Abstract
The case of 21-year-old man with an asthma history from childhood presenting severe respiratory distress associated with a right lower thoracic pain has been studied. The non–contrast Computed Tomography (CT)-chest scan showed a basal ground-glass opacity (GGO) of the right lung leading to suspicion of COVID-19 pneumonia. However, the molecular Reverse transcription polymerase chain reaction test and blood serology were negative while laboratory analyses revealed high levels of D-dimers (D-D). In addition, 2 repeated COVID-19 tests were negative. A thoracic CT angiography was disclosed due to the persistence of pain at the lower right thoracic side and hemoptysis that shows a bilateral distal pulmonary embolism with a right-sided basal subsegmental ischemia. We discuss a fortuitous discovery of pulmonary embolism associated with peripheral basal ground-glass opacities similar to radiological manifestations of SARS-CoV-2 pneumonia.
Keywords: Artery embolism, CT chest angiography, Covid-19, Ground-glass opacity, Pneumonia, Chest pain
Introduction
Acute pulmonary embolism (APE) is the most serious clinical presentation of venous thrombo-embolism (VTE) with fatal pulmonary embolism (PE) being a common cause of sudden death. PE is the third most frequent cardiovascular disease after acute myocardial infarction (AMI) and stroke, with an annual incidence of 1-2 per 1,000 people (100-200 per 100,000 inhabitants) [1]. APE is characterized by numerous clinical manifestations which are the result of a complex interplay between different organs. The symptoms are therefore various and part of a complex clinical picture [1]. For these reasons, despite being common, APE often remains elusive as a diagnosis and practitioners should maintain a high level of suspicion for this disease in high-risk patients [2]. Pulmonary Computed Tomography angiography (CTA) is the imaging modality of choice in suspected APE due to the technical advancements along with the immediate and widespread availability of this test. The CTA is well established as a fast and reliable method to exclude or diagnose PE [3].
It has been shown that there is a causal link between APE and the occurrence of ground glass opacity (GGO) defined as hazy increased opacity of the lung, with preservation of bronchial, and vascular margins [4]. This radiological finding is also common in SARS-CoV-2 pneumonia’ [5] which may be confusing during this pandemic period. The scope of this report is to investigate if the presence of ground-glass opacities in COVID-19 pneumonia doesn't omit other causes of ground-glass opacities.
Case presentation
The case of a 21-year-old man with asthma and allergies history since childhood. This case showed no indication of drug intoxication and was admitted to our institution for brutal dyspnea with lower pain in the right side associated with hemoptysis of mild abundance and fever. We suspected a SARS-CoV-2 pulmonary infection considering the clinical presentation and the actual pandemic. Thereafter, he was admitted to an isolation ward while laboratory and radiological investigations were performed. During the few months before and after hospitalization, the patient had no manifestations of COVID-19 pneumonia.
A laboratory report showed a high level of leukocytosis at 14000/mm3[4000-11000/ mm3]* 23% of which were eosinophils [0.02-0.63/ mm3]*, a high level of D-Dimers (5000 u/mL) [≤500 u/mL]*, thrombocytopenia (124000/mm) [150000-400000/ mm3]*, a high level of blood ferritinemia (702 ng/mL) [30-300ng/mL]*, and C-reactive-protein (90 mg/L) [≤8 u/mL]*.
The molecular RT-PCR test for COVID-19, as well as serology, were negative. A CT-chest scan without contrast was performed at the admission. Yet, lower thoracic chest pain, cough, and hemoptysis were persistent, therefore a CT chest angiography was realized after 24 hours. A Doppler Ultrasound of the lower limbs and echocardiography were realized during the patient's hospitalization. A non–enhanced chest CT scan has shown a peripheral sub-pleural ground-glass opacity in the right lower segment (Fig. 1). No other anomalies were found. Accordingly, the initial diagnosis of COVID-19 pneumonia was held.
Fig. 1.
Axial (A) and coronal (B) section lung window of CT- chest angiography showing a peripheral subpleural ground-glass opacity in the lower segment of right lung.
