Abstract
The pandemic of SARS-CoV-2 stimulates significant efforts and approaches to understand its global spread. Although the recent introduction of the vaccine is a crucial prophylactic step, the effective treatment for SARS-CoV-2 is still undiscovered. An in-depth analysis of symptoms and clinical parameters, as well as molecular changes, is necessary to comprehend COVID-19 and propose a remedy for affected people to fight that disease.
The analysis of available clinical data and SARS-CoV-2 infection markers underlined the main pathogenic process in COVID-19 is cytokine storm and inflammation. That led us to suggest that the most important pathogenic feature of SARS-CoV-2 leading to COVID-19 is oxidative stress and cellular damage stimulated by iron, a source of Fenton reaction and its product hydroxyl radical (•OH), the most reactive ROS with t1/2–10−9s. Therefore we suggest some scavenging agents are a reasonable choice for overcoming its toxic effect and can be regarded as a treatment for the disease on the molecular level.
Keywords: SARS-CoV-2, COVID-19, Inflammation, Iron, Fenton reaction, Epigenetics, DNA methylation, Oxidative stress, ROS, 8-Oxo-guanosine, Lycopene
1. Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) is responsible for developing coronavirus disease 19 (COVID-19). COVID-19 is an infective-inflammatory disease and has so far affected more than 45 million people and killed more than 1.2 million people worldwide, with most deaths (74%) occurring in the population over the age of 65 [1].
SARS-CoV-2 is an RNA virus of ca. 30 000 nucleoside genome length. It shows a low substitution per site in the range of 1.5–10−4. Sequence substitutions are characterized by a preponderance of cytosine to uracil transitions, which can be ascribed to pyrimidine deamination. The excess of U over C is almost 2-fold, giving 32% of uracil and 18% of cytosine. SARS-CoV-2 shows some interesting features, e.g., all over-represented codons end with A/U, and low codon usage bias, which is an effect of mutational pressure and natural selection. Nucleotide composition analysis revealed that SARS-CoV-2 Wuhan-Hu-1 strain has the highest compositional value of uridine (32.2%), which was followed by adenosine (29.9%), and similar composition of guanosine (19.6%) and cytidine (18.3%) [2].
SARS-CoV-2 is transmitted through respiratory droplets or by direct contact. The virus enters through the nose, mouth or eyes, and then spreads to the back of the nasal passages. It binds to and enters the airway epithelial cells via the dimerized angiotensin-converting enzyme 2 (ACE2) on the surface. From there, it spreads to the mucous membranes of the throat and bronchial tubes, eventually entering the lungs, where it infects type 2 alveolar epithelial cells called pneumocytes [3].
Recently it has been shown that to infect cells, in addition to ACE2, SARS-CoV-2 uses another receptor called neuropilin-1 (NRP1) (Fig. 1 ). Because ACE2 is expressed at a very low level in most cells, some entry cofactors on the surface of host cells are necessary. Such function is played by neuropilin-1, which binds furin-cleaved substrates, facilitates SARS-CoV-2 entry and infections [5,7].
Fig. 1.
The scheme of SARS-CoV-2 entry to the cell with indicated possible ways of prevention with natural products. The virus invades the cell through binding of its spike protein the cell's angiotensin converting enzyme 2 receptor. Spike protein, after cleavage by host proteases, binds to cell surface receptor - neuropilin-1. Moreover, S1 domain of SARS-CoV-2 spike glycoprotein interacts with human CD26, for the viral entry into the host cell. CD26 is expressed on the membrane of many cells, including T and NK cells of the immune system, as well as is present in the blood plasma and cerebrospinal fluid in a soluble form [[4], [5], [6]].
Severe acute respiratory distress syndrome (ARDS) is characterized by a loss of beneficial lung surfactant and increased oxidative stress and inflammation [8]. The severity and outcome of COVID-19 largely depend on a patient's age, but not only. In severe cases of COVID-19, the virus enters the bloodstream and infects kidneys, esophagus, bladder, ileum, heart, and central nervous system (CNS). Extra-pulmonary manifestations of COVID-19 are associated with a much higher mortality rate [9].
2. COVID-19 symptomatology
The common clinical symptoms of COVID-19 are fever and cough, sputum production, sore throat, headache, myalgia, arthralgia, rhinorrhoea, and diarrhea [10]. In laboratory tests, COVID-19 patients present with cytokine storm and high systemic inflammatory parameters as elevated C-reactive protein, ferritin, bradykinin, increased white blood cell counts, and lymphopenia. Inflammation and immunosenescence contribute to the development of cytokine storm. Tightly controlled activation of the innate immune system is essential for viral recognition and clearance. Cytokine storm results from the sustained activation of the inflammatory signaling cascade, which results in hypercoagulation in small blood vessels, leading to tissue damage and multi-organ failure [10,11]. D-dimer, a fibrin degradation product, as well as prognostic of disseminated intravascular coagulation, and elevated levels of the cytokine IL-6, are associated with the increased clinical fatality of the disease [12]. During viral infections and inflammation, anemia, caused by pro-inflammatory cytokines, is frequently observed. Some of them, like IL-1β, TNF-α, and IL-6, directly affect iron homeostasis [13]. The release of cytokines, particularly IL-6, results in the upregulation of the iron regulatory hormone hepcidin produced by hepatocytes and released in the blood flow to regulate systemic iron homeostasis [14,15].
On the contrary, there are also data showing that, compared to other inflammatory diseases and sepsis, the levels of cytokines in severely ill COVID-19 patients are low, and the virus does not cause cytokine storm in those cases. That can suggest other factors have to be considered to explain the virus's impact on organ dysfunction [16].
A high reactivation of the immune system affected by SARS-CoV-2 induces a surge of pro-inflammatory factors resulting in host cells and organ damage through hypercoagulability, oxidative stress, and altered iron metabolism [17]. Coagulopathy increases morbidity and mortality of patients with COVID-19. They show low hemoglobin levels and increased total bilirubin, as well as ferritin. The level of this protein is an indirect marker of the total amount of iron in the body [14]. In addition to ferritin, other serum biomarkers as D-dimer, CRP, IL-6, and lactate dehydrogenase have been suggested to identify high-risk COVID-19 patients [18].
3. Iron and ferritin
An increased ferritin level induces immunological dysregulation and contributes to the cytokine storm, increasing the severity of COVID-19. Immune dysregulation is observed in extreme hyperferritinemia through immune-suppressive and pro-inflammatory effects. High serum ferritin is due to the dissociation of iron from the 1 beta chain of hemoglobin. Viral ORF8 binds to the porphyrin of heme and displaces iron [19,20]. Hemoglobinopathy and iron dysmetabolism seriously compromise erythrocytes’ capacity to perform oxygen transport [13].
