Abstract
Background:
Pyelonephritis is the most common bacterial infection in children that can cause renal failure if not diagnosed or treated early. We used serum biomarker interleukins (IL-6 and IL-8) and then confirmed the results by the findings dimercaptosuccinic acid (DMSA) scan to distinguish upper-tract infection from lower-tract infection.
Methods:
Serum IL-6 and IL-8 were measured in 57 children with newly diagnosed untreated urinary tract infection (UTI) documented by a positive urine culture. All children had a DMSA to determine whether serum IL6, IL-8 can be used as a marker to predict upper-tract from lower-tract infection. IL-6 and IL8 were determined by the enzyme link immunosorbent assay (ELISA) technique.
Results:
Of the 57 patients, 24 (42%) had renal parenchymal lesions on the DMSA scan. Patients with abnormal DMSA had significantly higher serum IL-6 and IL-8 compared with those with normal DMSA scan (187.1 ± 113.1 ng/mL vs. 396.1 ± 246.0 ng/mL, P = 0.005; and 165 ± 76.1 ng/mLvs. 190.8 ± 60.8 ng/mL, P = 0.026, respectively). Pyelonephritis was more frequent in children younger than 20 months old (n = 36, 63%, P < 0.005) and more prevalent in girls (n = 36, 63%, P = 0.005). Serum IL-6 had a sensitivity of 67.3% and a specificity of 63.0% and serum IL8 had a sensitivity of 80.1% and a specificity of 73.5% in the differential diagnosis of pyelonephritis and cystitis (P = 0.03).
Conclusions:
Serum levels of IL-6 and IL-8 are both sensitive biomarkers of UTI and can discriminate the upper from lower tract urinary infections. Determination of these biomarkers may help to identify patients with acute pyelonephritis and need for DMSA study.
Keywords: Children, cystitis, dimercaptosuccinic acid scan, interleukin-6, interleukin-8, pyelonephritis
Introduction
Urinary tract infection (UTI) is the most common bacterial infection in children and adolescents.[1,2] It is also one of the most common causes of hospitalizations among infants and toddlers. The clinical symptoms of the lower and upper UTI in young children are often uncharacteristic or nonspecific.[3] Further, accurate diagnosis and differentiation between lower and upper UTI is a major clinical challenge in clinical practice due to the high prevalence of UTI recurrence and long-term complications in children.[4]
Currently, the diagnosis of UTI is based on the presence of clinical symptoms in combination with the results of nitrite strip test indicating the presence of bacteria in the urine, presence of white blood cells in urine, and positive urine culture.[1,2] Urine culture is the gold standard in UTI diagnosis, but it is time consuming.[5]
Although 99 m Tc dimercaptosuccinic acid (DMSA) scintigraphy of the kidney is the gold standard in the diagnosis of acute pyelonephritis in children, its routine clinical use has several limitations.[6] The DSMA scan may not be readily available in all medical facilities; it involves exposure to radiation and is costly.
In recent years, number of novel biomarkers of UTI such as C-reactive protein,[7] secretory immunoglobulin A (IgA),[8] heparin-bonding protein,[9] α-1 microglobulin (α1 Mg),[10] interleukins, N-acetyl-beta-D-glucosaminidase (NAG)[11] and procalcitonin[12,13] have been identified to help to distinguish between upper-tract infection (pyelonephritis) and lower-tract infection (cystitis). Of these biomarkers, serum and urine interleukin 6 (IL-6) and interleukin 8 (IL-8) are shown to be more specific and sensitive markers of inflammation and early detection of acute pyelonephritis.[14,15,16,17]
The present study aimed to investigate the diagnostic significance of IL-6 and IL-8; the two promising UTI biomarkers to distinguish upper from lower tract urinary infections among children presenting with the first episode of UTI.
Methods
This prospective cross-sectional study was carried out to evaluate and compare serum IL-6 and IL-8 levels with the DMSA scan findings to differentiate upper-tract infection (pyelonephritis) from lower-tract infection (cystitis) in 57 children (ages between 12 months and 4 years) with the first episode of acute UTI in Amiralmomenin Hospital of Semnan University Medical Center, Semnan, Iran. Children with a known history of UTI, kidney disease, hypertension, or chronic infections were excluded from the study.
