavirus pneumonia has afflicted over 110,749,023 people in more than 221 countries throughout the world and killed over 2,455,131 people as of 21 February 2021. In China, COVID-19 started in Wuhan and spread rapidly across the whole country, and an initial public restriction has played an important role in limiting the spread of infection (Chinazzi et al. 2020). The government has strictly restricted the movement of people and transportation; industrial and economic activities have been greatly reduced. However, restrictions may be less effective once the outbreak is more widespread.
Early studies showed that SARS-CoV-2 has a pathogenic mechanism analogous to the SARS coronavirus, causing potential damage to vital organs including the heart, lungs, liver, and kidneys (Qiu et al. 2020). Many solid observation evidences confirmed the important role of airborne transmission in the spread of COVID-19 (Van Doremalen et al. 2020; Liu et al. 2020). Also, air pollution has been recognized to exacerbate the transmission and severity of respiratory viral infections such as MERS and SARS (Domingo and Rovira 2020; Singh 2016, Yin and Wunderink 2018). The recent literature described the potential associations between atmospheric pollutants and the outbreak of COVID-19 (Contini and Costabile 2020; Dutheil et al. 2020). In some Northern Italian areas, the high propagation capacity of SARS-CoV-2 may be related to an elevated level of ambient particulate matter (Martelletti and Martelletti 2020). A study in 3122 US counties observed that urban air pollution is likely to increase COVID-19 case fatality and mortality rates (Liang et al. 2020). In China, more viral infections were found in the areas afflicted by high PM, nitrogen dioxide, carbon monoxide, and formaldehyde (Pansini and Fornacca 2021). The viruses attach to air pollutants (Reche et al. 2018) and pollutants actually act as the airborne medium of SARS-CoV-2 (Contini and Costabile 2020)
We have long known that acute to chronic exposure to atmospheric pollutants such as PM2.5, PM10, nitrogen dioxide (NO), ozone (O3), sulfur dioxide (SO2), and carbon monoxide (CO) may cause inflammation with systemic effects, usually in the lung, and induce oxidative stress (Al-Kindi et al. 2020; Bind et al. 2012; Newbury et al. 2019). Past work has suggested that exposure to ambient ground-level atmospheric pollutants, such as PM2.5 and O3, can impose a huge burden on the respiratory and cardiovascular system and thus cause many diseases, including stroke, chronic obstructive pulmonary disease (COPD), myocardial infarction, asthma, and congestive heart conditions (Ho et al. 2019; Lelieveld et al. 2019; Schraufnagel et al. 2019). In in vitro studies, NO2 has also been reported to correlate with cellular inflammation, bronchial hyperresponsiveness, and increased risk of infection (Koenig 2000). SO2 may contribute to respiratory symptoms in both healthy patients and patients with potential pulmonary disease, particularly causing changes in airway physiology (Chen et al. 2007).
Since SARS-CoV-2 could survive and remain infectious in aerosols for several hours, and may have a significant effect on human morbidity and mortality throughout the world (Van Doremalen et al. 2020), it is crucial to probe the associations between atmospheric pollutants and COVID-19 incidence. The current studies have evaluated the relationship between the individual pollutants and COVID-19 morbidity or mortality in Italy (Zoran et al. 2020), England (Travaglio et al. 2021), the Netherlands (Andree 2020), and America (Wu et al. 2020). However, few studies have focused on the impact of acute atmospheric pollutant exposure on daily COVID-19 incidence in China. For example, Zhu et al. evaluated cumulative lag effects of ambient airborne pollutants with daily COVID-19 confirmed cases using generalized additive models (Zhu et al. 2020). This paper aims to discuss the impacts of airborne pollutants on COVID-19 morbidity in 41 cities in China (excepting Wuhan), controlling for meteorological variables. To evaluate the impacts of these factors on COVID-19 fast diffusion and fatality, time-series values of selected atmospheric and weather variables over the period January 20−February 29, 2020, together with daily newly COVID-19 confirmed cases have been examined.
Methods
Data collection
We performed a daily time-series study of the correlations between daily newly COVID-19 confirmed cases and air pollutants exposures. The analysis included COVID-19 confirmed cases that occurred among people of the 41 Chinese cities from January 20 to February 29, 2020, of which the cumulative number of which exceeds 100 and the environmental data are available (excepting Wuhan). Since Wuhan with the largest outbreaks and lack of available test may have under-reported cases, we did not take Wuhan into account in our data. Data on daily newly COVID-19 confirmed cases for each city over the study period was obtained from the records kept in the local health commissions and reviewed by the National Health Commission of the People’s Republic of China.
Values of daily 24-h average levels of ambient PM2.5, PM10, SO2, NO2, and CO as well as daily 8-h mean levels of O3 for each city were obtained from https://www.aqistudy.cn/. We averaged the valid monitoring data of selected airborne pollutants in each city, and obtained the daily mean levels of the pollutants. Meanwhile, we gathered daily average temperature and average relative humidity data for each city from http://pm.kksk.org/ to control for the miscellaneous effects of weather conditions.
Statistical analysis
We assessed the detrimental effects of airborne pollutants on COVID-19 incidence using a two-stage analysis strategy which has been widely applied in multicity time-series research (Chen et al. 2017; Liu et al. 2018). To be specific, the relationship between daily COVID-19 confirmation and pollutants (PM2.5, O3, SO2, and NO2) was assessed in separate models for each city using generalized additive Poisson models (GAM) at first stage. At second stage, a random-effects meta-analysis was undertaken to pool the effect estimates at the multicity level. The models were applied to each pollutant separately.
In stage 1, GAM were used in the scope of distributed lag linear modeling framework to approximate city-specific effects of pollutants on COVID-19 morbidity. The model includes the following explanatory variables: (1) log (the number of people newly infected with SARS-CoV-2 every day); (2) the day of the week, which takes into account possible variations within a week; (3) smooth functions of elapsed time to adjust for time varying influences on COVID-19 morbidity; and (4) smooth functions of mean temperature and mean relative humidity on the same day to correct for possible nonlinear and lagged confounding effects of weather conditions. The basic model was shown by Eq. (1):
| 1 |
where E(Yn) is the expected count of daily newly COVID-19 confirmed cases on day n; β is the regression coefficient; Zn is the level of selected pollutants on the day n; timen is the variable for time with a df natural cubic spline on day n to control for long-term trends; TEMP and RH are the mean temperature and mean relative humidity on day n with a df natural cubic spline; and DOWn is the variable for the day n. The df value of smooth functions of elapsed time, mean temperature, and mean relative humidity have an effect on parameter estimation and the stability of the model. Using minimum the residual partial autocorrelation function plots (PACF) and lower generalized cross-validation (GCV) values, the appropriate df value was selected (Amini et al. 2019). This model was applied to each city and air pollutants separately. In this stage, we set 14 as maximum lag day of air pollutants because the incubation period of COVID-19 can vary from 2 to 14 days, mostly 3−7 days (Lauer et al. 2020; Lin and Li 2020).