Iron is a crucial element in all organisms. It has unique properties due to its redox potential, which makes it an essential cofactor for several proteins and enzymes involved in critical cellular functions like energy production, DNA replication, and transcription. Also, most viruses need iron since they require the host metabolic apparatus to replicate their genome and produce mRNAs to translate functional viral proteins [17,21,22]. It is evident that cellular iron repletion boosts viral replication and spread, but iron deficiency may interfere with a viral life cycle.
Ferritin is the main iron storage site in its ferric state (Fe+3) and binds 4500 iron molecules. An increased serum ferritin level is associated with systemic inflammation. Many data show that high serum ferritin levels accompany many diseases like acute respiratory distress syndrome, atherosclerosis, or cancer. Serum ferritin leaks from damaged cells and is losing most of its iron on the way. Leaving that iron in an unligated form stimulates further oxidative cell damage [23]. The iron-induced hydroxyl radical formation leads to oxidative damage, which is likely to be a contributory factor in many if not all diseases. Therefore one can suggest that hyperferritinemia is associated with a state of iron toxicity resulting from damaged tissue releasing free iron [13].
4. Reactive oxygen species (ROS)
Oxidative stress is accompanied by cytokine storm leading to ROS-dependent apoptosis of endothelial cells and the release of coagulation factors and clot formation [24]. Excess of intracellular ferric (Fe+3) ion (unligated) interacts with molecular oxygen generating ferrous (Fe+2) ion, which further down reacts with hydrogen peroxide (H2O2) producing extremely reactive hydroxyl radical •OH in the Fenton reaction [22,25]. The Fenton reaction is the most common source of •OH in the cell [26]. Reactive oxygen species derived from molecular oxygen show highly reactive superoxide radical (O2 −), hydroxyl radical (•OH), and also nonradical hydrogen peroxide (H2O2). Among ROS, H2O2 is of particular interest because it is relatively stable and can diffuse freely through the cellular membranes. It can generate the hydroxyl radicals locally by an iron-mediated Fenton reaction. ROS play a critical role in several physiological functions like proliferation and signaling pathways. In cellular (redox) systems, ROS level is tightly regulated to avoid excessive damage to cellular macromolecules. An imbalance of redox equilibrium leads to persistent oxidative stress favouring senescence, inflammation, and carcinogenesis. Reactive oxygen species cause a release of iron from storage in ferritin as well as damaging DNA, lipids, and proteins [Edeas et al., 2020]. Cellular damage involves reduced redox-active metal ions (ferrous and cuprous) that react with metabolically produced hydrogen peroxide H2O2. Hydroxyl radical (•OH) formed in the Fenton reaction is the site-specific product because of metal ions close to or bound to DNA [27].
Oxidative stress during viral infection involves multiple interactions between host and virus [22,28]. The activated phagocytes may also release pro-oxidant cytokines such as tumor necrosis factor and interleukin-1 [29]. The organism infected with various viruses (e.g. HIV, hepatitis, influenza and SARS-CoV-2) activates the phagocytes, associated with ROS production.
During SARS-CoV-2 infection, the interaction with iron metabolism and oxygen supply is also linked to the Fenton reaction, like other viruses [28]. SARS-CoV-2 induces hemoglobin degradation and iron (Fe+2) release, a cofactor of Fenton reaction in which hydroxyl radical (•OH), the most reactive oxygen species, is produced [22].
One should also mention that hydroxyl radical formation correlates with products of cellular oxidative stress such as 8-hydroxydeoxyguanosine in DNA as well as 4-hydroxynonenal and malondialdehyde guanine adducts of DNA [23,30,31]. These last two aldehydes are the products of radical oxidation of phospholipids, related to COVID-19 dyslipidemia [30].
8-hydroxyguanosine (8-OH-G), a primary oxidized base lesion formed by ROS, particularly •OH, induces G to T transversion mutations that lead to cell death in mammals if it accumulates in DNA [32].
5. Epigenetics of brain diseases
Epigenetics is defined as heritable changes in gene expression associated with modifications of DNA (methylation) or chromatin proteins (methylation and acetylation) that are not due to any alteration in the DNA nucleotide sequence [33]. DNA methylation is a significant control program that modulates gene expression in a plethora of organisms.
The excess of ROS triggers epigenetic machinery in the cell by damaging 5-methylcytosine, which results in total DNA (genome) hypomethylation. The lowering/decreasing of 5-methylcytosine contents is the origin of many pathologies, like cancer and cardiovascular diseases [[34], [35], [36], [37], [38]]. Global DNA hypomethylation is also observed during cellular senescence [39]. Aging and age-related diseases include defined changes in 5-methylcytosine content are generally characterized by genome-wide hypomethylation and promoter-specific hypermethylation [40]. The relation of the 8-OH-G contents showed a clear increase with subjects of older age [41]. The clear link between increased oxidative stress, monitored by 8-OH-G, and total DNA demethylation, provides background on oxidative 5-methylcytosine degradation, not necessarily the enzymatic one (Fig. 2 ) [37].
Fig. 2.
DNA is one of the main cellular targets to be damaged through reactive oxygen species. Hydroxyl radical (•OH), that arises in Fenton reaction, is the most reactive ROS and modify guanosine in DNA to 8-OH-Gua, which is a marker of oxidative damage as well as a hot spot for mutations. m5C, the epigenetic element of DNA, can be also oxidized forming 5-hydroxymethylcytosine [37].
Epigenetic dysregulation, immune defects, advanced biological age, and other factors increase the risk of cytokine storm and COVID-19 fatality. Epigenetic dysregulation of the immune system and of the renin-angiotensin system may increase fatality risk. A variety of biological clocks has been shown to predict human health and longevity more accurately than chronological age. An individual with a biological age more advanced than their chronological one is thought to be undergoing accelerated aging, which may increase the risk of COVID-19. Individuals with comorbidities such as cardiovascular disease, diabetes, obesity, and COPD, are at greater risk for COVID-19 fatality [1].