Urinalysis and urine culture were obtained in all children at the study onset. Children with positive urine cultures were enrolled in the study and all had kidney ultrasound and DMSA imaging studies. Blood for IL-6 and IL-8 determinations was obtained from each patient at the time of admission to the hospital. The blood samples were centrifuged and the serum was stored at −70°C until the time of analysis. IL-6 and IL-8 were measured using immunoassay enzyme link immunosorbent assay (ELISA) (Amazon Human IL-6 and IL-8 ELISA Kit).
Statistical analyses were performed using SPSS 16 software (SPPS, Inc, Chicago, Illinois). The normally distributed data were expressed as mean ± standard deviation. The differences of the variable were analyzed using Student's t-test. The Chi-square test was used for comparing serum IL-6 and IL-8 levels with DMSA scans. P value less than 0.05 was considered statistically significant. The number of participants needed for this study with a 95% confidence interval was 52 patients as validated by Altman DG, et al.[18]
The study was conducted in accordance with the Deceleration of Helsinki. Written parental informed consent was obtained for all participants prior to the study enrollment. The local health research ethic board before the commencement of the study approved the study Protocol.
Results
This prospective study was conducted between January 2017 and December 2018. The study population included 21 boys (38%) and 36 girls (62%) between 1 and 4 years old. Of these, 10 (27.2%) were less than 20 months. Of the 57 patients, 24 (42%) had pyelonephritis as documented by parenchymal lesions on the DMSA scans. The remaining 33 (58%) patients had normal findings on DMSA confirming lower UTI diagnosis [Table 1].
Table 1.
Clinical and laboratory characteristics of children with UTI
| Patients n=57 | Pyelonephritis n (%) | Lower UTI n (%) | Sensitivity % | Specificity % | P |
|---|---|---|---|---|---|
| <20 months, n=36 | 10 (27.8%) | 26 (72.2%) | - | - | 0.01 |
| ≥20 months, n=21 | 14 (66.7%) | 7 (33.3%) | - | - | |
| Serum IL-6 (ng/mL) | 187.1±113.1 | 165±76.1 | 67.3 | 63.0 | 0.04 |
| Serum IL-8 (ng/mL) | 396.1±246.0 | 190.8±60.8 | 80.1 | 73.5 | 0.02 |
| Parenchymal lesions on DMSA scan | 24 (42%) | - | - |
UTI=Urinary tract infection; IL-6=Interleukin-6; IL-8, Interleukin-8; DMSA=Dimercaptosuccinic acid
Patients with abnormal DMSA scan presented with febrile illness and all had significantly higher serum IL-6 and IL-8 compared with those with normal DMSA (187.1 ± 113.1 ng//mL vs. 396.1 ± 246.0 ng/mL, P = 0.005; and 165 ± 76.1 ng/mL vs. 190.8 ± 60.8 ng/mL, P < 0.026, respectively) [Table 1]. Serum levels of IL-6 and IL-8 did not differ significantly between the upper and lower urinary tract infections (p = 0.07). The cutoff levels for serum IL-6 and IL-8 to discriminate upper from lower UTI were 30 and 117 ng/mL, respectively.
Pyelonephritis was more frequent in children younger than 20 months old (n = 36, 63%, P < 0.005) and more prevalent in girls (n = 36, 63%, P = 0.005). Serum IL8 had a sensitivity of 80.1% and a specificity of 73.5% and serum IL-6 had a sensitivity of 67.3% and a specificity of 63.0% in the differential diagnosis of pyelonephritis and cystitis (p = 0.03) [Figure 1].
Figure 1.