With the progressive intensive pain of the right lung and hemoptysis and the fact that the molecular RT-PCR test and serology for COVID-19 were negative, CT chest angiography showed total occlusion of the posterior branch of the right inferior pulmonary artery and partial occlusion of the inferior branch of the left pulmonary artery (Fig. 2). We also noticed a condensation and extension of the pre-existing ground-glass opacity associated with low pleural effusion (Fig. 3). The diagnosis of bilateral peripheral pulmonary embolism causing a right posterobasal pulmonary infarction was retained. A curative dose of anticoagulants and corticosteroids was introduced. The patient did not show manifestations of COVID-19 infection during the hospitalization and a 1 month follow-up. Two Repeated COVID-19 tests were negative. The thoracic CT angiography after 1 month showed recanalization of the pulmonary artery that was initially occluded and a decrease of right basal condensation (Fig. 4).
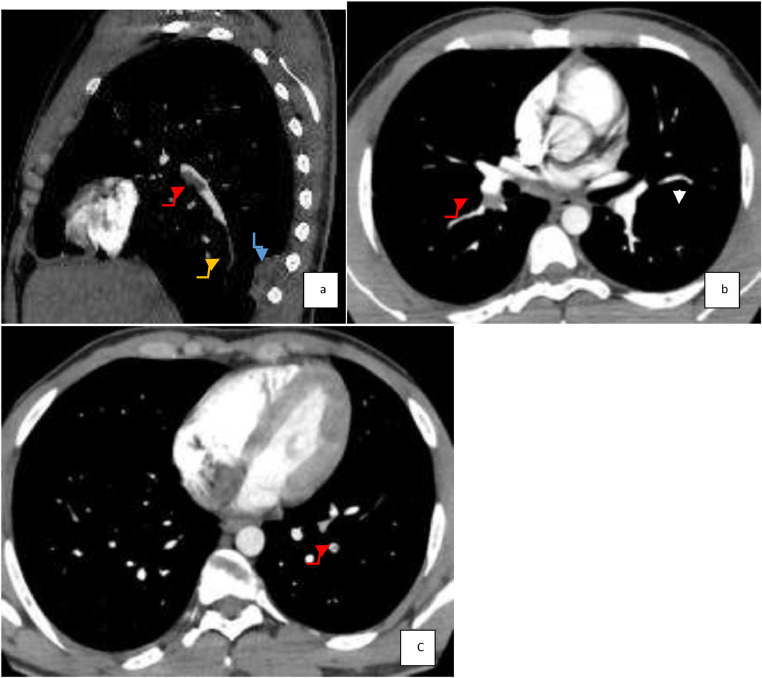
Fig. 2.
Sagittal (A) and axial (B,C) reconstructions angiography CT images shows a total stenosis of the posterior branch of the right inferior pulmonary artery (yellow arrow) with ischemia of lung (blue arrow) and a total occlusion of the inferior branch of the right and left pulmonary artery (C) (red arrow) (Color version of the figure is available online.)
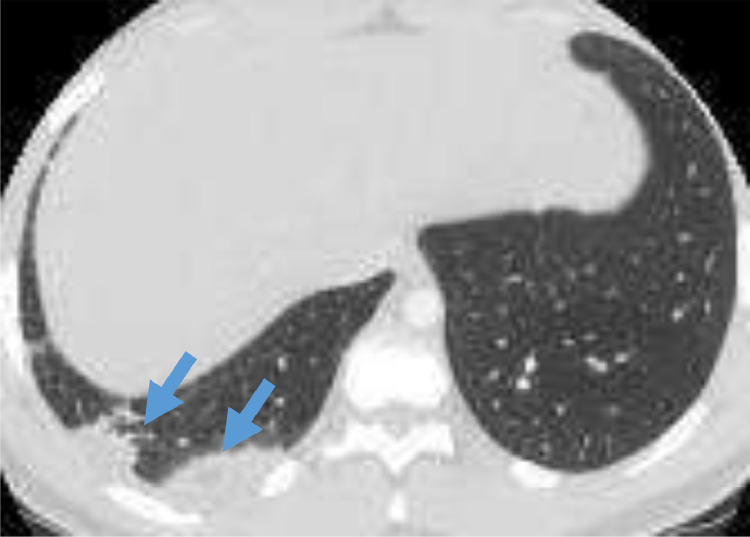
Fig. 3.