In stage 2, a meta-analysis of random effects was performed to combine the city-specific effect estimates; thus, we obtained the estimates of the immediate effects of air pollutants at the multicity average level. We calculated the delayed and cumulative effects of airborne pollutants on daily new COVID-19 incidence and presented as relative risks (RRs) and corresponding 95% confidence intervals (CIs) associated with a 10-μg/m3 rise in levels of the pollutants. The following formulas were used:
| 2 |
| 3 |
where β is the predicted regression coefficient of the model; std is the standard error of the model.
Further to the primary model, we also fitted two-pollutant models which each included adjustment to one other pollutant. The correlation between airborne pollutants concentrations and COVID-19 morbidity was considered valid if there is no significant difference between the effect estimates of the single-pollutant and two-pollutant models. We also conducted stratified analyses to evaluate the feasible the pollutants — COVID-19 incidence association by case location. The location of cases was categorized into cities in Hubei and cities outside Hubei.
All statistical analyses were completed using the R3.6.3 software. Two-sided statistical tests were used, and the statistical significance was set at p-value <0.05.
Results
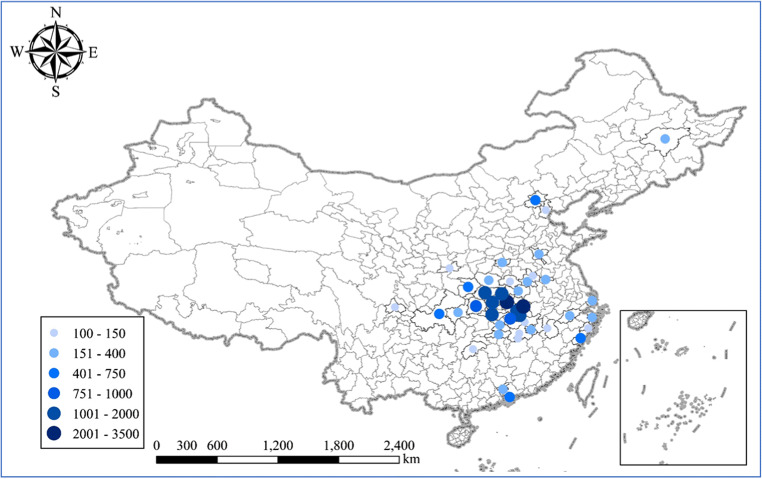
Figure 1 shows the positions of the 41 cities studied in the PRC and the descriptive statistics on cumulative COVID-19 confirmed cases are shown in Table S1. From January 20 to February 29, 2020, there was a total of 22,970 confirmed cases for COVID-19 in the 41 cities, 16,687 (72.6%) of cases were detected in cities in Hubei, and 6283 (27.4%) were reported in other provinces. Xiaogan was the highest of the 12 cities in Hubei with about 3451 COVID-19 confirmed cases, while Enshi was the lowest city with 258 confirmed cases. Among the 21 cities outside Hubei included in this study, Chongqing had the highest number of confirmed cases (n = 576), whereas the lowest confirmed cases were observed in Shaoyang (n = 136). According to the National Bureau of Statistics, despite the population of cities outside Hubei studied (approximately 145.1 million in 2019) is 2.5 times higher than that in cities in Hubei (approximately 59.3 million in 2019), the number of COVID-19 confirmed cases in Hubei is 2.6 times higher than that in cities outside Hubei, which elucidates the weak association between population and COVID-19 spread. Drastic control measures implemented are likely to have helped reduce the spread of the virus by decreasing contact and increasing the physical distance between those who have COVID-19 and those who do not, which may imply the role of case importation in transmission in cities across China (Kraemer et al. 2020).
Fig. 1.
Cumulative confirmed cases in 41 Chinese cities from January 20 to February 29, 2020
Table 1 provides a description of all atmospheric and weather variables recorded over the period covered by this research, and the pollutants in each city can be seen in Table S2. The daily mean PM2.5 level was 51.0 μg/m3, which has exceeded the daily concentration limit set in the Ministry of Ecology and Environment of China on ambient air quality of 35 μg/m3 and > 2 times above than the WHO guideline of 25 μg/m3. Analogously, the mean value of PM10 (62.4 μg/m3) was higher than the Chinese standard and the WHO guideline of (50 μg/m3). The levels of other pollutants were lower than the Chinese standards and the WHO guideline. The mean values of O3, NO2, SO2, and CO were 75.9 μg/m3, 18.8 μg/m3, 7.7 μg/m3, and 0.9 mg/m3, respectively. As a response to COVID-19 lockdown and declining economic activity, NO2, SO2, and CO declined sharply, while O3 kept steady or even increased (Chu et al. 2021; Pei et al. 2020). The average daily temperature was 7.6 °C, varying from −22.5 to 23.0 °C (interquartile range of 5.3 °C); for relative humidity, the average was 74.7%, with interquartile range (IQR) of 21.5%. On account of the contagion of COVID-19, most industrial activities were prohibited, and nearly all avoidable outdoor human activities stopped during the study period. However, severe air pollution episodes still occurred in China, especially in the North China Plain, illustrating large emissions reduction in transportation and industries may not improve severe air pollution, since unfavorable meteorology is inevitable (Wang et al. 2020b).
Table 1.
Descriptive statistics of daily airborne pollutants and weather variables in 41 Chinese cities from January 20 to February 29, 2020
| Variables | Min | Q25 | Median | Q75 | Max | Mean | SD |
|---|---|---|---|---|---|---|---|
| PM2.5 (μg/m3) | 2.0 | 26.0 | 42.0 | 65.0 | 270.0 | 51.0 | 35.9 |
| PM10 (μg/m3) | 5.0 | 34.0 | 53.0 | 80.0 | 338.0 | 62.4 | 39.8 |
| NO2 (μg/m3) | 3.0 | 11.0 | 16.0 | 23.0 | 116.0 | 18.8 | 11.8 |
| SO2 (μg/m3) | 2.0 | 5.0 | 6.0 | 9.0 | 56.0 | 7.7 | 5.3 |
| CO (mg/m3) | 0.2 | 0.6 | 0.8 | 1.0 | 2.3 | 0.9 | 0.3 |
| O3 (μg/m3) | 5.0 | 58.0 | 76.0 | 94.0 | 150.0 | 75.9 | 23.4 |
| Temperature (°C) | −22.5 | 5.0 | 7.6 | 10.3 | 23.0 | 7.6 | 5.5 |
| Relative humidity (%) | 9.3 | 65.2 | 75.8 | 86.8 | 100 | 74.7 | 15.2 |
Spearman correlation coefficients for pollutant and meteorological variable pairs for the study period are given in Table 2. Across the study period, PM2.5 concentrations were closely correlated with PM10 concentrations (Pearson’s correlation coefficient r = 0.793), but less so with CO (r = 0.563) and even slightly correlated with NO2 (r = 0.414), SO2 (0.365), and O3 (r = 0.196). O3 was weakly correlated with other pollutants, whereas the highest correlation coefficient of 0.196 with PM2.5. For other pollutants (NO2, SO2, and CO), the pattern of correlations was broadly analogous to O3. In addition, temperature and relative humidity were negatively correlated with all pollutants. Since the Spearman rank-order correlation analyses indicated a high correlation between temperature and relative humidity and several air pollutants, we incorporated these meteorological factors into the models to assess their underlying confounding effects.
