Significance
Measles remains a major cause of infant death globally. On rare occasions, measles virus infection of the central nervous system (CNS) leads to a fatal progressive inflammation of the brain many years after the initial infection. MeV isolates from such CNS infections harbors fusion (F) protein mutations that result in a hyperfusogenic phenotype. The small number of hyperfusogenic MeV-F mutants identified thus far limits our ability to understand how these mutations are selected in the context of CNS infections. We performed a saturating mutagenesis screen of MeV-F to identify a large set of mutants that would mimic the hyperfusogenic phenotype of MeV-F in CNS infections. Characterization of these mutants shed light on other paramyxoviruses known to establish chronic CNS infections.
Keywords: measles virus, fusion, mutagenesis, viral encephalitis, Nipah virus
Abstract
Measles virus (MeV) is resurgent and caused >200,000 deaths in 2019. MeV infection can establish a chronic latent infection of the brain that can recrudesce months to years after recovery from the primary infection. Recrudescent MeV leads to fatal subacute sclerosing panencephalitis (SSPE) or measles inclusion body encephalitis (MIBE) as the virus spreads across multiple brain regions. Most clinical isolates of SSPE/MIBE strains show mutations in the fusion (F) gene that result in a hyperfusogenic phenotype in vitro and allow for efficient spread in primary human neurons. Wild-type MeV receptor-binding protein is indispensable for manifesting these mutant F phenotypes, even though neurons lack canonical MeV receptors (CD150/SLAMF1 or nectin-4). How such hyperfusogenic F mutants are selected and whether they confer a fitness advantage for efficient neuronal spread is unresolved. To better understand the fitness landscape that allows for the selection of such hyperfusogenic F mutants, we conducted a screen of ≥3.1 × 105 MeV-F point mutants in their genomic context. We rescued and amplified our genomic MeV-F mutant libraries in BSR-T7 cells under conditions in which MeV-F-T461I (a known SSPE mutant), but not wild-type MeV, can spread. We recovered known SSPE mutants but also characterized at least 15 hyperfusogenic F mutations with an SSPE phenotype. Structural mapping of these mutants onto the prefusion MeV-F trimer confirm and extend our understanding of the F regulatory domains in MeV-F. Our list of hyperfusogenic F mutants is a valuable resource for future studies into MeV neuropathogenesis and the regulation of paramyxovirus F.
Measles is a highly contagious acute infectious disease caused by measles virus (MeV) [Genus: morbillivirus, Family: Paramyxoviridae, and Order: Mononegavirales (1)]. There has been a resurgence of measles in recent years due to the lack or lapse of comprehensive vaccine coverage. The global incidence of measles in 2019 of 120 per million represents a 6.7-fold increase from its nadir in 2016 (18 per million). Primary MeV infections also caused an estimated 207,500 deaths globally the same year (2). These deaths occurred mostly in children under 5 y of age, who are also most susceptible to complications of pneumonia or diarrhea and dehydration. Measles continues to exert its toll after recovery from acute infection. Because of virus-induced depletion of B cell memory pools—a form of immunological amnesia—recovered children can become newly susceptible to common childhood infectious diseases (3–5). In the long term, MeV can also cause chronic latent central nervous system (CNS) infections such as measles inclusion body encephalitis (MIBE) and subacute sclerosing panencephalitis (SSPE) (6). MIBE is restricted to patients who are immunocompromised, whereas SSPE can occur in fully immunocompetent people 7 to 10 y after primary MeV infection (7). The incidence of SSPE is rare, although more recent estimates of its occurrence range from 22/100,000 to 30 to 59/100,000 in children that acquire measles before the age of five (8, 9). The fact that SSPE remains invariably fatal reflects our limited understanding of the neuropathogenic complications of measles.
MeV is a nonsegmented single-stranded negative sense RNA virus that is considered a prototypical paramyxovirus (10). Its genome encodes six genes that give rise to eight to nine proteins. The nucleocapsid (N) encapsidates the RNA genome forming RNase-resistant ribonucleoproteins (RNPs) during viral replication. The phospho-(P) and large (L) proteins form the RNA-dependent RNA polymerase complex that act as a viral transcriptase (P-L) or replicase (N-P-L) at appropriate points in the viral life cycle. The matrix (M) protein facilitates the assembly and budding of the RNP genome from the plasma membrane into virions that contain the fusion (F) and receptor binding proteins (RBP, formerly termed H). All paramyxoviruses require the coordinate action of F and RBP to mediate membrane F (11, 12). Some paramyxoviruses like MeV are preferentially cell associated, can spread cell to cell, and efficiently form multinucleated giant cell syncytia in appropriate receptor-positive cells (13).
Primary MeV strains use CD150 and nectin-4 on immune and epithelial cells, respectively (14, 15), neither of which are expressed on neurons or other brain parenchyma cells. This adds to the mystery of how MeV establishes a chronic latent CNS infection that recrudesces many years after recovery from the primary infection. However, characteristic mutations are known to arise in CNS MeV isolates from patients with SSPE or MIBE. Nonsense mutations that result in a nonfunctional M protein (16) and missense mutations that result in a hyperfusogenic F protein (17, 18) are commonly found. Recombinant MeVs with a functional deletion of the M protein or expressing the hypermutated M protein from an SSPE MeV isolate exhibit enhanced fusogenicity and increased neurovirulence (19, 20). Similarly, F mutants from neuropathogenic MeV strains also show a hyperfusogenic phenotype in cells that do not express detectable amounts of canonical MeV receptors (CD150 and nectin-4). This in vitro hyperfusogenic phenotype is correlated with the ability of neuropathogenic MeV strains to initiate a spreading infection in the CNS in vivo and in human neuronal cell cultures in vitro (21–23). However, syncytia are never observed in the brain or in human neuronal cells. It is unclear how neuropathogenic MeV spreads within the CNS and between neurons without forming syncytia. Proposed mechanisms include the use of an MeV neuronal receptor (although a definitive candidate has not been identified) (6) or host factors that could facilitate the putative transsynaptic spread mediated by the hyperfusogenic F protein (24). Nectin-elicited cytoplasmic transfer of MeV (25) has been proposed as a means to establish the initial transfer of infectious RNPs from epithelial cells to neurons but not subsequent CNS spread.
Regardless of the underlying mechanism, both MeV-F and RBP are indispensable for neuronal spread. This suggests that receptor engagement and F protein triggering remain essential for MeV spread in the CNS. The convergence of data indicates that the functional hallmark of mutations from SSPE and MIBE strains is the gain of a hyperfusogenic phenotype mediated by MeV-F. Importantly, these hyperfusogenic MeV-F mutants manifest their phenotype most clearly in cells that do not express the canonical MeV receptors (CD150 and nectin-4). For example, a single point mutant from the SSPE Osaka-2 strain (T461I) is able to confer upon wild-type (wt) MeV (IC323) the ability to form syncytia and replicate in Vero cells. Similarly, the recombinant IC323-T461I virus can now infect neurons in culture and cause substantial neuropathology when injected into brains of suckling hamsters (21). Hyperfusogenic F mutations are reported to reduce MeV virion production in CD150- and nectin-4–expressing cells (26), suggesting counterselection of hyperfusogenic mutation in CD150- and nectin-4–expressing cells.
The MeV-F protein is functionally constrained (27) and also well conserved among all clinical isolates (28). The hyperfusogenic F mutations that neuropathogenic MeV acquires must therefore benefit its spread in the CNS. Our ability to understand the fitness landscape of such MeV-F mutations is currently limited by the relatively small number of MeV-F mutations reported to exhibit such a hyperfusogenic SSPE phenotype (6, 29). A comprehensive account of the mutational spectrum that can give rise to this hyperfusogenic phenotype will facilitate a better understanding of how these MeV-F mutations confer their fitness advantage.
In this study, we generated a saturation point mutagenesis library of MeV-F in its genomic context. We then designed a fitness screen in which only viral genomes bearing MeV-F mutations that mimic the hyperfusogenic SSPE phenotype will have a selective advantage. We not only identified a number of MeV-F mutations similar to ones that have already been reported (6) but also numerous additional mutations that span all three structural domains of MeV-F (30). Structure–function studies confirm the SSPE phenotype of these mutations and identified a new site on the MeV-F trimer that regulates MeV-F activity. Finally, we identified a hyperfusogenic mutation in a highly conserved residue in the F peptide of MeV-F that was generalizable to Nipah virus (NiV), a member of the only other paramyxovirus genus known to harbor viruses that cause chronic latent CNS infections.
Results
Saturation Mutagenesis Screen for MeV-F Mutants with Hyperfusogenic SSPE Phenotypes.
Rationale.
