Abstract
Background
Vaginal laxity may result from trauma to the pelvic floor muscle, which may affect patients’ sensation and quality of life. Vaginal rejuvenation, including surgical or nonsurgical interventions, aims to improve laxity. In this study, we aimed to establish a strategy for vaginal rejuvenation by comparing surgical and nonsurgical methods.
Methods
A retrospective clinical study was performed on patients who complained about vaginal laxity from 2017 to 2019. The degree of vaginal laxity severity was evaluated by vaginal examination in each patient. The patients were categorized as having a light, moderate or severe degree of vaginal laxity, and different correction methods were chosen accordingly. The Female Sexual Function Index (FSFI) questionnaire was administered to the patients preoperatively and at three months and one year after treatment.
Results
Seventeen patients with severe-degree vaginal laxity were treated with vaginoplasty. The total FSFI score was 23.21±2.57 before the operation and significantly increased to 29.36±1.84 (P<0.01) at one year after surgery. Eleven patients with moderate-degree vaginal laxity were treated with vaginoplasty and had a significant improvement in the total FSFI score at one year after surgery (29.86±1.74, P<0.01) compared with the FSFI score before surgery (23.41±2.84). Three patients with moderate-degree vaginal laxity were treated with a CO2 laser and tended to have increased FSFI scores but did not show significant improvement after the operation. CO2 laser treatment was performed on 16 patients with light-degree vaginal laxity. The total FSFI score improved from 23.76±2.35 to 26.16±2.58 at one year (P<0.05).
Conclusions
The strategy for vaginal rejuvenation should be selected based on the degree of vaginal laxity severity. Surgical treatment is suitable for severe- and moderate-degree vaginal laxity while nonsurgical treatment is suitable for light-degree vaginal laxity.
Keywords: Vaginal laxity, vaginal rejuvenation, vaginoplasty, nonsurgical vaginal rejuvenation
Introduction
Sensation loss caused by vaginal laxity is a common problem for women after childbirth. Although the etiological relationship between vaginal laxity and childbirth is not well clarified, it is now generally accepted that vaginal delivery may result in trauma to the levator ani muscle along the pelvic floor (1). It was also found that vaginal delivery is associated with an increased diameter of the hiatus of the levator ani muscle (2,3). Women with vaginal laxity may complain of decreased friction during coitus and diminished sexual satisfaction (4), and sexual dysfunction due to vaginal laxity has also been confirmed by questionnaires such as the female sexual function index (FSFI) (5). Therefore, vaginal laxity not only physically stretches the perineum but also has a large effect on sexual satisfaction (6).
It was reported that 48% of patients who experienced vaginal delivery reported vaginal laxity, but 62% never discussed vaginal laxity with anyone despite 50% feeling that improving tightness would increase sexual satisfaction (7). In an international survey of urogynecologists, 83% of the 563 respondents described vaginal laxity as underreported by their patients (8). Therapies available to these patients have included a range of options that are often minimally effective, such as Kegel exercises. On the other hand, vaginal plastic surgery or vaginal rejuvenation has been shown to be an effective treatment for vaginal laxity caused by childbirth, aging or estrogen deficiency (7). From 2014 to 2019, vaginal rejuvenation, including surgical or nonsurgical interventions, increased nearly 220% and is currently practiced by over 25% of plastic surgeons (9).
Surgical methods such as vaginoplasty and perineoplasty have historically been used for wound repair after delivery, but now, they have been increasingly used for vaginal laxity and aesthetic concerns (10). Meanwhile, the use of energy-based devices as nonsurgical treatments for vaginal laxity has currently become popular in the community and medical fields. However, the idea that nonsurgical treatment, including fractional laser and radiofrequency (RF) devices, can deal with vaginal laxity is difficult to accept according to the plausible mechanism or several studies supported by manufacturers. This prompted the U.S. Food and Drug Administration to issue a press announcement stating that the safety and effectiveness of energy-based devices have not been established (11).
In this study, we performed a retrospective clinical study on patients who complained about vaginal laxity. According to the degree of vaginal laxity severity, different strategies were selected to meet the medical requirements of the patients. Based on the characteristic treatment of vaginal laxity in our study, we aimed to establish a strategy for vaginal rejuvenation.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-5655).
