Abstract
New York City is the metropolitan area in the United States with the highest number of new HIV diagnoses nationwide. The End-The-Epidemic (EtE) initiative calls for identifying persons with HIV who remain undiagnosed, linking and retaining persons living with HIV to maximize viral suppression, and facilitate access to pre-exposure prophylaxis (PrEP) for patients at increased risk of HIV. HIV screening represents the first step to both the primary and secondary HIV prevention cascades. We conducted an online, anonymous, cross-sectional survey of residents at all stages of training within four residency programs at one institution in Northern Manhattan between August 2017 and August 2018. All internal medicine, emergency medicine, obstetrics and gynecology trainees, and pediatrics were invited to complete the survey via email. Of 298 eligible trainees, 142 (48%) completed the survey. Most trainees were aware of the HIV testing law and agreed that HIV testing was their responsibility, but few successfully screened most of their patients. Most trainees were not knowledgeable about non-occupational post-exposure prophylaxis (nPEP) or PrEP, but felt that it was important to provide these services across settings. Barriers to HIV, nPEP, and PrEP varied across specialties. Ending the HIV epidemic will require efforts across clinical specialties. In this survey from an EtE jurisdiction, most trainees felt that it is important to provide HIV prevention services in most settings; however, their knowledge and comfort with HIV prevention services other than testing were low. Barriers varied across specialties, and developing specialty-specific materials for trainees may be beneficial.
Keywords: HIV prevention, PrEP, PEP, HIV testing, medical trainee, medical resident
Introduction
New York City is the metropolitan area in the United States with the highest number of new HIV diagnoses nationwide.1,2 Recognizing this urgent need, New York State proposed a multidimensional “End-The-Epidemic” (EtE) initiative to decrease new HIV infections and drive down prevalence by the end of 2020.3 The three-pillar initiative called for identifying persons with HIV who remained undiagnosed, linking and retaining persons living with HIV (PLWH) in care to maximize viral suppression (secondary prevention), and facilitating access to pre-exposure prophylaxis (PrEP) for patients at increased risk of HIV (primary prevention).3
HIV screening is the critical first step to both the primary and secondary HIV prevention cascades. HIV screening offers the opportunity to identify PLWH who may be undiagnosed and link them to care. Immediate antiretroviral therapy has become the standard of care as treatment as prevention has become widely accepted.
In addition to the crucial importance of diagnosing new cases of HIV, HIV screening presents a unique opportunity to identify and engage HIV-negative individuals in HIV prevention efforts and offer effective prevention services like non-occupational post-exposure prophylaxis (nPEP) and PrEP. Despite its importance, missed opportunities for HIV screening and referrals to HIV prevention services are common in both the adult and pediatric settings.4–9 Minimizing missed opportunities for HIV prevention will be required if we intend to “End-The-Epidemic”.
Studies show that a lack of knowledge and training among health care workers is a major hindrance to the provision of HIV prevention services.10 Graduate medical training, in which resident physicians complete mentored training, is an opportunity to improve provider delivery of HIV screening and provision of postexposure prophylaxis (PEP) and PrEP. During that time, physicians establish medical practices that they continue to access throughout their professional careers.11,12 Incorporating HIV screening, PrEP, and PEP into the training curriculum can support future screening practices, which is what is required to reach the EtE goals.
Methods
Design and setting
We conducted an online, anonymous, cross-sectional survey of residents at all stages of training within four residency programs between August 2017 and August 2018. All residents (n = 298) in internal medicine (IM), emergency medicine (EM), obstetrics and gynecology (Ob/Gyn), and pediatrics (Peds) were invited by chief residents, program directors, and faculty to complete the survey via email. Five recruitment reminders were sent during the course of the survey collection.
Questionnaire
The survey instrument was developed based on a review of the literature and the clinical experience of the investigative team. We assessed attitudes and practices around sexual health with a focus on perceived barriers to the provision of sexual health services [i.e., HIV screening, sexually transmitted infection (STI) screening, provision of PrEP and PEP services, and hepatitis C virus (HCV) screening]. The survey contained 56 questions; responses related to HCV and STI screening have been published elsewhere.13,14 During the survey, we defined routine screening as “lab-based screening for patients over age 13 in the absence of symptoms.”