Axial CT angiography of lung window showing condensation and extension of the pre-existing ground-glass opacity of the lower segment of right lung (blue arrows) (Color version of the figure is available online.)
Fig. 4.
Sagittal Maximum intensity projection reconstruction of CT chest images (A) showing partial repermeabilization of the inferior right pulmonary artery (yellow arrow). Axial CT angiography section mediastinal window (B) showing decrease of the condensation of lower segment of right lung 1 month late (white arrow) (Color version of the figure is available online.)
Discussion
The criteria for suspicion of a viral acute respiratory syndrome due to COVID-19 was established by the World Health Organization (WHO). The suspicion is based on anamnestic, epidemiologic, biological, and radiological data [6]. This was initially about the virus invasion at the alveolus level which spreads to the interstitium causing more dense condensation [7]. During the pandemic, the no-contrast chest CT scan was used for the diagnosis and mass screening especially for patients who initially had a negative RT-PCR test. Also, it was the first assessment in emergency structures where the results of RT-PCR and serology are late. Indeed, the RT-PCR detection of viral nucleic acid in the airways, presents 94% sensitivity, and 37% specificity [8], while the CT chest scanner presents 91% specificity and a 90% sensitivity [9].
Ground-glass types of alveolar consolidation are no specific and could lead to many etiologies, oedema (of the cardiogenic origin or acute respiratory distress syndrome (ARDS)), hemorrhage (pulmonary trauma, arterial rupture, embolic infarction), inflammation (fibrosis, hypersensitivity, acute or chronic eosinophilia), an attack by toxic inhalation with “:paraquat” or an invasion by tumor cells (broncho-alveolar carcinoma, lymphoma) [10,11].
In the present case, the main differential diagnoses were: Bacterial or viral pneumonia due to COVID-19, alveolar hemorrhage given the context of hemoptysis. Finally, it was an alveolar hemorrhage resulting from an artery embolism.
The unilaterality, uni or multifocal, peripheral ground-glass opacity predominantly in the lower lobes, was described in 93% of subclinical patients, during the first week after the onset of symptoms in COVID-19 [12]. The thrombotic situation is correlated to inflammation caused by SARS-CoV-2. The coagulopathy associated with COVID-19 is different from conventional sepsis [13].
In order not to delay the diagnosis of a pulmonary embolism whatever its origin, performing thoracic CTA in advance remains a real challenge for emergency physicians and radiologists [14]. An advice paper from the European Society of Radiology [15] suggests that contrast-enhanced CT should be more widely used when assessing patients with COVID-19 pneumonia, especially in those with marked elevation of D-dimers. In our case, this recommendation has been applied. All molecular, parasitic, and serologic investigations were strictly normal in our patient with a favorable response after introducing anticoagulant and corticosteroid therapy.
Conclusion
The discovery of ground-glass opacity in a patient with respiratory symptoms, especially in this period of the pandemic, leading to possible COVID-19 pneumonia diagnosis in the early stages, should not omit other causes of ground-glass opacities. A contrast-enhanced CT chest is recommended at the beginning to identify a distal artery embolism before molecular RT-PCR's confirmation. Ground-glass opacities can have many etiologies resulting from interstitium aggression. In our case, it was an alveolar hemorrhage resulting from artery embolism.
[*]: Normal laboratory values
Availability of data and material
Data available within the article.
Code availability
(N/A).
Footnotes
Acknowledgments: This study was not funded.
Competing Interests: The authors declare that they have no conflict of interest.