Methods
A retrospective study was performed between 2017 and 2019 in Shanghai Ninth People’s Hospital. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of Shanghai Ninth People’s Hospital (No. 2017-302-T222). All patients signed informed consent forms.
The inclusion criteria were as follows: female patients aged 25 to 40 years who complained about vaginal laxity and had a history of vaginal delivery. The exclusion criteria included menopause; history of urogynecologic operations; symptomatic genital prolapse; and estrogen, anticholinergic medication or antihistamine use. All patients who met the inclusion criteria from 2017 to 2019 were included in this study.
Vaginal laxity was confirmed through vaginal examination, which had been described in Abedi’s study (12). The degree of vaginal laxity severity was evaluated in this examination process. In the lithotomic position, patients were asked to squeeze the examiner’s two fingers with the vagina. If the pressure was strong and could last more than 3 seconds, the patients were regarded as having a light degree of vaginal laxity. Less pressure lasting from 1–3 seconds was regarded as a moderate degree of vaginal laxity. Nearly no pressure on 2 fingers and only a little pressure on 3 or more fingers was regarded as severe vaginal laxity.
For patients with severe laxity, surgical vaginal rejuvenation was suggested, and all patients in the severe group chose vaginoplasty. The vaginoplasty performed was similar to Abedi’s technique (12). Briefly, the vaginal mucosa is elevated to expose the levator ani muscles, and stitches are started from the upper triangle of the vagina to the edge of the hymen to tighten the muscles. The perineal gap was also repaired if needed. The size of the vagina was considered normal if no more than two fingers could be tightly inserted into the vagina after repair. All operations were performed by one surgeon (YL) under local anesthesia.
Patients with light laxity were advised to receive CO2 laser treatment. The CO2 laser (SmartXide2, DEKA, Florence, Italy) was set with a DOT (microablative zone) power of 30 W, a dwell time of 1,000 usec, and a DOT spacing of 1,000 µm. In total, three treatments within a one-month interval were performed for each patient. All laser treatments were performed by one surgeon (S-X.M). Patients with moderate laxity were also advised to have vaginoplasty, but some chose the laser treatment.
The FSFI questionnaire was administered to the patients preoperatively and at three months and one year after treatment. The FSFI questionnaire addresses six different domains (desire, arousal, lubrication, orgasm, satisfaction, and pain/discomfort) ranging from 0 (no sexual activity in the past 4 weeks) or 1 (very dissatisfied) to 5 (very satisfied). The sum of the 6 final domain scores was reported as the total FSFI score. The evaluation of patient satisfaction rates and vaginal examinations were also performed at the one-year follow-up. To minimize variability, one surgeon performed the vaginal examinations to evaluate the degree of laxity before and after the operations. The data from same surgeon was used for data analysis.
Statistical analysis
The results are expressed as the mean ± SD (standard deviation). Statistical analysis was conducted with Statistical Package for Social Sciences (SPSS) 10.0. (IBM Corporation, NY, USA). One-way ANOVA was used to determine the probability of significant differences, and a P value <0.05 was considered to be statistically significant.
Results
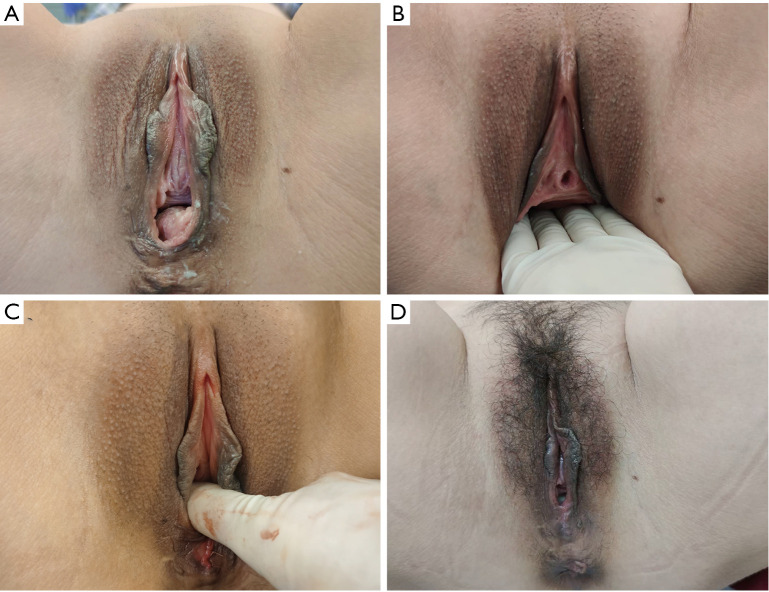
In total, 47 patients with vaginal laxity confirmed by vaginal examination were included in the study. Seventeen patients with severe-degree vaginal laxity were treated with vaginoplasty. In the vaginal examination, the tightening effects of vaginoplasty resulted in the ability to hold no more than two fingers after surgery. One typical case was present in Figure 1. The total FSFI score was 23.21±2.57 before the operation and significantly increased to 30.14±1.2 (P<0.01) at three months after surgery. The FSFI was 29.36±1.84 (P<0.01) at one year after surgery. The satisfaction rate in this group of patients was 88.23% (15/17).