The cardinal phenotype of hyperfusogenic MeV-F mutants from SSPE and MIBE strains is the ability to pair with wt MeV-RBP and form syncytia in cells that do not express the canonical MeV receptors. In order to better understand the mechanistic features that underlie the hyperfusogenic phenotype of such MeV-F mutants, we designed a screen of a saturating genomic MeV-F mutant library using BSR-T7 cells, where this phenotype was the most apparent and rMeV could be rescued with high efficiencies (27). As shown in Fig. S1, a rMeV bearing the well-characterized F-T461I hyperfusogenic mutant derived from the Osaka-2 SSPE strain (31) was able to infect, spread, and replicate in BSR-T7 cells, whereas its isogenic wt rMeV (IC323-GFP) counterpart could not. The latter confirms that BSR-T7 cells, a hamster-derived cell line, do not express the canonical MeV receptors, as wt rMeV-IC323 replicates well, and forms obvious syncytia in cells that express human CD150 or nectin-4 (32). Syncytia and spread (GFP counts) was readily observed with the control rMeV-F T461I hyperfusogenic mutant but not its isogenic wt counterpart (SI Appendix, Fig. S1 A and B). We observed significant differences as early as 2 d posttransfection/rescue. RT-qPCR for genome copy numbers confirmed productive replication of rMeV-F-T461I (SI Appendix, Fig. S1C), which produced several 1,000-fold more viral genomes than wt rMeV at day 8 postrescue.
Library preparation.
Next, we used error-prone PCR to generate a saturating mutagenesis library that covered the entire F gene. We reasoned that only mutants that result in the hyperfusogenic SSPE phenotype exemplified by rMeV-F-T461I would have a fitness advantage when rescued in BSR-T7 cells (SI Appendix, Fig. S1C). In order to rescue this MeV-F library in its genomic context and have the requisite coverage (SI Appendix, Table S1), we generated four independent mutagenesis libraries of equivalent sizes (402 to 418 nucleotides [nt]) that altogether span the entire MeV-F gene (Fig. 1A). The size limitation of each library (∼400 nt) was imposed by the maximum amplicon size we could sequence confidently on Illumina machines (250 nt paired-end [PE] reads). The cloning strategy to shuttle each mutagenesis library into the genomic context of rMeV-IC323 is depicted in Fig. 1B. Before embarking on making all four libraries, we randomly chose library 3 (MeV-F open reading frame, nt 840 to 1,241) to optimize our error-prone PCR conditions. Fig. 1C summarizes the distribution of mutation rates we observed when we sequenced library 3 generated from low, medium, and high error-prone PCR conditions. Sequencing the same region amplified with high-fidelity DNA polymerase served as our background control. The mutations were evenly distributed across this library 3 region regardless of mutation rates (SI Appendix, Fig. S2 A–D), which averaged 0.04% for plasmid DNA (background) and 0.12%, 0.18%, and 0.27% for the low, medium, and high mutation settings, respectively (SI Appendix, Fig. S2E). The mutational spectrum was also relatively unskewed with a transition/transversion (Ts/Tv) ratio close to 1 (0.81). We chose the high error rate condition to move forward with all four libraries because we aimed to introduce one mutation/400 bp (0.25%), which was the size of each library segment. When we set the threshold detection limit for mutations at 0.08% (double the sequencing error rate [0.04%] of the negative control in SI Appendix, Fig. S2E) and used the high “mutational setting” for our error-prone PCR conditions, 97.3% of the region covered in library 3 were mutated.
Fig. 1.
Preparation of genomic MeV-F saturation mutagenesis libraries. (A) Schematic of MeV-F showing the relevant structural and functional domains. Domain 1, 2, and 3 are defined in the previous study (12, 49). Domain 1, 2, and 3 correspond to β barrel domain in the head, immunoglobulin-like domain in the head, and the neck. Regions targeted by libraries of 1 to 4 are indicated below the schematic. The nt and aa positions in the MeV-F open reading frame (ORF) are indicated counting from the initiator methionine. (B) The strategy for using error-prone PCR to construct the MeV-F saturating mutagenesis library in its genomic context is shown. Point mutations in a given library region of F gene were introduced first by error-prone PCR (red X box). Backbone DNA was prepared by high-fidelity PCR. Then, insert and backbone DNA was assembled by exonuclease, DNA polymerase, and DNA ligase with NEBuilder (NEB). The full F ORF, now containing the mutated F library region and flanked by NruI/PacI restriction sites, was then transferred to the MeV genome-coding plasmid via direct ligation using the same unique restriction sites in the untranslated regions flanking the MeV-F gene. In this way, four independent measles genome plasmid libraries were generated with saturating F mutations that altogether cover the entire gene. (C) The distribution of mutation rates in pcDNA-MV323-F libraries (library 3) generated under low, medium, or high error-prone PCR conditions or amplified with high-fidelity DNA polymerase from the parental “plasmid” is shown. Mutation rates of individual position in the insert (840 to 1,241 nt) were evaluated by NGS, then the distribution of mutation rates at each nt position was shown in box-and-whisker plot. The plot shows the 10/90 percentile (whisker), 25/75 percentile (box), and median (horizontal bar), which summarizes the NGS data shown in SI Appendix, Fig. S2.
When the rest of libraries (1, 2, and 4) in pCDNA3-morbillivirus (MV)-F were made with the same high mutation setting, there was also no obvious skewing in the distribution and spectrum of mutations (SI Appendix, Fig. S3 A–C). The mutation rate of libraries 1 (0.33%), 2 (0.27%), and 4 (0.22%) were similar to that of library 3 (0.25%), and all had Ts/Tv ratios close to 1 (SI Appendix, Fig. S3D). Then, each of the F gene–mutated libraries were independently transferred into the genome coding plasmid as depicted in Fig. 1B. Sequencing of the MeV-F libraries in the MeV genome showed that the mutation rate and spectrum were maintained in all libraries, with the exception of library 4 where, for unknown reasons, the average mutation rate dropped from 0.22 to 0.14% (SI Appendix, Table S1). Given that we aimed for one mutation/400 bp and that saturation point mutagenesis requires ∼1,600 distinct mutations/library, the number of independent genomic clones we generated per library (range: 2.32 to 8.55 × 104) ensured that every possible nt substitution at every position was adequately represented. This was confirmed by deep sequencing our genomic libraries where, as expected, the coverage was 99% for all libraries except library 4 (SI Appendix, Table S1).
Identification of Putative Hyperfusogenic MeV-F Genomic Clones in Our Library Screens.
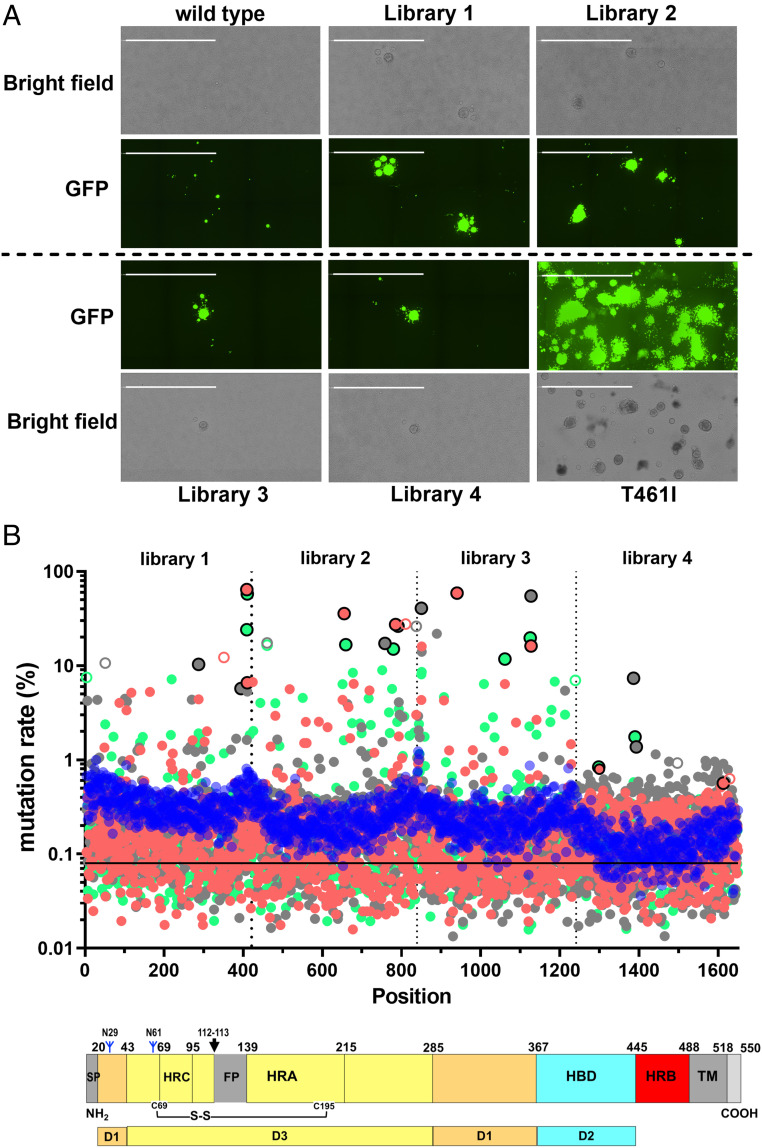
We then used our efficient reverse genetics system to rescue wt MeV (IC323-GFP), the four MeV-F mutated libraries, and the hyperfusogenic rMeV-F-T461I (positive control) in BSR-T7 cells as described in SI Appendix, Fig. S1 (27, 33). The virus producer cells were grown for 8 d with one passage at day 4. The average number of rescue events in each of these screening trials were around 60,000 to 90,000, which is sufficient to represent the mutational diversity present in each library (SI Appendix, Table S1). When wt rMeV-IC323 was rescued and passaged under these conditions, only single cells turned EGFP+, which did not spread. In contrast, libraries 1 to 4 each gave rise to obvious foci of spreading EGFP+ syncytia by day 8 (Fig. 2A). Each of these large spreading syncytia likely represents a hyperfusogenic mutant similar to that seen with the MeV-F-T461I positive control. These phenotypic observations were confirmed and extended upon analysis of F gene sequences by next-generation sequencing (NGS) at 8 d postrescue. While the genome plasmid libraries contained a relatively even distribution of mutations, we detected a clear selection of fit mutants in all four MeV-F libraries at day 8 postrescue (Fig. 2B).