Table 2.
Spearman correlations between airborne pollutants and meteorological variables in all cities during the study period
| Factors | PM2.5 | PM10 | NO2 | SO2 | CO | O3 | TEMP |
|---|---|---|---|---|---|---|---|
| PM10 | 0.793** | ||||||
| NO2 | 0.414** | 0.331* | |||||
| SO2 | 0.365* | 0.244 | 0.355* | ||||
| CO | 0.563** | 0.390* | 0.302 | 0.364* | |||
| O3 | 0.196 | 0.193 | 0.056 | 0.068 | -0.118 | ||
| TEMP | -0.834** | -0.677** | -0.328* | -0.307 | -0.576** | -0.278 | |
| RH | -0.388* | -0.327* | -0.448* | -0.012 | -0.155 | -0.531** | 0.452** |
Note: TEMP and RH indicate ambient temperature and relative humidity, respectively; * and ** indicate P < 0.05 and P < 0.01, respectively
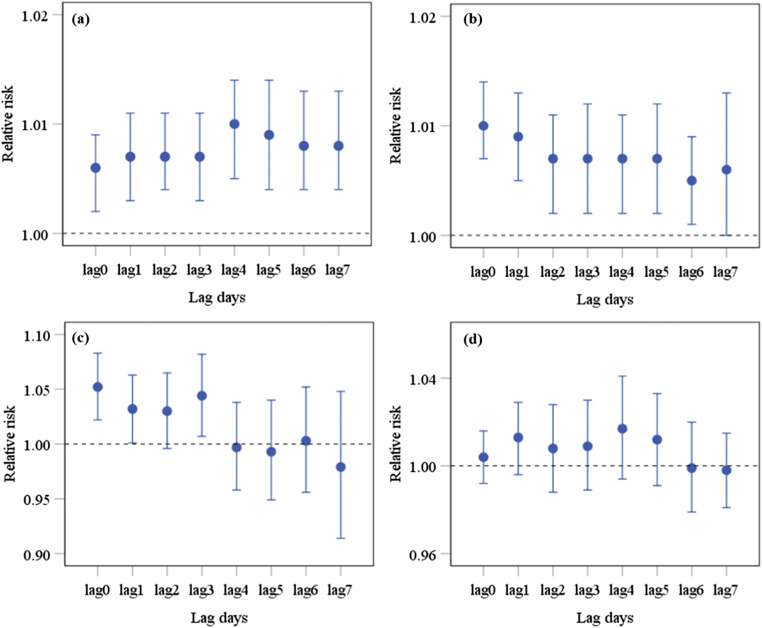
Figure 2 gives the pooled relative risk in daily newly COVID-19 confirmed cases (and 95% CIs) associated with a 10-μg/m3 rise in airborne pollutants for single-day lags from lag of 0 to 7. In the main model for PM2.5, each 10 μg/m3 elevation of exposure to PM2.5 was observed to coincide a small increase in daily newly COVID-19 confirmed cases in the same day (lag 0), with RR (95% CI) of 1.005 (1.001, 1.011). For longer lags, the RR increased gradually until lag 4, reaching a maximum of 1.010 (1.004, 1.016) before decreasing. We observed positive associations between O3 and daily newly COVID-19 confirmed cases from lag of 0 to 5 with the strongest RR (95% CI) of 1.011 (1.007, 1.014) at lag 0. Fewer remarkable findings were observed in the model for SO2, with significant positive associations of SO2 and daily newly COVID-19 confirmed cases at lag 0 [1.052 (1.022, 1.083)], lag 1 [1.032 (1.001, 1.063)], and lag 3 [1.044 (1.007, 1.082)]. In addition, there was no association between increases in NO2 and COVID-19 outcomes at any single-day lag. Generally, associations with daily newly COVID-19 confirmed cases tended to be positive for single-day lags, and the RRs were slightly higher for PM2.5 than O3, both less than SO2.
Fig. 2.
