Abstract
Traditional non-participatory research methodologies have struggled to address the needs of multicultural populations in the United States (U.S.). Community-based participatory research (CBPR) is a research paradigm offering a unique opportunity for culturally appropriate research and improving health equity. CBPR is an equitable, strength-based approach involving all stakeholders throughout the research process. We investigate the field of psychology’s utilization of CBPR as an approach for working with multicultural populations to collaboratively address relevant and impactful research questions. A total of 1912 CBPR-related articles, from 2004 to 2014, were identified using PsycINFO, PubMed, and CINAHL Complete databases. Of these, approximately 16% (n = 311) met our criteria for psychology-related CBPR articles accounting for a negligible amount (<1%) of peer-reviewed publications in mainstream psychological journals during the same time period. Among U.S. psychology-related CBPR articles, 86% focused on multicultural and marginalized populations. Prominent topics of investigation included physical health, mental and behavioral health, and theoretical or methodological articles. Features of publications, including authors’ training, types of journals, study populations, and topics under investigation, were explored for all 1912 publications. Findings highlight an opportunity for further utilization of CBPR within psychology, with key implications for health equity. Recommendations for increasing CBPR uptake within the discipline are also offered.
Keywords: Community-based participatory research, Systematic review, Research with Black, Indigenous and people of color, Health equity, Research methods, Multicultural populations
Introduction
Achieving health equity among multicultural populations in the United States (U.S.) represents one of the key next frontiers in health-related research and promotion. Racial/ethnic minorities (i.e., non-White demographic groups such as African American, Latinos, Asian, Pacific Islander and Native Hawaiian, and American Indian/Alaska Native) now account for over half of the U.S. population under one year of age and are expected to account for over 50% of the general population by 2044 (U.S. Census Bureau, 2015). At the same time, racial/ethnic minorites experience higher rates of chronic diseases such as hypertension, diabetes, HIV/AIDS, cancer, and cardiovascular disease (Crook & Peters, 2008), along with premature death and higher infant mortality (CDC, 2013). It is imperative that scientific paradigms evolve to more effectively meet the needs of multicultural and marginalized communities and individuals. Psychologists have long focused on improving population health and well-being. However, traditional non-participatory research methodologies have oftentimes struggled to translate research into actionable steps to reduce health inequities. Communities with little social capital and particularly segregated communities of color continue to suffer from an unfair burden of disease and mortality (LaVeist, Gaskin, & Trujillo, 2011). Community-based participatory research (CBPR) has emerged as an alternative research orientation with the potential to better engage diverse communities to promote sustainable improvements in health and other outcomes (Wallerstein, Duran, Oetzel, & Minkler, 2018). This paper reviews the state of CBPR within psychology and offers recommendations for our field to better meet the needs of multicultural communities and improve health equity.
Along with other articles in this special collection, we aim to advance the science of CBPR and promote community-engaged research for the field of psychology and other complementary public health and clinical and social science disciplines. Other papers in this special suite of articles elaborate further contributions from the Engage for Equity (E2) study, including measures of partnering processes and outcomes, promising practices, and implementation resources to strengthen effectiveness of CBPR partnerships. To complement these papers on metrics, processes, and practices of community-engaged research, we present a comprehensive 10-year review of the CBPR literature in the field of psychology and highlight its potential application to increase inclusive and equitable research in psychology to improve the health and welfare of multicultural communities. We strive to contextualize the other articles included in this special section and offer readers an overview of current efforts within psychology and draw attention to shortcomings and opportunities for additional implementation within our field.
Increased Popularity and Demand for Community-Engaged Research
Inequities in health and access to resources faced by poor and communities of color are well documented (APA, 2020). Meanwhile, prevention and intervention efforts have largely failed to address this health inequity gap (CDC, 2013). Racial/ethnic minorities continue to be underrepresented in research despite their increasing population size and their higher burden of disease (Chen, Lara, Dang, Paterniti, & Kelly, 2014). This negatively impacts our ability to develop effective diagnoses and treatments and limits our ability to strengthen existing public health promotion and prevention efforts. By meaningfully engaging specific groups impacted by health inequities, we could better understand how theoretical models and proposed solutions may work and also evaluate differential impacts across populations rather than simply reporting average effects (Whitehead, 2007). Moreover, some argue there is often a disconnect between evidence-based research and practice and the needs and lived experiences of these communities (Goldberg-Freeman et al., 2007).
Proper research representation and engagement of multicultural populations, along with cultural centeredness and humility in research and practice, continue to lag in mainstream psychology (Sue, Zane, Nagayama Hall, & Berger, 2009). Research and interventions with racial/ethnic minority populations are often relegated to adapting or tailoring evidence-based interventions (Dutta, 2007), and only recently has there been an emphasis on cultural competence and cultural humility to effectively work with minority groups (Greene-Moton & Minkler, 2019; Sue, 2001). Despite its oversight in traditional non-participatory science, engaging multicultural populations offers a key opportunity for health-related research and the refinement of scientific theories and measurement tools (Institute of Medicine [IOM], 2013; Kagawa Singer, Dressler, & George, 2016). Thus, innovative approaches to research and to development of interventions and/or prevention efforts are critically needed.
Community-engaged research (CEnR) has emerged as a potential alternative to traditional non-participatory research approaches (Ahmed & Palermo, 2010), offering an opportunity to build meaningful partnerships with communities and stakeholders outside of academia, and together tackle relevant and impactful research questions. Funding agencies, including the National Institutes of Health, Clinical Translational and Science Awards program, Patient-Centered Outcomes Research Institute, and others, along with government agencies and foundations (Leviton & Green, 2018) are increasingly including expectations of community engagement in their funded or priority research. Similarly, offices of community engagement are becoming more common in research universities.
Community-engaged research is an umbrella term that encompasses a range of research orientations (more information is provided on the introduction to this special collection), with the most recognized form being CBPR (Balls-Berry & Acosta-Pérez, 2017). Engagement in CEnR can be anywhere in a continuum from university outreach to communities and community-based research to formal partnerships with shared authority, written agreements, and reciprocal support. Thus, we concentrate on CBPR as a CEnR approach with established principles and as one of the most commonly used forms of CEnR (Balls-Berry & Acosta-Pérez, 2017; Gehlert & Coleman, 2010; Ross et al., 2010). Moreover, CBPR has its origins within social justice movements (e.g., Paulo Freire), while other CEnR approaches such as Participatory Action Research and Research Practice Partnership have more roots in the educational sciences (Ortiz et al., 2020).
Community-Based Participatory Research
Community-based participatory research for health is a collaborative research effort that equitably involves all stakeholders or partners in the process while recognizing each other’s strengths (Wallerstein et al., 2018). CBPR is an orientation to research that involves the community in all stages of the research process and conducts research with the community, rather than on or in the community (Wallerstein et al., 2018). In CBPR, research questions and goals are deeply rooted in community needs, their ways of knowing, and their theories of change. Moreover, CBPR’s core principles include a commitment to lasting impacts and to social justice, community capacity building, advocacy, and policy applications. This community and culture-centeredness qualify CBPR as a culturally appropriate form of research (Wallerstein et al., 2019; Walters et al., 2008).
Community-based participatory research has been effective in challenging and redressing social and health inequities (Minkler et al., 2014; Wallerstein & Duran, 2010). CBPR succeeds in improving health outcomes, improving trust, and developing partnerships among communities and researchers (Horowitz, Robinson, & Seifer, 2009; O’Mara-Eves et al., 2015). Moreover, CBPR excels in bridging the gap between science and practice to effectively reduce health inequities (Wallerstein & Duran, 2006). A scoping meta-review—a review of reviews—has also supported key outcomes associated with CBPR including organizational changes, sustainability of partnerships and projects, empowerment changes, improvements in power relations, cultural revitalization, community transformation, and increased health equity (Ortiz et al., 2020). While a comprehensive overview of CBPR’s origins and history is beyond the scope of this paper, a recent article reviews historical developments of CBPR (Collins et al., 2018) and more details—including specifics on different terminology—can also be found on the introduction of this special collection.