Fig. 2.
Fitness screen of MeV-F mutagenesis libraries identifies hyperfusogenic F mutants. (A) Representative images from rescue of MeV-F libraries at 8 dpt in BSR-T7 cells show spreading GFP+ syncytia of varying sizes in all libraries except for wt MeV, suggesting that hyperfusogenic mutants are being positively selected. The T461I rescue well showed multiple giant syncytia as expected since only a single clone was transfected. Images were captured by the Celigo Imaging Cytometer (Nexcelom) and is a computational composite of several identical fields of view taken in each well. (Scale Bar, 2 mm.) (B) Mutation rate across the F gene in our saturation mutagenesis genome plasmid libraries before transfection and rescue are indicated by the solid blue circles. The horizontal line at 0.08% represents the threshold we used to define a genuine mutation at any given position. Distribution statistics of the mutants in each genomic library is given in SI Appendix, Table S1. Salmon (replicate 1), gray (replicate 2), and green solid circles (replicate 3) represent the mutation rate for each library rescued three independent times (replicates 1 to 3 for libraries 1 to 4 = 12× total) based on MeV-F genomic RNA extracted from BSR-T7 cells at 8 d postrescue. The graph is a concatenation of deep sequencing results of libraries 1, 2, 3, and 4. The salmon, gray, and green circles outlined in black represent the two most predominant mutants in each library and replicate as indicated in SI Appendix, Table S2. These mutants were chosen for functional validation in Fig. 3. The open circles correspond to synonymous passenger mutations that were associated with their cognate hyperfusogenic mutants (detailed in SI Appendix, Table S2). A scaled schematic of the MeV-F protein is shown below the graph for interpretative convenience. SP, signal peptide; HRC, Heptad repeat C; FP, fusion peptide; HRA, heptad repeat A; HRB, heptad repeat B; TM, transmembrane domain. D1, D2, and D3 in F protein correspond to domains 1, 2, and 3 in Fig. 1A.
Each library was independently passaged three times for a total of 12 replicates that made up the screen of the entire MeV-F gene. Some mutants were reproducibly selected in more than one replicate (e.g., L137H and L137F) and/or can account for more than 50% of the library reads at that position (e.g., G376V, T314P, and L137F). SI Appendix, Table S2 shows the top hit list from these screening experiments. Mutants selected from each library in each replicate were ranked by their percent representation at that position. Despite some stochasticity, it was clear that some amino acids (aa) positions or microdomains were hotspots for mutations that putatively conferred a hyperfusogenic phenotype. This was underscored by the G376V mutant in library 3, which not only dominated the outgrowth of mutants in replicate 1 and 2, but also, a “fourth” replicate performed during our preliminary optimization experiments (SI Appendix, Table S3). The synonymous mutations that showed up as top hits in SI Appendix, Table S2 (e.g., nt 351 mutant in replicate 1 of library 1) were almost always on the same reads of other putative hyperfusogenic mutants, suggesting that these were “passenger” mutations.
Library 4 appeared to be an outlier in that the top hits in all three replicates never exceeded 2%, except for N462K in replicate 2 (7.3%). The relatively low mutation rate in the genome library (0.14% versus 0.25 to 0.35% for libraries 1 to 3, SI Appendix, Table S1) might have reduced the efficiency and spread of mutants that would have otherwise been detected as hyperfusogenic. Remarkably, we were still able to detect and select for previously reported hyperfusogenic mutants such as N462K (34) and N465S (21) in addition to new mutations like G464W.
Selected MeV-F Mutants Have a Hyperfusogenic Phenotype.
We developed a quantitative image-based F assay (QIFA) to evaluate the L number of potential hyperfusogenic MeV-F mutants identified in our screen. QIFA is premised upon detecting syncytia frequency in which syncytia are defined by statistically robust criteria. We first transfected Lifeact-EGFP alone into BSR-T7 cells and obtained a size distribution of single cells in the absence of any syncytia (SI Appendix, Fig. S4A). We observed that 13 pixels was the median size of single-cell populations (n = 2,605), and GFP objects 260 pixels (20× median single-cell size) were rare in that more than 99% of cells imaged were <260 pixels. So, we defined a bona fide syncytium as having 260 pixels and calculated syncytia frequency as a percent (%) of total GFP counts. To help us identify syncytia, we transfected increasing amounts of plasmids expressing MeV-RBP and F-T461I along with a fixed amount Lifeact-EGFP. Our QIFA was highly specific and quantitative, but the QIFA metric (syncytia frequency %) had a dynamic range that plateaued around 8 to 10% (SI Appendix, Fig. S4 B and C). The massive syncytia that formed in a finite area (e.g., between 50 and 100 ng MeV-RBP/F-T461I transfected) limits the numerator. Nonetheless, the assay could be made more or less sensitive by simply increasing or decreasing the hours posttransfection (hpt) before syncytia are quantified (see below).
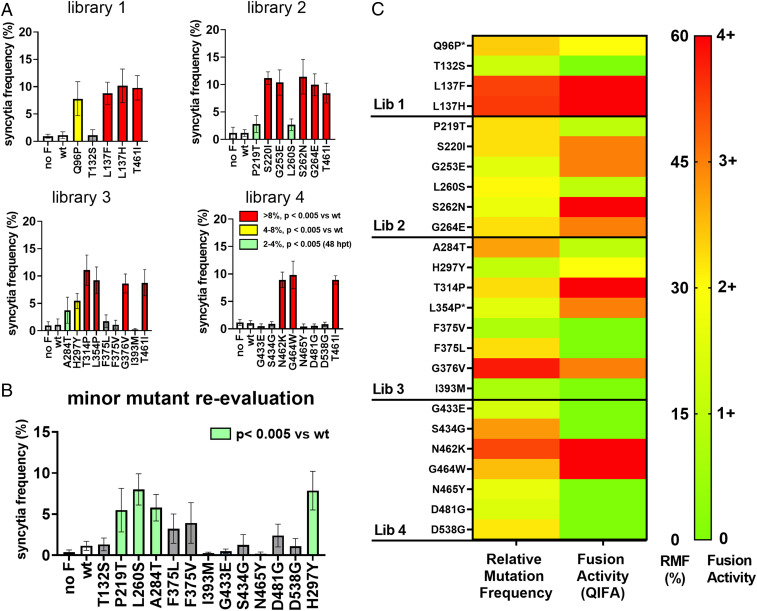
Next, we chose the best two nonsynonymous mutants from each individual experiment in SI Appendix, Table S2 (Library 1: Q96P, T132S, L137H, and L137F; Library 2: P219T, S220I, G253E, L260S, S262N, and G264E; Library 3: A284T, H297Y, T314P, L354P, F375L, and G376V; and Library 4: G433E, S434G, N462K, G464W, N465Y, and D538G) plus two mutants (F375V and I393M) from the preliminary screen of library 3 (SI Appendix, Table S3). We also included the D481G mutant (third-best mutant in replicate 2 of library 4) because this corresponds to stalk region in which no previous hyper-F mutant was reported. We tested F activity of these mutants in comparison with wt F protein, which remained mostly as single cells. Several mutants (L137H, L137F, S220I, G253E, S262N, G264E, T314P, L354P, G376V, and G464W) showed greatly increased F activity ( 8%) comparable to the positive control T461I mutant (Fig. 3A and SI Appendix, Fig. S5A) at 30 hpt. Some (Q96P and H297Y) showed moderately increased F activity (<8%). Others (P219T, L260S, A284T, and F375V) showed only slightly increased syncytia frequency, which only became statistically significant from wt at 48 hpt (Fig. 3B and SI Appendix, Fig. S5B).
Fig. 3.