Figure 1.
A typical case of severe vaginal laxity treated by surgery. The patient was 35 years old and had a history of vaginal delivery. (A) The appearance before surgery, (B) on vaginal examination, four of the surgeon’s fingers could be held, (C) only one of the same surgeon’s fingers could be held after surgery. (D) The appearance at 3 months after surgery.
Fourteen patients with moderate-degree vaginal laxity were referred for surgical treatment, but 3 patients preferred nonsurgical methods. These 3 patients were treated with a CO2 laser and had a trend of increasing FSFI scores but did not show significant improvement after the operation (23.83±1.86 vs. 25.5±1.04, P>0.05). These 3 patients were not satisfied with the results and decided to have further surgical treatment within 1 year, so the long-term FSFI data were missing among these patients. The other 11 patients with moderate-degree vaginal laxity were treated with vaginoplasty and had a significant improvement in the total FSFI score at three months (30.38±1.7, P<0.01) and one year after surgery (29.86±1.74, P<0.01) compared with the FSFI score before the operation (23.41±2.84). In the vaginal examination, the tightening effects of vaginoplasty would resulted in the ability to hold one or two fingers after surgery. A total of 90.9% of the patients (10/11) with moderate-degree vaginal laxity treated with surgery were satisfied with the outcome. CO2 laser treatment was suggested to and performed on 16 patients with a light degree of vaginal laxity. The total FSFI score improved from 23.76±2.35 to 28.09±1.7 (P<0.01) at three months and 26.16±2.58 at one year (P<0.05) after the last CO2 treatment (Figure 2). In the vaginal examination, the tightening effects of CO2 treatment would resulted in the ability to hold two fingers. The satisfaction rate of these patients was 87.5% (14/16).
Figure 2.
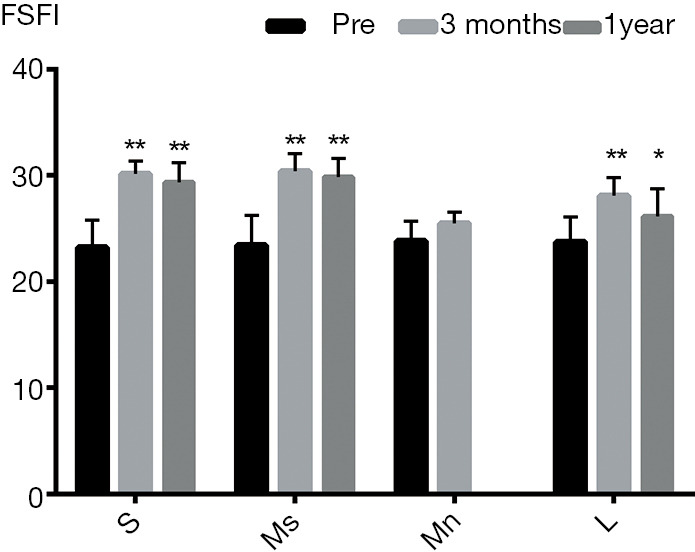
The total FSFI scores before and after treatment. S: severe vaginal laxity with surgical treatment; Ms: moderate degree of vaginal laxity with surgical treatment; Mn: moderate degree of vaginal laxity with nonsurgical treatment; L: light degree of vaginal laxity with nonsurgical treatment. (**, P<0.01; *, P<0.05).