Given that CBPR is an orientation to research rather than a set of methods, research questions involving community members or stakeholders (e.g., patient groups, professionals of a certain discipline, and leaders in an area of inquiry) are well suited for this approach. Additionally, projects grappling with issues of equity, social justice, sustainability, and/or areas of inquiry with less current knowledge are also excellent candidates for this research orientation. CBPR has been successful in engaging hard-to-reach groups such as racial/ethnic minorities, persons living with HIV/AIDS, sexual minorities, and youth (Clements-Nolle & Bachrach, 2008). Nonetheless, studies using CBPR range in populations from community members from racial/ethnic populations (Cohen, Lopez, Malloy, & Morello-Frosch, 2012), firefighters (Delisle, Delisle, Chaney, Stopka, & Northcutt, 2013), medical students (Dehaven, Gimpel, Dallo, & Billmeier, 2011), nurses (Katz, Martinez, & Paul, 2011), children (Hunsberger, McGinnis, Smith, Beamer, & O’Malley, 2014), to psychiatric populations (Barrow, Alexander, McKinney, Lawinski, & Pratt, 2014). Applications of CBPR continue to grow in the extant literature, with a recent scoping review identifying 104 English-language reviews of distinct outcomes and populations (Ortiz et al., 2020).
CBPR and Psychology
The field of psychology has increasingly focused on improving physical and mental illnesses and working toward achieving optimal health and well-being. The American Psychological Association (APA) has also emphasized the need to increase the representation of multicultural populations in research and in the workforce, and to promote the study of cultural related factors in all psychological domains (APA, 2002). APA’s multicultural guidelines call on all aspects of the profession to strive for multicultural competence (APA, 2017). While psychology was founded on the study of individual differences, and many subdisciplines are focused on understanding individual-level phenomena (e.g., developmental, cognitive, and personality), virtually all psychological phenomena are shaped by culture, including visual perception, spatial reasoning, categorization, moral reasoning, motivations, and intelligence (Arnett, 2008; Heinrich, Heine, & Norenzayan, 2010). Moreover, subdisciplines such as community psychology, counseling, social psychology, and, more recently, health psychology have decades of work within ecological, empowerment, and social justice perspectives (Murray & Poland, 2006; Speer & Hughey, 1995). Justice is also a core principle of community psychology and psychology at large (APA, 2017; Prilleltensky, 2001). Understanding the role of culture and context, including socioeconomic factors, in psychology and the various psychological subdisciplines will continue to advance the field as a whole. CEnR, such as CBPR, could assist in infusing cultural concepts, link across psychology subdisciplines, and to other related fields, and offer our profession a chance to create a paradigm shift that incorporates a culture-centered perspective (Dutta, 2007; Pedersen, 2001).
Community-based participatory research also offers psychology a unique opportunity to enhance patient-centered research and care, to strengthen our ethical principles and practices, to increase the effectiveness and sustainability of our interventions, boost the real-world generalizability of our research endeavors, and close the research-practice gap (Collins et al., 2018). Recent publications have reviewed the unique benefits and challenges faced by psychologists engaging in this work and delineate differences between traditional non-participatory research and CBPR approaches in psychological research (Collins et al., 2018). CBPR can be of particular relevance to the subfields of clinical, health, school and community psychology and those involved in any consumer or health services related research. For instance, employing CBPR, health psychologists have engaged with African American patients in a randomized control trial to tailor a health behavior intervention (Bogart & Uyeda, 2009). Others have partnered with schools to address childhood obesity and promote policy changes (Patel et al., 2009) and engaged consumers of mental health services in the improvements of such services at a local community mental health center (Case et al., 2014). Reviews have also examined the use of CBPR for mental health issues (Stacciarini, Shattell, Coady, & Wiens, 2011). Additional key examples within psychology have included applying CBPR to issues related to substance use (Nieweglowski et al., 2018), to the growing opioid epidemic (Venner et al., 2018), and it has been listed as a promising avenue to bringing psychological interventions for chronic pain into communities (Ehde, Dillworth, & Turner, 2014).
Psychologists also bring many unique skills that can add value to CBPR partnerships, although some skills and knowledge vary by subdiscipline (e.g., industrial/organizational vs developmental psychology). We have key knowledge in the areas of motivation, behavior change, substance use disorders, mental health and brief interventions, individual differences and change, etc., that would be beneficial to understanding health and related issues, as well as in devising effective interventions. Psychologists are also well trained in assessment and psychometrics that can be an important asset to projects involving data collection, particularly in novel areas or those with nascent or scant literature. We also bring scientific rigor and knowledge of particular methodologies including experimental designs, treatment, and efficacy trials. Finally, our discipline brings a service orientation, which includes values of helping people, customers, patients, and the community.
Goals of the Present Review
Given the importance and utility of CBPR as an alternative research orientation, we examine the current state of CBPR application within psychology. We investigate whether CBPR is a popular approach used in psychology by reviewing the relevant literature over a ten-year period. We explore several features of publications, including authors’ training and employment positions, types of journals publishing CBPR articles, study populations, and topics under investigation. We also elaborate on some of the potential challenges regarding the application of CBPR in psychology. Finally, we offer some suggestions for how the field, in general, could further incorporate CBPR into its research toolbox. We hope results will generate preliminary and baseline data from which to evaluate future community engagement efforts within the discipline.
Methods
We conducted a comprehensive literature review of published, peer-reviewed articles using PsycINFO, PubMed, and CINAHL Complete databases. These represent some of the most comprehensive databases in psychology, social sciences, and health sciences fields such as nursing, public health, medicine, psychiatry, and others, and most importantly, have used CBPR and “community-based participatory research” as a Medical Subject Headings (MeSH) term since 2009, rather than other community engagement terms. CBPR as a MeSH term also encompasses entry terms such as “participatory research” and “community-based research.”
Search Strategy
“Community-based participatory research” and “CBPR” were employed as keyword search terms and MeSH headings, and were intended to provide a wide scope of CBPR-related manuscripts. The search was limited to peer-reviewed articles and publications between January 2004 and December 2014. No language, population, research design, country, or other restrictions were imposed. After identifying duplications, articles were manually inspected for relevance. Electronic searches were conducted between July 2014 and September 2015.
Community-based participatory research was chosen as the main terminology for this review given its prevalence and current popularity within the medical and health sciences fields and with national organizations such as the Centers for Disease Control and Prevention (CDC) and the Institute of Medicine (IOM; IOM, 2003, 2016). As previously discussed, while CEnR encompasses a variety of models and levels of community engagement, CBPR is currently the most popular widely used CEnR model in the U.S. (Balls-Berry & Acosta-Pérez, 2017; Gehlert & Coleman, 2010; Jones & Wells, 2007; Ross et al., 2010) and hence chosen for this review. This is consistent with search terms used in other CBPR reviews, including in MeSH, published in psychological and other relevant journals (Jacquez, Vaughn, & Wagner, 2013; Stacciarini et al., 2011). Further details on the history and evolution of CEnR and CBPR terms are provided by Dr. Wallerstein in the introduction to this special collection of articles.
Selection Criteria
Inclusionary criteria for the articles were: (a) related to CBPR; and (b) published in a peer-reviewed journal between January 2004 and December 2014. Articles meeting these criteria were classified as general CBPR-related manuscripts (i.e., in any discipline of study including psychology). Furthermore, of these articles meeting inclusionary criteria, psychology-related CBPR articles were classified as such if the first or last author was a psychologist by training and/or the article was published in a journal dedicated to psychological research and/or applied work. An internet search (e.g., faculty pages, CVs or bio available online, LinkedIn, and other online profiles) was conducted on all first and last authors in order to assess their graduate training or degree. Doctorate-level psychologists were included as psychologists regardless of their current academic or employment position. The first author was conceptualized as the person making the most significant contribution to the manuscript and potentially organizing and leading other co-authors. Given medical journals’ publishing guidelines, a similar conceptualization was applied to the last author who is often the more senior or lead researcher. Psychology journals were determined by lists from the APA, the Association for Psychological Science (APS), and journals describing their aims or scope with psychology as a primary discipline. Articles for which the first and last authors’ training could not be determined were not included in the final sample.