The survey participants were first asked to demonstrate their knowledge of the New York State HIV testing law (mandates the offer of HIV testing to all patients aged 13 years or older) and the current guidelines for PrEP and PEP, specifically, the CDC and/or New York City Department of Health and Mental Hygiene (NYCDOHMH) guidelines. Subsequently, participants were asked to identify their comfort with identifying and assessing patients for PrEP and PEP eligibility.
Participants were then asked about their experiences with routine HIV screening, provision of PEP services, and provision and linkage to PrEP services. The responses were in agreement with statements about their attitudes and efficacy of routine screening using 5-point Likert-type scales (1-strongly disagree; 5-strongly agree). Responses were designed to encompass the steps needed to provide HIV prevention services starting from self-perceived job responsibility to successful provision of the HIV prevention service.
Participants were then asked to identify their top 3 barriers to routine screening for HIV (9 barriers), for PEP, and for PrEP (10 barriers) based on a list of barriers provided. The barriers were organized into four domains: constraints on the health delivery system and competing demands on the provider's time (3 barriers); follow-up of results (3 barriers); the provider's patient population (3 barriers); and training issues (1 barrier, PEP/PrEP only). Participants were asked to choose three of the potential barriers to provision of each of these services.
Data analysis
We conducted descriptive analyses to summarize the sample overall and grouped by residency program. Likert responses were treated as ordinal data, ranking the most negative response as 1 and most positive as 5. Where applicable, responses were combined. For each barrier, we report the percentage of individuals who chose that option.
This research protocol was approved by the Institutional Review Board at Columbia University Irving Medical Center.
Results
Trainee characteristics
Of the 298 eligible trainees, 142 (48%) completed the survey. The median survey response time was 17.5 min [interquartile range (IQR) 12–31]. Response rate did not differ by specialty, with a range of 46% (Peds) to 49% (IM). Overall, residents were more likely to be female (61%) and White (61%), with a median age of 29 (IQR 27– 30). Most trainees self-identified as heterosexual, and 10% identified as sexual minority. Overall, residents report taking an in-depth sexual history on 34% (IQR 19–70) of patients ranging from 10% (6–30) among emergency department (ED) trainees to 75% (50–81) in Peds (Table 1).
Table 1.
Demographics of Respondents
| Characteristic | Overall, n = 142a | IM n = 63a | Peds, n = 37a | EM, n = 28a | Ob/Gyn, n = 14a |
|---|---|---|---|---|---|
| Age | 29.00 (27.25, 30.00) | 28.00 (27.50, 30.00) | 28.00 (27.00, 29.00) | 29.50 (28.00, 31.50) | 28.50 (28.00, 29.75) |
| Self-identified gender | |||||
| Male | 56 (39%) | 25 (40%) | 13 (35%) | 16 (57%) | 2 (14%) |
| Female | 86 (61%) | 38 (60%) | 24 (65%) | 12 (43%) | 12 (86%) |
| Race/ethnicity | |||||
| Asian | 28 (20%) | 9 (14%) | 5 (14%) | 12 (43%) | 2 (14%) |
| Hispanic | 8 (5.6%) | 2 (3.2%) | 3 (8.1%) | 2 (7.1%) | 1 (7.1%) |
| Non-Hispanic Black | 2 (1.4%) | 0 (0%) | 1 (2.7%) | 1 (3.6%) | 0 (0%) |
| Non-Hispanic White | 87 (61%) | 42 (67%) | 26 (70%) | 8 (29%) | 11 (79%) |
| Prefer not to answer | 17 (12%) | 10 (16%) | 2 (5.4%) | 5 (18%) | 0 (0%) |
| Self-identified sexual identity | |||||
| Heterosexual | 126 (90%) | 54 (87%) | 35 (95%) | 26 (96%) | 11 (79%) |
| Gay or lesbian | 11 (7.9%) | 7 (11%) | 1 (2.7%) | 1 (3.7%) | 2 (14%) |
| Bisexual | 3 (2.1%) | 1 (1.6%) | 1 (2.7%) | 0 (0%) | 1 (7.1%) |
| Unknown | 2 | 1 | 0 | 1 | 0 |
| On what percentage of your patients older than the age of 13 years do you perform an in-depth sexual history | 34 (19, 70) | 30 (20, 41) | 75 (50, 81) | 10 (6, 30) | 50 (25, 80) |
Statistics presented: median (IQR): n (%).