Discussion
Vaginal laxity means different things to different patients (13), but the most common complaint from patients was actually the effect of genital sensation and sexual function instead of the laxity itself. There are many options provided by surgeons and aesthetic practices for improving vaginal laxity; however, the degree of laxity has seldom been mentioned. Ostrzenski’s 4-degree classification (14) mainly focused on the mucosa and appearance, and an objective evaluation of the degree of vaginal laxity is still missing. In our study, patients with vaginal laxity were included, and suitable treatment was suggested according to the degree of laxity measured by vaginal examination. We mainly focused on the pressure from the pelvic floor muscle since the separable muscle should be the most important target in vaginoplasty. Therefore, patients with poor pressure were classified as having severe-degree vaginal laxity, and surgical treatment was suggested. If the pressure was acceptable, the pelvic floor muscle may still be functional and should not be operated on. The patient would be regarded as having light-degree vaginal laxity, and a nonsurgical treatment, i.e., the CO2 laser, was preferred by both doctors and patients.
Many clinical studies have proven that vaginoplasty or colpoperineoplasty can increase sexual function in reproductive-aged women (15-17). In our study, patients who underwent surgical treatment had a significant increase in FSFI scores and higher satisfaction. In the follow-up, improvement in vaginal pressure remained. It was implied that the levator ani muscle plays an important role in regulating the motor response of the vagina and orgasm (16). In those who underwent surgery, the tightening effects were mainly based on the levator ani muscles, which can well explain the significant and stable improvement resulting from the surgery. In our one-year follow-up after vaginoplasty, several patients’ husbands gave us feedback that sexual satisfaction was significantly improved.
On the other hand, surgical treatment is a more invasive operation than nonsurgical methods such as CO2 lasers. Although research on nonsurgical vaginal rejuvenation has increased greatly in recent years, there is still a lack of solid evidence that any energy-based device could effectively tighten the levator ani muscle. The main effect of energy-based devices, including CO2 lasers, are to induce the production and remodeling of collagen and elastin; they may also stimulate neovascularization (18). Histologically, biopsies after treatment revealed increased epithelial thickness, restoration of epithelial structures, and enhanced collagen deposition (19,20). All these beneficial changes would help to restore normal vaginal physiology and improve sexual function. In our study, if the patients did not have much vaginal pressure loss at the examinations, the function of pelvic floor muscle was considered acceptable. These patients were regarded as having a light degree of vaginal laxity, and CO2 laser treatment was suggested. The satisfaction rates among these patients were also high (13/16), mainly because the treatment was minimally invasive and the effectiveness was distinct as well. It is not surprising that several patients with moderate-degree vaginal laxity did not show much improvement with only CO2 laser treatment because the beneficial effects of this method are on epithelial structures rather than muscles, which would not be sufficient to restore vaginal function in these cases. Additionally, surgical treatment of patients with moderate-degree vaginal laxity achieved good improvement in FSFI and the highest satisfaction rates (10/11).
Vaginal laxity also means different things to different doctors. Surgical and nonsurgical treatments have their own advantages and disadvantages. Surgeons who use a single treatment method as a “one fits all” solution would no longer be regarded as experts in this field.
Based on our clinical observations and available evidence to date, the degree of laxity severity based on vaginal pressure should be measured before any treatment. For patients with a large loss of vaginal pressure, vaginoplasty should be performed to restore muscle tension, which would effectively improve vaginal function. For patients with acceptable vaginal pressure, surgery could be helpful, but it is a more invasive procedure. Nonsurgical treatments, such as CO2 lasers, are more suitable and should have more beneficial effects on the vaginal mucosa. Therefore, the strategy for vaginal rejuvenation should be properly selected by doctors, as we have suggested (Figure 3).
Figure 3.