Pooled relative risks of daily newly COVID-19 confirmed cases associated with (a) PM2.5, (b) O3, (c) SO2, and (d) NO2. Note: Error bars are 95% CIs
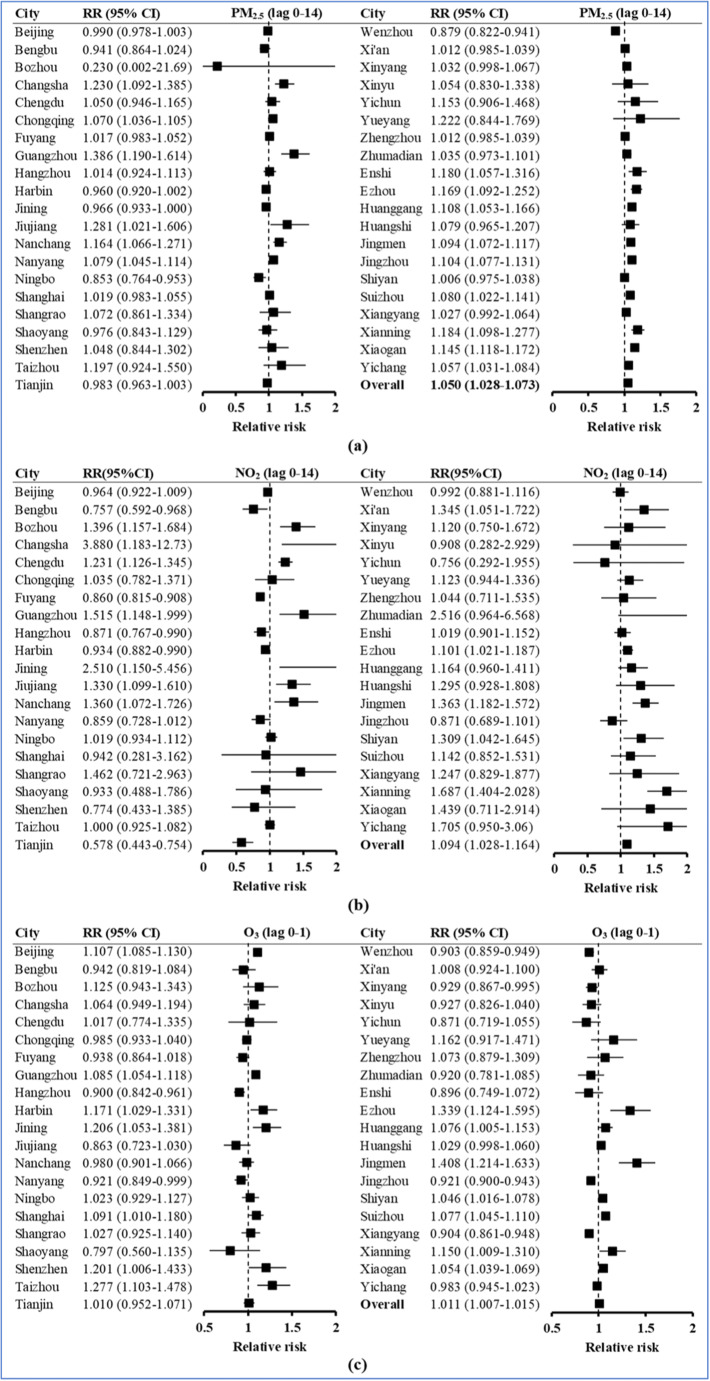
Since prominent correlations between atmospheric pollutants and COVID-19 incidence were observed at several moving averages lags (Table 3), the cumulative effects were further examined. City-specific and the strongest pooled effect estimates of daily newly COVID-19 confirmed cases with increases in the 14−day average of PM2.5 and NO2 are presented in Fig. 3a and 3b. PM2.5 and NO2 significantly increased the risk of daily COVID-19 incidence at lag 0−14 [1.050 (1.028, 1.073) and 1.094 (1.028, 1.164), respectively]. For individual cities, the city-specific estimates of the relative risks in daily newly COVID-19 confirmed cases varied greatly, ranging from 0.230 (for Bozhou) to 1.386 (for Guangzhou) in PM2.5 concentration and ranging from 0.578 (for Tianjin) to 3.880 (for Changsha) in NO2 concentration. As shown in Fig. 3c, each 10 μg/m3 increase in O3 was associated with daily newly COVID-19 confirmed cases in lag 0−1 and the pooled RR (95% CI) was 1.011 (1.007, 1.015). In the city level, the highest RRs of O3 were observed in Jingmen, Ezhou, and Taizhou, while the lowest RRs were observed in Shaoyang and Jiujiang.
Table 3.
Cumulative effect estimates on different lag days of airborne pollutants in all cities
| Lag days | RR (95% CI) | |||
|---|---|---|---|---|
| Pollutants | PM2.5 | O3 | SO2 | NO2 |
| Lag 0 |
1.006 (1.002–1.009) |
1.010 (1.007–1.014) |
1.052 (1.022–1.083) |
1.004 (0.992–1.016) |
| Lag 1 |
1.007 (1.003–1.011) |
1.009 (1.005–1.013) |
1.032 (1.001–1.063) |
1.013 (0.996–1.029) |
| Lag 2 |
1.007 (1.004–1.011) |
1.007 (1.002–1.011) |
1.030 (0.996–1.065) |
1.008 (0.988–1.028) |
| Lag 3 |
1.007 (1.003–1.011) |
1.007 (1.002–1.012) |
1.044 (1.007–1.082) |
1.009 (0.989–1.030) |
| Lag 4 |
1.010 (1.005–1.014) |
1.007 (1.002–1.011) |
0.997 (0.958–1.038) |
1.017 (0.994–1.041) |
| Lag 5 |
1.009 (1.004–1.014) |
1.007 (1.002–1.012) |
0.993 (0.949–1.040) |
1.012 (0.991–1.033) |
| Lag 6 |
1.008 (1.004–1.013) |
1.005 (1.001–1.009) |
1.003 (0.956–1.052) |
0.999 (0.979–1.020) |
| Lag 7 |
1.008 (1.004–1.013) |
1.006 (1.000–1.013) |
0.979 (0.914–1.048) |
0.998 (0.981–1.015) |
| Lag 0–1 |
1.003 (1.000–1.007) |
1.011 (1.007–1.015) |
0.999 (0.961–1.038) |
0.995 (0.984–1.007) |
| Lag 0–3 |
1.005 (1.000–1.011) |
1.009 (1.004–1.015) |
1.039 (0.982–1.100) |
1.004 (0.991–1.018) |
| Lag 0–7 |
0.998 (0.988–1.007) |
1.009 (1.001–1.017) |
0.938 (0.852–1.033) |
0.986 (0.968–1.006) |
| Lag 0–14 |
1.050 (1.028–1.073) |
1.021 (0.994–1.049) |
0.812 (0.632–1.043) |
1.094 (1.028–1.164) |
Fig. 3.
Forest plot for cumulative RRs (95% CI) of daily newly COVID-19 confirmed cases associated with a 10-ug/m3 increase in (a) PM2.5 at lag 1-14; (b) NO2 at lag 0-14; (c) O3 at lag 0–1
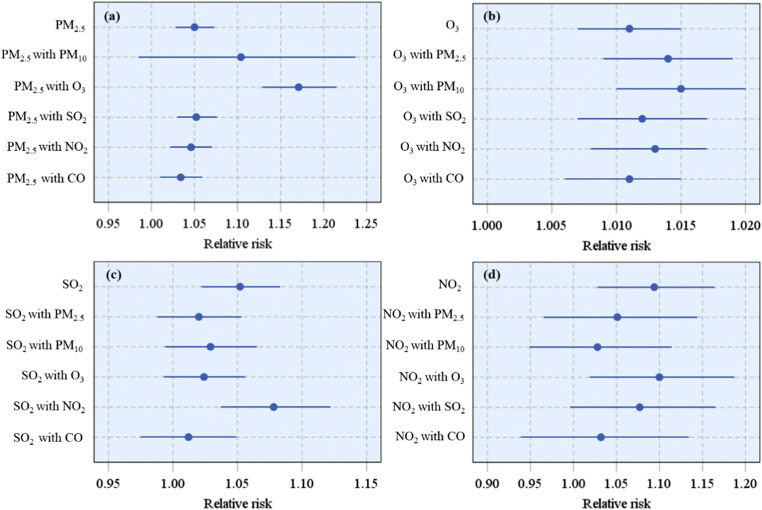
We analyzed two-pollutant models for air pollutants to test interdependences of the pollutants. In such models with PM2.5 as one thereof, the RRs were generally unchanged or increased except adjusting for PM10, compared with the value in the single-pollutant models (Fig. 4a). Similarly, in models with O3 as one of the pollutants, the RRs were generally unchanged or slightly increased compared with its value in the single-pollutant model (Fig. 4b). However, the associations between SO2 (Fig. 4c) or NO2 (Fig. 4d) and risk of COVID-19 incidence were no longer significant at some lags in two-pollutant models (except for O3 and NO2). The effects of SO2 were stronger after adjusting for NO2 but were non-significant after adjusting for other pollutants (PM2.5, PM10, O3, and CO). Each 10 μg/m3 rise in concentration of SO2 at lag 0 coincided with an increase of 2.6% [95% CI (1.5, 3.9)] risk of COVID-19 incidence after adjusting for NO2. Similarly, each 10-μg/m3 rise in concentration of NO2 at lag 0−14 coincided with an exacerbation of 0.6% [95% CI (−0.9, 2.3)] risk of COVID-19 incidence after adjusting for O3. Overall, PM2.5 had the most robust association with daily newly COVID-19 confirmed cases when adjusted for confounding by other pollutants.