EM, emergency medicine; IM, internal medicine; IQR, interquartile range; Ob/Gyn, obstetrics and gynecology; Peds, pediatrics.
HIV screening knowledge, responsibilities, implementation, and attitudes by location
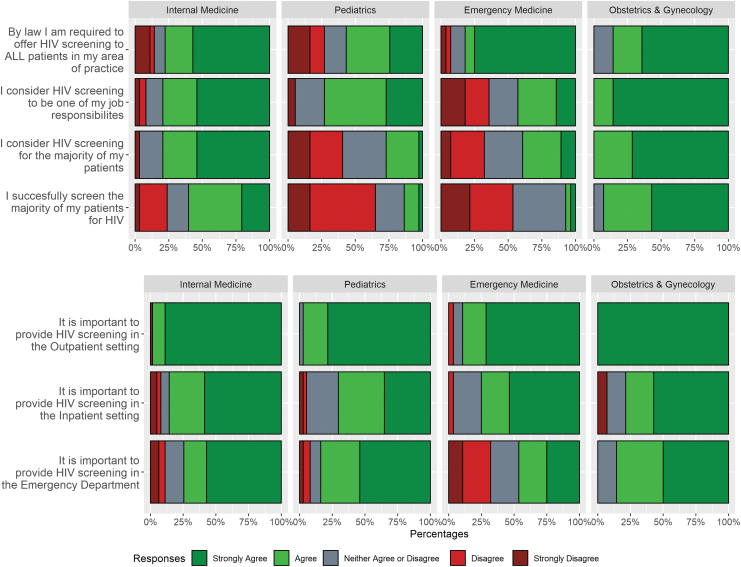
A majority of trainees were aware of the law to offer HIV screening (57–86%). Most trainees considered HIV screening one of their job responsibilities, but it varied from universally considered by Ob/Gyn (100%) to less than half of trainees in EM (43%). Participants' responses varied on whether they considered and successfully screened patients, with Ob/Gyn reporting the greatest agreement (100% and 93%) and EM the lowest (39% and 7%). Respondents universally agreed that providing HIV screening in the outpatient setting was important. The majority of respondents supported inpatient and ED HIV screening, with the exception of EM trainees in the ED (46%) (Fig. 1).
FIG. 1.
Knowledge, attitudes, and beliefs about routine HIV screening among trainees (n = 142) by area of training. The responses were in agreement with statements about their attitudes and efficacy of routine screening using 5-point Likert-type scales (1-strongly disagree; 5-strongly agree). HIV, human immunodeficiency virus. Color images available online.
Barriers to routine HIV screening
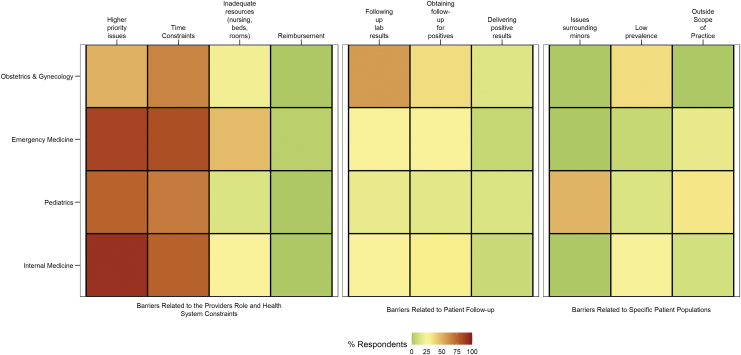
Of the three domains examined, health systems constraints posed the greatest barrier to respondents across all training programs, followed by barriers related to patient follow-up.