Validation of selected hyperfusogenic MeV-F mutants by a QIFA. We selected the top-two mutants from each replicate experiment across all four libraries (SI Appendix, Table S2) to assess their F phenotype (see text for details). We transfected MeV-F/RBP-F and Lifeact-EGFP into BSRT-T7 cells and quantified syncytia formation via our QIFA as described in SI Appendix, Fig. S4. (A) Standard QIFA using 200 ng each of MeV-RBP and the indicated MeV-F. Images were captured at 30 hpt and analyzed. Data shown are mean (± SD) syncytia frequency (%) per total GFP counts from five independent experiments. Red, yellow, and green bars indicate syncytia formation at the levels indicated in the key. Dunnet’s multiple comparison test was used for the detection of statistically significant differences above wt MeV-RBP and F. Mutants from each library were assayed with MeV-F-T461I always serving as a positive internal control. Representative images of the summary data in A are shown in SI Appendix, Fig. S5A. For mutants that did not show significant syncytia at 30 hpt, we reevaluated them at 48 hpt. (B) Representative F images of C are shown in SI Appendix, Fig. S5B. A heat map summarizes how well the putative hyperfusogenic mutants identified in our library screens correspond to their fusogenic activity. (C) Since each library had a different average mutation rate (SI Appendix, Table S1) and each replicate was independently rescued and passaged, we first calculated the relative mutation frequency (RMF) for each of the top-ranked mutants (SI Appendix, Table S2). RMF = the mutation rate for a given mutation/highest mutation rate for that experiment. In this way, the highest ranked mutant in each library for a given replicate was always 100%, and all mutants in that experiment were enriched relative to that highest ranked mutant. (Left) The RMF for the indicated mutants from all three replicates can thus be averaged and shown as mean RMF. (Right) The F activity for the same mutants was categorized into five groups: 0, same as wt; 1+, syncytia visible only after 48 h; 2+, 4 to 8% at 30 hpt; 3+, 8% at 30 hpt; and 4+, significantly different from wt at low expression conditions (25 ng MeV-RBP/F transfected) (SI Appendix, Fig. S4).
To further differentiate between all the hyperfusogenic mutants that gave ≥8% syncytia frequency, we repeated our QIFA on these mutants using less amounts of transfected MeV-F/RBP (25 ng each). Under these limiting conditions, 6 of the 11 mutants still showed significant syncytia formation above wt (SI Appendix, Fig. S6 A and B), as did our positive control T461I mutant. These mutants were located in the C terminus of the F peptide (L137F and L137H), at the protomer interface (S262N), and in the neck region between the head and stalk domains (T314P, N462K, and G464W).
Although there was a general correlation between the relative mutational frequency of the dominant mutants identified in the screening experiments and their fusogenicity as measured by our QIFA, not all the mutants identified in the screening experiments were hyperfusogenic (Fig. 3C). Nonetheless, we were able to identify at least 15 MeV-F mutations that had a hyperfusogenic SSPE phenotype, effectively doubling the list of hyperfusogenic SSPE-like mutants to date (SI Appendix, Table S4).
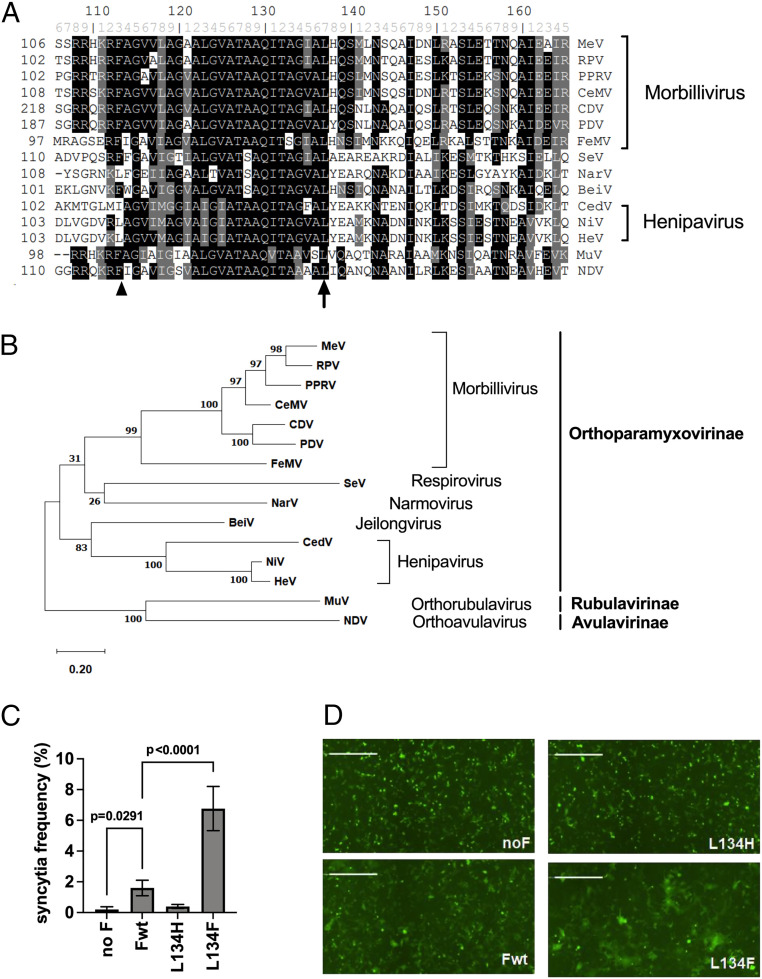
A Hyperfusogenic Mutation in the Conserved F Peptide Region Is Generalizable to the NiV F Protein.
L137F and L137H mutants repeatedly showed up and were often the predominant mutations in all three replicates of library 1 screens (SI Appendix, Table S2). In addition, our QIFA revealed L137F and L137H to be as hyperfusogenic as the positive control T461I mutant (Fig. 3A). L137 in MeV-F is located toward the C terminus of the F peptide. The homologous leucine is conserved among all major paramyxoviruses (Fig. 4A), as demonstrated by our alignment of the F peptide region from the indicated viruses. We chose an overrepresentation of F proteins from MVs and henipaviruses, as paramyxoviruses that use protein-based receptors may have differential features for F activation (35). Nonetheless, a phylogenetic tree shows that we chose prototypical viruses that span the diversity within the Paramyxoviridae (Fig. 5B). We speculated that mutation in this position may also change the F activity of other paramyxoviruses, particularly those of henipaviruses, the only other genus of paramyxoviruses known to use protein receptors and also cause chronic latent CNS infections (36). Thus, we introduced these mutations into NiV-F (L134H and L134F) and evaluated their F activity (when cotransfected with NiV-RBP) by our QIFA. L134F markedly enhanced the F activity of NiV-F beyond wt, whereas L134H did not (Fig. 4 C and D). Interestingly, L137F was also significantly more hyperfusogenic than L137H when F was evaluated under limiting conditions (SI Appendix, Fig. S6 A and B).
Fig. 4.
The homologous mutation of MeV-F-L137F in NiV-F (NiV-F-L134F) renders NiV-F hyperfusogenic. (A) The aa sequence alignment of the F peptide region flanking the L137 residue in MeV (arrow) shows that it is highly conserved among paramyoviruses. The F1/F2 protease cleavage site (arrowhead) is indicated as a point of reference. Prototypic viruses were chosen to represent paramyxoviruses from all three subfamilies and the major genera within each subfamily. (B) A phylogenetic tree of the F protein sequence demonstrates that the selected F proteins span the diversity within Paramyxoviridae. The aa sequences were aligned by clustalw, and the phylogeny was generated by the maximum likelihood method using MEGA 10 (version 10.1.8). The numbers at the node indicate the fidelity by bootstrap test (1,000 times). The scale indicates substitutions per site. (C) Introduction of the homologous mutation at this position (L134F) made the NiV-F protein hyperfusogenic. F activity in NiV-RBP and F-transfected cells was evaluated by our QIFA as described in Fig. S4. Mean values of five independent experiments are shown with error bar indicating SD. Dunnet’s multiple comparison test was used for tests of significance for the indicated comparisons. (D) Representative images of data presented in B. Images were generated by the Celigo Imaging Cytometer, as described in previous figures. (Scale Bar, 500 μm.) F protein sequences are from measles virus (MeV, NP_056922), canine distemper virus (CDV, NP_047205), rinderpest virus (RPV, YP_087124), peste-des-petitis-ruminants virus (PPRV, YP_133826), phocine distemper virus (PDV, YP_009177602), cetacean morbillivirus (CeMV, NP_945028), feline morbillivirus (FeMV, YP_009512962), Sendai virus (SeV, NP_056877), mumps virus (MuV, NP_054711), Nipah virus (NiV, NP_112026) Hendra virus (HeV, NP_047111), Cedar virus (CedV, YP_009094085), Newcastle disease virus (NDV, YP_009513197), Nariva virus (NarV, YP_006347587), and Beilong virus (BeiV, YP_512250).
Fig. 5.
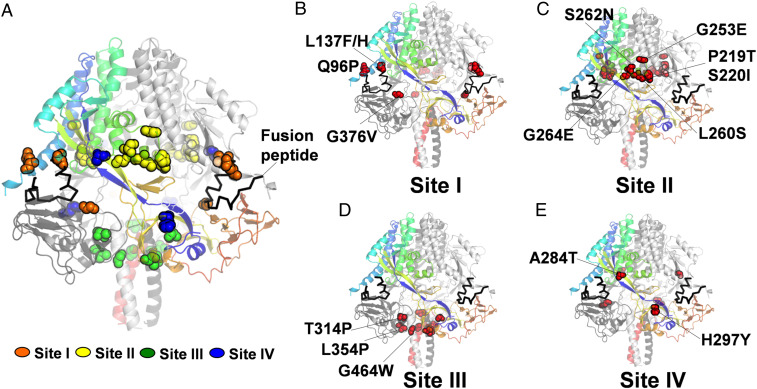
Structural mapping of hyperfusogenic F mutants. (A) The aa residues (spheres) whose substitutions confer hyperfusogenicity were mapped onto the trimeric prefusion MeV-F structure (Protein Data Bank: 5YXW) using Pymol. A ribbon model is shown in which each of the protomers is colored rainbow, dark gray, and light gray, respectively. (B–D) The majority of mutants discovered in this study, while novel, mapped to the three sites (I, II, and III) that were previously used to classify extant hyperfusogenic mutants by Hashiguchi et al. (E) Two mutants, A284T and H297Y, mapped to a structurally distinct beta sheet that connects the head and neck domains, which we term site IV. (A) In the aggregate model showing all the mutants, site I to IV mutants are represented by orange, yellow, green, and blue spheres, respectively.