References
- 1.Morrone D, Morrone V. Acute pulmonary embolism: Focus on the clinical picture. Korean Circ J. 2018;48(5):365–381. doi: 10.4070/kcj.2017.0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morici B. Diagnosis and management of acute pulmonary embolism. JAAPA. 2014;27(4):18–22. doi: 10.1097/01.JAA.0000444729.09046.09. [DOI] [PubMed] [Google Scholar]
- 3.Albrecht MH, Bickford MW, Nance JW, Jr, Zhang L, De Cecco CN, Wichmann JL. State-of-the-art pulmonary CT angiography for acute pulmonary embolism. AJR Am J Roentgenol. 2017;208(3):495–504. doi: 10.2214/AJR.16.17202. [DOI] [PubMed] [Google Scholar]
- 4.Thoma P, Rondelet B, Mélot C, Tack D, Naeije R, Gevenois PA. Acute pulmonary embolism: relationships between ground-glass opacification at thin-section CT and hemodynamics in pigs. Radiology. 2009;250(3):721–729. doi: 10.1148/radiol.2503081134. [DOI] [PubMed] [Google Scholar]
- 5.Kolta MF, Ghonimy MBI. COVID-19 variant radiological findings with high lightening other coronavirus family (SARS and MERS) findings: radiological impact and findings spectrum of corona virus (COVID-19) with comparison to SARS and MERS. Egypt J Radiol Nucl Med. 2020;51(1):172. [Google Scholar]
- 6.World Health Organization website. Novel coronavirus: China. www.who.int/csr/don/12-january 2020-novel-coronavirus-china/en/. Published January 12, 2020. Accessed January 19, 2020.
- 7.Shi Heshui, Han Xiaoyu, Jiang Nanchuan, Cao Yukun, Al walid Osamah, Gu Jin. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. AVRIL. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim H, Hong H, Yoon SH. Diagnostic performance of CT and reverse transcriptase polymerase chain reaction for coronavirus disease 2019: a meta-analysis. Radiology. 2020;296(3):E145–E155. doi: 10.1148/radiol.2020201343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guillaume Herpe, Mathieu Lederlin, Mathieu Naudin, Mickaël Ohana, Kathia Chaumoitre, Jules Gregory. Valérie Vilgrain. Efficacy of chest CT for COVID-19 pneumonia diagnosis in france. Radiology. 2021;298(2):2021. doi: 10.1148/radiol.2020202568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kauczor Hans-Ulrich, Heitmann Kjell, Heussel Claus Peter, Marwede Dirk, Uthmann Thomas, Thelen Manfred. Automatic detection and quantification of ground-glass opacities on high-resolution ct using multiple neural networks: Comparison with a density mask. AJR. 2000;175:5:1329–1334. doi: 10.2214/ajr.175.5.1751329. [DOI] [PubMed] [Google Scholar]
- 11.Kim YT, Jou SS, Lee HS, Gil HW, Yang JO, Lee EY. The area of ground glass opacities of the lungs as a predictive factor in acute paraquat intoxication. J Korean Med Sci. 2009;24(4):636–640. doi: 10.3346/jkms.2009.24.4.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luo Lin, Luo Zhendong, Jia Yizhen, Zhou Cuiping, He Jianlong, Lyu Xinping. CT differential diagnosis of COVID-19 and non-COVID-19 in symptomatic suspects: a practical scoring method. BMC Pulm Med. 2020;20:129. doi: 10.1186/s12890-020-1170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowles L, Platton S, Yartey N, Dave M, Lee K, Hart DP. Lupus anticoagulant and abnormal coagulation tests in patients with Covid-19. N Engl J Med. 2020;16;383(3):288–290. doi: 10.1056/NEJMc2013656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moreira BL, Santana PRP, Zanetti G, Marchiori E. COVID-19 and acute pulmonary embolism: what should be considered to indicate a computed tomography pulmonary angiography scan? Rev Soc Bras Med Trop. 2020;53 doi: 10.1590/0037-8682-0267-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bompard Florian, Monnier Hippolyte, Saab Ines, Tordjman Mickael, Abdoul Hendy, Fournier Laure. Pulmonary embolism in patients with COVID-19 pneumonia. Eur Respir J. 2020;56(1) doi: 10.1183/13993003.01365-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available within the article.