Specifically, higher priority issues and time constraints were the most frequently cited system barriers for EM (86%, 82%), IM (92%, 76%), Peds (76%, 68%), and Ob/Gyn (50%, 64%). Ob/Gyn had the widest variety of barriers chosen by at least one-third of participants, including following up laboratory results (57%), obtaining follow-up for positives (36%), and low prevalence (36%). Pediatrics was notably concerned with issues surrounding minors (49%). A number of trainees in Peds (32%, 14%), EM (18%, 7%), IM (11%, 24%), and OB (0% and 36%) felt HIV screening was outside their scope of practice and perceived the prevalence of HIV to be low, respectively (Fig. 2).
FIG. 2.
Self-reported barriers to routine HIV testing among trainees by area of training. Individuals were asked to identify their top 3 barriers to routine screening for HIV (n = 9), which were organized into three domains. Percent of individuals choosing any individual barrier were reported. HIV, human immunodeficiency virus. Color images available online.
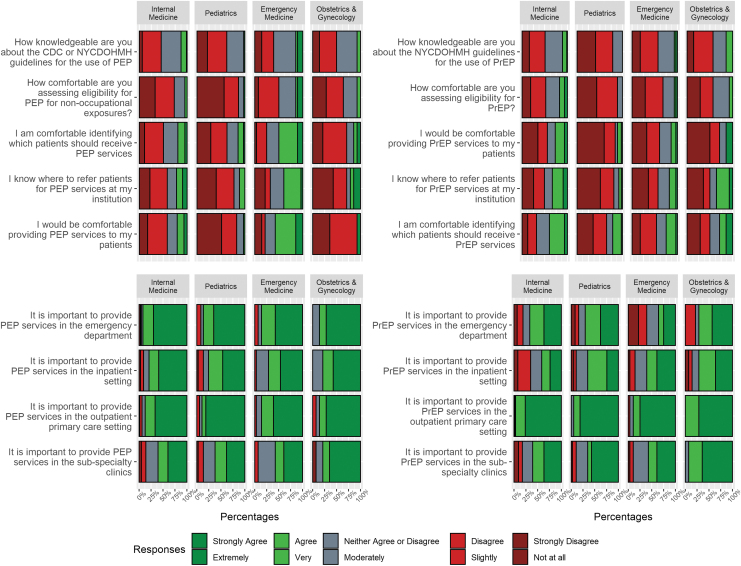
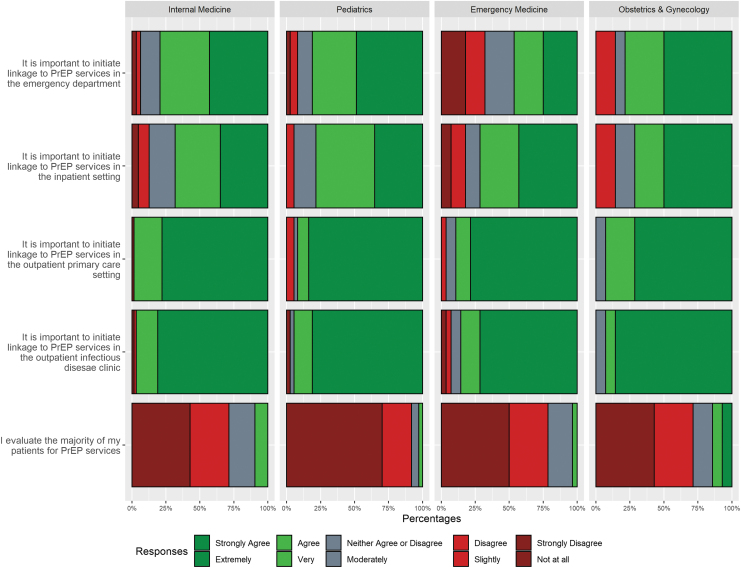
PrEP knowledge, responsibilities, implementation, and attitudes by location
Most trainees were neither knowledgeable (0–14%) about the guidelines for the use of PrEP nor comfortable (0–17%) assessing for PrEP eligibility (Fig. 3). The minority of trainees (22–40%) were comfortable identifying which patients should receive PrEP services, knew where to refer patients for PrEP (8–36%), or would be comfortable providing PrEP services to their patients (11–27%). Most trainees agreed that it was important to initiate linkage to PrEP services in the outpatient (89–98%), infectious disease clinic (86–97%), and inpatient (71–78%) settings. Only a minority (46%) of ED trainees felt that it was important to link patients to PrEP services in the ED, although an additional 21% neither agreed nor disagreed (Fig. 4). Virtually all providers agreed that it was important to provide PrEP services in the outpatient primary care setting (89–100%) and subspecialty clinics (57–93%). Most felt that it was important to provide PrEP services in the inpatient setting trainees (61–71%) except for IM (41%) and in the ED (67–71%) except for EM (36%) trainees (Fig. 3).