Fig. 4.
Pooled RRs (95% CI) of daily newly COVID-19 confirmed cases associated with a 10-ug/m3 rise in (a) PM2.5 at lag 1-14; (b) 03 at lag 0-1; (c) SO2 at lag 0, and (d) NO2 at lag 0-14, with and without adjustment for other airborne pollutants
Stratified analysis by regions showed that relative risks in cities in Hubei were larger than those in cities outside Hubei because Hubei was the province with the most severe COVID-19 outbreak (Table S3). In cities in Hubei, the associations remained positive and significant for most pollutants. Notably, positive associations were also founded for O3 at lag 0−1 for cities outside Hubei, while no prominent effects were observed for other pollutants. Overall, the maximum cumulative RRs were found in cities in Hubei, which were 1.094 (95% CI: 1.064, 1.124) for PM2.5 at lag 0−14; 1.016 (95% CI: 1.011, 1.021) for O3 at lag 0−1; 1.080 (95% CI: 1.045, 1.117) for SO2 at lag 0; and 1.213 (95% CI: 1.085, 1.356) for NO2 at lag 0−14, respectively. Our result is consistent with the findings of the study by Wang et al., who found that the correlations between COVID-19 and ambient PM were stronger for cities inside Hubei than those outside Hubei, and had the highest RR at lag 0−14 for PM2.5 (Wang et al. 2020a).
Discussion
To date, epidemiologic evidence regarding the underlying relationships of ambient atmospheric pollutants on COVID-19 outbreak is insufficient. In this study, we analyzed multisite data on airborne pollutants and daily newly COVID-19 confirmed cases in 41 Chinese cities, although Wuhan (the worst affected city of China) was not included. We observed modest correlations between daily newly COVID-19 confirmed cases and acute exposure to NO2, and to a lesser extent, with PM2.5, O3, and SO2. In the analysis of main models for pollutants, we observed that the RRs (95% CI) for the associations between daily newly COVID-19 confirmed cases and PM2.5, O3, SO2, and NO2 were 1.050 (1.028, 1.073) at lag 0−14, 1.011 (1.007, 1.015) at lag 0−1, 1.052 (1.022, 1.083) at lag 0, and 1.094 (1.028, 1.164) at lag 0−14 per each 10-μg/m3 increment, respectively. The finding suggests that air pollution is an important factor in COVID-19 infection. To be specific, our results indicate that an air pollution with high PM2.5, O3, SO2, and NO2 likely favor the COVID-19 transmission.
Some research has shown that acute exposure to air pollutants is correlated with COVID-19 prevalence or fatality. Study conducted carried out in 120 cities across China revealed increases in daily counts of confirmed cases of 2.24%, 4.76%, −7.79%, and 6.94% each 10-μg/m3 increment in PM2.5, O3, SO2, and NO2 as well (Zhu et al. 2020). Comparing our results to the aforementioned analysis, our findings for SO2 and COVID-19 incidence are completely opposite to their results. It is not clear why the correlations between air pollution and daily COVID-19 morbidity would be different in our study from associations reported by different studies, but it might be explained by factors such as the different scale of the study city and amount of data, fewer considered meteorological variables, and relative higher concentrations and big fluctuation of pollutants during study period. Furthermore, uncontrolled residual confounding or chance as possible explanations should also be considered.
Moreover, several multicity studies about individual pollutants have also been reported. A multicity study (Wang et al. 2020a) in 72 cities (excluding Wuhan) reported a summary estimate for daily COVID-19 confirmed cases of 1.016 (1.015, 1.018) per 10 μg/m3 rise in the level of PM2.5 at lag 0−14. A national American analysis observed a significant increment of 7.1% (1.2%, 13.4%) and 11.2% (3.4%, 19.5%) in COVID-19 case fatality and mortality per IQR in NO2 (Liang et al. 2020). In England, studies also reported increases in COVID-19 incidence in addition to mortality alongside rises in NOx or SO2, meaning that regional variations in the two pollutants may predict the numbers of COVID-19 cases and death (Travaglio et al. 2021). A study conducted in 120 Chinese cities (excluding Wuhan) by multivariate negative binomial regression implicated that the increased number of COVID-19 confirmed cases was accompanied by acute exposure to elevated levels of PM2.5 and O3 and reduced levels of SO2 (Zhou et al. 2021). It should be noted that some studies summarized above reported a negative significant association between SO2 and COVID-19 incidence; this may be due to the relatively low levels of SO2. Our two-pollutant models found a non-significant association between SO2 and COVID-19 incidence after adjusting for other pollutants such as PM2.5 and O3, suggesting that the mechanism of the interaction between SO2 and other pollutants should be explored in future studies.
Whether the observed correlations between air pollutants are independent of other pollutants is a significant issue for air quality control and health risk assessment. In the present study, although the degree of the correlation between PM2.5 and O3 has changed in two-pollutant models, the correlation between the two remained mostly significant, which provides evidence supporting the independent health impacts of PM2.5 and O3. It is remarkable that the estimates of relative risk of COVID-19 incidence per 10-μg/m3 rise with the decrease of PM2.5 levels have no significant effects, a finding that may reflect the close correlations of PM2.5 with PM10 caused by similar sources. As for SO2, the two-pollutant models indicated that the estimated effect of SO2 on COVID-19 incidence was attributable to confounding by other air pollutants (except NO2). In addition, although NO2 are key O3 precursors (Naja and Lal 2002), the two-pollutant model indicated that NO2 has a strong and independent influence on COVID-19 incidence, meaning that the influence of NO2 may not be mediated by O3.