Testing COVID-19 patients for total DNA methylation and 8-oxo-guanosine contents, which is the marker of oxidative DNA damage, could be a step initial for follow-up MRI scans combined with a neurological examination. That suggests the epigenetic route of SARS-CoV2 infection in the central nervous system as the background for further and delayed pathologies. The brain is especially susceptible to the damaging effects of ROS because of its high metabolic activity, oxygen consumption, and low capacity for cellular regeneration [29]. The central nervous system is highly vulnerable to oxidative stress due to several factors such as great energy demand and mitochondrial activity, restricted cell renewal, and a large quantity of iron and polyunsaturated fatty acids. These features increase CNS susceptibility for typical neurodegenerative hallmarks linked with oxidative stress such as impaired mitochondrial function, increased oxidative damage, defect in ubiquitin-proteasome system, changes in iron metabolism, presence of abnormal, aggregated proteins, inflammation, and cytotoxicity. It has been shown that ROS may play an important role not only in physiological senescence but also in the development of neurodegenerative diseases [42,43]. A various degree of DNA hypomethylation in four major neurodegenerative diseases: Alzheimer's disease, Parkinson's disease, Huntington's disease, and amyotrophic lateral sclerosis has been already observed [[42], [43], [44]]. Oxidative stress is heavily involved in several multiple sclerosis pathological hallmarks such as myelin destruction, axonal degeneration, and inflammation [45].
The SARS-CoV-2 infection showed a strong influence on the central nervous system. Many data have already been collected presenting its acute manifestations in the brain. However, chronic consequences are still unknown. Because brain is the top receiver of blood per cardiac output, and therefore especially prone to redox imbalance. The already detected MRI changes in COVID-19 patients include FLAIR intensity disturbances, typically found in brain tumors, neurodegenerative disorders, and neuroinflammation [46,47]. The most common were cortical FLAIR signal abnormalities, as well as white matter hyperintense lesions on FLAIR and diffusion with variable enhancement, associated with hemorrhagic lesions, and extensive and isolated white matter microhemorrhages [48,49]. FLAIR hyperintensity is not very specific and can appear in various CNS disorders, like demyelination, neurodegeneration, inflammation, and neoplasms, as well as being a sign of ischemic events [43,46]. Hyperintense white matter lesions on T2/FLAIR brain MRI are prevalent findings in elderly cohorts, and their prevalence increases from 15% at the age of 60–80% at the age of 80 [47].
6. Anti-oxidative therapeutics in COVID-19
Currently, there are no drugs approved for efficient treatment of COVID-19. Many supporting therapies were implemented because of the pandemic, like remdesivir and ivermectin, which reduce viral RNA activity. Several drugs are under investigation, and some of them are thought to restrict SARS-Co-2 entry into the cytoplasm. For example, nafamostat mesylate, inhibits coronavirus entrance into human epithelial cells (EC50 10 mM), as well as hypercoagulopathy [50]. There are also drugs that were shown to improve COVID-19 clinical symptoms, like convalescent plasma, corticosteroids, favipiravir, ribavirin, galidesivir, sofosbuvir, hydroxychloroquine (HCQ), azithromycin, doxycycline, lopinavir, heparin, tissue plasminogen activator, stilbene, ebelsen, metformin, tocilizumab, aculizumab, interferon β and γ, interleukinin 1 inhibitors, mesenchymal stem cells, nitric oxide, cannabidiol, N-acetylcysteine, calcifediol, vitamin C and D [14,[51], [52], [53], [54], [55], [56], [57], [58], [59], [60]]. Up to now, the most promising one is remdesivir, which is approved for emergency use by FDA [92], but the clinical trials are ongoing [60,61].
It is obvious that new specific therapies against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are urgently required. Because there is no specific therapy against SARS-CoV-2 infection, some drugs have been repurposed. The anti-malarial drugs chloroquine (CQ) and the less toxic hydroxychloroquine, used to treat autoimmune diseases for their immunomodulatory and anti-thrombotic properties, have been proposed. Although in some recent studies a clinical improvement in COVID-19 patients has been observed, the clinical efficacy of CQ and HCQ in COVID-19 has yet to be proven in randomized controlled studies, many of which are currently ongoing, also considering pharmacokinetics, optimal dosing regimen, therapeutic level and duration of treatment and taking into account patients with different severity degrees of disease [62].
Older people are more prone to develop severe forms of COVID-19 [1]. Oxidative stress results in deleterious effects in both aging and SARS‐CoV‐2 infection. It is also linked to the comorbidities that predispose to poor outcomes with SARS‐CoV‐2 infection. Oxidative stress diminishing not only slows aging, but also reduces the comorbidities placing individuals at high risk of poor outcomes from SARS‐CoV‐2 [Zarafabian et al., 2020]. Individuals who live healthy lifestyles and consume geroprotectors such as metformin, resveratrol, and NAD + boosters may have a decreased risk of COVID-19 fatality [1,63,64].
As mentioned before, oxidative stress during viral infection causes various interactions with the host leading to severe clinical syndromes, including the decrease of hemoglobin quote, iron increase, the release of toxic heme, and feroptosis. They are described as key players in the pathology of SARS-CoV-2 infection, and important triggers of inflammation disturb lung function. In such cases, antioxidant supplementation can ameliorate the consequences of infection. Although positive effects have been observed in infected cells and animals, there are no accurate clinical data for many antioxidants and diet supplements (Fig. 1). On the other hand, various nutraceuticals and functional foods have a wide potential for preventing viral infection and modulation of immune responses [4].
Recently it has been shown that SARS-CoV-2 spike (S) glycoprotein receptor binding domains tightly bind linolenic acid. If so, the fatty acid-binding pocket offers a promising target for the development of small molecule anti-COVID-19 inhibitors, which block binding of S protein to ACE-2 receptor [65]. Free fatty acids show a broad spectrum of activities, making them attractive agents for various medical applications.
Some potential therapies in hemoglobin dysfunction and COVID-19 pathophysiology can be found in natural compounds with antioxidant properties. Generally, an antioxidant is a substance that delays, prevents, or removes oxidative damage to a target molecule (the cell). Still, oxidative stress is defined as an imbalance between oxidants and antioxidants, leading to a disruption of redox signaling and control, and molecular damage [66]. The other natural compounds, for example curcumin, quercetin, phloretin, berberine, sulforaphone and many other show a preventive potential towards SARS-CoV-2 infection [14,66,67]. They may act as ROS scavengers or through epigenetic mechanisms (Fig. 1).
Among the plethora of antioxidants, there is a huge group of carotenoids (700 compounds). Carotenoids are a family of natural compounds, plant pigments that provide much of the color we see in nature. They occur in fruits and vegetables and give plants their bright yellow, orange and red colours. They are synthesized by plants and microorganisms but not in humans. They are well recognized as diet supplements with multiple health benefits. Carotenoids are recognized for their anti-oxidative and anti-inflammatory effects. They have also been proposed as anti-viral agents, based on the indirect contribution of the anti-oxidative and anti-inflammatory activities to the function of the immune system overall strength of the body [68]. One of the best-known carotenoids is lycopene, the red pigment of tomato [69].