FIG. 3.
Knowledge, attitudes, and beliefs about the provision of postexposure and PrEP among trainees by area of training. Responses were in agreement with statements about their attitudes and efficacy of routine screening using 5-point Likert-type scales (1-strongly disagree; 5-strongly agree or 1-not at all; 5-extremely). Question stems were shortened for display purposes. PEP, postexposure prophylaxis; PrEP, pre-exposure prophylaxis; NYCDOHMH, New York City Department of Health and Mental Hygiene. Color images available online.
FIG. 4.
Attitudes about PrEP linkage among trainees by area of training. The responses were in agreement with statements about their attitudes and efficacy of PrEP linkage to care using 5-point Likert-type scales (1-strongly disagree; 5-strongly agree or 1-not at all; 5-extremely). PrEP, pre-exposure prophylaxis. Color images available online.
Barriers to provision of PrEP services
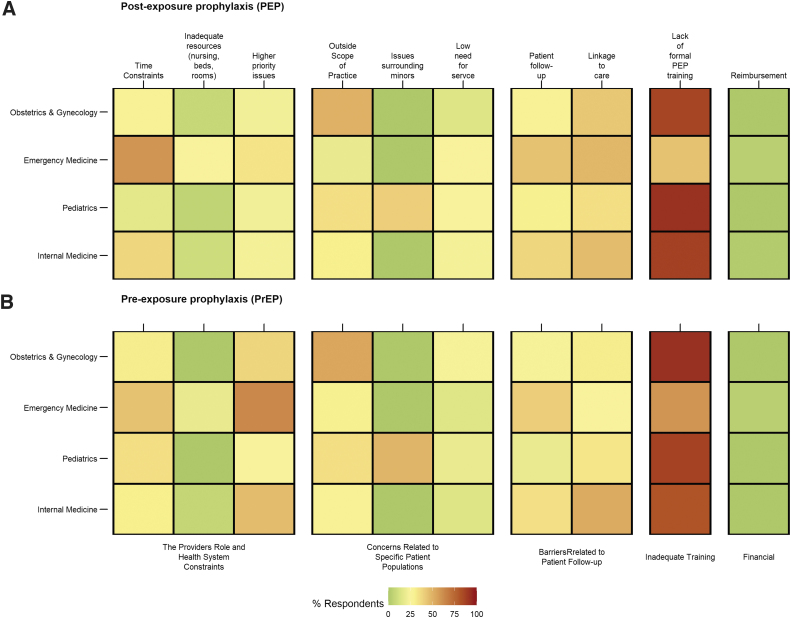
Of the four domains examined, inadequate training posed the greatest barrier to respondents across all training programs, Ob/Gyn (92%), EM (59%), Peds (87%), and IM (81%). Barriers were more diverse than seen for HIV screening, however, higher priority issues and time constraints were the most frequently cited system barriers for EM (63%, 44%), IM (46%, 30%), Peds (24%, 35%), and Ob/Gyn (39%, 31%). Patient follow-up was a significant barrier for EM (41%) and IM (35%) and linkage to care was a significant barrier for all four specialties, including 54% of IM trainees. Pediatrics was notably concerned with issues surrounding minors (49%). A considerable number of trainees in Peds (35%, 19%), EM (30%, 15%), IM (29%, 14%), and OB (54% and 23%) felt that providing PrEP services was outside their scope of practice and perceived the need for PrEP services to be low, respectively (Fig. 5).
FIG. 5.
