Abstract
Background
To observe the changes in corneal densitometry (CD) with a Pentacam after implantable collamer lens (ICL) V4c implantation in myopia patients, and to investigate potential influencing factors.
Methods
We reviewed 65 eyes of 33 patients (mean age, 29.08±5.54 years) with myopia or myopic astigmatism who underwent ICL V4c implantation. Clinic parameters and Pentacam images of corneal topography and CD were obtained pre- and postoperatively.
Results
After an average of 52±2.2 months follow-up, the efficacy and safety indexes assessed at the last follow-up were 1.03±0.18 and 1.21±0.21, respectively. Except in the central annular zone of 0–2 mm, the CD values increased significantly at postoperative day 1 and decreased significantly until postoperative 1 year (P<0.05). The increase in CD values at different annular zones at postoperative day 1 was ranked as: 0–2 mm <2–6 mm < 6–10 mm. No significant difference was observed in corneal density at 1 week, 1 month, and 1-year follow-up when compared with the preoperative value (P>0.05). The CD value at 4 years follow-up increased significantly and correlated positively with age and preoperative uncorrected distance visual acuity, and negatively with preoperative spherical equivalent and intraocular pressure (IOP) (P<0.05).
Conclusions
ICL V4c implantation demonstrated safety and efficacy for myopia correction. The CD value increased at 4 years postoperatively and correlated with age, preoperative spherical equivalent, uncorrected distance visual acuity, and IOP.
Keywords: Implantable collamer lens (ICL), corneal densitometry (CD), Pentacam, safety
Introduction
The cornea is a major element of the refractive component of the eye. Corneal transparency plays a key role in maintaining good vision (1). Corneal clarity can be considered an important indicator to evaluate corneal health (2), and especially corneal transparency, after refractive surgery or cross-linking surgery. Corneal clarity can be evaluated using both subjective and objective methods. The subjective method involves using a slit lamp microscope to observe whether the cornea is opaque or not (3). In contrast, the objective method involves measuring corneal densitometry (CD) with the Scheimpflug camera of a Pentacam. CD is the backscatter of the cornea, and it can sensitively and accurately document the change in corneal clarity (4).
Implantable collamer lens (ICL) implantation is an effective and reversible method to correct myopia (5-7). Compared with the traditional refractive surgery for myopia, it maintains the integrity and biomechanical characteristics of the cornea and reduces the risk of corneal ectasia and corneal haze (8,9). However, as an intraocular surgery, ICL implantation also has some risks such as corneal endothelial damage or intraocular pressure (IOP) elevation, which may affect the cornea and lead to CD changes.
ICL V4c is a central-hole-designed posterior chamber phakic intraocular lens. Both ICL and ICL V4c are reported to be safe and effective in correcting myopia and myopic astigmatism (10). Furthermore, there was no difference in the postoperative visual outcome between ICL and ICL V4c. However, compared to the original version of ICL, the central hole can effectively increase the aqueous circulation from the posterior to the anterior chamber, and avoid the need for iridotomy or iridectomy which occurred in the previous version of ICL surgery (11). The simplified surgery process reduces the risks of corneal endothelium cell loss and high IOP, which in turn leads to CD changes. Chen et al. (12) reported that CD increased in the early stage and decreased gradually one year after ICL implantation; no significant difference was observed in CD value between the 1-year follow-up and pre-operation. Few reports have focused on the long-term follow-up of CD value after ICL implantation. We conducted this study to observe the CD change 4 years after ICL V4c implantation and to analyze possible influencing factors.
We present the following article in accordance with the MDAR reporting checklist and TREND reporting checklist (available at http://dx.doi.org/10.21037/atm-20-6628).
Methods
Subjects
This was an observational study. We retrospectively reviewed 65 eyes of 33 patients (6 males and 27 females with a mean age of 29.1±5.54 years) who consecutively underwent routine preoperative examinations and then ICL V4c implantation from February 2015 to October 2015 at the Eye & ENT Hospital of Fudan University. Inclusion criteria were as follows: age 20–40 years, stable refraction (no more than 0.50 D increase in two years), no contact lens use for at least two weeks, and endothelial cell density (ECD) >2,000 cells/mm2. Exclusion criteria were as follows: corneal or lens disease, uncontrolled glaucoma, retinal detachment, ocular inflammation, a history of ocular trauma or surgery, and systemic diseases.
This study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Eye and ENT Hospital of Fudan University (No. 2013015-1) and informed consent was obtained from all the patients after a complete description of the study.
Examinations
Preoperatively, as well as at 1 day, 1 week, 1 month, 1 year, and 4 years postoperatively, corneal topography and densitometry values were obtained from Pentacam HR (Oculus, Germany), and the following ophthalmological findings were assessed: (I) uncorrected distance vision acuity (UDVA), manifest refraction, corrected distance visual acuity (CDVA), and slit lamp examination; (II) IOP as measured by a noncontact tonometer (Canon Full Auto Tonometer TX-F; Canon, Inc., Tokyo, Japan); and (III) ECD (SP-2000P, Topcon Corporation, Japan).