7. Therapeutic properties of lycopene
As discussed above, various data that support the association of oxidative stress and ROS with SARS-CoV-2 infection and pathogenesis (Fig. 2). It seems that there is a possibility to restrict the effects of ROS in COVID-19 patients with lycopene [69]. Knowing the therapeutic potential of lycopene in various diseases as a strong antioxidant and epigenetic modulator, we would like to suggest the significant potential role of lycopene in the treatment of COVID-19.
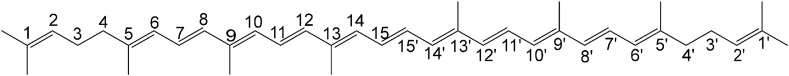
Lycopene is a red-pigmented polyunsaturated hydrocarbon (linear carotenoid) with chemical formula C40H56 and a molecular mass of 536.85 Da. It contains 11 conjugated and 2 non-conjugated double bonds (Fig. 3 ). It is lipophilic and therefore more soluble in fat. Due to double bonds, cis-trans isomerization takes place [70]. The mean plasma level of lycopene varies from 0.2 to 1.1 nmol/ml [71]. Lycopene has a half-life of ca 2–3 days when consumed [72]. It has been recognized as a safe product for daily dietary intake, which does not show any adverse effects on an individual's health even at the highest intake level of 3 g/kg/day [73,74]. Humans absorb ca 10–30% of lycopene present in their diet. It is absorbed in the small intensive where, together with lipids, contributes to the formation of micelles, which are transported into mucosal cells and the gastrointestinal tract [75].
Fig. 3.
Chemical structure of lycopene [69]. It is a highly unsaturated open straight chain hydrocarbon consisting of 11 conjugated and 2 unconjugated double bonds. Through that it has a strong single-oxygen quenching ability and is a potent antioxidant.
Lycopene has been proposed as a compound that can reduce oxidative stress-mediated human diseases like cancer, metabolic and neurodegenerative diseases, as well as viral infections [[72], [75], [91]]. It also shows antidiabetic, cardioprotective, antiinflammatory, hepatoprotective, neuroprotective, and bone protective properties. Its mechanisms of action can be divided into oxidative and non-oxidative.
Lycopene most likely acts through the oxidative mechanism. Because of 11 conjugated double bonds, through many electrons, it can neutralize (scavenge) free radicals, therefore reducing oxidative stress, and preventing lipids, proteins, and DNA damage [76]. ROS are electrochemically imbalanced molecules and therefore highly reactive and capable of modifying cell components [77,78]. Thus, it prevents the potential transformation of normal cells to cancer cells [79]. It has been shown that lycopene consumption of 30 mg/day could alleviate the lymphocyte DNA damage and urinary 8-OH-G contents compared to control levels [80].
Lycopene also modulates gene functions, carcinogen-metabolizing enzymes, apoptosis, and immune function [79]. It increases gap junction communications, anti-proliferation, pro-differentiation, and anti-lipid peroxidation activities. With the induction of cytochrome P450 and hepatic quinine reductase, it promotes the removal of carcinogens and foreign substances from the body. It inhibits anti-oncogenes‘ phosphorylation, G0/G1 and S-phase of the cell cycle, as well as the activities of platelet-derived growth factor-BB, and matrix metalloproteinases-2 and -9, what results in the decreased tumor growth, invasion, and metastasis [79].
Lycopene shows great beneficial effects in the treatment of several diseases. It showed potential efficacy in the treatment of high-grade gliomas [81], lung cancer [82], and prostate cancer [83]. CNS tumors were proven to arise from oxidative state imbalances [37], as were the other cancers [82,83].
In the CNS, lycopene also acts as a prophylactic and therapeutic agent in other disorders, such as Alzheimer's disease, Parkinson's disease, Huntington's disease, cerebral ischemia, epilepsy, and depression. Lycopene also improves the cognition and memory ability of rodents in such pathologies as diabetes, colchicine exposure, high-fat diet, and aging. Moreover, it can prevent neuro-toxicities induced by monosodium glutamate, trimethyltin, methylmercury, tert-butyl hydroperoxide, and cadmium [84]. All of the mentioned disorders are caused by oxidative stress [85].
Lycopene is also active in viral infections [86,87]. Increased oxidative damage has been found in HCV infection. Administration with lycopene caused HCV clearance and reduced hepatic fibrosis in chronic hepatitis C [Seren et al., 2015]. Lycopene is a powerful antioxidant and counteracts liver damage. It also has a role in the prevention of hepatocellular carcinoma. It seems that lycopene may also enhance the overall response rate to anti-viral therapy and delay the progression of the disease [Seren et al., 2015]. Therefore, it can be applied for the treatment of COVID-19 because of some similarities between HCV and SARS-CoV-2 (Fig. 1).
Moreover, people observed that after drinking a tomato shake, the blood levels of lycopene were significantly lower in participants who had also taken an iron supplement [88]. That only supports the above-mentioned facts that excess of iron ions results in higher ROS production. Lycopene absorbs that excess, is used out, what results in lower body fluids concentration. That state resembles SASR-CoV-2 infection, which is connected with increased iron levels [89].
All the above-mentioned arguments and examples suggest lycopene can be used for the treatment and prevention of COVID-19 [90].
8. Perspectives
There is still a long way to go before we fully understand SARS-CoV-2 action and pathogenesis of COVID-19, but we know already that inflammation, as well as natural compounds, are elements of the equation, and natural antioxidants should be considered as promising candidates for effectively treating patients with SARS-CoV-2.