Self-reported barriers to (A) PEP and (B) PrEP provision among trainees by area of training. Individuals were asked to identify their top 3 barriers to routine screening for HIV (n = 10), which were organized into four domains. Percent of individuals choosing any individual barrier were reported. PEP, postexposure prophylaxis; PrEP, pre-exposure prophylaxis. Color images available online.
nPEP knowledge, responsibilities, implementation, and attitudes by location
Most trainees were neither knowledgeable (3–14%) about the guidelines for the use of nPEP nor comfortable (3–14%) assessing for nPEP eligibility (Fig. 3). The minority of trainees in IM (19%), Peds (14%), and OB/GYN (14%) were comfortable identifying which patients should receive nPEP services, knew where to refer patients for PrEP (22%, 11%, and 21%) or would be comfortable providing nPEP services to their patients (21%, 3%, 7%). Notably EM residents were more likely to be comfortable identifying patients who should receive nPEP services (50%), know where to refer patients for nPEP (39%), and would be comfortable providing nPEP services (57%). Most trainees agreed that it was important to provide nPEP services in the outpatient (87–89%), inpatient (76–79%), and ED settings (86–92%). Substantially less trainees agreed with providing PEP in the subspecialty clinics (57–79%) (Fig. 3).
Barriers to provision of nPEP services
Of the four domains examined, inadequate training posed the greatest barrier to respondents across all training programs, Ob/Gyn (86%), EM (44%), Peds (92%), and IM (87%). Barriers were more diverse than seen for HIV screening and PrEP with barriers related to the provider's role and health system constraints notably lower than for HIV testing and PrEP and surpassing 50% only once (time constraints, EM, 59%). Notably barriers related to patient follow-up were most identified with patient follow-up and linkage to care the most frequently cited system barriers for EM (44%, 48%), IM (38%, 46%), Peds (30%, 35%), and Ob/Gyn (29%, 43%). Intriguingly patient follow-up was a significant barrier for EM (41%) and IM (35%) and linkage to care was a significant barrier for all four specialties, including 54% of IM trainees. Pediatrics was again concerned with issues surrounding minors (41%). A surprising number of trainees in Peds (35%), EM (19%), IM (30%), and OB (50%) felt that providing PEP services was outside their scope of practice (Fig. 5).
Discussion
HIV testing is the first step in the HIV prevention cascade and represents an opportunity to identify individuals living with HIV and link them to care as well as to identify individuals at risk and link them to comprehensive HIV testing services. The CDC HIV testing guidelines have been in place since 2006, and the NYS HIV testing law requiring an offering of testing has been in place since 2010. While it was reassuring that the vast majority of residents were aware of the law to offer HIV screening, it was concerning that slightly more than half of pediatric residents were aware of the requirement to screen patients older than 13 years of age. Most of the trainees surveyed agreed that they were responsible for screening their patients for HIV and indicated that they saw the importance of HIV screening in the inpatient, outpatient, and emergency room setting. The exception was the ED trainees. Only 43% of the ED trainees indicated that they felt it was the responsibility of emergency rooms to screen for HIV.
To achieve the pillars, set out by the EtE initiatives, low threshold, barrier-free services need to be in place for patients who have never been linked to HIV prevention and treatment can access these services. EDs in the United States have served as “safety nets” where patients seek care when they do not know where else to go. Routine HIV testing in EDs is critical as many of patients in the ED have an unknown HIV status. Studies have shown that many patients with newly diagnosed HIV had visited an emergency room before their diagnosis.4,6,15–17 HIV screening in the ED has also been proven to be cost effective.18 The American College of Emergency Room Physicians has endorsed HIV screening in the ED, however, with the very sensible caveats; screening is optimized to not interfere with the mission of the ED, integration exists with the health care system, and there are policies and procedures to address each set of the care cascade.19 To follow this endorsement and achieve the EtE aims, increased efforts are needed to educate trainees on the guidelines, procedures, and importance of universal HIV testing.