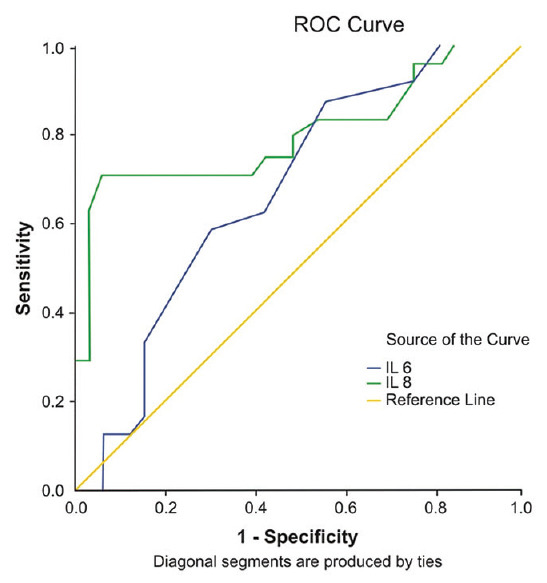
Comparison of serum interleukin-6 and interleukin-8 sensitivity and specificity to discriminating upper from lower urinary tract infection
Discussion
This study reports on the diagnosis and localization of the site of UTI in children using IL-6 and IL-8 as UTI biomarkers. Data suggest that serum levels of IL-8 and IL-6 have diagnostic value to differentiate between acute pyelonephritis and lower UTI in children less than 12 years old with the newly diagnosed untreated UTI.
The decision to choose IL-8 and IL-6 in this study was based on their specific bioactivity characteristics in response to inflammation of both white blood cells and the epithelial cells of the urinary tract.[13,14,15,16,17]
In the present study, serum IL-6 and IL-8 concentrations greater than 30 and 117 ng/mL were highly indicative of acute pyelonephritis, respectively. Based on the present study, serum IL-8 and IL-6 reached sensitivity 80% and 67% and specificity of 73% and 63%, for the diagnosis of pyelonephritis, respectively. Further, our study showed a positive correlation between renal parenchyma lesions and serum concentrations of IL-8 and IL-6.
The findings in the present are similar to the study reported by Sheu et al.[17] These authors found that the concentrations of both IL-8 and IL-6 were significantly higher in patient with pyelonephritis in comparison with the patients with lower UTI. They also compared the serum concentrations of both interleukins in patients with pyelonephritis that was confirmed by DMSA scan. In their study, serum IL-6 had a higher sensitivity and specificity for the diagnosis of pyelonephritis in comparison with serum IL-8.[17] Gurgoze, et al. also found serum IL-6 concentration was significantly higher in pyelonephritis than in lower UTI.[13]
In contrast to these studies, yet similar to our study, Otto et al. found serum concentration of IL-8 was significantly higher in patients with pyelonephritis than in the patients with lower tract infections.[19]
The discrepancy between the findings reported in our study and in the study reported by Sheu, et al. and Gurgoze, et al. regarding the diagnostic value of interleukins in separating lower from upper UTIs can be explained with a number of reasons. Perhaps one of the most important reasons for the discrepant findings is the diversity in the design of the studies, which include patient ethnicity, age of patient, history of previous, UTI, inflammatory syndromes, onset of UTI, and use of antimicrobial agents. The present study included children less than 12 years old with the newly diagnosed untreated UTI.
Conclusions
The present study suggests that IL-6 and IL-8 both are sensitive biomarkers of UTI that can differentiate acute pyelonephritis from lower urinary tract infections in children with the newly diagnosed untreated UTI. Measuring serum IL-6 and IL-8 may be a useful test for the diagnosis and localization of the site of UTI particularly in high-risk infants in whom pyelonephritis is the leading cause of infection.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Semnan University of Medical Sciences as part of a medical student graduation dissertation supported this study.