CRediT authorship contribution statement
Anna-Maria Barciszewska: Conceptualization, Methodology, Resources, Investigation, Writing – original draft, Visualization, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
List of abbreviations
- ACE2
angiotensin-converting enzyme 2
- ARDS
acute respiratory distress syndrome
- CNS
acute respiratory distress syndrome
- COVID-19
coronavirus disease 19
- CQ
chloroquine
- FLAIR
Fluid-attenuated inversion recovery (MRI sequence)
- HCQ –
hydroxychloroquine
- NRP1
neuropilin-1
- ROS
reactive oxygen species
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
References
- 1.Mueller A.L., McNamara M.S., Sinclair D.A. Why does COVID-19 disproportionately affect older people? Aging (Albany NY) 2020 May 29;12(10):9959–9981. doi: 10.18632/aging.103344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hou W. Characterization of codon usage pattern in SARS-CoV-2. Virol. J. 2020 Sep 14;17(1):138. doi: 10.1186/s12985-020-01395-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ni W., Yang X., Yang D., Bao J., Li R., Xiao Y., Hou C., Wang H., Liu J., Yang D., Xu Y., Cao Z., Gao Z. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit. Care. 2020 Jul 13;24(1):422. doi: 10.1186/s13054-020-03120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haslberger A., Jacob U., Hippe B., Karlic H. Mechanisms of selected functional foods against viral infections with a view on COVID-19: mini review. Funct. Food Health Dis. 2020;10(5):195–209. doi: 10.31989/ffhd.v10i5.707. [DOI] [Google Scholar]
- 5.Cantuti-Castelvetri L., Ojha R., Pedro L.D., Djannatian M., Franz J., Kuivanen S., van der Meer F., Kallio K., Kaya T., Anastasina M., Smura T., Levanov L., Szirovicza L., Tobi A., Kallio-Kokko H., Österlund P., Joensuu M., Meunier F.A., Butcher S.J., Winkler M.S., Mollenhauer B., Helenius A., Gokce O., Teesalu T., Hepojoki J., Vapalahti O., Stadelmann C., Balistreri G., Simons M. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020 Nov 13;370(6518):856–860. doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raha A.A., Chakraborty S., Henderson J., Mukaetova-Ladinska E., Zaman S., Trowsdale J., Raha-Chowdhury R. Investigation of CD26, a potential SARS-CoV-2 receptor, as a biomarker of age and pathology. Biosci. Rep. 2020 Dec 23;40(12) doi: 10.1042/BSR20203092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly J.L., Simonetti B., Klein K., Chen K.E., Williamson M.K., Antón-Plágaro C., Shoemark D.K., Simón-Gracia L., Bauer M., Hollandi R., Greber U.F., Horvath P., Sessions R.B., Helenius A., Hiscox J.A., Teesalu T., Matthews D.A., Davidson A.D., Collins B.M., Cullen P.J., Yamauchi Y. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. 2020 Nov 13;370(6518):861–865. doi: 10.1126/science.abd3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C., Zhang Y., Song J., Wang S., Chao Y., Yang Z., Xu J., Zhou X., Chen D., Xiong W., Xu L., Zhou F., Jiang J., Bai C., Zheng J., Song Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in wuhan, China. JAMA Intern Med. 2020 Jul 1;180(7):934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li S., Ma F., Yokota T., Garcia G., Jr., Palermo A., Wang Y., Farrell C., Wang Y.C., Wu R., Zhou Z., Pan C., Morselli M., Teitell M.A., Ryazantsev S., Fishbein G.A., Ten Hoeve J., Arboleda V.A., Bloom J., Dillon B.J., Pellegrini M., Lusis A.J., Graeber T.G., Arumugaswami V., Deb A. Metabolic reprogramming and epigenetic changes of vital organs in SARS-CoV-2 induced systemic toxicity. JCI Insight. 2020 Dec 7 doi: 10.1172/jci.insight.145027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J., Hlh Across Speciality Collaboration, Uk COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020 Mar 28;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. 10229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garvin M.R., Alvarez C., Miller J.I., Prates E.T., Walker A.M., Amos B.K., Mast A.E., Justice A., Aronow B., Jacobson D. A mechanistic model and therapeutic interventions for COVID-19 involving a RAS-mediated bradykinin storm. Elife. 2020 Jul 7;9 doi: 10.7554/eLife.59177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matacic C. Blood vessel injury may spur disease's fatal second phase. Science. 2020 Jun 5;368(6495):1039–1040. doi: 10.1126/science.368.6495.1039. [DOI] [PubMed] [Google Scholar]
- 13.Kernan K.F., Carcillo J.A. Hyperferritinemia and inflammation. Int. Immunol. 2017 Nov 1;29(9):401–409. doi: 10.1093/intimm/dxx031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cavezzi A., Troiani E., Corrao S. COVID-19: hemoglobin, iron, and hypoxia beyond inflammation. A narrative review. Clin. Pract. 2020 May 28;10(2):1271. doi: 10.4081/cp.2020.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ganz T. Iron and infection. Int. J. Hematol. 2018 Jan;107(1):7–15. doi: 10.1007/s12185-017-2366-2. [DOI] [PubMed] [Google Scholar]
- 16.Leisman D.E., Ronner L., Pinotti R., Taylor M.D., Sinha P., Calfee C.S., Hirayama A.V., Mastroiani F., Turtle C.J., Harhay M.O., Legrand M., Deutschman C.S. Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir Med. 2020 Dec;8(12):1233–1244. doi: 10.1016/S2213-2600(20)30404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edeas M., Saleh J., Peyssonnaux C. Iron: innocent bystander or vicious culprit in COVID-19 pathogenesis? Int. J. Infect. Dis. 2020 Aug;97:303–305. doi: 10.1016/j.ijid.2020.05.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ayanian S., Reyes J., Lynn L., Teufel K. The association between biomarkers and clinical outcomes in novel coronavirus pneumonia in a US cohort. Biomarkers Med. 2020 Aug;14(12):1091–1097. doi: 10.2217/bmm-2020-0309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu W., Li H. COVID-19: attacks the 1-beta chain of hemoglobin and captures the porphyrin to inhibit human heme metabolism. ChemRxiv. 2020 doi: 10.26434/chemrxiv.11938173.v9. [DOI] [Google Scholar]
- 20.Figlerowicz M., Mania A., Lubarski K., Lewandowska Z., Służewski W., Derwich K., Wachowiak J., Mazur-Melewska K. First case of convalescent plasma transfusion in a child with COVID-19-associated severe aplastic anemia. Transfus. Apher. Sci. 2020 Oct;59(5) doi: 10.1016/j.transci.2020.102866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drakesmith H., Prentice A. Viral infection and iron metabolism. Nat. Rev. Microbiol. 2008 Jul;6(7):541–552. doi: 10.1038/nrmicro1930. [DOI] [PubMed] [Google Scholar]