Structural Mapping of Hyperfusogenic MeV-F Mutations.
Extant hyperfusogenic mutations in MeV-F can be categorized into three sites based on how they mapped onto the crystal structure of stabilized trimeric MeV-F (30). Site I mutations are in the region surrounding the fusion peptide, site II mutants localize to the interface of the protomers, and site III mutations cluster in the neck domain between head and stalk. Most of our hyperfusogenic mutants mapped to one of these sites (Fig. 5A). Mutants mapping to site I (Q96P, L137F, L137H, F375V, and G376V, Fig. 5B) can potentially affect F peptide exposure and the biophysical properties of the F peptide itself. Site II mutants such as P219T, S220I, G253E, L260S, S262N, and G264E (Fig. 5C) can disrupt the interprotomer interactions that keep F from being prematurely triggered. Site III mutants (T314P, L354P, and G464W) at the base of the head domain (Fig. 5D) can also destabilize the F trimer, resulting in lower activation energy for F triggering. Interestingly, two of our hyperfusogenic mutants, A284T and H297Y, are located on the beta sheet connecting the head and neck region (corresponds to Y277 to G301). This region is structurally distinct from sites I to III and no hyperfusogenic SSPE-derived mutants have been mapped to this beta sheet. We propose classifying this region as site IV, which may represent an F-regulatory domain encompassing at least the two mutants identified in our study (Fig. 5E, A284T and H297Y).
Recombinant Measles Virus Expressing Selected Hyperfusogenic F Mutants Recapitulate the SSPE Phenotype.
To confirm that the hyperfusogenic MeV-F mutants identified in our screen was necessary and sufficient to confer an SSPE phenotype, we chose four mutants (L137F, S262N, H297Y, and G464W) to rescue as isogenic rMeV. We chose the best mutant from sites I to IV as evaluated by our QIFA (Fig. 3A and SI Appendix, Fig. S6A). For site III, we chose G464W instead of N462K because N462K has already been reported (34). rMeV-IC323EGFP with the L137F, S262N, or G464W F mutations formed huge syncytia (Fig. 6A) and replicated several hundredfold better than wt, even at day 6 postrescue (Fig. 6B). rMeV with the F-H297Y mutant showed a less dramatic increase in the syncytia size at day 6 but nonetheless showed significant increase in genome copy numbers by 8 d postrescue compared to wt (Fig. 6C). To substantiate the biological relevance of our structural mapping efforts, we used a well-characterized F inhibitory peptide (FIP) that not only blocks MeV F (37) but does so specifically by interacting directly with residues in site III such as G464 (30). We found that the G464W mutant was resistant to FIP but not the other nonsite III mutants (Fig. 6 D and E). To ensure that these results were not due to differences in surface expression and/or F protein cleavage, we performed cell surface biotinylation experiments. Briefly, surface-expressing F proteins were pull downed by streptavidin beads after cell surface protein biotinylation and the immunoprecipitated cell surface MeV-F detected by Western blot using an MeV-F–specific antibody (Fig. 6F). Densitometry showed that surface F protein expression was highest in wt F and the T461I mutant, but all the hyperfusogenic mutants (L137F, S262N, G464W, and H297Y) were expressed at ∼50% of wt levels mutants (Fig. 6G). Cleavage efficiency was also evaluated by the analyzing the ratio of F1/F0 (Fig. 6H), which showed no significant differences in cleavage efficiency between wt and any of the hyperfusogenic mutants. Altogether, these results show that the hyperfusogenic phenotype was not due to overexpression or more efficient cleavage of the indicated F mutants.
Fig. 6.
Recombinant MeV expressing the hyperfusogenic F mutants from each of the four sites exhibit the expected phenotype. Recombinant MeV with wt F, T461I, and representative F mutations (L137F, S262N, G464W, and H297Y) from sites I to IV (Fig. 4) were rescued in Bsr-T7 cells. Virus growth was monitored via fluorescence microscopy. (A) At day 6 postrescue (with one passage at day 3), cytosolic RNA was collected, and genome copy number was quantified by RT-qPCR. (B) Genome copy numbers for all the mutants were normalized to that for wt MeV, which was set to 1. (B and C) Growth of H297Y mutants was further evaluated for 8 d incubation period (with one passage at day 4). (C) Data shown are mean relative genome copy numbers (± SD) from five independent experiments. (B and C) Statistically significant differences from wt were determined by Dunnet’s multiple comparison test (B) and t test (C). Syncytia images were generated by the imaging cytometer as in previous figures. (Scale Bar, 2 mm.) MeV-specific FIP inhibited the F activity of all the hyperfusogenic mutants except the G464W mutant, as evaluated by our QIFA. (D) Data shown are mean (± SD) from five independent experiments. Representative images of the F inhibitory data are shown in E. P < 0.05 or <0.01 for the indicated comparisons (Student’s t test). Images generated on the image cytometer as before. (Scale Bar, 500 μm.) (F and G) Cell surface biotinylation experiments show that the L137F, S262N, G464W, and H297Y hyperfusogenic mutants were expressed at lower levels than wt F or F-T461I. At 48 hpt, biotinylated cell surface proteins on MeV-F transfected 293T cells were pulled down by streptavidin beads and Western blotted with an MeV-F–specific antibody. Cadherin and GAPDH served as respective cell surface and cytosolic protein controls. The upper and lower blots in F show the input and surface protein (streptavidin pull-down) fraction, respectively. The full-length F0 and cleaved F1 products are marked (arrowhead). * indicates the nonspecific band from the cytosol (upper blot), which disappeared in the cell surface pull-down fraction (lower blot). G shows the relative F1 surface expression levels of the various F proteins normalized to wt F set at 1 (based on densitometric measurements). H shows the F1/F0 ratio of cell surface F, which indicates cleavage efficiency. Data shown are the average and range of two independent experiments.
A cardinal feature of SSPE MeV strains is the ability to infect and spread in primary human neurons, which do not express the canonical receptors for primary strains of MeV (CD150 and nectin-4). The wt MeV can infect neurons, albeit inefficiently, but neurovirulent SSPE/MIBE MeVstrains can infect and spread in cultured primary human neurons. To mimic primary human neuronal infection, we used human induced pluripotent stem cells (hiPSC)-derived, neurogenin 2 (NGN2)-induced glutamatergic neurons that are a well-characterized model of excitatory forebrain neurons (38). These NGN2 neurons have been extensively characterized by next-generation sequencing, and interrogation of the NGS dataset indicates that these neurons are negative for nectin-4 (39) (also available at https://schroden.shinyapps.io/BrennandLab-ExpressionApp-limited/). In addition, SI Appendix, Fig. S7 shows that the neurons used for these infection studies expressed the neuron-specific marker of β3 tubulin outlining the cell body and axon of neuron.
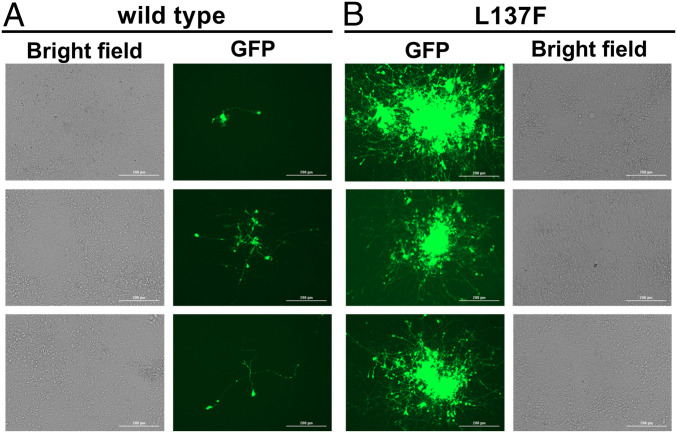
Upon wt rMeV-IC323EGFP infection, we detected a few GFP+ neurons at 2 d postinfection (dpi). GFP appeared distributed in the cell bodies as well as the dendrities and axons that outlined the neurons distinctly (Fig. 7A). On rare occasions, a small cluster of GFP+ neurons could be found connected by GFP+ neurites, which suggest a slow cell-to-cell spread of MeV (Fig. 7 A, Middle and Bottom). This is reminiscent of what was reported by Sato et al. in NT2-derived neurons (22). In contrast, inoculation of the same neuronal cultures with the rMeV-F-L137F mutant resulted in much larger clusters of GFP+ neurons that sometimes appeared to coalesce (Fig. 7 B, Top). The latter show that hyperfusogenic F mutants identified in our screen can recapitulate the SSPE phenotype involving efficient spread in human neurons.