Corneal light backscatter, measured as the CD from Scheimpflug images, was expressed in gray scale units (GSU) and ranged from 0 (100% transparent) to 100 (completely opaque). CD values were presented in the average CD table. The cornea was divided into three layers including the anterior layer (the first 120 µm of the corneal thickness), the posterior layer (the last 60 µm of cornea) and the central layer (between the anterior layer and the posterior layer). The total layer was the volume between the epithelium and the endothelium of the cornea. The four annular zones of each layer were listed as: (I) first annular zone, central 0–2 mm; (II) second zone, 2–6 mm; (III) third zone, 6–10 mm; and (IV) fourth zone, 10–12 mm. Since the most peripheral annular zone 10–12 mm has weak reproducibility and repeatability, it was not included in our analysis.
Operation procedure
After antibiotic eye drops four times per day for 3 days, two experienced surgeons (XT Zhou, XY Wang) performed the surgeries. With topical anesthesia, a 3.0 mm temporal or superior incision was made at corneal limbus. After injection of a viscosurgical agent (1.7% sodium hyaluronate; Bausch & Lomb, China) into the anterior chamber, an ICL with a central port was gently inserted. All remaining hyaluronate was subsequently washed out using a balanced salt solution after the footplates of the ICL were placed in the posterior chamber. The details of the procedure were previously reported (13). Postoperatively, patients received topical treatment of antibiotic and steroid eye drops for two weeks.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS version 23.0, IBM). All values are expressed as mean ± SD. Normal distribution was tested using the Shapiro-Wilk test. Generalized estimating equation (GEE) model was applied to adjust for inter-eye dependency. Repeated measurement analysis was used to compare the differences before and after ICL V4c implantation. Spearman correlation analysis was applied to identify relationships between CD value at 4 years follow-up and preoperative and postoperative parameters. P<0.05 was considered statistically significant.
Results
All eyes underwent uneventful ICL V4c implantation without complications. Clinical parameters before and after ICL V4c implantation are shown in Table 1.
Table 1. The clinical outcome parameters of the eyes before and after the ICL V4c implantation.
| Follow-up time point | Pre-op | 1-day Post-op | 1-week Post-op | 1-month Post-op | 1-year Post-op | 4-year Post-op |
|---|---|---|---|---|---|---|
| UDVA (logMAR) | 1.36±0.39 (0.82–2.00) | 0.01±0.03a (−0.08 to 0.1) | 0.00±0.04a (−0.18 to 0.10) | −0.04±0.07abc (−0.17 to 0.10) | −0.02±0.05abcde (−0.17 to 0.10) | 0.01±0.07ade (−0.18 to 0.10) |
| CDVA (logMAR) | 0.01±0.06 (0.08–0.22) | −0.01±0.03a (−0.08 to 0.1) | −0.01±0.03a (−0.08 to 0.1) | −0.06±0.06abc (−0.18 to 0.1) | −0.07±0.06abc (−0.18 to 0.05) | −0.07±0.06abc (−0.18 to 0.05) |
| IOP (mmHg) | 14.65±2.78 (8.3–20.1) | 16.65±1.73a (12.30–22.10) | 15.13±1.79b (11.20–19.80) | 13.77±2.70bc (9.20–20.80) | 14.13±1.96bc (10.60–20.10) | 14.17±2.38bc (10.9–20.1) |
| SE (diopter) | −10.57±2.76 (−5.50 to −18.0) | −0.26±0.24a (−1.00 to 0.38) | −0.20±0.25ab (−0.88 to 0.38) | −0.17±0.26abc (−0.88 to 0.38) | −0.18±0.23abe (−0.88 to 0.25) | −0.37±0.31abcde (−0.88 to 0.25) |
| CCT (μm) | 509±23.92 (466–560) | 526±33.15a (472–642) | 506±24.46b (460–559) | 509±23.77b (467–556) | 509±23.37b (469–561) | 509±25.24b (462–562) |
a, vs. pre-op, P<0.05; b, vs. 1-day Post-op, P<0.05; c, vs. 1-week Post-op, P<0.05; d, vs. 1-month Post-op, P<0.05; e, 1-year Post-op vs. 4-year Post-op, P<0.05. Postop, postoperative; Preop, preoperative; UDVA, uncorrected distance visual acuity; CDVA, corrected distance visual acuity; IOP, intraocular pressure; SE, spherical equivalent; CCT, central corneal thickness.