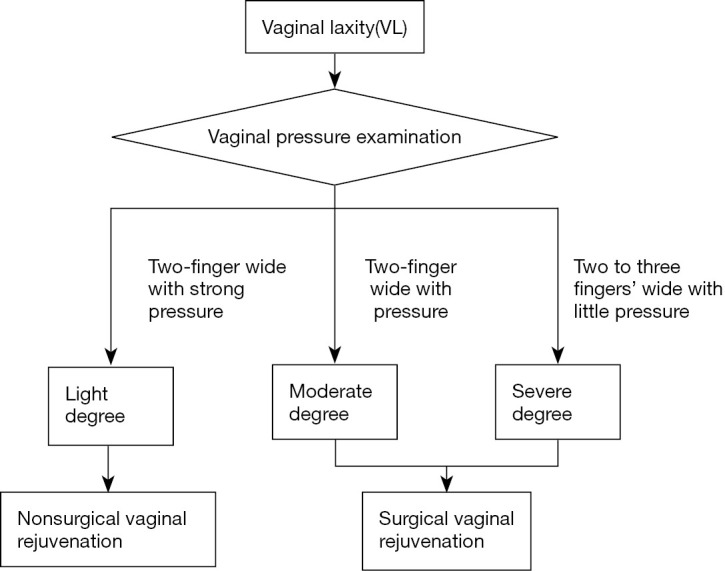
The strategy for vaginal rejuvenation.
The limitation of this study was that RF therapy was not included. As another popular nonsurgical treatment, RF can also restore vaginal tissue and improve sexual function (21). The mechanism of RF is similar to that of lasers in that RF mainly contributes to stimulating mucosal tissue activation and revitalization (21). In addition, the results of this study came from a single institution and involved a limited number of cases. Additional cases are needed in future clinical studies to further confirm our proposed approach. A multicenter study should be performed to increase the credibility of our research.
Conclusions
Vaginal rejuvenation can restore sexual function for women after childbirth. The strategy for vaginal rejuvenation should be selected based on the degree of vaginal laxity severity, which is measured by vaginal pressure. Surgical treatment, such as vaginoplasty, is suitable for severe- and moderate-degree vaginal laxity, while nonsurgical treatment, such as CO2 laser treatment, is suitable for light-degree vaginal laxity.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This work was supported by the Special fund of Chinese Association of Plastic and Aesthetics (No. FRPR201601-05).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of Shanghai Ninth People’s Hospital (No. 2017-302-T222). All patients signed informed consent forms.
Footnotes
Provenance and Peer Review: This article was commissioned by the Guest Editors (Drs. Oscar J. Manrique, John A Persing, and Xiaona Lu) for the series “Transgender Surgery” published in Annals of Translational Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-5655
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-5655
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-5655). The series “Transgender Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
References
- 1.Dietz HP, Wilson PD, Milsom I. Maternal birth trauma: why should it matter to urogynaecologists? Curr Opin Obstet Gynecol 2016;28:441-8. 10.1097/GCO.0000000000000304 [DOI] [PubMed] [Google Scholar]
- 2.de Araujo CC, Coelho SA, Stahlschmidt P, et al. Does vaginal delivery cause more damage to the pelvic floor than cesarean section as determined by 3D ultrasound evaluation? A systematic review. Int Urogynecol J 2018;29:639-45. 10.1007/s00192-018-3609-3 [DOI] [PubMed] [Google Scholar]
- 3.Kamisan Atan I, Gerges B, Shek KL, et al. The association between vaginal parity and hiatal dimensions: a retrospective observational study in a tertiary urogynaecological centre. BJOG 2015;122:867-72. 10.1111/1471-0528.12920 [DOI] [PubMed] [Google Scholar]
- 4.Ulubay M, Keskin U, Fidan U, et al. Safety, Efficiency, and Outcomes of Perineoplasty: Treatment of the Sensation of a Wide Vagina. Biomed Res Int 2016;2016:2495105. 10.1155/2016/2495105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qureshi AA, Sharma K, Thornton M, et al. Vaginal Laxity, Sexual Distress, and Sexual Dysfunction: A Cross-Sectional Study in a Plastic Surgery Practice. Aesthet Surg J 2018;38:873-80. 10.1093/asj/sjx255 [DOI] [PubMed] [Google Scholar]
- 6.Goodman MP, Placik OJ, Benson RH, 3rd, et al. A large multicenter outcome study of female genital plastic surgery. J Sex Med 2010;7:1565-77. 10.1111/j.1743-6109.2009.01573.x [DOI] [PubMed] [Google Scholar]