While Ob/Gyn (100%), Peds (73%), and IM (79%) agreed that HIV screening was one of their job responsibilities, there was remarkable drop-off for pediatrics when looking at consideration of HIV screening (27%) and successful HIV screening (14%). Issues surrounding minors was a significant concerning among pediatric trainees as was the feeling that HIV testing was outside their scope of practice. This highlights a significant education issue as NYS reclassified HIV as a STI, making it easier to expand testing, treatment, and prevention, and removing the requirement for parental consent. As HIV testing is the first step in the HIV prevention cascade it is critical to include patients of all ages, in particular the CDC stressed the importance of, “ targeting primary prevention efforts to persons aged <18 years, specifically those aged 16–17 years, and continuing through the period of elevated risk in the mid-twenties.”20
Despite internal efforts at trainee education by our HIV prevention program staff and a substantial effort by the city of New York through social marketing, very few trainees surveyed were knowledgeable about the NYCDOHMH guidelines for the administration of PEP and PrEP. A minority of providers were comfortable assessing eligibility, identifying candidates for services, providing services to their patients, or knew where to refer patients for HIV prevention services. Identifying PrEP and PEP candidates and providing services or knowing where to refer them is a necessary step in the provision of HIV prevention services. At our site, we have online guidelines and a “warm-line” (9 am to 5 pm) to provide guidance as well as arrange same-day visits for HIV prevention services. In addition, the city of New York also has a 24-h PEP hotline that can arrange for PEP starts remotely and arrange for follow-up at dedicated sites. However, these services are contingent on timely identification of individuals in need of these services. Once identified virtually, all providers agreed that providing linkage to PrEP services was important at all sites of care. While ED providers were hesitant about providing PrEP in the ED, there was considerable agreement about providing linkage. However, this may be hindered by most providers being unaware of where to refer patients for PEP and PrEP services. The identification of candidates for HIV prevention services and linkage to appropriate settings from the ED has significant potential as targeted screening has found that a substantial proportion of patients are PrEP eligible.21 Given the competing demands on ED providers; institutions focused on expanding HIV prevention services to the ED may be best served focusing on HIV testing and PrEP linkage as opposed to directly providing services.
When asked what barriers existed in providing HIV prevention services in their departments, the ED trainees, for example, listed that there were generally higher priority issues (86%), time constraints (82%), and inadequate resources (46%). PrEP uptake nationwide continues to be inadequate and inequitable, frequently missing subpopulations with the highest rates of HIV. To counter these trends, every medical specialty need be trained in the identification of candidates for HIV prevention services and the provision of PEP, and at a minimum linkage to PrEP services, if not provision. This requires the education of HIV Prevention modalities to trainees in all areas of medicine. Notably, emergency room trainees report higher priority issues. In the ED, patients will benefit from the provider understanding the importance of a PrEP referral after treating a patient for an STI or offering an HIV test, systems are needed to make this easier for providers. This includes things such as prescreening questionnaires, automated alerts, and nurse driven screenings that can allow patients to receive important health services without responsibility falling solely on the ED provider.
Ending the HIV epidemic will require efforts across clinical specialties. Medical education can “imprint” positive HIV prevention behaviors on providers, leading to an increase in the provision of HIV prevention services in the future. In this survey from an EtE jurisdiction, most trainees felt that it is important to provide HIV prevention services in most settings, however, their knowledge and comfort with HIV prevention services other than HIV testing were low. Trainees were uncomfortable identifying candidates for HIV prevention services, providing HIV prevention services, and were unsure where to refer patients for services they recognized as important. Barriers varied across specialties, however, developing specialty-specific materials and resources for trainees may be beneficial.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under award numbers K23AI150378, L30AI133789, and UM1AI069470.
References
- 1. New York State Department of Health AIDS Institute—HIV Epidemiological Profile—2016. 2016. Available at: https://www.health.ny.gov/diseases/aids/general/statistics/epi/docs/epi_profile2016.pdf (Last accessed August3, 2017).
- 2. Centers for Disease Control and Prevention. HIV Surveillance Report. 2017. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2017-vol-29.pdf (Last accessed May1, 2019).