Safety and efficacy
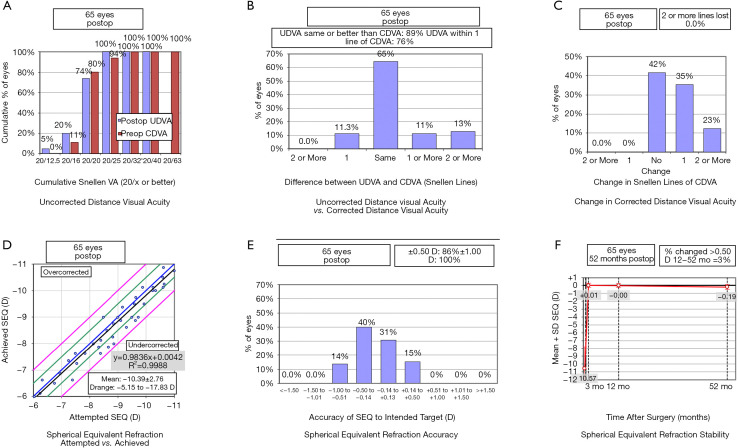
The mean follow-up duration was 52±2.2 months (range, 48–54 months). At the last follow-up, the safety and efficacy indexes were 1.21±0.21 (range, 1–1.71), and 1.03±0.18 (range, 0.8–1.5). 74% of the eyes (48 eyes) had a postoperative UDVA ≥20/20. Further, no eye had a postoperative UDVA <20/40. 89% (58 eyes) of the eyes had postoperative UDVA ≥ preoperative CDVA. No eyes showed a decline in CDVA, and 58% of the eyes (38 eyes) achieved one or more lines (Figure 1A,B,C).
Figure 1.
The clinical outcomes of 65 myopic eyes at last follow-up—4 years post the implantable collamer lens V4c implantation. (A) The preoperative corrected distance visual acuity (CDVA) vs. the postoperative uncorrected distance visual acuity (UDVA); (B) the difference between preoperative CDVA and postoperative UDVA; (C) the change in CDVA; (D) the attempted vs. the achieved spherical equivalent refraction change; (E) the distribution of postoperative spherical equivalent refraction accuracy; (F) the stability of spherical equivalent refraction up to 52 months. D, diopters; Postop, postoperative; Preop, preoperative; mo, months.
Predictability and stability
A scatter plot was used to show the attempted versus achieved spherical equivalent (SE) corrections (Figure 1D). 86% (56 eyes) of the eyes were within ±0.50 D and all eyes were within ±1.0 D of the attempted refraction (Figure 1E). There was no significant change in refraction between 3 months and 1-year follow-up. The average SE (actual − target) powers were −0.004±0.24 and −0.18±0.33 D at 1-year and the last follow-up session, respectively (Figure 1F).
Clinical outcome parameters
A significant difference was observed in SE, UDVA, and CDVA values between pre- and postoperative measurements (P<0.05). SE became emmetropic from 1 day to 1-year postoperatively. There was, however, a myopic shift in SE at the last follow-up. CDVA at 1 month was better than CDVA at 1 day and 1 week postoperatively, and it remained stable at 1-year until the last follow-up. There was a slight increase in IOP at 1 day and 1 week after surgery, but it decreased to preoperative levels at 1 month and remained stable until the last follow-up. The central corneal thickness (CCT) at 1 day after surgery showed a significant increase, but it decreased to preoperative levels at 1 week and had no significant change until the last follow-up.
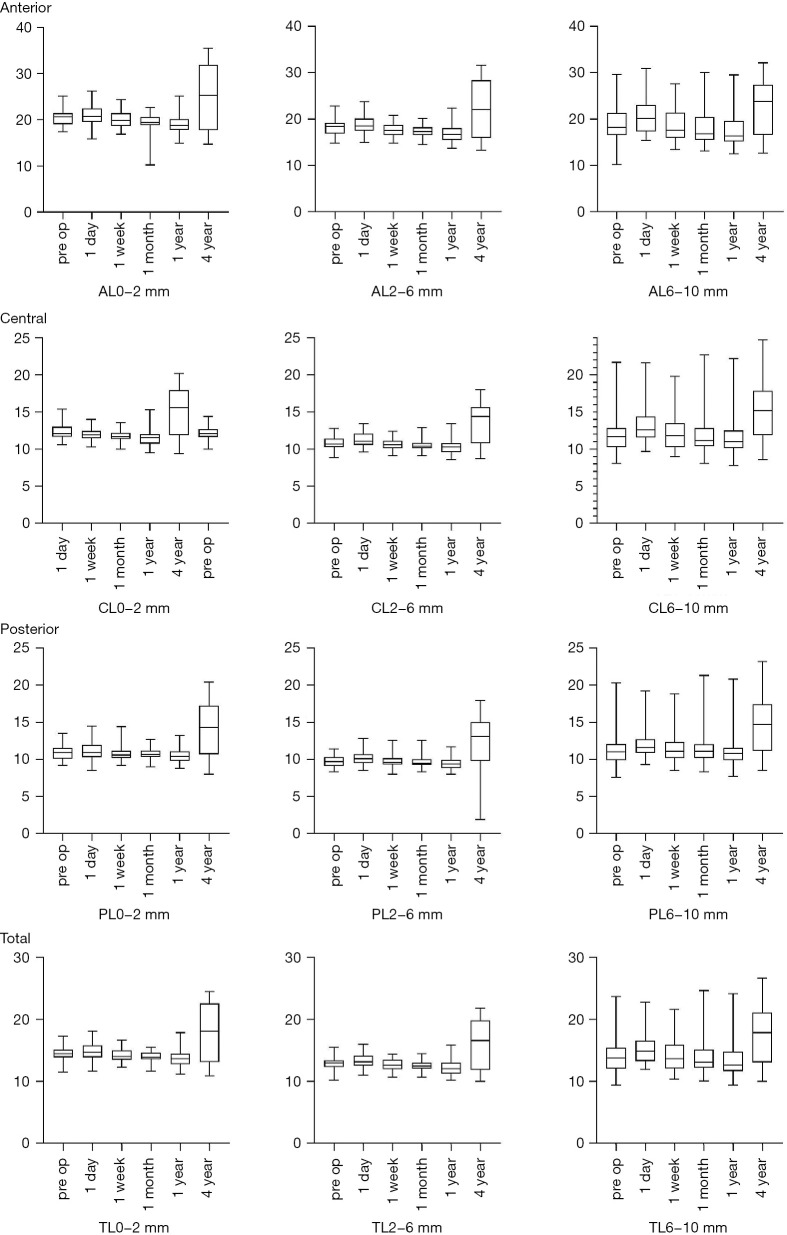
CD
Table 2 and Figure 2 display CD values before and after surgery.