- 7.Vanaman M, Bolton J, Placik O, et al. Emerging Trends in Nonsurgical Female Genital Rejuvenation. Dermatol Surg 2016;42:1019-29. 10.1097/DSS.0000000000000697 [DOI] [PubMed] [Google Scholar]
- 8.Pauls RN, Fellner AN, Davila GW. Vaginal laxity: a poorly understood quality of life problem; a survey of physician members of the International Urogynecological Association (IUGA). Int Urogynecol J 2012;23:1435-48. 10.1007/s00192-012-1757-4 [DOI] [PubMed] [Google Scholar]
- 9.Placik OJ, Devgan LL. Female Genital and Vaginal Plastic Surgery: An Overview. Plast Reconstr Surg 2019;144:284e-97e. 10.1097/PRS.0000000000005883 [DOI] [PubMed] [Google Scholar]
- 10.Furnas HJ, Canales FL. Vaginoplasty and Perineoplasty. Plast Reconstr Surg Glob Open 2017;5:e1558. 10.1097/GOX.0000000000001558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.FDA Warns Against Use of Energy-Based Devices to Perform Vaginal "Rejuvenation" or Vaginal Cosmetic Procedures: FDA Safety Communication. Available online: https://wwwfdagov/MedicalDevices/Safety/AlertsandNotices/ucm615013htm
- 12.Abedi P, Jamali S, Tadayon M, et al. Effectiveness of selective vaginal tightening on sexual function among reproductive aged women in Iran with vaginal laxity: a quasi-experimental study. J Obstet Gynaecol Res 2014;40:526-31. 10.1111/jog.12195 [DOI] [PubMed] [Google Scholar]
- 13.Qureshi AA, Tenenbaum MM, Myckatyn TM. Nonsurgical Vulvovaginal Rejuvenation With Radiofrequency and Laser Devices: A Literature Review and Comprehensive Update for Aesthetic Surgeons. Aesthet Surg J 2018;38:302-11. 10.1093/asj/sjx138 [DOI] [PubMed] [Google Scholar]
- 14.Ostrzenski A. An acquired sensation of wide/smooth vagina: a new classification. Eur J Obstet Gynecol Reprod Biol 2011;158:97-100. 10.1016/j.ejogrb.2011.04.019 [DOI] [PubMed] [Google Scholar]
- 15.Jamali S, Abedi P, Rasekh A, et al. The Long Term Effect of Elective Colpoperineoplasty on Sexual Function in the Reproductive Aged Women in Iran. Int Sch Res Notices 2014;2014:912786. 10.1155/2014/912786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inan C, Agir MC, Sagir FG, et al. Assessment of the Effects of Perineoplasty on Female Sexual Function. Balkan Med J 2015;32:260-5. 10.5152/balkanmedj.2015.15073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woodward AP, Matthews CA. Outcomes of revision perineoplasty for persistent postpartum dyspareunia. Female Pelvic Med Reconstr Surg 2010;16:135-9. 10.1097/SPV.0b013e3181cc8702 [DOI] [PubMed] [Google Scholar]
- 18.Photiou L, Lin MJ, Dubin DP, et al. Review of non-invasive vulvovaginal rejuvenation. J Eur Acad Dermatol Venereol 2020;34:716-26. 10.1111/jdv.16066 [DOI] [PubMed] [Google Scholar]
- 19.Salvatore S, Franca K, Lotti T, et al. Early Regenerative Modifications of Human Postmenopausal Atrophic Vaginal Mucosa Following Fractional CO2 Laser Treatment. Open Access Maced J Med Sci 2018;6:6-14. 10.3889/oamjms.2018.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci 2015;30:429-36. 10.1007/s10103-014-1677-2 [DOI] [PubMed] [Google Scholar]
- 21.Sekiguchi Y, Utsugisawa Y, Azekosi Y, et al. Laxity of the vaginal introitus after childbirth: nonsurgical outpatient procedure for vaginal tissue restoration and improved sexual satisfaction using low-energy radiofrequency thermal therapy. J Womens Health (Larchmt) 2013;22:775-81. 10.1089/jwh.2012.4123 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as