- 3. New York State Department of Health AIDS Institute—2015 Blueprint on Ending the AIDS Epidemic. Available at: https://www.health.ny.gov/diseases/aids/ending_the_epidemic/index.htm (Last accessed October10, 2016)
- 4. Zucker J, Patterson B, Ellman T, et al. . Missed opportunities for engagement in the prevention continuum in a predominantly Black and Latino Community in New York City. AIDS Patient Care STDS 2018;32:432–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Joseph D, Zucker J, Cennimo D, Swaminathan S. Missed testing opportunities for HIV screening and early diagnosis in an urban tertiary care center. AIDS Res Treat 2017;2017:5708620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Felsen UR, Torian L V., Futterman DC, et al. . An expanded HIV screening strategy in the Emergency Department fails to identify most patients with undiagnosed infection: Insights from a blinded serosurvey. AIDS Care 2019;32:202–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Duffus WA, Davis HT, Byrd MD, Heidari K, Stephens TG, Gibson JJ. HIV testing in women: Missed opportunities. J Womens Health 2012;21:170–178 [DOI] [PubMed] [Google Scholar]
- 8. Joseph D, Zucker J, Cennimo D, et al. . Missed testing opportunities for HIV screening and early diagnosis in an urban tertiary care center. AIDS Res Treat 2017;2017:5708620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gutman CK, Middlebrooks L, Camacho-Gonzalez A, Shah B, Belay Z, Morris CR. Asymptomatic adolescent HIV: Identifying a role for universal HIV screening in the pediatric emergency department. AIDS Patient Care STDS 2020;34:373–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pleuhs B, Quinn KG, Walsh JL, Petroll AE, John SA. Health care provider barriers to HIV pre-exposure prophylaxis in the United States: A systematic review. AIDS Patient Care STDS 2020;34:111–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Phillips RL, Petterson SM, Bazemore AW, Wingrove P, Puffer JC. The effects of training institution practice costs, quality, and other characteristics on future practice. Ann Fam Med 2017;15:140–148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dine CJ, Bellini LM, Diemer G, et al. . Assessing correlations of physicians' practice intensity and certainty during residency training. J Grad Med Educ 2015;7:603–609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Winetsky D, Zucker J, Carnevale C, et al. . Attitudes, practices and perceived barriers to hepatitis C screening among medical residents at a large urban academic medical center. J Viral Hepat 2019;26:1355–1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zucker J, Carnevale C, Theodore D, et al. . Attitudes and perceived barriers to sexually transmitted infection screening among graduate medical trainees. Sex Transm Dis Available at: https://journals.lww.com/stdjournal/Abstract/9000/Attitudes_and_Perceived_Barriers_to_Sexually.97742.aspx [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 15. Zucker J, Cennimo D, Sugalski G, Swaminathan S. Identifying areas for improvement in the HIV screening process of a high-prevalence emergency department. AIDS Patient Care STDS 2016;30:247–253 [DOI] [PubMed] [Google Scholar]
- 16. Felsen UR, Bellin EY, Cunningham CO, Zingman BS. Unknown HIV status in the emergency department: Implications for expanded testing strategies HHS public access. J Int Assoc Provid AIDS Care 2016;15:313–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Torian L V, Felsen UR, Xia Q, et al. . Undiagnosed HIV and HCV infection in a New York City emergency department, 2015. Am J Public Health 2018;108:e1–e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jacobsen MM, Walensky RP. Modeling and cost-effectiveness in HIV prevention. Curr HIV/AIDS Rep 2016;13:64–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. ACEP Board of Directors. HIV Testing and Screening in the Emergency Department. 2014. Available at: https://www.acep.org/patient-care/policy-statements/hiv-testing-and-screening-in-the-emergency-department/
- 20. Ocfemia MCB, Dunville R, Zhang T, Barrios LC, Oster AM. HIV diagnoses among persons aged 13–29 years—United States, 2010–2014. MMWR Morb Mortal Wkly Rep 2018;67:212–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kulie P, Castel AD, Zheng Z, et al. . Targeted screening for HIV pre-exposure prophylaxis eligibility in two emergency departments in Washington, DC. AIDS Patient Care STDS 2020;34:516–522 [DOI] [PMC free article] [PubMed] [Google Scholar]