Table 2. The corneal densitometry before and after ICL V4c implantation.
| Variables | Pre-op | 1-day Post-op | 1-week Post-op | 1-month Post-op | 1-year Post-op | 4-year Post-op |
|---|---|---|---|---|---|---|
| AL0-2 mm | 20.4±1.87 | 21.00±2.22 | 19.99±1.72ab | 19.43±1.78abc | 19.04±2.05abc | 24.97±6.72abcde |
| AL2-6 mm | 18.22±1.75 | 18.99±2.06a | 17.69±1.46ab | 17.34±1.18ab | 16.99±1.89abc | 22.51±5.87abcde |
| AL6-10 mm | 19.20±4.41 | 20.62±3.97a | 18.89±3.99b | 18.26±4.03ab | 18.02±4.46abc | 22.51±6.01acde |
| CL0-2 mm | 12.17±0.92 | 12.35±0.98 | 11.96±0.81b | 11.80±0.69ab | 11.56±1.07abc | 15.14±3.34abcde |
| CL2-6 mm | 10.0±0.81 | 11.35±0.96a | 10.64±0.70b | 10.50±0.70ab | 10.37±1.03ab | 13.58±2.83abcde |
| CL6-10 mm | 12.08±2.69 | 13.20±2.43a | 12.23±2.47b | 11.96±2.77b | 11.87±2.93b | 15.17±3.87abcde |
| PL0-2 mm | 10.87±0.93 | 11.14±1.27 | 10.75±0.83b | 10.76±0.74b | 10.53±0.97 ab | 14.03±3.50abcde |
| PL2-6 mm | 9.75±0.81 | 10.16±0.97a | 9.73±0.81b | 9.72±0.87b | 9.49±0.92b | 12.54±3.22abcde |
| PL6-10 mm | 11.18±2.20 | 11.95±1.78a | 11.46±1.88b | 11.41±2.22b | 11.26±2.34b | 14.67±3.69abcde |
| TL0-2 mm | 14.50±1.17 | 14.79±1.25 | 14.25±1.02b | 14.05±0.84ab | 13.71±1.29abc | 18.06±4.44abcde |
| TL2-6 mm | 12.93±1.04 | 13.45±1.17a | 12.70±0.84b | 12.52±0.79ab | 12.26±1.22abc | 16.26±3.80abcde |
| TL6-10 mm | 14.16±2.97 | 15.25±2.54a | 14.18±2.66b | 13.87±2.89b | 11.26±2.34b | 17.48±4.41abcde |
a, vs. pre-op, P<0.05; b, vs. 1-day Post-op, P<0.05; c, vs. 1-week Post-op, P<0.05; d, vs. 1-month Post-op, P<0.05; e, 1-year Post-op vs. 4-year Post-op, P<0.05. Postop, postoperative; Preop, preoperative; AL, anterior layer; CL, central layer; PL, posterior layer; TL, total layer
Figure 2.
Densitometry of the cornea at different follow-up times after implantable collamer lens V4c implantation. Pre-op, Pre operation; AL, anterior layer; CL, central layer; PL, posterior layer; TL, total layer.
On postoperative day 1, the CD values increased significantly at the different layers, except for the one of the 0–2 mm annular zone, compared with pre-operation (P<0.05). The increase in CD values was ranked as: 0–2 mm area < 2–6 mm area < 6–10 mm area.
At 1-week follow-up, the CD values of 0–2 mm and 2–6 mm annular zones at the anterior layer decreased, and the other CD values had no statistical significance when compared with preoperative values (P>0.05). In addition, the CD values of all annular zones at different layers decreased significantly compared with 1 day after operation (P<0.05).