Procedure
A total of six research assistants were trained as coders and directly supervised by the first author, who also served as a coder. Training occurred by simultaneously coding the same set of articles until achieving consistency. Random checks were conducted throughout in which two coders worked on the same articles for comparison purposes. Regular meetings allowed for discussion of coding questions and served as further training and consistency checks among coders.
Each article was coded for first and last authors’ training, population studied (e.g., racial/ethnic minorities, children and youth, LGBTQ community, low income, rural, and women), and general area of inquiry (e.g., mental and behavioral health, physical health, theory and methods, ethics, and environmental health). For articles authored by a psychologist, we also coded their concentration in graduate training (i.e., clinical, experimental, and counseling), with experimental representing an overarching category including social psychology, developmental, cognitive, community psychology, and other psychological subdisciplines. Each psychologist’s current position was also coded to investigate whether place of employment is associated with publishing CBPR-related work. Furthermore, the publishing journal for each article was coded into one of the following categories: psychology, public health, nursing, medical journal, interdisciplinary journal (including or not including psychology), social science journal, social work, and health education, communication, and promotion.
As another indicator of the field of psychology’s utilization of CBPR, the number of CBPR-related articles published in psychological journals was compared to the total number of articles published in mainstream psychological journals in that same time period. We estimated the total number of peer-reviewed publications during these inclusive 2004–2014 years in all APA, APS, and other coded journals stating psychology as a primary discipline in their Aims and Scope. A total of 104 journals were identified as related to psychology. For each journal, we assessed the number of issues per year and average number of peer-reviewed publications per issue in order to calculate a total number of publications per year and overall total during these inclusive years.
Results
Our overall search revealed a total of 2338 articles. Of these, 426 papers were excluded due to not being related to CBPR (n = 299), not meeting the peer-reviewed criteria (n = 104), or difficulties in locating the first author’s training (n = 23). Generally, papers excluded due to not being related to CBPR only mentioned CBPR either in their references or future directions. Figure 1 offers details on inclusion and exclusion of studies. Overall, 311 (16%) of the included papers (N = 1912) met our criteria of a psychology-related CBPR article. The large majority of these met the criteria of a psychologist by training as the first or last author (n = 248, 80%), while only 18 articles (6%) met the journal criteria and 45 (14%) were classified as meeting both the author and journal criteria.
Fig. 1.
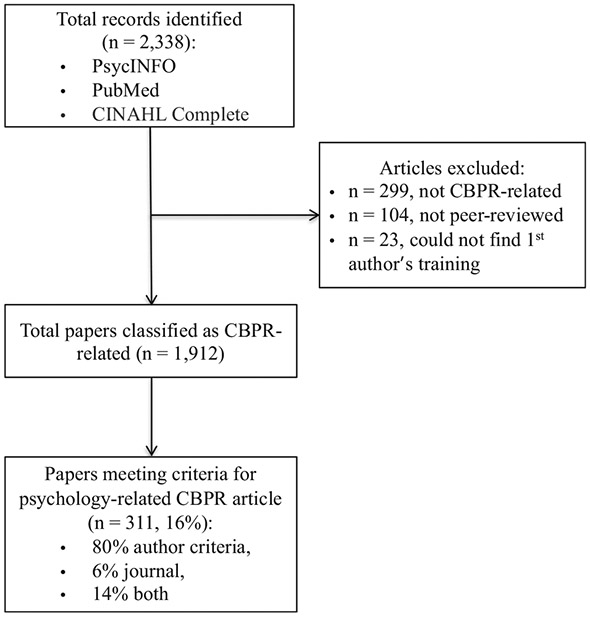
General description of studies identified, and inclusion criteria
Authors’ Related Information
To explore which disciplines or fields of study are at the forefront of CBPR-related work, we coded the first and last author’s training for all unique authors, n = 2877. Public health professionals (e.g., Doctor of Public Health and Master of Public Health) and individuals with medical degrees (i.e., MDs) represent 36% (n = 1051) of the authors publishing CBPR-related work. Psychologists and nursing scholars followed, representing 10% (n = 288) and 9% (n = 270) of the authors, respectively. Other social scientists (e.g., sociology, economics, and anthropology) accounted for another 7% (n = 206). Other notable disciplines included social work (n = 106, 4%), hard sciences such as math and engineering (n = 82, 3%), nutritional sciences (n = 58, 2%), health communication, health education and behavior (n = 73, 3%), and education (n = 94, 3%). Moreover, 15% (n = 430) of authors held a variety of degrees including gerontology, JDs, theology, pharmacy, business, linguistics, history, geography, and others. Finally, 8% of the authors (n = 219) did not have an advance degree, possibly showcasing the number of community partners (e.g., pastors and community-based organization members) serving as authors on publications.
Psychologists as Authors
Psychologists who were authors on the CBPR-related papers tended to have clinical (46%) or experimental backgrounds (47%) in their graduate education, with fewer from counseling concentrations (6%). Author concentration was missing for 1% of these authors, who were all determined to be international scholars. Notably, only about a third (26%) of the psychologists were currently employed in traditional psychology departments (including psychology and counseling departments). Many were employed by other academic departments (19%) such as sociology, health education, community health sciences, African American studies, and social welfare, followed by Schools of Public Health (14%) and psychiatry departments (12%). Fewer of them were employed by medical schools (10%), hospitals (7%), and research or policy centers (4%). Another 8% were employed by a variety of sectors including the National Institutes of Health and the private sector.
Journal Related Information
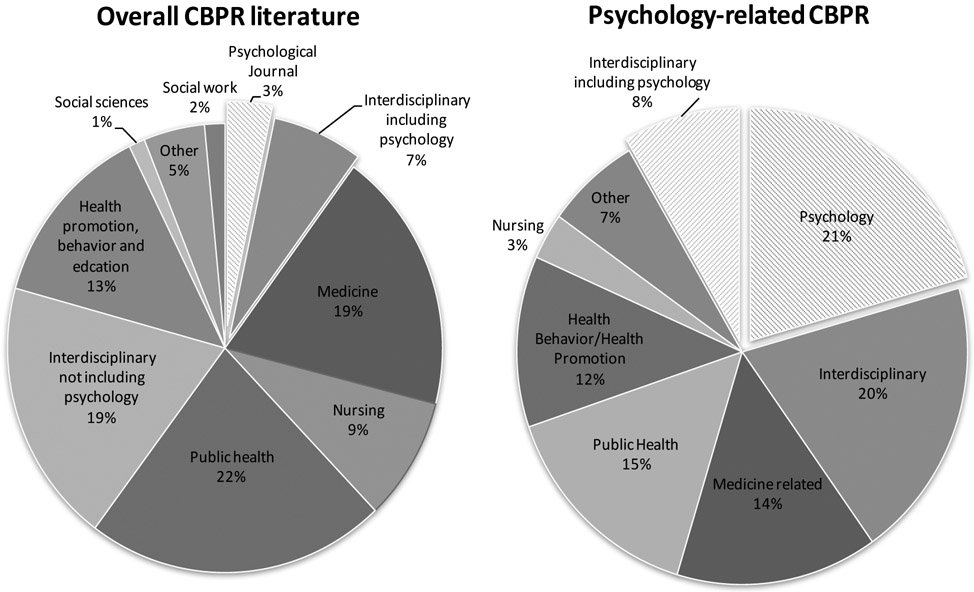
Among all journals that published CBPR-related articles included in this review, those uniquely positioned within psychology (e.g., APS or APA journals) only accounted for 3% of the publications from 2004 to 2014. In addition, interdisciplinary journals explicitly mentioning psychology as a main discipline accounted for an additional 7% of the total CBPR-related publications. Public health-related journals published 22 % of the articles, followed by medical (19%) and interdisciplinary journals (19%) that do not mention psychology as a discipline. Health promotion, health communication, and education journals accounted for another 13% of the CBPR-related publications, followed by nursing journals at 9%. Figure 2 offers details on journals for both the overall literature and for psychology-related articles.
Fig. 2.