Previous experiments on coronaviruses in controlled conditions show that it can survive at around 4 °C and a relative humidity of 20−80%, and inactivates rapidly above 20 °C (Casanova et al. 2010). It seems that specific climate conditions, especially ambient temperature and humidity, modulate the survival and spread of SARS-CoV-2. A systematic review suggested that warm and humid climates seem to weaken the transmission of COVID-19, while the certainty of the evidence produced was graded as low (MecenasI et al. 2020). Analogously, a time-series analysis in mainland China found with a relative humidity of 67−85.5%, every 1 °C elevation in temperature resulted in a decrease in the daily confirmed cases of 36−57% (Qi et al. 2020). Contrary to the above conclusion, a study across China suggests that the spread speed of the COVID-19 outbreak is independent of temperature, while the temperature dependence of the propagation reported in earlier related work was likely to be an artifact since the temperature dependence blurred with a prevailing zonal pattern of spread across the north-temperature zone, reflecting the primary patterns of human activities (Jamil et al. 2020). In addition, ultraviolet photons have also been considered to play the possible role in the modulation of COVID-19 epidemiology (Nicastro et al. 2020).
The underlying pathophysiological mechanism for developing COVID-19 is perplexing and very few toxicological literature on biological plausibility have been published. It has been reported (Frontera et al. 2020) that chronic exposure to PM2.5 leads to overexpression of alveolar angiotensin-converting enzyme 2 (ACE-2) receptor, which is crucial in protecting the lung from air pollution (Alifano et al. 2020; Lin et al. 2018), as well as the main receptor of SARS-CoV-2 (Zhou et al. 2020). This may increase the viral load in a body exposed to pollutants, thus occupying ACE-2 receptors and weakening host defenses. Furthermore, exposure to NO2 may bring a second hit after exposure to PM2.5, causing severe forms of SARS-CoV-2 to appear in the lungs where ACE-2 depleted, leading to worse results. The current toxicology literature suggests that exposure to ambient ground-level ozone is pertinent to the emergence of respiratory diseases such as asthma, influenza, and SARS (Zoran et al. 2020). O3 is a potential oxidizer and may induce oxidative stress, which may harm the immune systems and organs such as the lung and heart, by changing the host’s resistance to viral and bacterial infections (Ciencewicki and Jaspers 2007). A study in northern Italy (Conticini et al. 2020) has shown that an overexpression of interleukin-8(IL-8), interleukin-7 (IL-17), and tumor necrosis factor-α (TNF-α), induced by O3, contributes to prolonged systemic and respiratory system inflammation and eventually leads to an innate immune system hyperactivation. Compared to PM2.5 and O3, fewer research has studied the biological pathways of harmful effects of NO2 and SO2. The virological explanation might be that NO2 causes the reactions of components in the airway surface fluids (ASF) of the respiratory tract and lungs, resulting in highly reactive proteins and lipid oxidation products that can cause inflammation by subsequently damaging epithelial cells through secondary reactions (Gamon and Wille 2016). Another study by Chauhan et al. (2003) has done research on the relation between NO2 exposure and respiratory disease caused by proven respiratory viral infections including coronavirus.
Our study indicates that air pollutants are important in analyzing the pathogenesis of COVID-19 and that the effect of air pollutants on the disease deserves more attention. It is also subject to some limitations. Primarily, the correlations between air pollutants and COVID-19 confirmation were affected by many other factors, such as strict prevention measure and population migration. Secondly, as the definitions of COVID-19 cases changed at different stages of the epidemic, the number of COVID-19 confirmed cases may be affected. Next, we only focused on cities across China where the cumulative COVID-19 confirmed cases exceed 100 and the environmental data are available (except Wuhan) during the study period, so the estimate of air pollutant effects cannot be generalized to other countries. Finally, stratified analyses by gender or age on were not analyzed in our study due to a lack of detailed information on each infectious case. Future studies should be developed to overcome these limitations, and the mechanisms of the impact on COVID-19 risk deserve further study.
Conclusion
In conclusion, our data show that daily COVID-19 confirmed cases are positively correlated with short-term exposure to atmospheric pollutants, such as PM2.5, O3, SO2, and NO2 in 41 cities across China, and the robust associations between PM2.5 or O3 and daily newly COVID-19 confirmed cases were not complicated by the other air contaminants assessed. Exposure to NO2 for the 14-day average concentration exhibited the most obvious cumulative lagged effect on daily COVID-19 confirmed cases. These results can lay the foundation for the study of correlations between airborne pollutant exposure and potential health risks of COVID-19. The effects of atmospheric pollutants on COVID-19 incidence exhibited a positive variation, suggesting that not only extensive public health control measures but also the lag effect of ambient air pollutants should be considered for curbing COVID-19 infection.
Supplementary Information
(DOCX 27 kb)
Author contribution
BQ Lu and N Wu performed the data analyses, and X Li revised the manuscript. JK Jiang conceived and designed the experiments.
Funding
The funding for this study was provided by the National Natural Science Foundation of China (Nos. 21876029 and 91843301).