References
- 1.Foxman B, Brown P. Epidemiology of urinary tract infections: Transmission and risk factors, incidence, and costs. Infect Dis Clin North Am. 2003;17:227–41. doi: 10.1016/s0891-5520(03)00005-9. [DOI] [PubMed] [Google Scholar]
- 2.Paintsil E. Update on recent guidelines for the management of urinary tract infections in children: The shifting paradigm. Curr Opin Pediatr. 2013;25:88–94. doi: 10.1097/MOP.0b013e32835c14cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dulczak S, Kirk J. overview of the evaluation, diagnosis, and management of urinary tract infections in infants and children. Urologist Nurs. 2005;25:185–91. [PubMed] [Google Scholar]
- 4.Balighian E, Burke M. Urinary btractrial infections in children. Pediatr Rev. 2018;39:3–12. doi: 10.1542/pir.2017-0007. [DOI] [PubMed] [Google Scholar]
- 5.Urinary tract infection. Clinical practice guidelines for the diagnosis and management of the initial; UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011;128:595–610. doi: 10.1542/peds.2011-1330. www.pediatrics.org/chi/doi/10.1542/peds. 2011.1330. [DOI] [PubMed] [Google Scholar]
- 6.Puseljic S, Arambasic J, Gardasnanic J, Milan V, Puseljic I, Sipl M. The value of Tc99m-DMSA renal scintigraphy in evaluation of severity of parenchyma lesions in children with acute urinary tract infection. Acta Med Croatica. 2003;57:5–10. [PubMed] [Google Scholar]
- 7.Garin EH, Olavarria F, Araya C, Broussain M, Barrera C, Young L. Diagnostic significance of clinical and laboratory findings to localize site of urinary infection. Pediatr Nephrol. 2007;22:1002–6. doi: 10.1007/s00467-007-0465-7. [DOI] [PubMed] [Google Scholar]
- 8.Deo SS, Vaidya AK. Elevated levels of secretory immunoglobulin A (sIgA) in urinary tract infections. Indian J Pediatr. 2004;71:37–40. doi: 10.1007/BF02725654. [DOI] [PubMed] [Google Scholar]
- 9.Kjolvmark C, Pahlman L, Akesson P, Linder A. Heparin-binding protein: A. diagnostic biomarker of urinary tract infection in adults. Open Forum Infect Dis. 2014:1–ofu004. doi: 10.1093/ofid/ofu004. doi: 10.1093/ofid/ofu004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mantur M, Kemona H, Dabrowska M, Dabrowska J, Sobolewdki S, Prokopowicz J. Alpha 1-microglobin as a marker of proximal tubular in urinary tract infection in children. Clin Nephrol. 2000;53:283–87. [PubMed] [Google Scholar]
- 11.Vigano A, Assael BM, Dalla Villa A, Gagliardi L, Principi N, Ghezzi P, et al. N-acetyl-beta-D-glucosaminidase (NAG) isoenzyme in children with upper and Lower urinary tract infections. Clin Chim Acta. 1983;130:297–304. doi: 10.1016/0009-8981(83)90304-2. [DOI] [PubMed] [Google Scholar]
- 12.Kotoula A, Gardikis S, Tsalkidis A, Mantadakis S, Zissimopoulos A Kambori K, et al. Procalcitonin for the early prediction of renal parenchymal involment in children with UTI: Preliminary results. Int Urol Nephrol. 2009;41:393–9. doi: 10.1007/s11255-008-9472-2. [DOI] [PubMed] [Google Scholar]
- 13.Gurgoze MK, Akarsu S, Yilmaz E, Godekmerdan A, Akca Z, Ciftci I, et al. Proinflammatory cytokines and procalcitonin in children with acute pyelonephritis. Pediatr Nephrol. 2005;20:1445–8. doi: 10.1007/s00467-005-1941-6. [DOI] [PubMed] [Google Scholar]
- 14.Nanda N, Juthani-etha M. Novel biomarkers for the diagnosis of urinary tract infection-a systemic review. Biomark Insights. 2009;4:111–21. doi: 10.4137/bmi.s3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olszyna DP, Vermeulen H, Baan AH, Speelman P, van Deventer SJ, Gouma DJ, et al. Urine interleukin-8 is a marker for urinary tract infection in postoperative patients. Infection. 2001;29:274–7. doi: 10.1007/s15010-001-1157-z. [DOI] [PubMed] [Google Scholar]
- 16.Azab S, Zakaria M, Raafat M, Seief H. The combination of urinary IL-6 and renal biometry as useful diagnostic tools to differentiate acute pyelonephritis from lower urinary tract infection. Int Braz J Urol. 2016;42:810–6. doi: 10.1590/S1677-5538.IBJU.2016.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sheu JN, Chen MC, Lue KH, Cheng SL, Lee IC, Chen SM, et al. Serum and urine levels of interleukin-6 and interleukin-8 in children with acute pyelonephritis. Cytokine. 2006;36:276–82. doi: 10.1016/j.cyto.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Altman DG, Anderson PK. Calculating the number needed to treat for trials where the outcome is time to event. BMJ. 1999;319:1492–5. doi: 10.1136/bmj.319.7223.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Otto G, Burdick M, Strieter R, Godaly G. Chemokine response to febrile urinary tract infection. Kidney Int. 2005;68:62–70. doi: 10.1111/j.1523-1755.2005.00381.x. [DOI] [PubMed] [Google Scholar]