At 1-month follow-up, there was no significant difference in the CD values of 6–10 mm annular zones at different layers and the ones of 0–2 and 2–6 mm annular zones at the posterior layer when compared with pre-operation (P>0.05). Compared with 1-day postoperatively, the CD values in all zones decreased significantly (P<0.05). There was no significant change in other areas except for 0–2 mm annular zones at the anterior layer when compared with 1 week after operation.
At 1-year follow-up, no significant difference was observed in the CD values of 6–10 and 2–6 mm annular zones at the posterior layer, while the CD values of other annular zones decreased significantly compared with pre-operation (P<0.05). All CD values decreased compared with 1 day after operation (P<0.05). The CD values of 0–2 and 2–6 mm annular zones at the total layer and of all annular zones at the anterior layer decreased, and there was no significant difference in other zones when compared with 1 week after operation. No significant difference was observed in the CD values compared with 1 month after surgery.
At the last follow-up 4 years after surgery, compared with pre-operation and other follow-ups, the CD values of all annular zones at different layers were significantly increased (P<0.05), except that there was no significant change in the 6–10 mm annular zones compared with the 1-day follow-up.
At 4-years follow-up, the CD values of 6–10 mm annular zone at different layers correlated positively with age (P<0.05) and negatively with preoperative IOP (P<0.05), while the values of 0–2 and 2–6mm annular zones at different layers correlated positively with preoperative UDVA and those of 0–2 and 2–6 mm annular zones at anterior and total layers correlated negatively with preoperative SE (P<0.05). However, there were no significant correlations between CD values at 4 years follow-up and preoperative CDVA, CCT, or other postoperative parameters (P>0.05; Table 3).
Table 3. Spearman correlation between corneal densitometry at last follow-up and preoperative parameters.
| Pre op | Age | SE | UDVA | IOP | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| r | P value | r | P value | r | P value | r | P value | ||||
| AL0-2 mm | 0.066 | 0.600 | −0.312 | 0.011 | 0.374 | 0.002 | −0.053 | 0.673 | |||
| AL2-6 mm | 0.079 | 0.530 | −0.289 | 0.020 | 0.376 | 0.002 | −0.044 | 0.727 | |||
| AL6-10 mm | 0.334 | 0.007 | −0.113 | 0.368 | 0.201 | 0.109 | −0.281 | 0.024 | |||
| CL0-2 mm | 0.128 | 0.309 | −0.233 | 0.062 | 0.339 | 0.006 | −0.157 | 0.212 | |||
| CL2-6 mm | 0.140 | 0.265 | −0.197 | 0.116 | 0.333 | 0.007 | −0.195 | 0.120 | |||
| CL6-10 mm | 0.434 | 0.000 | −0.150 | 0.234 | 0.193 | 0.123 | −0.317 | 0.010 | |||
| PL0-2 mm | 0.152 | 0.228 | −0.235 | 0.060 | 0.335 | 0.006 | −0.210 | 0.094 | |||
| PL2-6 mm | 0.172 | 0.171 | −0.207 | 0.099 | 0.322 | 0.009 | −0.194 | 0.121 | |||
| PL6-10 mm | 0.508 | 0.000 | −0.153 | 0.225 | 0.211 | 0.092 | −0.368 | 0.003 | |||
| TL0-2 mm | 0.096 | 0.446 | −0.276 | 0.026 | 0.347 | 0.005 | −0.120 | 0.340 | |||
| TL2-6 mm | 0.114 | 0.367 | −0.245 | 0.049 | 0.346 | 0.005 | −0.117 | 0.353 | |||
| TL6-10 mm | 0.422 | 0.000 | 0.123 | 0.328 | 0.185 | 0.140 | −0.329 | 0.008 | |||
Preop, preoperative; AL, anterior layer; CL, central layer; PL, posterior layer; TL, total layer; SE, spherical equivalent; UDVA, uncorrected distance visual acuity; IOP, intraocular pressure.
Corneal ECD
The average corneal ECD was 2,956±235, 3,012±235, and 2,859±211 cells/mm2 at pre-operation, 1 month, and 4 years follow-up, respectively. The ECD at 4 years follow-up decreased by 3.12%±3.70% compared with preoperative values. No case had an ECD <2,000 cells/mm2 or a significant ECD loss of ≥30%. There was no correlation between ECD and CD values (P>0.05).
Vault
The average vault was 453.23±193.36, 462.65±179.35, and 424.92±185.68 µm at 1-month, 1-year, and 4-years follow-up, respectively. There was no significant difference in vault between postoperative 1 month and 1 year. The vault at the last follow-up was significantly lower than at 1 month and 1-year follow-up (P<0.05). Forty-eight eyes (74%) were between 250 and 750 µm, 15 eyes (23%) were between 150 and 250 µm. No eye was less than 150 µm, and 2 eyes (3%) were >750 µm. No cataract or high IOP was observed in eyes with vaults less than 250 µm and more than 750 µm. There was no significant correlation between vault and CD values.