Journal classification for overall CBPR-related and psychology-related CBPR articles. Note. Left panel (N = 1912 articles) represents the overall CBPR-related literature. Other category includes journals such as ethics journals, environmental, nutritional, and exercise sciences. Right panel (n = 311) represents the psychology-related CBPR articles. Due to small size, the Other category also includes social work and social sciences journals
Psychology-Related CBPR Articles
Among the 311 articles meeting criteria for psychology-related CBPR manuscripts, only 21% were published in mainstream psychology journals, potentially reducing their impact on the larger discipline. It is worth noting that the American Journal of Community Psychology accounted for the majority (42%) of these mainstream psychology publications. An additional 8% were published in interdisciplinary journals that explicitly mention psychology as a main discipline. Medicine related journals and public health accounted for another 29% of the publications, while general interdisciplinary journals accounted for 20% (see Fig. 2).
Furthermore, in order to investigate the impact of these 311 publications compared to the larger psychological literature, we estimated the total number of peer-reviewed articles published by mainstream psychological journals in the same time period. A total of 104 journals were identified. We estimated that these journals published approximately 48,953 peer-reviewed articles between 2004 and 2014. Thus, these journals published only 63 (i.e., psychology-related CBPR articles meeting the journal criteria) or 0.1% CBPR-related articles according to our criteria. Notably, the majority of these psychology-related publications appeared in more recent years with 79% being published between 2010 and 2014.
Populations of Interest within CBPR Empirical Studies
To gain insights into the potential contribution of CBPR to working with multicultural populations and increasing cultural appropriateness in research, we explored the population of interest for all CBPR-related articles that presented empirical data (see Table 1 for details). Racial/ethnic minority populations accounted for 42% of the articles, followed by 23% of manuscripts concerned with other underrepresented groups in research, including low-income communities, LGBTQ communities, individuals with HIV or AIDS, rural populations, persons with disability, children, youth, and women. Another 12% of articles did not include any population or participants (e.g., theory and method-related publications) or focused on international populations (12%). Thus, within the U.S., 85% of the CBPR-related publications focused on racial/ethnic minorities and other underrepresented groups. Similar to the larger CBPR literature, 48% of the psychology-related CBPR articles dealt with racial/ethnic minority populations and 21% with other vulnerable and/or marginalized groups (see Table 1). Another 10% did not focus on any population and 9% dealt the international samples. Thus, in the U.S. alone and among articles with samples, 86% of psychology-related CBPR manuscripts focused on multicultural or marginalized populations.
Table 1.
Description of CBPR-related articles’ population of interest
| Overall CBPR literature N = 1912 (%) |
Psychology-related CBPR articles n = 311 (%) |
|
|---|---|---|
| Racial/ethnic minorities | 800 (42%) | 150 (48%) |
| Latinos/Hispanics | 185 (10%) | 30 (10%) |
| African Americans | 179 (9%) | 45 (14%) |
| Native American/Alaska Native | 173 (9%) | 42 (13%) |
| AANHPI | 125 (7%) | 19 (6%) |
| Multiple racial/ethnic groups | 138 (7%) | 14 (5%) |
| Other underrepresented groups in research | 439 (23%) | 65 (21%) |
| Low income, underserveda | 131(7%) | 20 (6%) |
| HIV/AIDS and LBTGQ | 36 (2%) | 5 (2%) |
| Immigrants and refugees | 76 (4%) | 9 (3%) |
| Children, and youth | 101 (5%) | 25 (8%) |
| Women | 33 (2%) | 0 (0%) |
| Rural populations | 62 (3%) | 6 (2%) |
| International populations | 237 (12%) | 29 (9%) |
| Theory/methods with no sample | 225 (12%) | 32 (10%) |
| Otherb | 211 (11%) | 35 (11%) |
Abbreviation: AANHPI, Asian American, Native Hawaiian, and Pacific Islander.
Includes individuals with disabilities and individuals with severe mental illness.
Includes researchers, health service providers (e.g., nurses and medical students), and general partnerships.
Finally, we investigated general categories of inquiry. Within the overall published CBPR-related literature (N = 1912), the majority of the published papers (33%) were related to physical health (e.g., diabetes, hypertension, cancer, and physical activity), followed by theoretical or methodology related publications (19%). Mental and behavioral health-related manuscripts accounted for a total of 14% of the articles after combining articles only dealing with mental or behavioral health outcomes with those dealing with multiple categories including mental or behavioral health (e.g., environmental justice and mental health). Other major categories of inquiry included articles with multiple outcomes excluding mental health (6%), environmental health and injustice (6%), policy (3%), and ethics (3%) related publications. Within the psychology-related CBPR literature (n = 311), articles dealing with mental health issues account for a total 26% of the publications (see Table 2). Similar to the larger CBPR literature described previously, physical health-related (30%) and theory or methods (21%) are also prominent areas of inquiry. Table 2 offers further description of articles’ areas of inquiry.
Table 2.
Description of CBPR-related articles’ main inquiry category
| Overall CBPR literature N = 1912 (%) |
Psychology-related CBPR articles N = 311 (%) |
|
|---|---|---|
| Physical health | 622 (33%) | 93 (30%) |
| Theory and methods | 357 (19%) | 66 (21%) |
| Mental and behavioral health | 178 (9%) | 63 (20%) |
| Environmental health/justice | 122 (6%) | 8 (3%) |
| Ethics | 54 (3%) | 4 (1%) |
| Policy | 51 (3%) | 5 (2%) |
| Education/curriculum development | 49 (3%) | 7 (2%) |
| Health care related | 79 (4%) | 4 (1%) |
| Methods for engaging vulnerable populations | 17 (1%) | 2 (1%) |
| Health communication/promotion | 31 (2%) | 4 (1%) |
| Multiple categories excluding mental and behavioral health | 121 (6%) | 12 (4%) |
| Multiple categories including mental and behavioral health | 100 (5%) | 20 (6%) |
| Other | 131 (7%) | 23 (7%) |
Multiple categories represent articles with multiple key areas of interest (e.g., environmental health and policy, physical and mental or behavioral health, ethics, and methods).
Discussion
The present study explored the extent to which CBPR is being utilized within the field of psychology. Our results indicate a limited, although seemingly increasing, application of CBPR. Among the overall CBPR-related literature explored, 16% met our criteria for a psychology-related CBPR manuscript and less than a third of these psychology-related CBPR articles were published in a psychology journal. Key areas of inquiry included physical health, theory and methodological issues, and mental and behavioral health. Investigating populations of interest confirmed that CBPR is well suited for research with multicultural populations and groups traditionally underrepresented in research, with the large majority of the studies dealing with racial/ethnic minority and other marginalized groups.
While there is no current benchmark or framework with which to assess whether psychology-related CBPR articles, as defined by our criteria, represent an underutilization of CBPR by the psychology field, journal placement can perhaps offer some sense of the impact within the discipline. Assuming that scholars are more likely to read and publish within their discipline’s academic journals, manuscripts within these journals are more likely to influence the field. However, less than a third of psychology-related CBPR articles were published in a psychology-related journal. One potential explanation for this finding can be found in our results. Approximately 70% of the psychologists authoring these manuscripts are not currently employed by traditional psychology departments. These scholars are likely placing their work in journals favored by their current employer’s discipline. Additionally, we estimated that only around 0.1% of all publications in mainstream psychological journals within 2004 and 2014 were CBPR related.
As CBPR becomes an increasingly popular approach with funding agencies and for research with multicultural populations, efforts to increase its uptake and visibility within the psychology discipline would be of utmost importance. The last couple of decades have marked significant efforts within academic institutions to increase their capacity for meaningful community engagement. For example, in 2006, the Clinical Translational and Science Award consortium launched 60 academic health centers with the goal of increasing community engagement as an avenue to improve translation and dissemination efforts, improving clinical practice, and ultimately solve large public health problems (Michener et al., 2012). This has also come with an acknowledgment of the need to expand traditional non-participatory research methodologies. Academic medical centers have been among those at the forefront of these efforts (Michener et al., 2012). Thus, increased awareness within our discipline of our own efforts toward CEnR, and CBPR as a specific form of CEnR would aid in our ability to remain competitive in an increasingly innovative and fast-changing academic landscape. Findings from the present paper can help generate ideas and a better understanding of our current standing within these larger efforts.