Fig. 7.
Recombinant MeV with hyperfusogenic F-L137F mutant infects and spreads efficiently in primary human neurons. Homogenous iPSC-derived, NGN2-induced glutamatergic neurons, seeded and differentiated in 24-well plates, were infected with 5,000 PFU of wt MeV (A) or MeV-F-L137F (B) per well. (A) At 2 dpi, rare GFP+ neurons could be seen in wt MeV-infected wells. GFP was localized to the cell body as well as the axon and dendrites. Occasionally, small clusters of several neurons could be seen (Middle). (B) In contrast, MeV-F-L137F infected wells showed numerous GFP positive neurons in L clusters at 2 dpi. Three representative images from three independent infections are shown. Images were taken on the Cytation 3. (Scale Bar, 200 μm.)
Discussion
Our saturating mutagenesis screen allowed us to evaluate the fitness landscape that allowed for the selection of hyperfusogenic MeV-F mutants associated with SSPE/MIBE phenotypes, which is the ability to pair with wt MeV-RBP and form syncytia in cells lacking the canonical MeV receptors. We identified at least 15 such hyperfusogenic mutants, effectively doubling the list of known hyperfusogenic SSPE/MIBE mutants curated in the past several decades (SI Appendix, Table S4). These mutants are a community resource which can be used to shed further light on F regulatory mechanism and aid in the search for the putative neuronal receptor for MeV.
The antigenic variability of MeV is highly constrained (40). All vaccine strains are derived from genotype A, yet sera from vaccinees can neutralize the broad range of circulating genotypes. The monoserotypic nature of MeV implies the lack of antigenic drift and functional constraints on its surface envelope glycoproteins. The latter is highlighted by our previous study showing that MeV-F and RBP are completely intolerant to 15 bp (5 aa) insertions during a whole genome transposon mutagenesis screen (27). However, the unit of selection in neurovirulent MeV strains appears to be single nt mutations in MeV-F that confer the ability for neuronal spread (6, 21). This adaptation of MeV to spread within the CNS is correlated with in vitro syncytia formation and cell-to-cell spread in the absence of canonical receptors. Therefore, we prepared saturation point mutagenesis libraries of MeV-F in its genomic context and performed a reverse genetics rescue screen in a hamster-derived cell line (BSR-T7), where hyperfusogenic SSPE-like F mutants can spread and replicate but not wt MeV (SI Appendix, Fig. S1). The use of the well-characterized F-T461I SSPE mutant helped us in choosing the optimal cell line for the screen and served as a positive control for each replicate (Fig. 1) and functional validation (Fig. 3).
For saturation coverage, we prepared four separate libraries of ∼400 nt in size that altogether span the entire F gene (Fig. 2). There are biological and technical reasons for this strategy. To ascertain single mutations that can act independently in a given library, the library size is limited by the maximal Illumina read depth (2× 250 bp PE reads), which is effectively <450 bp, excluding the primer binding sites. To maximize the quality of our library and sensitivity of our screen, we also wanted the biggest difference between the average mutation rate of our libraries and the intrinsic error rate of Illumina sequencing, which we confirmed to be 0.04% in our hands (Fig. 2C and SI Appendix, Fig. S2E). Illumina’s reported error rate is between Q35 to Q40 (0.035 to 0.001%). If we had targeted the entire 1.6 kb F gene with an average of one point mutation, the average mutation rate would be 0.063%, which will be statistically indistinguishable from intrinsic Illumina error rate. However, introducing a single point mutation in ∼400 bp will result in an average mutation rate of 0.25%, which is comfortably eightfold above the background error rate. A similar strategy was also adopted by a previous influenza mutagenesis screening study (41, 42), in which the authors separated the influenza genome into 52 parts comprising of 250 bp segments.
Although some synonymous mutants appeared in our top hit list (SI Appendix, Table S2), most were on the same read of other nonsynonymous mutations that were later confirmed to be hyperfusogenic. This suggests that these synonymous mutations are passenger mutations associated with bona fide hyperfusogenic mutations. Separation of the F gene into four independent libraries thus enabled us to designate these synonymous or neutral mutations as such.
The veracity of our functional screen for hyperfuosgenic MeV-F in its genomic context is underscored by our ability to recover most of the extant hyperfusogenic F mutants that exhibit an SSPE phenotype, as long as that mutant was present in our original library. For hyperfuosgenic mutants that we did not recover, close inspection of our data (SI Appendix, Table S4) revealed that they were either not present in the original genomic mutant library [e.g., L454W (23)], present but outcompeted by a distinct mutant at the same aa residue (e.g., T461A>>T461I and G464W>>G464E), or known to be hypefusogenic only when present together (G168R, E170G, AS440P, R520C, and L550P). This lends greater support to the 16 hyperfusogenic mutants we validated from our screening experiments (library 1: Q96P, L137H, and L137F; library 2: P219T, S220I, G253E, L260S, S262N, and G264E; library 3: A284T, H297Y, T314P, L354P, and G376V; library 4: N462K and G464W). Except for the previously characterized N462K mutant, others were all novel mutants.
L137 mutants are particularly interesting. L137 is located in the C terminus of F peptide and is highly conserved among all paramyxoviruses. The homologous L134F mutation in the NiV-F protein also made NiV-F hyperfusogenic in the presence of NiV-RBP (Fig. 4 C and D). How far this extends to other paramyxoviruses is a subject for future studies.
In addition to validating their phenotype in our F assays, we rescued four mutants (one from each library) as independent rMeV clones and showed that they exhibited the expected hyperfusogenic SSPE phenotype (Fig. 6). These data indicate our saturation mutagenesis screening system is robust and efficiently identifies mutants dictated by the screening conditions, even if we were not able to retrieve all of previously reported hyperfusogenic mutants (SI Appendix, Table S4). This system can also be applied to genes of interest in other paramyxoviruses to find interferon vulnerable mutations for better vaccine development as was done for influenza (41).
We used BSR-T7 cells as a screening cell line, partly because this cell line allows efficient paramyxovirus rescue. In addition, this cell line doesn’t allow wt MeV growth or syncytia formation, which is convenient for the selection of hyperfusogenic mutants. It might be worth trying screening in human CNS cell lines to get a different fitness profile in the future study.
A majority of the previously reported hyperfusogenic mutations (SI Appendix, Table S4) are located on site III (part of library 3 and library 4 in our study) in the prefusion structure of trimeric MeV-F (Fig. 5 and SI Appendix, Table S4), which might have overemphasized the contribution of this site (base of the head domain) to the neurovirulent hyperfusogenic phenotype. However, our screening found many strong phenotypic mutations in site 1 and site 2, suggesting that mutations in all sites found across all three structural domains of F can contribute to the hyperfusogenic phenotype. In addition, we found mutants—A284T and H297Y—which are located in the beta sheet (Y277-G301) that connect the head and neck domains (Fig. 5E). These two mutants in this structurally distinct site IV do not appear to have as strong a phenotype but are nonetheless real, as rMeV-F-H297Y can grow and replicate in BSR-T7 cells.
As expected from crystal structure, G464W may resist FIP inhibition because G464 directly interacts with FIP in the complex crystal structure (30). Our data showed that G464W was indeed resistant to FIP inhibition (Fig. 6E) just as G464E was also reported as an FIP-resistant hyperfusogenic mutation (43). These observations suggest that our screen can be judiciously applied to study the barriers to drug or antibody resistance. However, FIP resistance and hyperfusogenicity are not always linked. They can be independent phenotypes. Ha et al. identified FIP escape mutants in which some mutants showed FIP resistance and hyperfusogenicity (e.g., N462K), and some mutants showed only FIP resistance without hyperfusogenicity (e.g., D458N) (43). The difference in the destabilization of F protein, which is suggested by Watanabe et al. (26), and mutations that change the binding interface for FIP without destabilizing F may be responsible for the discrepancy of profile.
We note that the representative hyperfusogenic mutants rescued as point mutants in rMeV-F (L137F, S262N, G464W, and H297Y) were all expressed at the cell surface ∼50% of wt or lower, whereas total production seems similar (Fig. 6F). Although low cell surface expression is not an intrinsic quality of hyperfusogenic proteins (T461I is expressed similarly to wt), the lower stability of hyperfusogenic F proteins at the cell surface or decreased transportation to cell surface are potential issues that can be examined in future studies.
Finally, we acknowledge that while mutations that alter the lengths of the F cytoplasmic tail is common among most SSPE-derived virus sequences (18, 44), our screen was not designed to identify such alterations in cytoplasmic tail lengths. Truncations in the cytoplasmic tail of wt MeV-F (IC-B) alone do not confer a hyperfusogenic phenotype in SLAMF1 or nectin-4 negative cells, whereas single point mutations derived from either SSPE or MIBE strains do (21, 31). Recombinant MeV with F proteins possessing such an in vitro hyperfusogenic phenotype also exhibit lethal neuropathogenicity in suckling hamsters (21), which underscores the relevance of our screen to identify hyperfusogenic F associated with neurovirulent phenotypes.
Our reverse genetics rescue screen based on a particular phenotype is made possible by the transformative improvements in the efficiency of paramyxovirus rescue. This can now be applied to any gene in any paramyxoviruses for which rescue efficiency is high enough.