Discussion
The transparency of the cornea mainly depends on the organized arrangement of collagen fibrils in the stroma (14). The integrity of each layer, and the normal function and metabolism of the cornea, are all essential factors to maintain its transparency. Under aging and pathological conditions such as trauma, disease, or oxidative stress, CD increases and corneal transparency decreases, which leads to a decline in vision. CD changes have been reported in keratitis and after corneal refractive surgery or cross-linking surgery for keratoconus (15-17).
CD measurement based on the Scheimpflug imaging system constitutes an objective index of corneal health; it can be used as a parameter to follow corneal diseases, and to ensure the safety of corneal and anterior segment surgery. Alnawaiseh et al. (18) reported that CD values increased in Fuch’s corneal endothelial dystrophy. CD measured by Pentacam has been often used to follow the success of cross-linking surgery in patients with keratoconus (19,20). ICL V4c implantation avoids corneal ablation in traditional refractive surgery, but it remains unclear whether an anterior segment surgery leads to a change in CD. Our study focused on the long-term changes in CD values after 4 years of ICL V4c implantation, and on the possible influencing factors.
The results showed that there was a significant increase in CD values at all annular zones at different layers on the first day after surgery, except for those of the 0–2 mm annular zone. All CD values at 1 week, 1 month, and 1-year follow-up decreased compared with the 1 day follow-up but did not differ from the preoperative values. There was no significant difference in CD between 1 year and 1-month follow-ups. However, the CD value increased significantly 4-years after surgery compared with preoperative and other postoperative follow-up points, except for the value at the 6–10 mm annular zone of the anterior layer, which did not change. At 1-day follow-up, in all three zones, the change in the CD value was higher closer to the peripheral area. We speculate that this was related to limbal corneal incision edema. As corneal incision edema gradually subsided, CD values gradually decreased from 1-week after surgery, and the trend of CCT change also confirmed this. This is consistent with the findings of Ishikawa et al. (21), who demonstrated that CD values increased 1 day after cataract surgery, and gradually decreased 1 week after surgery. The increase in CD values 4 years after surgery may be related to the changes in metabolism and collagen fiber arrangement of corneal endothelial cells with aging.
The average age of the patients in this study was 29.08±5.54 years, and it was positively correlated with CD values at 4-years follow-up, which is consistent with previous reports (22,23). Ní Dhubhghaill et al. (22) reported that the CD value near the limbus increased with age. The average age was 34.1 years in their study and the CD value of 6–10 mm annular zone was 17.5±1.79 GSU, which was close to the 17.48±4.41 GSU at 4-years follow-up in our study. Cankaya et al. (23) reported that age was highly positively correlated with CD, which is consistent with the results of our study.
In our study, the average preoperative SE was −10.57±2.76 D, and it correlated with the CD value. Garzón et al. (24) observed 338 eyes and found that the CD value was not correlated with SE, which might be because the average SE in their study was −3.57±1.81 D, while the SE in our study was much higher. Dong et al. (25) reported that in high myopia the CD value was negatively correlated with SE; they hypothesized that changes in corneal histology related to high myopia led to a decrease in the CD value, which needs further pathophysiological investigation.
In this study, the mean preoperative logmar UDVA was 1.36±0.39, and it positively correlated with the CD value. The higher the CD value, the lower the cornea transparency, which led to a higher logmar UDVA value. Schaub et al. (26) reported that the logmar UDVA decreased as the CD value decreased 2 years after Descemet membrane endothelial keratoplasty. Alnawaiseh et al. (20) observed that the CD value at 2 years after cross-linking surgery for keratoconus was lower than that at pre-operation when the UDVA improved.
In this study, the average IOP was 14.65±2.78 mmHg, and no significant difference in IOP was observed between pre-operation and 4 years follow-up. There was a negative correlation between preoperative IOP and CD values. Most studies (27,28) found that IOP was positively correlated with CD values; high IOP might affect the function of corneal endothelial cells and lead to changes in the CD value. The density of corneal endothelial cells decreased by 3.12%±3.70% at 4 years follow-up, which was in accordance with the normal physiological loss; hence, no significant decrease was observed. Yang et al. (29) reported similar results. Since the IOP in this study was within the normal range, it is necessary to enroll a larger sample to explore the relationship between IOP and CD values in future investigations.
After an average follow-up of 52±2.2 months, the safety index was 1.21±0.21, and the efficacy index was 1.03±0.18. ICL V4c showed good results not only in high myopia and myopic astigmatism, but also demonstrated efficiency in moderate and even low myopia patients. The vault at the follow-ups was within the safe range, similarly to previous studies (30,31). Yan et al. (30) reported that the safety index was 1.24±0.26, and the efficacy index was 1.05±0.20 two years after ICL V4c implantation. Lee et al. (31) observed that the safety index was 1.20±0.26 and the efficacy index, 1.04±0.32 at least 5 years after ICL V4c implantation. As the ICL models with a central port (V4c, EVO, EVO+) are becoming more popular, the long-term safety and effectiveness are always of concern. The follow-up time in this study was at least 4-years and the safety and efficacy indexes were still satisfactory, which indicates that ICL V4c implantation is safe and effective in the long-term.