CBPR and Health Inequities
Our results highlight the potential of CBPR as a research orientation well suited for multicultural populations. Among all U.S. CBPR-related publications, racial/ethnic minorities and other marginalized communities account for 85% of all samples and 86% of CBPR-related publications within psychology. In contrast, psychology has traditionally struggled to engage underrepresented populations and to meaningfully incorporate culture into research questions and designs (Suinn & Borrayo, 2008). WEIRD samples (western, educated, industrialized, rich, and democratic) account for the majority of psychological research samples (Arnett, 2008; Heinrich et al., 2010). Thus, our findings underscore CBPR’s potential to increase our engagement of multicultural and underrepresented populations in research, with key implications for the cultural relevance of our questions and interventions, and the refinement of our theories and measurement tools (Dutta, 2007; Kagawa Singer et al., 2016; Whitehead, 2007).
While the early years in the 1990s of CBPR focused on describing principles and practices of case studies, the interest in the contribution of collaborative processes to health and health equity outcomes has been growing. The first review of CBPR research projects in 2004 from the Agency for Health Care Research and Quality identified only 12 articles with evidence of outcomes. However, a recent scoping review of reviews (meta, systematic, narrative, and other review methodologies, not individual studies) from 2005 to 2018 found over 100 English-language articles; fifty-five of these contained evidence of outcomes, ranging from intermediate outcomes of program sustainability, support networks, and policy changes, as well as health behavior and health equity outcomes (Ortiz et al., 2020). The E2 study, described in the introduction to this special collection, has also identified which partnering practices are most promising for contributing to health and equity outcomes (Oetzel et al., 2018). This question of the added value of participatory practices associated with outcomes remains critically important for psychology as well as the extant literature in other disciplines.
Positive outcomes from CBPR are well documented in the extant literature (Horowitz et al., 2009; Ortiz et al., 2020; Wallerstein & Duran, 2006; Wallerstein et al., 2018). By increasing community participation and ownership, CBPR affects change from within communities in part by increasing compliance and aiding sustainability efforts (Wallerstein & Duran, 2006). Assessment tools are now available that allow partnerships to evaluate different aspects of their CBPR efforts, including impact on system change and health outcomes (Oetzel et al., 2015; Sandoval et al., 2012). Furthermore, CBPR assists in the development of potentially innovative research questions and solutions with direct applicability to community needs (Bogart & Uyeda, 2009), making these efforts well positioned to address issues of health equity. Nonetheless, lasting impacts and upstream level changes must be intentional among partnerships and projects. For example, our data shows that only a small percentage of the articles reviewed relate to policy. This is true for psychology-related articles and those in the overall CBPR literature, raising some concerns for long-lasting equity impacts.
While social justice approaches are not mainstream in psychology, many scholars do work within this framework (Collins et al., 2018). Subdisciplines such as community psychology, counseling, social psychology, and, more recently health psychology, have decades of work within ecological and social justice perspectives (Murray & Poland, 2006). Justice is also a core principle of psychology at large (APA, 2002; Prilleltensky, 2001). Unfortunately, despite an articulation of social justice values, most of the work remains at a theoretical level with little translation into systematic research agendas, action, or prevention efforts (Prilleltensky, 2001). CBPR and other CEnR models offer an opportunity to meaningfully engaged with historically disenfranchised communities, improve population health, and bridge the gap between research and practice for social change.
Challenges and Recommendations to CBPR in Psychology
Given the potential benefits of community engagement and CBPR in particular, along with their growing demand by funding agencies, governing bodies, and community groups, we offer some recommendations to promote the increased use of these models within the field of psychology. Recommendations are based on challenges identified in the extant literature. Given that these challenges are often prevalent throughout academia, we hope this section is relevant for various fields hoping to increase their CEnR. We acknowledge our data evaluated the prevalence of CBPR’s utilization rather than its effectiveness in bringing about desirable outcomes or its scientific rigor. While this presents a tension with the following recommendations, we also acknowledge the growing literature around the positive outcomes of CBPR, some of which we highlight. Thus, recommendations below are within the framework that usefulness of CBPR has been increasingly recognized, creating some urgency for psychology to stay up to date with a changing scientific environment.
Diversity among Faculty and Student Researchers
One possible challenge to the increased application of CBPR in psychology is the lack of racial/ethnic minority researchers. Racial/ethnic minorities represent only 16% of the active psychology workforce, compared to 40% of the general U.S. workforce (APA Center for Workforce Studies, 2015). Minority faculty comprise <14% of the total faculty among U.S. psychology graduate departments (Hart, Wicherski, & Kohout, 2011). Although it is not necessary to be a minority to do research with multicultural populations, the vast majority of researchers involved with underrepresented communities are minorities themselves (Viets et al., 2009). The lack of diversity among researchers may also contribute to community mistrust, affecting participation and the development of meaningful research partnerships. Therefore, increasing recruitment and retention of diverse researchers and graduate students is key (Viets et al., 2009). CBPR may also help with the recruitment of youth and recent college graduates by involving them in the research process. CBPR projects have documented increases in personal capacity, with individuals participating in projects pursuing higher education, grants, and acquiring other skills (Israel et al., 2010; Rhodes, Malow, & Jolly, 2010).
Training
Granting and accreditation agencies are increasingly demanding CBPR in both funded projects and graduate programs (Horowitz et al., 2009; IOM, 2016). Our curricula must then be adept at training the next generation of researchers in CBPR methods (Ahmed & Palermo, 2010). Studies have found that researchers tend to use methods in which they were trained (Stacciarini et al., 2011), making graduate training particularly important. Unfortunately, most psychology graduate departments offer a single course covering multicultural issues, including research methods for multicultural populations. Moreover, most curricula lack policy or advocacy training, which are often components of CBPR projects. If not provided within graduate programs, acquiring this knowledge represents an additional burden for upcoming psychologists and may deter their participation in CBPR projects. Training in CEnR, including CBPR, has been growing, including semester courses, week-long institutes, or short trainings for community and academic partners within Universities, especially academic health centers (Coombe et al., 2019; Parker, Holland, Dennison, Smith, & Jackson, 2018). While departments may not have faculty able to teach a full course on CBPR, online trainings with ancillary materials are now available (Smikowski et al., 2009). Schools of Public Health may also be more likely to teach or engage in CBPR, while CBPR training and networking can also be integrated into psychology-related national conferences (Rodriguez Espinosa, Gil-Kashiwabara, Clifasefi, & Collins, 2020).
Academia
The culture of academia must also change to encourage students and faculty to engage in CBPR. First, we must value communities as key partners in the research process with valuable input including recruitment, interpretation of findings, and adapting of interventions. Second, the promotion and tenure process must value research impact including community-engaged scholarship and efforts to improve health equity over quantity of projects and/or publications (Nyden, 2003; Seifer, Blanchard, Jordan, Gelmon, & McGinley, 2012). The creation and support of academic centers with the mission to increase community-engaged scholarship, decrease health inequities, and serve the needs of low-income communities is needed (Gelmon, Blanchard, Ryan, & Seifer, 2012). These centers may train and support faculty, especially junior faculty, as they engage in CBPR. National CBPR networks are also available that guide and support researchers as they strengthen their proposals and projects (Nyden, 2003).
Journal Responsiveness
As psychology and academia in general make the needed changes to increase the likelihood that scholars will engage in CBPR-related work, journals in the discipline will be called upon to change their publication guidelines and encourage CBPR-related submissions. This may require some education for editors and reviewers in order to better evaluate CBPR manuscripts.
Criticisms of CBPR
Community-based participatory research is not without challenges, including the need for training and experiences in high-quality participatory research not typically found in masters or doctoral level curricula (Ahmed & Palermo, 2010), being time-intensive and requiring an iterative approach oftentimes requiring flexibility in research implementation, balancing complex demands of partners and bureaucratic systems, existing lack of trust among community partners due to institutional histories, and different language and communication styles (Freeman, Seifer, Stupak, & Martinez, 2014; Israel et al., 2005). Another concern in the literature relates to potential difficulties in applying research designs familiar to granting agencies such as randomized controlled trials (RCTs) within a CBPR framework due to ethical and political challenges that arise with random assignment of communities to comparison conditions (Buchanan, Miller, & Wallerstein, 2007). However, RCTs employing a CBPR model are increasing and have shown high success rates in recruiting and retaining minority individuals while achieving significant intervention effects (Chung et al., 2010; De las Nueces, 2012). Within indigenous communities, for example, a recent special issue of Prevention Science highlights the growth of rigorous science within cultural-centered methodologies (Whitesell, Mousseau, Parker, Rasmus, & Allen, 2018).