Materials and Methods
Cell Lines.
The 293T cells (American Type Culture Collection [ATCC]), Vero cells (CCL-81; ATCC), and BSR-T7 cells (45) were propagated in Dulbecco’s modified Eagle’s medium (DMEM) (Invitrogen) supplemented with 10% fetal bovine serum (Atlanta Biologicals) at 37 °C. Vero cells constitutively expressing human SLAM (Vero-hSLAM cells) were gifted from Dr. Yusuke Yanagi (Kyushu University, Fukuoka, Japan) (46).
Plasmids and Viruses.
We modified the genome coding plasmid for MeV (p[+] MV323-AcGFP) (47) and generated pEMC-MV323-EGFP by moving the AcGFP gene to the 3′ terminus of the genome as shown in Fig. 2B. The cognate hammerhead ribozyme was added, and rescue of rMeV was performed as described (33). Briefly, 4 × 105 BSR-T7 cells were seeded in 6-well plates. The next day, the indicated rMeVs were rescued by our five-plasmid transfection protocol [comprising the cognate MeV T7-driven antigenomic clone; T7-driven MeV-N, -P, and -L; and codon-optimized T7-polymerase (T7opt, Addgene) (33)]. Transfected cells were incubated at 37 °C with medium replacement every day. Replication kinetics and passaging conditions are detailed below. The full length viral genomic plasmid was maintained in Stbl2 Escherichia coli (Thermo Fisher Scientific) with growth at 30 °C.
MeV RBP and F genes were amplified from p(+) MV323-AcGFP and cloned into pCDNA3 or pCAGGS vector, creating pCDNA3-MV-F, pCAGGS-MV-RBP, and pCAGGS-MV-F. We introduced mutations or modified the plasmids using error-prone PCR or site-directed mutagenesis, respectively. We used In-Fusion (Clontech) cloning to shuttle the mutated PCR fragments into our pEMC-MV323-EGFP backbone. Primer sets used for making each mutant are listed in SI Appendix, Table S5.
Error-Prone PCR-Based Mutagenesis.
We used error-prone PCR to introduce point mutations in the F gene according to manufacturer’s protocol (Genemorph II random mutagenesis kit, Agilent). We generated four libraries (402 to 418 bp in size) that covered the entire F gene (Fig. 1A). We built each library into a shuttle plasmid as shown in Fig. 2B using NEBuilder (New England Biolabs [NEB]). Each shuttle plasmid library was transformed into Stellar competent cells (Clontech) and >20,000 colonies were generated for each library. Bacterial colonies were collected 24 h after plating, amplified in Terrific Broth (Research Products International), and plasmid DNA purified by Plasmid DNA Maxi Prep Kits (Thermo Fisher Scientific). Next, the pCDNA3-MV323-F mutated libraries was inserted into the pEMC-MV323-EGFP genomic backbone by compatible ends (Nru I-HF and Pac I) ligation cloning (T4 DNA ligase, NEB), followed by transformation into electrocompetent cells with ElectroMAX stbl4 (Thermo Fisher Scientific), securing >20,000 colonies in each library. Genomic libraries were prepared the same as for the shuttle plasmid libraries above.
Growth Comparisons between wt and Hyperfusogenic rMeVs.
The wt or F-T461I rMeVs were rescued by transfection of one well (6-well plate) of BSR-T7 cells, then cells were grown with medium replacement every day. At day 4, BSR-T7 cells were trypsinized, and one out of six cells were passed into a new well (6-well plate) then grown for an additional 4 d. The number of GFP positive cells was counted at day 2, day 4, and day 8 by Celigo Imaging Cytometer (Nexcelom). Supernatant was collected for titration at day 4 and day 8. For rMeV-F L137F, S262N, and G464W, we passaged the cells at day 3 and counted the cells at day 6 because extensive syncytia detached by day 8.
Quantification of Viral Titers by Plaque Assay.
Measuring viral titers in supernatants were done on Vero-hSLAM cells. Briefly, we infected confluent Vero-hSLAM cells (12-well plate format) with 500 μL of serially diluted viral supernatant for 1 h, followed by medium replacement with 1% methylcellulose containing DMEM. About 4 d later, the number of GFP+ plaques were counted by fluorescence microscopy.
Passaging Virus in the Screening Experiment.
Genomic F mutant libraries were rescued in BSR-T7 cells as for wt rMeV described above. For each library, at day 4, BSR-T7 cells in one well of 6-well plate were trypsinized and spilt into 6 wells of a 6-well plate. Then BSR-T7 cells with rMeVs were grown for an additional 4 d (total 8 d). Cytosolic RNA was extracted, reverse transcribed, amplified, and subjected to 2 × 250 bp Illumina-based amplicon sequencing.
RT-PCR and Illumina Sequencing.
Cytosolic RNA was extracted with TRIzol (Thermo Fisher Scientific). The entire F gene (∼1.7 kb) was first amplified by RT-PCR (Superscript III, Thermo Fisher Scientific). The RT-PCR fragments were then used as a template for nested PCR (CloneAmp HiFi PCR) to amplify the sequence of the cognate mutant library (402 to 418 bp, excluding primer sequence). Primers used are indicated in SI Appendix, Table S5.
DNA library preparations, sequencing reactions, and initial bioinformatics analysis were conducted at GENEWIZ, Inc. DNA library preparation was performed using NEBNext Ultra DNA Library Prep kit following the manufacturer’s recommendations (Illumina). End-repaired adapters were ligated after adenylation of the 3′ends. The pooled DNA libraries were sequenced by MiSeq on a 2 × 250 PE configuration. Base calling was conducted by the Illumina Control Software (HiSeq Control Software) on the Illumina instrument.
Data Analysis and Selection of the Top Hit List.
PE Fastq files were merged by BBtools to make single read. We trimmed low-quality nts by PRINSEQ because the 5′ and 3′ ends of sequences tend to show lower quality (48). We trimmed nts until PRINSEQ found the first nt of quality value (Q) ≥33, and then we selected the read with the average Q33.
Wiggle file (include nt counts at each position) were generated from processed SAM and BAM files with Integrative Genomics Viewer tools. Mutation rates were calculated from nt counts at each position using reference sequence file.
Genome Quantification by qPCR.
Extracted RNA was reverse transcribed by genome-specific primer (SI Appendix, Table S5) with Tetro Reverse Transcriptase (Bioline), then the number of genomes was quantified by SensiFAST SYBR & Fluorescein Kit (Bioline) and CFX96 Touch Real-Time PCR Detection System (Biorad).
QIFA.
The rationale, validation, and performance characteristics of our image-based F assay are detailed in SI Appendix, Supplementary Methods.
FIP.
FIP (Z-d-Phe-Phe-Gly-OH) was purchased from BACHEM (#4015768). FIP was dissolved into 10 mM solution by DMSO. FIP solution was added to the medium at the final concentration of 2% (200 μM) at 3 h posttransfection. DMSO was used as a negative control of FIP.
Cell Surface Expression Analysis of F Protein.
Cell surface biotinylation was used to check for proper expression and processing of hyperfusogenic F proteins. Details are provided in SI Appendix, Supplementary Methods.
Neuron Infection Experiment.
Human NGN2-induced glutamatergic neurons were generated from hiPSCs as previously described (38). Details are given in SI Appendix, Supplementary Methods.
A total of 5 × 103 PFU/well (tittered in Vero-hSLAM cells) of wt MeV and MeV-F L137F were used to infect hiPSC-derived neurons for 1 h, after which the virus-containing media was removed and replaced by fresh neuronal growth media. Cells were incubated for 2 d then fixed by 2% PFA at 2 dpi. Infected cells were visualized by Cytation 3 (Biotek).
Immunofluorescence Staining.
Human NGN2-induced glutamatergic neurons were fixed with 4% PFA and blocked by 2% BSA in phosphate-buffered saline, followed by primary and secondary antibody reaction. Mouse monoclonal anti-β3 tubulin antibody (clone TUJ1, Stemcell Technologies) was chosen as primary antibody, and goat anti-mouse IgG conjugated with Alexa 488 (Thermo Fisher Scientific) was chosen as secondary antibody. Nucleus were stained by Hoechst. Images were visualized by Cytation 3 (Biotek).
Ethics Declaration.
Our study with regards to the use of the hiPSC cells was approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai. In addition, all hiPSC research was conducted with approval from the Embryonic Stem Cell Research Overview committee at the Icahn School of Medicine at Mount Sinai. Informed consent was obtained from all skin cell donors as part of a study directed by Judith Rapoport, MD at the National Institute of Mental Health.
Supplementary Material
Acknowledgments
This work was supported by the Japan Agency for Medical Research and Development (AMED) Grant 20wm0325002h (to T.H.), the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant Number 20H03497 (to T.H.), and the Joint Usage/Research Center program of Institute for Frontier Life and Medical Sciences, Kyoto University. S.I. and C.-T.H. were supported by Fukuoka University’s Clinical Hematology and Oncology Study Group Fellowship and a postdoctoral fellowship from the Ministry of Science and Technology (Taipei, Taiwan), respectively. This study was supported in part by NIH Grants AI115226 and AI123449 to B.L.