- 22.Khomich O.A., Kochetkov S.N., Bartosch B., Ivanov A.V. Redox biology of respiratory viral infections. Viruses. 2018 Jul 26;10(8):392. doi: 10.3390/v10080392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kell D.B., Pretorius E. Serum ferritin is an important inflammatory disease marker, as it is mainly a leakage product from damaged cells. Metall. 2014 Apr;6(4):748–773. doi: 10.1039/c3mt00347g. [DOI] [PubMed] [Google Scholar]
- 24.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M., Kaptein F.H.J., van Paassen J., Stals M.A.M., Huisman M.V., Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020 Jul;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sies H. Findings in redox biology: from H2O2 to oxidative stress. J. Biol. Chem. 2020 Sep 25;295(39):13458–13473. doi: 10.1074/jbc.X120.015651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Winterbourn C.C. Reconciling the chemistry and biology of reactive oxygen species. Nat. Chem. Biol. 2008 May;4(5):278–286. doi: 10.1038/nchembio.85. [DOI] [PubMed] [Google Scholar]
- 27.Cadet J., Wagner J.R. DNA base damage by reactive oxygen species, oxidizing agents, and UV radiation. Cold Spring Harb Perspect Biol. 2013 Feb 1;5(2) doi: 10.1101/cshperspect.a012559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Delgado-Roche L., Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch. Med. Res. 2020 Jul;51(5):384–387. doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waris G., Ahsan H. Reactive oxygen species: role in the development of cancer and various chronic conditions. J. Carcinog. 2006 May 11;5:14. doi: 10.1186/1477-3163-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sorokin A.V., Karathanasis S.K., Yang Z.H., Freeman L., Kotani K., Remaley A.T. COVID-19-Associated dyslipidemia: implications for mechanism of impaired resolution and novel therapeutic approaches. Faseb. J. 2020 Aug;34(8):9843–9853. doi: 10.1096/fj.202001451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Valko M., Rhodes C.J., Moncol J., Izakovic M., Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem. Biol. Interact. 2006 Mar 10;160(1):1–40. doi: 10.1016/j.cbi.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 32.Nakabeppu Y. Cellular levels of 8-oxoguanine in either DNA or the nucleotide pool play pivotal roles in carcinogenesis and survival of cancer cells. Int. J. Mol. Sci. 2014 Jul 15;15(7):12543–12557. doi: 10.3390/ijms150712543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pogribny I.P., Beland F.A. DNA hypomethylation in the origin and pathogenesis of human diseases. Cell. Mol. Life Sci. 2009 Jul;66(14):2249–2261. doi: 10.1007/s00018-009-0015-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smolarek I., Wyszko E., Barciszewska A.M., Nowak S., Gawronska I., Jablecka A., Barciszewska M.Z. Global DNA methylation changes in blood of patients with essential hypertension. Med Sci Monit. 2010 Mar;16(3):CR149–155. [PubMed] [Google Scholar]
- 35.Barciszewska A.M., Nowak S., Naskręt-Barciszewska M.Z. The degree of global DNA hypomethylation in peripheral blood correlates with that in matched tumor tissues in several neoplasia. PloS One. 2014 Mar 20;9(3) doi: 10.1371/journal.pone.0092599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barciszewska A.M. Global DNA demethylation as an epigenetic marker of human brain metastases. Biosci. Rep. 2018 Oct 22;38(5) doi: 10.1042/BSR20180731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barciszewska A.M., Giel-Pietraszuk M., Perrigue P.M., Naskręt-Barciszewska M. Total DNA methylation changes reflect random oxidative DNA damage in gliomas. Cells. 2019 Sep 11;8(9):1065. doi: 10.3390/cells8091065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barciszewska A.M. Total DNA methylation as a biomarker of DNA damage and tumor malignancy in intracranial meningiomas. BMC Canc. 2020 Jun 3;20(1):509. doi: 10.1186/s12885-020-06982-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barciszewska M.Z., Barciszewska A.M., Rattan S.I. TLC-based detection of methylated cytosine: application to aging epigenetics. Biogerontology. 2007 Dec;8(6):673–678. doi: 10.1007/s10522-007-9109-3. [DOI] [PubMed] [Google Scholar]
- 40.Johnson A.A., Akman K., Calimport S.R., Wuttke D., Stolzing A., de Magalhães J.P. The role of DNA methylation in aging, rejuvenation, and age-related disease. Rejuvenation Res. 2012 Oct;15(5):483–494. doi: 10.1089/rej.2012.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Siomek A., Gackowski D., Rozalski R., Dziaman T., Szpila A., Guz J., Olinski R. Higher leukocyte 8-oxo-7,8-dihydro-2'-deoxyguanosine and lower plasma ascorbate in aging humans? Antioxidants Redox Signal. 2007 Jan;9(1):143–150. doi: 10.1089/ars.2007.9.143. [DOI] [PubMed] [Google Scholar]
- 42.Kowalska M., Piekut T., Prendecki M., Sodel A., Kozubski W., Dorszewska J. Mitochondrial and nuclear DNA oxidative damage in physiological and pathological aging. DNA Cell Biol. 2020 Aug;39(8):1410–1420. doi: 10.1089/dna.2019.5347. [DOI] [PubMed] [Google Scholar]
- 43.Ousset P.J., Vellas B. Viewpoint: impact of the covid-19 outbreak on the clinical and research activities of memory clinics: an Alzheimer's disease center facing the covid-19 crisis. J Prev Alzheimers Dis. 2020;7(3):197–198. doi: 10.14283/jpad.2020.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lu H., Liu X., Deng Y., Qing H. DNA methylation, a hand behind neurodegenerative diseases. Front. Aging Neurosci. 2013 Dec 5;5:85. doi: 10.3389/fnagi.2013.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adamczyk-Sowa M., Galiniak S., Żyracka E., Grzesik M., Naparło K., Sowa P., Bartosz G., Sadowska-Bartosz I. Oxidative modification of blood serum proteins in multiple sclerosis after interferon beta and melatonin treatment. Oxid Med Cell Longev. 2017 doi: 10.1155/2017/7905148. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gwo C.Y., Zhu D.C., Zhang R. Brain white matter hyperintensity lesion characterization in T2 fluid-attenuated inversion recovery magnetic resonance images: shape, texture, and potential growth. Front. Neurosci. 