This study was limited by the relatively small sample size, and there was no age or diopter grouping. A larger sample size should be included in future research, and subjects with different age groups and diopters should be followed-up for a longer time.
Conclusions
Our findings demonstrate that ICL V4c implantation for myopia correction indicated safety and efficacy. CD values increased at postoperative day 1 and then decreased to the preoperative level within 1 year postoperatively but increased at 4 years postoperatively and correlated with age, preoperative SE, UDVA, and IOP.
Supplementary
The article’s supplementary files as
Acknowledgments
We would like to thank Editage (www.editage.cn) for English language editing.
Funding: This study was supported in part by the National Natural Science Foundation of China (Grant No. 81770955); Joint research project of new frontier technology in municipal hospitals (SHDC12018103); the Project of Shanghai Science and Technology (Grant No.17411950200); the National Natural Science Foundation of China for Young Scholars (Grant No. 81600762); the Project of Shanghai Science and Technology (Grant No. 19140900700) and the Shanghai Shenkang Hospital Development Center (Grant No. SHDC12016207).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Eye and ENT Hospital of Fudan University (No. 2013015-1) and informed consent was taken from all the patients after a complete description of the study.
Footnotes
Reporting Checklist: The authors have completed the MDAR reporting checklist and TREND reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-6628
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-6628
Peer Review File: Available at http://dx.doi.org/10.21037/atm-20-6628
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-6628). The authors have no conflicts of interest to declare.
References
- 1.Qazi Y, Wong G, Monson B, et al. Corneal transparency: genesis, maintenance and dysfunction. Brain Res Bull 2010;81:198-210. 10.1016/j.brainresbull.2009.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Otri AM, Fares U, Al-Aqaba MA, et al. Corneal densitometry as an indicator of corneal health. Ophthalmology 2012;119:501-8. 10.1016/j.ophtha.2011.08.024 [DOI] [PubMed] [Google Scholar]
- 3.McLaren JW, Wacker K, Kane KM, et al. Measuring Corneal Haze by Using Scheimpflug Photography and Confocal Microscopy. Invest Ophthalmol Vis Sci 2016;57:227-35. 10.1167/iovs.15-17657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shankar H, Taranath D, Santhirathelagan CT, et al. Repeatability of corneal first-surface wavefront aberrations measured with Pentacam corneal topography. J Cataract Refract Surg 2008;34:727-34. 10.1016/j.jcrs.2007.11.056 [DOI] [PubMed] [Google Scholar]
- 5.Igarashi A, Shimizu K, Kamiya K. Eight-year follow-up of posterior chamber Phakic intraocular Lens implantation for moderate to high myopia. Am J Ophthalmol 2014;157:532-9.e1. 10.1016/j.ajo.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 6.Packer M. Meta-analysis and review: effectiveness, safety, and central port design of the intraocular collamer lens. Clin Ophthalmol 2016;10:1059-77. 10.2147/OPTH.S111620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moya T, Javaloy J, Montés-Micó R, et al. Implantable Collamer Lens for myopia: assessment 12 years after implantation. J Refract Surg 2015;31:548-56. 10.3928/1081597X-20150727-05 [DOI] [PubMed] [Google Scholar]
- 8.Randleman JB, Russell B, Ward MA, et al. Risk Factors and Prognosis for Corneal Ectasia After LASIK. Ophthalmology 2003;110:267-75. 10.1016/S0161-6420(02)01727-X [DOI] [PubMed] [Google Scholar]
- 9.Vaddavalli PK, Hurmeric V, Wang J, et al. Corneal Haze Following Disruption of Epithelial Basement Membrane on Ultra-High-Resolution OCT Following Femtosecond LASIK. J Refract Surg 2012;28:72-4. 10.3928/1081597X-20111202-01 [DOI] [PubMed] [Google Scholar]
- 10.Hyun J, Lim DH, Eo DR, et al. A comparison of visual outcome and rotational stability of two types of toric implantable collamer lenses (TICL): V4 versus V4c. PLoS One 2017;12:e0183335. 10.1371/journal.pone.0183335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawamorita T, Uozato H, Shimizu K. Fluid dynamics simulation of aqueous humour in a posterior-chamber phakic intraocular lens with a central perforation. Graefes Arch Clin Exp Ophthalmol 2012;250:935-9. 10.1007/s00417-011-1850-2 [DOI] [PubMed] [Google Scholar]