Footnotes
The authors declare no competing interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2026027118/-/DCSupplemental.
Data Availability
The raw NGS results are uploaded at National Center for Biotechnology Information Gene Expression Omnibus: GSE14767. All other study data are included in the article and/or SI Appendix.
References
- 1.Amarasinghe G. K., et al., Taxonomy of the order Mononegavirales: Update 2017. Arch. Virol. 162, 2493–2504 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel M. K., et al., Progress toward regional measles elimination - Worldwide, 2000-2019. MMWR Morb. Mortal. Wkly. Rep. 69, 1700–1705 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mina M. J., et al., Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Science 366, 599–606 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mina M., et al., Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Science 348, 694–699 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petrova V. N., et al., Incomplete genetic reconstitution of B cell pools contributes to prolonged immunosuppression after measles. Sci. Immunol. 4, eaay6125 (2019). [DOI] [PubMed] [Google Scholar]
- 6.Watanabe S., Shirogane Y., Sato Y., Hashiguchi T., Yanagi Y., New insights into measles virus brain infections. Trends Microbiol. 27, 164–175 (2019). [DOI] [PubMed] [Google Scholar]
- 7.Ludlow M., McQuaid S., Milner D., de Swart R. L., Duprex W. P., Pathological consequences of systemic measles virus infection. J. Pathol. 235, 253–265 (2015). [DOI] [PubMed] [Google Scholar]
- 8.Bellini W. J., et al., Subacute sclerosing panencephalitis: More cases of this fatal disease are prevented by measles immunization than was previously recognized. J. Infect. Dis. 192, 1686–1693 (2005). [DOI] [PubMed] [Google Scholar]
- 9.Schönberger K., Ludwig M. S., Wildner M., Weissbrich B., Epidemiology of subacute sclerosing panencephalitis (SSPE) in Germany from 2003 to 2009: A risk estimation. PLoS One 8, e68909 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plemper R. K., Lamb R. A., “Paramyxoviridae: The viruses and their replication” in Fields Virology: Emerging Viruses, Howley P. M., Knipe D. M., Eds. (Wolters Kluwer, 2020), pp. 504–558. [Google Scholar]
- 11.Jardetzky T. S., Lamb R. A., Activation of paramyxovirus membrane fusion and virus entry. Curr. Opin. Virol. 5, 24–33 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plattet P., Alves L., Herren M., Aguilar H. C., Measles virus fusion protein: Structure, function and inhibition. Viruses 8, 112 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rota P. A., et al., Measles. Nat. Rev. Dis. Prim. 2, 16049 (2016). [DOI] [PubMed] [Google Scholar]
- 14.Mateo M., Navaratnarajah C. K., Cattaneo R., Structural basis of efficient contagion: Measles variations on a theme by parainfluenza viruses. Curr. Opin. Virol. 5, 16–23 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin L.-T., Richardson C. D., The host cell receptors for measles virus and their interaction with the viral hemagglutinin (H) protein. Viruses 8, 250 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cattaneo R., et al., Biased hypermutation and other genetic changes in defective measles viruses in human brain infections. Cell 55, 255–265 (1988). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ning X., et al., Alterations and diversity in the cytoplasmic tail of the fusion protein of subacute sclerosing panencephalitis virus strains isolated in Osaka, Japan. Virus Res. 86, 123–131 (2002). [DOI] [PubMed] [Google Scholar]
- 18.Schmid A., et al., Subacute sclerosing panencephalitis is typically characterized by alterations in the fusion protein cytoplasmic domain of the persisting measles virus. Virology 188, 910–915 (1992). [DOI] [PubMed] [Google Scholar]
- 19.Cathomen T., et al., A matrix-less measles virus is infectious and elicits extensive cell fusion: Consequences for propagation in the brain. EMBO J. 17, 3899–3908 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patterson J. B., et al., Evidence that the hypermutated M protein of a subacute sclerosing panencephalitis measles virus actively contributes to the chronic progressive CNS disease. Virology 291, 215–225 (2001). [DOI] [PubMed] [Google Scholar]
- 21.Watanabe S., et al., Mutant fusion proteins with enhanced fusion activity promote measles virus spread in human neuronal cells and brains of suckling hamsters. J. Virol. 87, 2648–2659 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sato Y., et al., Cell-to-cell measles virus spread between human neurons is dependent on hemagglutinin and hyperfusogenic fusion protein. J. Virol. 92, e02166–e02217 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jurgens E. M., et al., Measles fusion machinery is dysregulated in neuropathogenic variants. MBio 6, 1–12 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Makhortova N. R., et al., Neurokinin-1 enables measles virus trans-synaptic spread in neurons. Virology 362, 235–244 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Generous A. R., et al., Trans-endocytosis elicited by nectins transfers cytoplasmic cargo, including infectious material, between cells. J. Cell Sci. 132, jcs235507 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watanabe S., et al., Measles virus mutants possessing the fusion protein with enhanced fusion activity spread effectively in neuronal cells, but not in other cells, without causing strong cytopathology. J. Virol. 89, 2710–2717 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fulton B. O., et al., Mutational analysis of measles virus suggests constraints on antigenic variation of the glycoproteins. Cell Rep. 11, 1331–1338 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rota J. S., Hummel K. B., Rota P. A., Bellini W. J., Genetic variability of the glycoprotein genes of current wild-type measles isolates. Virology 188, 135–142 (1992). [DOI] [PubMed] [Google Scholar]
- 29.Angius F., et al., Analysis of a subacute sclerosing panencephalitis genotype B3 virus from the 2009-2010 South African measles epidemic shows that hyperfusogenic F proteins contribute to measles virus infection in the brain. J. Virol. 93, e01700–e01718 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hashiguchi T., et al., Structures of the prefusion form of measles virus fusion protein in complex with inhibitors. Proc. Natl. Acad. Sci. U.S.A. 115, 2496–2501 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ayata M., et al., The F gene of the Osaka-2 strain of measles virus derived from a case of subacute sclerosing panencephalitis is a major determinant of neurovirulence. J. Virol. 84, 11189–11199 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sugiyama T., et al., Measles virus selectively blind to signaling lymphocyte activation molecule as a novel oncolytic virus for breast cancer treatment. Gene Ther. 20, 338–347 (2013). [DOI] [PubMed] [Google Scholar]
- 33.Beaty S. M., et al., Efficient and robust Paramyxoviridae reverse genetics systems. mSphere 2, e00376–e00416 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doyle J., et al., Two domains that control prefusion stability and transport competence of the measles virus fusion protein. J. Virol. 80, 1524–1536 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Azarm K. D., Lee B., Differential features of fusion activation within the paramyxoviridae. Viruses 12, 161 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dawes B. E., Freiberg A. N., Henipavirus infection of the central nervous system. Pathog. Dis. 77, ftz023 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richardson C. D., Scheid A., Choppin P. W., Specific inhibition of paramyxovirus and myxovirus replication by oligopeptides with amino acid sequences similar to those at the N-termini of the F1 or HA2 viral polypeptides. Virology 105, 205–222 (1980). [DOI] [PubMed] [Google Scholar]
- 38.Ho S.-M., et al., Rapid Ngn2-induction of excitatory neurons from hiPSC-derived neural progenitor cells. Methods 101, 113–124 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schrode N., et al., Synergistic effects of common schizophrenia risk variants. Nat. Genet. 51, 1475–1485 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beaty S. M., Lee B., Constraints on the genetic and antigenic variability of measles virus. Viruses 8, 109 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Du Y., et al., Genome-wide identification of interferon-sensitive mutations enables influenza vaccine design. Science 359, 290–296 (2018). [DOI] [PubMed] [Google Scholar]
- 42.Ye J., et al., Error-prone pcr-based mutagenesis strategy for rapidly generating high-yield influenza vaccine candidates. Virology 482, 234–243 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ha M. N., et al., Mutations in the fusion protein of measles virus that confer resistance to the membrane fusion inhibitors carbobenzoxy-d-Phe-l-Phe-Gly and 4-nitro-2-phenylacetyl amino-benzamide. J. Virol. 91, e01026–e01117 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cathomen T., Naim H. Y., Cattaneo R., Measles viruses with altered envelope protein cytoplasmic tails gain cell fusion competence. J. Virol. 72, 1224–1234 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Buchholz U. J., Finke S., Conzelmann K. K., Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J. Virol. 73, 251–259 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ono N., et al., Measles viruses on throat swabs from measles patients use signaling lymphocytic activation molecule (CDw150) but not CD46 as a cellular receptor. J. Virol. 75, 4399–4401 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Seki F., et al., The SI strain of measles virus derived from a patient with subacute sclerosing panencephalitis possesses typical genome alterations and unique amino acid changes that modulate receptor specificity and reduce membrane fusion activity. J. Virol. 85, 11871–11882 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ma X., et al., Analysis of error profiles in deep next-generation sequencing data. Genome Biol. 20, 50 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen L., et al., The structure of the fusion glycoprotein of Newcastle disease virus suggests a novel paradigm for the molecular mechanism of membrane fusion. Structure 9, 255–266 (2001). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw NGS results are uploaded at National Center for Biotechnology Information Gene Expression Omnibus: GSE14767. All other study data are included in the article and/or SI Appendix.