Another issue is the difficulty in establishing informed consent, as it may not be evident who represents the community (Buchanan et al., 2007) or how many individuals must be involved to assure full representation of the community. Nonetheless, CBPR is arguably the best attempt to resolve issues of respect and autonomy in research (Morello-Frosch, Brown, & Brody, 2018). Moreover, developing trust and relationships with communities can be time-consuming and may require additional funding to support travel, gatherings, food, and potentially additional years at the start of a grant. Therefore, feasibility can also become a source of concern among academics, especially those under the pressure of promotion deadlines.
Strengths, Limitations, and Future Directions
Some key strengths of the present manuscript include the comprehensive nature of our review. To our knowledge, no other reviews in CBPR have included such a large number of articles. We also included articles from multiple disciplines and areas of scope, allowing for some comparisons of areas of interest and a general overview of the prevalence of CBPR-related work among different disciplines. For example, relevant reviews have included article samples ranging from 20 (Stacciarini et al., 2011) to 56 (Jacquez et al., 2013) compared to the nearly 2000 included in ours. Furthermore, we did not limit our search in terms of language, nationality, outcomes, populations, or other restrictions typically found in reviews. Future studies can use our results as a baseline from which to assess future developments around CBPR in general and within psychology.
Nonetheless, our work has some limitations. First, our search terminology was limited to “community-based participatory research” and “CBPR” in various databases and entries used by CBPR as a MeSH term in PubMed (e.g., “participatory research”). Articles using different terminology such as the umbrella CEnR term or alternative forms of CEnR such as “participatory action research” (PAR) may not have been included depending on the article’s use of terms. While we did not exclude articles using CEnR or other participatory research terminology such as PAR, and searched for CBPR terms in the full text, those using other terms exclusively (i.e., never mentioning CBPR in their full text) might not have been included. Thus, reviews with broader and various search terms might yield different articles. While CBPR is often the most popular CEnR model with defined principles and recognized by funding and governing institutions (Balls-Berry & Acosta-Pérez, 2017; Gehlert & Coleman, 2010; IOM, 2003; Ross et al., 2010), it is possible that publications using exclusively other terms were excluded, potentially altering our results. Moreover, our search terms could have influenced the disciplines represented by the authors, as CBPR may be a more prevalent term within medicine and public health. Although our search terms are not atypical in psychology-relevant CBPR reviews (Jacquez et al., 2013; Stacciarini et al., 2011), future studies employing a variety of terms could examine similar questions or evaluate whether results vary by the key terms employed, making a key contribution to future systematic reviews in the CEnR literature.
Our review is also intentionally general in nature to get a broad overview of current efforts within psychology. Future studies should more narrowly investigate efforts within particular areas such as community psychology or among articles dealing with community interventions, health and policy outcomes, or others. It is possible that the representation of CBPR within those varies compared to the larger field of psychology. Moreover, our coding scheme did not include assessing actual quality of these CBPR articles. While assessing the scientific rigor of the manuscripts we reviewed was beyond the scope of the present paper, there remains a need to systematically evaluate the quality of partnerships reported in the literature, their long-terms outcomes and level of analysis, and the relevance of their outcomes for health equity. This is particularly important as terms such as CBPR, CEnR, and others become more common, increasing their potential misuse as buzzwords. Level of community participation can vary across projects (Spears Johnson, Kraemer Diaz, & Arcury, 2016) and community engagement in research may not necessarily translate to novel questions or designs. Thus, future studies rating the quality of the partnerships and relating those to key outcomes including sustainability, policy changes, and other key changes are needed.
We also concentrated on peer-reviewed publications. It is possible that the gray literature might contain other articles of interest that were not included in the present review. In addition, it is possible that psychologists are engaging in CBPR at some level and may not have yet published this work. Finally, due to the large number of articles, our coding of authors’ training was limited to the first and last author. However, even though not exhaustive, we believe these captures both traditional psychology and more medical models for publication.
Conclusion
We reviewed CBPR’s current use in psychology and elaborate on some possible barriers and solutions for increased utilization. As evidenced by our review, additional efforts are needed by our profession in order to better incorporate CBPR and meet its increasing demand by national agencies. As a discipline, CBPR offers us the opportunity to work toward health equity and the empowerment of disenfranchised communities and individuals, in part via meaningful engagement of multicultural populations often underrepresented in research. We must reformulate our identities and make moral choices while fighting injustice and challenging ways of knowing. Within our field, this would involve a commitment to revisit our scientific paradigms and take the needed actions to train and support our workforce in research orientations better suited for research and practice with multicultural populations. Findings can serve as baseline from which to compare future community engagement efforts and offer insights into potential solutions.
Highlights.
We examine the field of psychology’s utilization of CBPR and review 1912 CBPR articles.
Approximately 16% of manuscripts (n = 311) met our criteria for psychology-related CBPR articles.
Of these, only 21% were published in mainstream psychology journals.
Racial/ethnic and marginalized communities account for 85% of all U.S. CBPR-related study samples.
Additional efforts could increase the use of CBPR within the field of psychology.
Acknowledgments
This work was supported by the Robert Wood Johnson Foundation Center for Health Policy and the Psychology Clinical Neuroscience Center at the University of New Mexico. We offer special thanks to Dr. Nina Wallerstein for her feedback on earlier versions of this manuscript, and acknowledge support, in part, by the “Transdisciplinary Research, Equity and Engagement Center for Advancing Behavioral Health” funded by NIMHD (U54 MD004811), “Research for Improved Health” funded by NARCH V (U261IHS0036), and “Engage for Equity (E2)” funded by NINR (1 R01 NR015241-01A1). During part of this work, the first author was supported by the Postdoctoral Fellowship in Cardiovascular Disease Prevention (T32), National Heart, Lung and Blood Institute (NHLBI), NIH 5 T32 HL007034-43. In addition, we thank research assistants Brissa Sotelo, Lluvia A. Trevizo, Ivette Miramontes, Celina Herrera, Danielle Mascarenas, and Andrea Henckel for their invaluable assistance in data coding.
Footnotes
Conflict of Interest
The authors declare that they have no competing interests to disclose.