- 12.Chen X, Shen Y, Xu HP, et al. One-year natural course of corneal densitometry in high myopic patients after implantation of an implantable collamer lens (model V4c). BMC Ophthalmol 2020;20:50-7. 10.1186/s12886-020-1320-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen X, Miao H, Naidu RK, et al. Comparison of early changes in and factors affecting vault following posterior chamber phakic implantable Collamer Lens im-plantation without and with a central hole (ICL V4 and ICL V4c). BMC Ophthalmol 2016;16:161-9. 10.1186/s12886-016-0336-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freegard TJ. The physical basis of transparency of the normal cornea. Eye 1997;11:465-71. 10.1038/eye.1997.127 [DOI] [PubMed] [Google Scholar]
- 15.Orucoglu F, Talaz S, Aksu A, et al. Corneal densitometry evaluation in archipelago keratitis. Int Ophthalmol 2014;34:99-102. 10.1007/s10792-013-9736-4 [DOI] [PubMed] [Google Scholar]
- 16.Lopes B, Ramos I, Ambrosio RJ. Corneal densitometry in keratoconus. Cornea 2014;33:1282-6. 10.1097/ICO.0000000000000266 [DOI] [PubMed] [Google Scholar]
- 17.Savini G, Huang J, Lombardo M, et al. Objective monitoring of corneal backward light scattering after femtosecond laser-assisted LASIK. J Refract Surg 2016;32:20-5. 10.3928/1081597X-20151207-08 [DOI] [PubMed] [Google Scholar]
- 18.Alnawaiseh M, Zumhagen L, Wirths G, et al. Corneal Densitometry, Central Corneal Thickness, and Corneal Central-to-Peripheral Thickness Ratio in Patients With Fuchs Endothelial Dystrophy. Cornea 2016;35:358-62. 10.1097/ICO.0000000000000711 [DOI] [PubMed] [Google Scholar]
- 19.Shen Y, Jian W, Sun L, et al. One-Year Follow-Up of Changes in Corneal 19. Densitometry After Accelerated (45 mW/cm2) Transepithelial Corneal Collagen Cross-Linking for Keratoconus: A Retrospective Study. Cornea 2016;35:1434-40. 10.1097/ICO.0000000000000934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alnawaiseh M, Rosentreter A, Eveslage M, et al. Changes in corneal transparency after cross-linking for progressive Keratoconus: long-term follow-up. J Refract Surg 2015;31:614-8. 10.3928/1081597X-20150820-07 [DOI] [PubMed] [Google Scholar]
- 21.Ishikawa S, Kato N, Takeuchi M. Quantitative evaluation of corneal epithelial edema after cataract surgery using corneal densitometry: a prospective study. BMC Ophthalmol 2018;18:334-40. 10.1186/s12886-018-0998-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ní Dhubhghaill S, Rozema JJ, Jongenelen S, et al. Normative values for corneal densitometry analysis by Scheimpflug optical assessment. Invest Ophthalmol Vis Sci 2014;55:162-8. 10.1167/iovs.13-13236 [DOI] [PubMed] [Google Scholar]
- 23.Cankaya AB, Tekin K, Kiziltoprak H, et al. Assessment of corneal backward light scattering in the healthy cornea and factors affecting corneal transparency. Jpn J Ophthalmol 2018;62:335-41. 10.1007/s10384-018-0584-7 [DOI] [PubMed] [Google Scholar]
- 24.Garzón N, Poyales F, Illarramendi I, et al. Corneal densitometry and its correlation with age, pachymetry, corneal curvature, and refraction. Int Ophthalmol 2017;37:1263-8. 10.1007/s10792-016-0397-y [DOI] [PubMed] [Google Scholar]
- 25.Dong J, Zhang Y, Zhang H, et al. Corneal densitometry in high myopia. BMC Ophthalmol 2018;18:182-7. 10.1186/s12886-018-0851-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schaub F, Enders P, Bluhm C, et al. Two-Year Course of Corneal Densitometry after Descemet membrane endothelial keratoplasty (DMEK). Am J Ophthalmol 2017;175:60-7. 10.1016/j.ajo.2016.11.019 [DOI] [PubMed] [Google Scholar]
- 27.Tekin K, Sekeroglu MA, Kiziltoprak H, et al. Corneal densitometry in healthy corneas and its correlation with endothelial Morphometry. Cornea 2017;36:1336-42. 10.1097/ICO.0000000000001363 [DOI] [PubMed] [Google Scholar]
- 28.Alnawaiseh M, Zumhagen L, Wirths G, et al. Corneal Densitometry, Central Corneal Thickness, and Corneal Central-to-Peripheral Thickness Ratio in Patients With Fuchs Endothelial Dystrophy. Cornea 2016;35:358-62. 10.1097/ICO.0000000000000711 [DOI] [PubMed] [Google Scholar]
- 29.Yang W, Zhao J, Sun L, et al. Four-year observation of the changes in corneal endothelium cell density and the correlated factors after Implantable Collamer Lens V4c implantation. Br J Ophthalmol 2020;16:316144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yan Z, Miao H, Zhao F, et al. Two-Year Outcomes of Visian Implantable Collamer Lens with a Central Hole for Correcting High Myopia. J Ophthalmol 2018;2018:8678352. 10.1155/2018/8678352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee J, Kim Y, Park S, et al. Long-term clinical results of posterior chamber phakic intra-ocular lens implantation to correct myopia. Clin Exp Ophthalmol 2016;44:481-7. 10.1111/ceo.12691 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as