Data availability
The datasets and codes used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval
Not applicable
Consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Al-Kindi SG, Brook RD, Biswal S, Rajagopalan S. Environmental determinants of cardiovascular disease: lessons learned from air pollution. Nat Rev Cardiol. 2020;17:656–672. doi: 10.1038/s41569-020-0371-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alifano M, Alifano P, Forgez P, Iannelli A. Renin-angiotensin system at the heart of COVID-19 pandemic. Biochimie. 2020;174:30–33. doi: 10.1016/j.biochi.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amini H, Trang Nhung N, Schindler C, Yunesian M, Hosseini V, Shamsipour M, Hassanvand MS, Mohammadi Y, Farzadfar F, Vicedo-Cabrera AM, Schwartz J, Henderson SB, Künzli N. Short-term associations between daily mortality and ambient particulate matter, nitrogen dioxide, and the air quality index in a Middle Eastern megacity. Environmental Pollution. 2019;254:113121. doi: 10.1016/j.envpol.2019.113121. [DOI] [PubMed] [Google Scholar]
- Andree BPJ (2020) Incidence of COVID-19 and connections with air pollution exposure: evidence from the Netherlands. Policy Research Working Paper Series: https://EconPapers.repec.org/RePEc:wbk:wbrwps:9221
- Bind MA, Baccarelli A, Zanobetti A, Tarantini L, Suh H, Vokonas P, Schwartz J. Air pollution and markers of coagulation, inflammation, and endothelial function associations and epigene-environment interactions in an elderly cohort. Epidemiology. 2012;23:332–340. doi: 10.1097/EDE.0b013e31824523f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova LM, Jeon S, Rutala WA, Weber DJ, Sobsey MD. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl Environ Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan AJ, Inskip HM, Linaker CH, Smith S, Schreiber J, Johnston SL, Holgate ST. Personal exposure to nitrogen dioxide (NO2) and the severity of virus-induced asthma in children. Lancet. 2003;361:1939–1944. doi: 10.1016/S0140-6736(03)13582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R, Yin P, Meng X, Liu C, Wang L, Xu X, Ross JA, Tse LA, Zhao Z, Kan H, Zhou M. Fine particulate air pollution and daily mortality: a nationwide analysis in 272 Chinese cities. Am J Respir Crit Care Med. 2017;196:73–81. doi: 10.1164/rccm.201609-1862OC. [DOI] [PubMed] [Google Scholar]
- Chen T-M, Kuschner WG, Gokhale J, Shofer S. Outdoor air pollution: nitrogen dioxide, sulfur dioxide, and carbon monoxide health effects. Am J Med Sci. 2007;333:249–256. doi: 10.1097/MAJ.0b013e31803b900f. [DOI] [PubMed] [Google Scholar]
- Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu B, Zhang S, Liu J, Ma Q, He H. Significant concurrent decrease in PM2.5 and NO2 concentrations in China during COVID-19 epidemic. J Environ Sci. 2021;99:346–353. doi: 10.1016/j.jes.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciencewicki J, Jaspers I. Air pollution and respiratory viral infection. Inhal Toxicol. 2007;19:1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contini D, Costabile F. Does air pollution influence COVID-19 outbreaks? Atmosphere. 2020;11:377. doi: 10.3390/atmos11040377. [DOI] [Google Scholar]
- Domingo JL, Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ Res. 2020;187:109650. doi: 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutheil F, Baker JS, Navel V. COVID-19 as a factor influencing air pollution? Environ Pollut. 2020;263:114466. doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the “double-hit” hypothesis. J Inf Secur. 2020;81:255–259. doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamon LF, Wille U. Oxidative damage of biomolecules by the environmental pollutants NO2• and NO3•. Acc Chem Res. 2016;49:2136–2145. doi: 10.1021/acs.accounts.6b00219. [DOI] [PubMed] [Google Scholar]
- Ghinai I, McPherson TD, Hunter JC, Kirking HL, Christiansen D, Joshi K, Rubin R, Morales-Estrada S, Black SR, Pacilli M, Fricchione MJ, Chugh RK, Walblay KA, Ahmed NS, Stoecker WC, Hasan NF, Burdsall DP, Reese HE, Wallace M, Wang C, Moeller D, Korpics J, Novosad SA, Benowitz I, Jacobs MW, Dasari VS, Patel MT, Kauerauf J, Charles EM, Ezike NO, Chu V, Midgley CM, Rolfes MA, Gerber SI, Lu X, Lindstrom S, Verani JR, Layden JE, Brister S, Goldesberry K, Hoferka S, Jovanov D, Nims D, Saathoff-Huber L, Hoskin Snelling C, Adil H, Ali R, Andreychak E, Bemis K, Frias M, Quartey-Kumapley P, Baskerville K, Murphy E, Murskyj E, Noffsinger Z, Vercillo J, Elliott A, Onwuta US, Burck D, Abedi G, Burke RM, Fagan R, Farrar J, Fry AM, Hall AJ, Haynes A, Hoff C, Kamili S, Killerby ME, Kim L, Kujawski SA, Kuhar DT, Lynch B, Malapati L, Marlow M, Murray JR, Rha B, Sakthivel SKK, Smith-Jeffcoat SE, Soda E, Wang L, Whitaker BL, Uyeki TM. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet. 2020;395:1137–1144. doi: 10.1016/S0140-6736(20)30607-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, Gabrovska N, Velizarova S, Prunk P, Osterman V, Krivec U, Lo Vecchio A, Shingadia D, Soriano-Arandes A, Melendo S, Lanari M, Pierantoni L, Wagner N, L'Huillier AG, Heininger U, Ritz N, Bandi S, Krajcar N, Roglić S, Santos M, Christiaens C, Creuven M, Buonsenso D, Welch SB, Bogyi M, Brinkmann F, Tebruegge M, Pfefferle J, Zacharasiewicz A, Berger A, Berger R, Strenger V, Kohlfürst DS, Zschocke A, Bernar B, Simma B, Haberlandt E, Thir C, Biebl A, vanden Driessche K, Boiy T, van Brusselen D, Bael A, Debulpaep S, Schelstraete P, Pavic I, Nygaard U, Glenthoej JP, Heilmann Jensen L, Lind I, Tistsenko M, Uustalu Ü, Buchtala L, Thee S, Kobbe R, Rau C, Schwerk N, Barker M, Tsolia M, Eleftheriou I, Gavin P, Kozdoba O, Zsigmond B, Valentini P, Ivaškeviciene I, Ivaškevicius R, Vilc V, Schölvinck E, Rojahn A, Smyrnaios A, Klingenberg C, Carvalho I, Ribeiro A, Starshinova A, Solovic I, Falcón L, Neth O, Minguell L, Bustillo M, Gutiérrez-Sánchez AM, Guarch Ibáñez B, Ripoll F, Soto B, Kötz K, Zimmermann P, Schmid H, Zucol F, Niederer A, Buettcher M, Cetin BS, Bilogortseva O, Chechenyeva V, Demirjian A, Shackley F, McFetridge L, Speirs L, Doherty C, Jones L, McMaster P, Murray C, Child F, Beuvink Y, Makwana N, Whittaker E, Williams A, Fidler K, Bernatoniene J, Song R, Oliver Z, Riordan A. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho S-C, Chuang K-J, Lee K-Y, Chen J-K, Wu S-M, Chen T-T, Lee C-N, Chang C-C, Feng P-H, Chen K-Y, Su C-L, Tsai C-Y, Chuang H-C. Chronic obstructive pulmonary disease patients have a higher risk of occurrence of pneumonia by air pollution. Sci Total Environ. 2019;677:524–529. doi: 10.1016/j.scitotenv.2019.04.358. [DOI] [PubMed] [Google Scholar]
- Jamil T, Alam I, Gojobori T, Duarte CM. No evidence for temperature-dependence of the COVID-19 epidemic. Front Public Health. 2020;8:436–436. doi: 10.3389/fpubh.2020.00436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig JQ. Health effects of ambient air pollution. Boston, MA: Springer; 2000. [Google Scholar]