References
- Ahmed SM, & Palermo A-G-S (2010). Community engagement in research: Frameworks for education and peer review. American Journal of Public Health, 100, 1380–1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association (2002). Guidelines on multicultural education, training, research, practice, and organizations change for psychologists. Washington, DC: Author. Available from: https://apastyle.apa.org/manual/related/guidelines-multicultural-education.pdf [last accessed April 1, 2020] [DOI] [PubMed] [Google Scholar]
- American Psychological Association (2017). Multicultural guidelines: An ecological approach to Context, Identity, and Intersectionality. Washington, DC: Author. Available from: http://www.apa.org/about/policy/multicultural-guidelines.pdf [last accessed September 5, 2019]. [Google Scholar]
- American Psychological Association (2020). Ethnic and racial minorities & socioeconomic status. Washington, DC: Author. Available from: https://www.apa.org/pi/ses/resources/publications/minorities [last accessed September 5, 2019]. [Google Scholar]
- American Psychological Association Center for Workforce Studies (2015). 2005–13: Demographics of the U.S. Psychology Workforce. Washington, DC: Author. Available from: http://www.apa.org/workforce/publications/13-demographics/index.aspx [last accessed March 1, 2019] [Google Scholar]
- Arnett JJ (2008). The neglected 95%: Why American psychology needs to become less American. The American Psychologist, 63, 602–614. [DOI] [PubMed] [Google Scholar]
- Balls-Berry JE, & Acosta-Pérez E (2017). The use of community engaged research principles to improve health: Community academic partnerships for research. Puerto Rico Health Sciences Journal, 36, 84–85. [PMC free article] [PubMed] [Google Scholar]
- Barrow SM, Alexander MJ, McKinney J, Lawinski T, & Pratt C (2014). Context and opportunity: Multiple perspectives on parenting by women with a severe mental illness. Psychiatric Rehabilitation Journal, 37, 176–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, & Uyeda K (2009). Community-based participatory research: Partnering with communities for effective and sustainable behavioral health interventions. Health Psychology, 28, 391–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchanan DR, Miller FG, & Wallerstein N (2007). Ethical issues in community-based participatory research: Balancing rigorous research with community participation in community intervention studies. Progress in Community Health Partnerships, 1, 153–160. [DOI] [PubMed] [Google Scholar]
- Case AD, Byrd R, Claggett E, De Veaux S, Perkins R, Huang C, … & Kaufman JS (2014). Stakeholders’ perspectives on community-based participatory research to enhance mental health services. American Journal of Community Psychology, 54, 397–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2013). Health disparities and inequalities report. Morbidity and Mortality Weekly Reports. Atlanta, GA. Available from: http://www.cdc.gov/minorityhealth/chdireport.html [last accessed April 2, 2019]. [Google Scholar]
- Chen MS, Lara PN, Dang JH, Paterniti DA, & Kelly K (2014). Twenty years post-NIH Revitalization Act: Enhancing minority participation in clinical trials (EMPaCT): Laying the groundwork for improving minority clinical trial accrual. Cancer, 120, 1091–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung B, Jones L, Dixon EL, Miranda J, Wells K, Partners, C, & Care Steering Council (2010). Using a community partnered participatory research approach to implement a randomized controlled trial: Planning community partners in care. Journal of Health Care for the Poor and Underserved, 21, 780–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements-Nolle K, & Bachrach AM (2008). CBPR with a hidden population: The Transgender Community Health Project a decade later. In Minkler M& Wallerstein N (Eds.), Community-based participatory research for health: From process to outcomes. San Francisco: John Wiley & Sons. [Google Scholar]
- Cohen A, Lopez A, Malloy N, & Morello-Frosch R (2012). Our environment, our health: A community-based participatory environmental health survey in Richmond, California. Health Education and Behavior: the Official Publication of the Society for Public Health Education, 39, 198–209. [DOI] [PubMed] [Google Scholar]
- Collins SE, Clifasefi SL, Stanton J, Board TLA, Straits KJE, Gil-Kashiwabara E, … & Wallerstein N (2018). Community-based participatory research (CBPR): Towards equitable involvement of community in psychology research. American Psychologist, 73, 884–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coombe CM, Schulz AJ, Brakefield-Caldwell W, Gray C, Guzman JR, Kieffer EC, … & Israel BA (2019). Applying experiential action learning pedagogy to an intensive course to enhance capacity to conduct community-based participatory research. Pedagogy in Health Promotion, 6, 168–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crook ED, & Peters M (2008). Health disparities in chronic diseases: Where the money is. The American Journal of the Medical Sciences, 335, 266–270. [DOI] [PubMed] [Google Scholar]
- De las Nueces D, Hacker K, DiGirolamo A, & Hicks LS (2012). A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Services Research, 47(3 Pt 2), 1363–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehaven MJ, Gimpel NE, Dallo FJ, & Billmeier TM (2011). Reaching the underserved through community-based participatory research and service learning: Description and evaluation of a unique medical student training program. Journal of Public Health Management and Practice: JPHMP, 17, 363–368. [DOI] [PubMed] [Google Scholar]
- Delisle AT, Delisle AL, Chaney BH, Stopka CB, & Northcutt W (2013). Methods for fostering a community academic partnership in a firefighter community. American Journal of Health Behavior, 37, 721–733. [DOI] [PubMed] [Google Scholar]
- Dutta MJ (2007). Communicating about culture and health: Theorizing culture-centered and cultural sensitivity approaches. Communication Theory, 17, 304–328. [Google Scholar]
- Ehde DM, Dillworth TM, & Turner JA (2014). Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. The American Psychologist, 69, 153–166. [DOI] [PubMed] [Google Scholar]
- Freeman E, Seifer SD, Stupak M, & Martinez LS (2014). Community engagement in the CTSA program: Stakeholder responses from a national Delphi process. Clinical and Translational Science, 7, 191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehlert S, & Coleman R (2010). Using community-based participatory research to ameliorate cancer disparities. Health and Social Work, 35, 302–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelmon S, Blanchard L, Ryan K, & Seifer SD (2012). Building capacity for community-engaged scholarship: Evaluation of the faculty development component of the faculty for the engaged campus initiative. Journal of Higher Education Outreach and Engagement, 16, 21–45. [Google Scholar]
- Goldberg-Freeman C, Kass N, Tracey P, Ross G, Bates-Hopkins B, Purnell L … & Farfel M (2007) You’ve got to understand community”: Community perceptions on “breaking the disconnect” between researchers and communities. Progress in Community Health Partnerships: Research, Education, and Action, 1, 231–240. [DOI] [PubMed] [Google Scholar]
- Greene-Moton E, & Minkler M (2019). Cultural competence or cultural humility?. Moving beyond the debate. Health Promotion Practice, 21, 142–145. 10.1177/1524839919884912 [DOI] [PubMed] [Google Scholar]
- Hart BM, Wicherski M, & Kohout JL (2011). 2010–11: Faculty in U.S. and Canadian graduate departments of psychology. Washington, DC: American Psychological Association Center for Workforce Studies. Available from: http://www.apa.org/workforce/publications/12-grad-study/index.aspx [last accessed May 3, 2019]. [Google Scholar]
- Heinrich J, Heine SJ, & Norenzayan A (2010). The weirdest people in the world? Behavioral and Brain Sciences, 33, 61–135. [DOI] [PubMed] [Google Scholar]
- Horowitz CR, Robinson M, & Seifer S (2009). Community-based participatory research from the margin to the mainstream: Are researchers prepared? Circulation, 119, 2633–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsberger M, McGinnis P, Smith J, Beamer BA, & O’Malley J (2014). Elementary school children’s recess schedule and dietary intake at lunch: A community-based participatory research partnership pilot study. BMC Public Health, 14, 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (2003). Who will keep the public healthy: Educating public health professionals for the 21st century. Committee on Educating Public Health Professionals for the (21st Century). Washington, DC. http://www.nap.edu/read/10542/chapter/1#xii [last accessed May 3 2020]. [Google Scholar]
- Institute of Medicine (2013). Leveraging culture to address health inequalities: examples from Native communities - workshop summary. Washington, DC: National Academy of Sciences. Available from: https://pubmed.ncbi.nlm.nih.gov/24830070/ [last accessed May 3 2020]. [PubMed] [Google Scholar]
- Institute of Medicine (2016). A framework for educating health professionals to address the social determinants of health. Washington, DC: National Academy of Sciences. Available from: https://www.nap.edu/catalog/21923/a-framework-for-educating-health-professionals-to-address-the-social-determinants-of-health [last accessed May 3 2019]. [PubMed] [Google Scholar]
- Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R, … & Burris A (2010). Community-based participatory research: A capacity-building approach for policy advocacy aimed at eliminating health disparities. American Journal of Public Health, 100, 2094–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Parker EA, Rowe Z, Salvatore A, Minkler M, López J, … & Halstead S (2005). Community-based participatory research: Lessons learned from the Centers for Children’s Environmental Health and Disease Prevention Research. Environmental Health Perspectives, 113, 1463–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacquez F, Vaughn LM, & Wagner E (2013). Youth as partners, participants or passive recipients: A review of children and adolescents in community-based participatory research (CBPR). American Journal of Community Psychology, 51, 176–189. [DOI] [PubMed] [Google Scholar]