2019 Apr 16;13:353. doi: 10.3389/fnins.2019.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haller S., Kövari E., Herrmann F.R., Cuvinciuc V., Tomm A.M., Zulian G.B., Lovblad K.O., Giannakopoulos P., Bouras C. Do brain T2/FLAIR white matter hyperintensities correspond to myelin loss in normal aging? A radiologic-neuropathologic correlation study. Acta Neuropathol Commun. 2013 May 9;1:14. doi: 10.1186/2051-5960-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kandemirli S.G., Dogan L., Sarikaya Z.T., Kara S., Akinci C., Kaya D., Kaya Y., Yildirim D., Tuzuner F., Yildirim M.S., Ozluk E., Gucyetmez B., Karaarslan E., Koyluoglu I., Demirel Kaya H.S., Mammadov O., Kisa Ozdemir I., Afsar N., Citci Yalcinkaya B., Rasimoglu S., Guduk D.E., Kedir Jima A., Ilksoz A., Ersoz V., Yonca Eren M., Celtik N., Arslan S., Korkmazer B., Dincer S.S., Gulek E., Dikmen I., Yazici M., Unsal S., Ljama T., Demirel I., Ayyildiz A., Kesimci I., Bolsoy Deveci S., Tutuncu M., Kizilkilic O., Telci L., Zengin R., Dincer A., Akinci I.O., Kocer N. Brain MRI findings in patients in the intensive care unit with COVID-19 infection. Radiology. 2020 Oct;297(1):E232–E235. doi: 10.1148/radiol.2020201697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kremer S., Lersy F., de Sèze J., Ferré J.C., Maamar A., Carsin-Nicol B., Collange O., Bonneville F., Adam G., Martin-Blondel G., Rafiq M., Geeraerts T., Delamarre L., Grand S., Krainik A., SFNR-Covid Group Brain MRI findings in severe COVID-19: a retrospective observational study. Radiology. 2020 Nov;297(2):E242–E251. doi: 10.1148/radiol.2020202222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Doi K., Ikeda M., Hayase N., Moriya K., Morimura N., Covid-UTH Study Group Nafamostat mesylate treatment in combination with favipiravir for patients critically ill with Covid-19: a case series. Crit. Care. 2020 Jul 3;24(1):392. doi: 10.1186/s13054-020-03078-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Singer B.D., Jain M., Budinger G.R.S., Wunderink R.G. A call for rational intensive care in the era of COVID-19. Am. J. Respir. Cell Mol. Biol. 2020 Jul;63(1):132–133. doi: 10.1165/rcmb.2020-0151LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Siddiqui A.J., Jahan S., Ashraf S.A., Alreshidi M., Ashraf M.S., Patel M., Snoussi M., Singh R., Adnan M. Current status and strategic possibilities on potential use of combinational drug therapy against COVID-19 caused by SARS-CoV-2. J. Biomol. Struct. Dyn. 2020 Aug 5:1–14. doi: 10.1080/07391102.2020.1802345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.De Flora S., Balansky R., La Maestra S. Rationale for the use of N-acetylcysteine in both prevention and adjuvant therapy of COVID-19. Faseb. J. 2020 Oct;34(10):13185–13193. doi: 10.1096/fj.202001807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Entrenas Castillo M., Entrenas Costa L.M., Vaquero Barrios J.M., Alcalá Díaz J.F., López Miranda J., Bouillon R., Quesada Gomez J.M. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 2020 Oct;203 doi: 10.1016/j.jsbmb.2020.105751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Keller M.J., Kitsis E.A., Arora S., Chen J.T., Agarwal S., Ross M.J., Tomer Y., Southern W. Effect of systemic glucocorticoids on mortality or mechanical ventilation in patients with COVID-19. J. Hosp. Med. 2020 Aug;15(8):489–493. doi: 10.12788/jhm.3497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salles É.L., Khodadadi H., Jarrahi A., Ahluwalia M., Paffaro V.A., Jr., Costigliola V., Yu J.C., Hess D.C., Dhandapani K.M., Baban B. Cannabidiol (CBD) modulation of apelin in acute respiratory distress syndrome. J. Cell Mol. Med. 2020 Nov;24(21):12869–12872. doi: 10.1111/jcmm.15883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sies H., Parnham M.J. Potential therapeutic use of ebselen for COVID-19 and other respiratory viral infections. Free Radic. Biol. Med. 2020 Aug 20;156:107–112. doi: 10.1016/j.freeradbiomed.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hedlund R., Diamond T.K., Uversky V.N. The latitude hypothesis, vitamin D, and SARS-Co-V2. J. Biomol. Struct. Dyn. 2020 Jul 17:1–3. doi: 10.1080/07391102.2020.1794973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wahedi H.M., Ahmad S., Abbasi S.W. Stilbene-based natural compounds as promising drug candidates against COVID-19. J. Biomol. Struct. Dyn. 2020 May 12:1–10. doi: 10.1080/07391102.2020.1762743. [DOI] [PubMed] [Google Scholar]
- 60.Taher M., Tik N., Susanti D. Drugs intervention study in COVID-19 management. Drug Metab Pers Ther. 2021 Apr 5 doi: 10.1515/dmdi-2020-0173. [DOI] [PubMed] [Google Scholar]
- 61.Wang S., Ye J., Kang Z., Peng H., Mackey V., Sun L. The COVID-19 pandemic and the potential treatment of the novel coronavirus SARS-CoV-2. Am J Transl Res. 2021;13(3):871–881. [PMC free article] [PubMed] [Google Scholar]
- 62.Quiros Roldan E., Biasiotto G., Magro P., Zanella I. The possible mechanisms of action of 4-aminoquinolines (chloroquine/hydroxychloroquine) against Sars-Cov-2 infection (COVID-19): a role for iron homeostasis? Pharmacol. Res. 2020 Aug;158 doi: 10.1016/j.phrs.2020.104904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Moskalev A., Chernyagina E., Kudryavtseva A., Shaposhnikov M. Geroprotectors: a unified concept and screening approaches. Aging Dis. 2017;8(3):354–363. doi: 10.14336/AD.2016.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Trendelenburg A.U., Scheuren A.C., Potter P., Müller R., Bellantuono I. Geroprotectors: a role in the treatment of frailty. Mech. Ageing Dev. 2019 Jun;180:11–20. doi: 10.1016/j.mad.2019.03.002. [DOI] [PubMed] [Google Scholar]