- Kraemer MUG, Yang CH, Gutierrez B, Wu CH, Klein B, Pigott DM, du Plessis L, Faria NR, Li RR, Hanage WP, Brownstein JS, Layan M, Vespignani A, Tian HY, Dye C, Pybus OG, Scarpino SV, Open C-DWG (2020): The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 368, 493-497 [DOI] [PMC free article] [PubMed]
- Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, Azman AS, Reich NG, Lessler J. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelieveld J, Klingmüller K, Pozzer A, Burnett RT, Haines A, Ramanathan V. Effects of fossil fuel and total anthropogenic emission removal on public health and climate. Proc Natl Acad Sci. 2019;116:7192–7197. doi: 10.1073/pnas.1819989116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang D, Shi L, Zhao J, Liu P, Sarnat JA, Gao S, Schwartz J, Liu Y, Ebelt ST, Scovronick N, Chang HH. Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. Innovation. 2020;1:100047. doi: 10.1016/j.xinn.2020.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CI, Tsai CH, Sun YL, Hsieh WY, Lin YC, Chen CY, Lin CS. Instillation of particulate matter 2.5 induced acute lung injury and attenuated the injury recovery in ACE2 knockout mice. Int J Biol Sci. 2018;14:253–265. doi: 10.7150/ijbs.23489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L, Li T. Interpretation of “Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the National Health Commission (Trial Version 5)”. Zhonghua Yi Xue Za Zhi. 2020;100:E001. doi: 10.3760/cma.j.issn.0376-2491.2020.0001. [DOI] [PubMed] [Google Scholar]
- Liu C, Yin P, Chen R, Meng X, Wang L, Niu Y, Lin Z, Liu Y, Liu J, Qi J, You J, Kan H, Zhou M. Ambient carbon monoxide and cardiovascular mortality: a nationwide time-series analysis in 272 cities in China. Lancet Planet Health. 2018;2:e12–e18. doi: 10.1016/S2542-5196(17)30181-X. [DOI] [PubMed] [Google Scholar]
- Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK, Sun L, Duan Y, Cai J, Westerdahl D, Liu X, Xu K, K-f H, Kan H, Fu Q, Lan K. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- Martelletti L, Martelletti P. Air pollution and the novel Covid-19 disease: a putative disease risk factor. SN Compr Clin Med. 2020;2:383–387. doi: 10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MecenasI P, RTdRM B, Carlos A, Rr V, Normando D. Effects of temperature and humidity on the spread of COVID-19: a systematic review. PLoS One. 2020;15:e0238339. doi: 10.1371/journal.pone.0238339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naja M, Lal S. Surface ozone and precursor gases at Gadanki (13.5 degrees N, 79.2 degrees E), a tropical rural site in India. J Geophys Res Atmos. 2002;107:13. doi: 10.1029/2001JD000357. [DOI] [Google Scholar]
- Newbury JB, Arseneault L, Beevers S, Kitwiroon N, Roberts S, Pariante CM, Kelly FJ, Fisher HL. Association of air pollution exposure with psychotic experiences during adolescence. Jama Psychiatry. 2019;76:614–623. doi: 10.1001/jamapsychiatry.2019.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicastro F, Sironi G, Antonello E, Bianco A, Biasin M, Brucato JR, Ermolli I, Pareschi G, Salvati M, Tozzi P, Trabattoni D, Clerici M (2020) Modulation of COVID-19 epidemiology by UV-B and -A photons from the sun.Social Science Electronic Publishing: 10.2139/ssrn.3620694
- Pansini R, Fornacca D (2021) COVID-19 higher mortality in Chinese Regions with chronic exposure to lower air quality. Frontiers in Public Health 8: 10.3389/fpubh.2020.597753 [DOI] [PMC free article] [PubMed]
- Pei Z, Han G, Ma X, Su H, Gong W. Response of major air pollutants to COVID-19 lockdowns in China. Sci Total Environ. 2020;743:140879. doi: 10.1016/j.scitotenv.2020.140879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H, Xiao S, Shi R, Ward MP, Chen Y, Tu W, Su Q, Wang W, Wang X, Zhang Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020;20:689–696. doi: 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reche I, D’Orta G, Mladenov N, Winget DM, Suttle CA. Deposition rates of viruses and bacteria above the atmospheric boundary layer. ISME J. 2018;12:1154–1162. doi: 10.1038/s41396-017-0042-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraufnagel DE, Balmes JR, Cowl CT, De Matteis S, Jung SH, Mortimer K, Perez-Padilla R, Rice MB, Riojas-Rodriguez H, Sood A, Thurston GD, To T, Vanker A, Wuebbles DJ. Air pollution and noncommunicable diseases a review by the Forum of International Respiratory Societies’ Environmental Committee, part 1: the damaging effects of air pollution. Chest. 2019;155:409–416. doi: 10.1016/j.chest.2018.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh SK. Middle East respiratory syndrome virus pathogenesis. Sem Respir Crit Care Med. 2016;37:572–577. doi: 10.1055/s-0036-1584796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M, Yu Y, Popovic R, Selley L, Leal NS, Martins LM. Links between air pollution and COVID-19 in England. Environ Pollut. 2021;268:115859. doi: 10.1016/j.envpol.2020.115859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Liu J, Li Y, Fu S, Xu X, Li L, Zhou J, Liu X, He X, Yan J, Shi Y, Niu J, Yang Y, Li Y, Luo B. Airborne particulate matter, population mobility and COVID-19: a multi-city study in China. BMC Public Health. 2020;20:1585. doi: 10.1186/s12889-020-09669-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P, Chen K, Zhu S, Wang P, Zhang H. Severe air pollution events not avoided by reduced anthropogenic activities during COVID-19 outbreak. Resour Conserv Recycl. 2020;158:104814–104814. doi: 10.1016/j.resconrec.2020.104814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X, Nethery RC, Sabath MB, Braun D, Dominici F (2020): Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis. Science advances 6, eabd4049eabd4049 [DOI] [PMC free article] [PubMed]
- Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology. 2018;23:130–137. doi: 10.1111/resp.13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J, Qin L, Meng X, Liu N (2021) The interactive effects of ambient air pollutants-meteorological factors on confirmed cases of COVID-19 in 120 Chinese cities. Environ Sci Pollut Res In: 10.1007/s11356-021-12648-9 [DOI] [PMC free article] [PubMed]
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Xie J, Huang F, Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoran MA, Savastru RS, Savastru DM, Tautan MN. Assessing the relationship between ground levels of ozone (O3) and nitrogen dioxide (NO2) with coronavirus (COVID-19) in Milan, Italy. Sci Total Environ. 2020;740:140005. doi: 10.1016/j.scitotenv.2020.140005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 27 kb)
Data Availability Statement
The datasets and codes used and/or analyzed during the current study are available from the corresponding author on reasonable request.