- Jones L, & Wells K (2007). Strategies for academic and clinician engagement in community-participatory partnered research. JAMA, 297, 407–410. [DOI] [PubMed] [Google Scholar]
- Kagawa Singer M, Dressler W, & George S, & NIH Expert Panel (2016). Culture: The missing link in health research. Social Science and Medicine, 170, 237–246. [DOI] [PubMed] [Google Scholar]
- Katz JR, Martinez T, & Paul R (2011). Community-based participatory research and American Indian/Alaska Native nurse practitioners: A partnership to promote adolescent health. Journal of the American Academy of Nurse Practitioners, 23, 298–304. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Gaskin DJ, & Trujillo AJ (2011). Segregated spaces, risky places: The effects of segregation on race inequalities. Washington, DC: Joint Center of Political and Economic Studies. [Google Scholar]
- Leviton L, & Green L (2018). Community-based participatory research in government and philanthropy. In Wallerstein N, Duran B, Oetzel J & Minkler M (Eds.), Community-based participatory research for health: Advancing social and health equity (3rd edn, pp. 363–368). San Francisco: Jossey-Bass. [Google Scholar]
- Michener L, Cook J, Ahmed SM, Yonas MA, Coyne-Beasley T, & Aguilar-Gaxiola S (2012). Aligning the goals of community-engaged research: Why and how academic health centers can successfully engage with communities to improve health. Academic Medicine, 87, 285–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Salvatore AL, Chang C, Gaydos M, Liu SS, Lee PT, … & Krause N (2014). Wage theft as a neglected public health problem: An overview and case study from San Francisco’s Chinatown District. American Journal of Public Health, 104, 1010–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morello-Frosch R, Brown P, & Brody JG (2018). Democratizing ethical oversight of research through CBPR. In Wallerstein NB, Duran B, Oetzel J & Minkler M (Eds.), Community-based participatory research for health: Advancing social and health equity (3rd edn, pp. 215–226). San Francisco: Jossey-Bass. [Google Scholar]
- Murray M, & Poland B (2006). Health psychology and social action. Journal of Health Psychology, 11, 379–384. [DOI] [PubMed] [Google Scholar]
- Nieweglowski K, Corrigan PW, Tyas T, Tooley A, Dubke R, Lara J, … & Addiction Stigma Research Team (2018). Exploring the public stigma of substance use disorder through community-based participatory research. Addiction Research and Theory, 26, 323–329. [Google Scholar]
- Nyden P (2003). Academic incentives for faculty participation in community-based participatory research. Journal of General Internal Medicine, 18, 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, & Thomas J (2015). The effectiveness of community engagement in public health interventions for disadvantaged groups: A meta-analysis. BMC Public Health, 15, 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oetzel JG, Wallerstein N, Duran B, Sanchez-Youngman S, Nguyen T, Woo K, … & Alegria M (2018). Impact of participatory health research: A test of the community-based participatory research conceptual model. BioMed Research International, 10.1155/2018/7281405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oetzel JG, Zhou C, Duran B, Pearson C, Magarati M, Lucero J, … & Villegas M (2015). Establishing the psychometric properties of constructs in a community-based participatory research conceptual model. American Journal of Health Promotion, 29, e188–e202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz K, Shea J, Nash L, Oetzel J, Garoutte J, Sanchez-Youngman S, & Wallerstein N (2020). Partnerships, processes, and outcomes: A health equity-focused scoping meta-review of community-engaged scholarship. Annual Review of Public Health, 41, 177–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker P, Holland D, Dennison J, Smith SH, & Jackson M (2018). Decolonizing the academy: Lessons from the graduate certificate in participatory research at The University of North Carolina at Chapel Hill. Qualitative Inquiry, 24, 464–477. [Google Scholar]
- Patel AI, Bogart LM, Uyeda KE, Martinez H, Knizewski R, Ryan GW, & Schuster MA (2009). School site visits for community-based participatory research on healthy eating. American Journal of Preventive Medicine, 37(6 Suppl 1), S300–S306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen PB (2001). Multiculturalism and the paradigm shift in counseling: Controversies and alternative futures. Canadian Journal of Counseling, 35, 15–25. [Google Scholar]
- Prilleltensky I (2001). Value-based praxis in community psychology: Moving toward social justice and social action. American Journal of Community Psychology, 29, 747–778. [DOI] [PubMed] [Google Scholar]
- Rhodes SD, Malow RM, & Jolly C (2010). Community-based participatory research: A new and not-so-new approach to HIV/AIDS prevention, care, and treatment. AIDS Education and Prevention, 22, 173–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez Espinosa P, Gil-Kashiwabara E, Clifasefi SM, & Collins SE (2020). Community-based participatory research in psychology: Theory, research, and practice. Half-day continuing education workshop to be presented at the American Psychological Association Annual Meeting, August 2020, Washington, DC. [Google Scholar]
- Ross LF, Loup A, Nelson RM, Botkin JR, Kost R, Smith GR, & Gehlert S (2010). The challenges of collaboration for academic and community partners in a research partnership: Points to consider. Journal of Empirical Research on Human Research Ethics: JERHRE, 5, 19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandoval JA, Lucero J, Oetzel J, Avila M, Belone L, Mau M, … & Wallerstein N (2012). Process and outcome constructs for evaluating community-based participatory research projects: A matrix of existing measures. Health Education Research, 27, 680–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifer SD, Blanchard LW, Jordan C, Gelmon S, & McGinley P (2012). Faculty for the Engaged Campus: Advancing community-engaged careers in the academy. Journal of Higher Education Outreach and Engagement, 16, 5–20. [Google Scholar]
- Smikowski J, Dewane S, Johnson ME, Brems C, Bruss C, & Roberts LW (2009). Community-based participatory research for improved mental health. Ethics & Behavior, 19, 461–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears Johnson CR, Kraemer Diaz AE, & Arcury TA (2016). Participation levels in 25 Community-based participatory research projects. Health Education Research, 31, 577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speer PW, & Hughey J (1995). Community organizing: An ecological route to empowerment and power. American Journal of Community Psychology, 23, 729–748. [DOI] [PubMed] [Google Scholar]
- Stacciarini J-M-R, Shattell MM, Coady M, & Wiens B (2011). Review: Community-based participatory research approach to address mental health in minority populations. Community Mental Health Journal, 47, 489–497. [DOI] [PubMed] [Google Scholar]
- Sue DW (2001). Multidimensional facets of cultural competence. The Counseling Psychologist, 29, 790–821. [Google Scholar]
- Sue S, Zane N, Nagayama Hall GC, & Berger LK (2009). The case for cultural competency in psychotherapeutic interventions. Annual Review of Psychology, 60, 525–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suinn RM, & Borrayo EA (2008). The ethnicity gap: The past, present, and future. Professional Psychology: Research and Practice, 39, 646–651. [Google Scholar]
- Census Bureau US (2015). Projections of the size and composition of the U.S. population: 2014 to 2060. Available from: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf [last accessed January 20 2019] [Google Scholar]
- Venner KL, Donovan DM, Campbell ANC, Wendt DC, Rieckmann T, Radin SM, … & Rosa CL (2018). Future directions for medication assisted treatment for opioid use disorder with American Indian/Alaska Natives. Addictive Behaviors, 86, 111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viets VL, Baca C, Verney SP, Venner K, Parker T, & Wallerstein N (2009). Reducing health disparities through a culturally centered mentorship program for minority faculty: The southwest addictions research group (SARG) experience. Academic Medicine, 84, 1118–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein NB, & Duran B (2006). Using community-based participatory research to address health disparities. Health Promotion Practice, 7, 312–323. [DOI] [PubMed] [Google Scholar]
- Wallerstein NB, & Duran B (2010). Community-based participatory research contributions to intervention research: The intersection of science and practice to improve health equity. American Journal of Public Health, 100, S40–S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein NB, Duran B, Oetzel J, & Minkler M (2018). Community-based participatory research for health: Advancing social and health equity (3rd edn). San Francisco: Jossey-Bass. [Google Scholar]
- Wallerstein N, Oetzel JG, Duran B, Magarati M, Pearson C, Belone L, … & Dutta MJ (2019). Culture-centeredness in community-based participatory research: Contributions to health education intervention research. Health Education Research, 34, 372–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KL, Stately A, Evans-Campbell T, Simoni JM, Duran B, Schultz K, … & Guerrero D (2008). "Indigenist" collaborative research efforts in Native American communities. In Stiffman A (Ed.), The nitty-gritty of managing field research. New York: Oxford University Press. [Google Scholar]
- Whitehead M (2007). A typology of actions to tackle social inequalities in health. Journal of Epidemiology and Community Health, 61, 473–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Mousseau A, Parker M, Rasmus S, & Allen J (2018). Promising practices for promoting health equity through rigorous intervention science with indigenous communities. Prevention Science, 21, 5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]