- 65.Toelzer C., Gupta K., Yadav S.K.N., Borucu U., Davidson A.D., Kavanagh Williamson M., Shoemark D.K., Garzoni F., Staufer O., Milligan R., Capin J., Mulholland A.J., Spatz J., Fitzgerald D., Berger I., Schaffitzel C. Free fatty acid binding pocket in the locked structure of SARS-CoV-2 spike protein. Science. 2020 Nov 6;370(6517):725–730. doi: 10.1126/science.abd3255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xian Y., Zhang J., Bian Z., Zhoun H., Zhang Z., Lin Z., Xu H. Bioactive natural compounds against humancoronaviruses: a review and perspective. Acta Pharm. Sin. B. 2020;10(7):1163–1174. doi: 10.1016/j.apsb.2020.06.002. 1163-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pruimboom L. Methylation pathways and SARS-CoV-2 lung infiltration and cell membrane-virus fusion are both subject to epigenetics. Front Cell Infect Microbiol. 2020 May 26;10:290. doi: 10.3389/fcimb.2020.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Elfiky A.A. Natural products may interfere with SARS-CoV-2 attachment to the host cell. J. Biomol. Struct. Dyn. 2020 May 5:1–10. doi: 10.1080/07391102.2020.1761881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grabowska M., Wawrzyniak D., Rolle K., Chomczyński P., Oziewicz S., Jurga S., Barciszewski J. Let food be your medicine: nutraceutical properties of lycopene. Food Funct. 2019 Jun 19;10(6):3090–3102. doi: 10.1039/c9fo00580c. [DOI] [PubMed] [Google Scholar]
- 70.Saawarn N., Shashikanth M.C., Saawarn S., Jirge V., Chaitanya N.C., Pinakapani R. Lycopene in the management of oral lichen planus: a placebo-controlled study. Indian J. Dent. Res. 2011 Sep-Oct;22(5):639–643. doi: 10.4103/0970-9290.93448. [DOI] [PubMed] [Google Scholar]
- 71.Schierle J., Bretzel W., Bühler I., Faccin N., Hess D., Steiner K., Schüep W. Content and isomeric ratio of lycopene in food and human blood plasma. Food Chem. 1997;59(3):459–465. doi: 10.1016/s0308-8146(96)00177-x. [DOI] [Google Scholar]
- 72.Rao A.V., Ray M.R., Rao L.G. Lycopene. Adv Food Nutr Res. 2006;51:99–164. doi: 10.1016/S1043-4526(06)51002-2. [DOI] [PubMed] [Google Scholar]
- 73.Singh D., Aggarwal S. Lycopene in oral diseases. Guident. 2012;5:73–74. [Google Scholar]
- 74.Gupta S., Jawanda M.K., Arora V., Mehta N., Yadav V. Role of lycopene in preventing oral diseases as a nonsurgical aid of treatment. Int. J. Prev. Med. 2015 Aug 5;6:70. doi: 10.4103/2008-7802.162311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chauhan K., Sharma S., Agarwal N., Chauhan B. Lycopene of tomato fame: its role in health and disease. IJPSR. 2011;10:99–115. [Google Scholar]
- 76.Palozza P., Catalano A., Simone R., Cittadini A. Lycopene as a guardian of redox signalling. Acta Biochim. Pol. 2012;59(1):21–25. [PubMed] [Google Scholar]
- 77.Crowe-White K.M., Phillips T.A., Ellis A.C. Lycopene and cognitive function. J. Nutr. Sci. 2019 May 29;8 doi: 10.1017/jns.2019.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jeong Y., Lim J.W., Kim H. Lycopene inhibits reactive oxygen species-mediated NF-κB signaling and induces apoptosis in pancreatic cancer cells. Nutrients. 2019 Apr 1;11(4):762. doi: 10.3390/nu11040762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.van Breemen R.B., Pajkovic N. Multitargeted therapy of cancer by lycopene. Canc. Lett. 2008 Oct 8;269(2):339–351. doi: 10.1016/j.canlet.2008.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Devaraj S., Mathur S., Basu A., Aung H.H., Vasu V.T., Meyers S., Jialal I. A dose-response study on the effects of purified lycopene supplementation on biomarkers of oxidative stress. J. Am. Coll. Nutr. 2008 Apr;27(2):267–273. doi: 10.1080/07315724.2008.10719699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Puri T., Goyal S., Julka P.K., Nair O., Sharma D.N., Rath G.K. Lycopene in treatment of high-grade gliomas: a pilot study. Neurol. India. 2010 Jan-Feb;58(1):20–23. doi: 10.4103/0028-3886.60389. [DOI] [PubMed] [Google Scholar]
- 82.Palozza P., Simone R.E., Catalano A., Mele M.C. Tomato lycopene and lung cancer prevention: from experimental to human studies. Cancers. 2011 May 11;3(2):2333–2357. doi: 10.3390/cancers3022333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mirahmadi M., Azimi-Hashemi S., Saburi E., Kamali H., Pishbin M., Hadizadeh F. Potential inhibitory effect of lycopene on prostate cancer. Biomed. Pharmacother. 2020 Sep;129 doi: 10.1016/j.biopha.2020.110459. [DOI] [PubMed] [Google Scholar]
- 84.Chen D., Huang C., Chen Z. A review for the pharmacological effect of lycopene in central nervous system disorders. Biomed. Pharmacother. 2019 Mar;111:791–801. doi: 10.1016/j.biopha.2018.12.151. [DOI] [PubMed] [Google Scholar]
- 85.Uttara B., Singh A.V., Zamboni P., Mahajan R.T. Oxidative stress and neurodegenerative diseases: a review of upstream and downstream antioxidant therapeutic options. Curr. Neuropharmacol. 2009 Mar;7(1):65–74. doi: 10.2174/157015909787602823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gupta M., Panizai M., Farooq Tareen M., Ortega-Martinez S., Doreulee N. An overview on novel antioxidant and anti-cancer properties of lycopene: a comprehensive review. GMJ Med. 2018;2(1):45–50. doi: 10.29088/GMJM.2018.45. [DOI] [Google Scholar]
- 87.Kwatra B. A review on potential properties and therapeutic applications of lycopene. Inter J Res Pharm Biomed Sci. 2020;4(4):33–44. doi: 10.32553/ijmbs.v4i4.1081. [DOI] [Google Scholar]
- 88.Kopec R.E., Caris-Veyrat C., Nowicki M., Bernard J.P., Morange S., Chitchumroonchokchai C., Gleize B., Borel P. The effect of an iron supplement on lycopene metabolism and absorption during digestion in healthy humans. Mol. Nutr. Food Res. 2019 Nov;63(22) doi: 10.1002/mnfr.201900644. [DOI] [PubMed] [Google Scholar]
- 89.Perricone C., Bartoloni E., Bursi R., Cafaro G., Guidelli G.M., Shoenfeld Y., Gerli R. COVID-19 as part of the hyperferritinemic syndromes: the role of iron depletion therapy. Immunol. Res. 2020 Aug;68(4):213–224. doi: 10.1007/s12026-020-09145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alothaid H., Aldughaim M.S.K., El Bakkouri K., AlMashhadi S., Al-Qahtani A.A. Similarities between the effect of SARS-CoV-2 and HCV on the cellular level, and the possible role of ion channels in COVID19 progression: a review of potential targets for diagnosis and treatment. Channels. 2020 Dec;14(1):403–412. doi: 10.1080/19336950.2020.1837439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Seren S., Mutchnick M., Hutchinson D., Harmanci O., Bayraktar Y., Mutchnick S., Sahin K., Kucuk O. Potential role of lycopene in the treatment of hepatitis C and prevention of hepatocellular carcinoma. Nutr. Canc. 2008;60(6):729–735. doi: 10.1080/01635580802419772. [DOI] [PubMed] [Google Scholar]
- 92.www.fda.gov/drugs/drug-safety-and-availability/fdas-approval-veklury-remdesivir-treatment-covid-19-science-safety-and-effectiveness.