Abstract
Background
Despite nation-wide efforts to reduce health care costs through hospital closures and centralization of services, little is known about the impact of such actions. We conducted this study to determine the effect of a hospital closure in Calgary and the resultant centralization of coronary revascularization procedures from 2 facilities to a single location.
Methods
Administrative data were used to identify patients who underwent coronary artery bypass grafting (CABG), including those who had combined CABG and valve procedures, and patients who underwent percutaneous transluminal angioplasty (PTCA) in the Calgary Regional Health Authority from July 1994 to March 1998. This period represents the 21 months preceding and the 24 months following the March 1996 hospital closure. Measures, including mean number of discharges, length of hospital stay, burden of comorbidity and in-hospital death rates, were compared before and after the hospital closure for CABG and PTCA patients. Multivariate analyses were used to derive risk-adjustment models to control for sociodemographic variables and comorbidity.
Results
The number of patients undergoing CABG was higher in the year following than in the year preceding the hospital closure (51.6 per 100 000 before v. 67.3 per 100 000 after the closure); the same was true for the number of patients undergoing PTCA (129.8 v. 143.6 per 100 000). The burden of comorbidity was significantly higher after than before the closure, both for CABG patients (comorbidity index 1.3 before v. 1.5 after closure, p < 0.001) and for PTCA patients (comorbidity index 1.0 before v. 1.1 after, p = 0.04). After adjustment for comorbidity, the mean length of hospital stay was significantly lower after than before the closure for CABG patients (by 1.3 days) and for PTCA patients (by 1.0 days). The adjusted rates of death were slightly lower after than before the closure in the CABG group. The adjusted rates of death or CABG in the PTCA group did not differ significantly between the 2 periods.
Interpretation
Hospital closure and the centralization of coronary revascularization procedures in Calgary was associated with increased population rates of procedures being performed, on sicker patients, with shorter hospital stays, and, for CABG patients, a trend toward more favourable short-term outcomes. Our findings indicate that controversial changes to the structure of the health care system can occur without loss of efficiency and reduction in quality of care.
Increasing health care costs and a political movement toward balancing the budget have contributed to a nation-wide emphasis on health care restructuring and a centralization of tertiary care services. In Alberta the regionalization and downsizing of the acute care sector has had a direct impact on the Calgary Regional Health Authority (CRHA), with the closure of 4 of its 8 large city hospitals and centralization of coronary revascularization procedures from 2 facilities to a single location. The centralization of cardiac procedures required both facility and staffing changes at the single location, including the addition of 2 new coronary catheterization laboratories and an increased number of postoperative ward beds and monitored step-down beds.
Critics of the hospital closures raised concerns about the ability of the surviving hospitals to accommodate and manage patients adequately and effectively. Public concerns were expressed over access and the possible deterioration of health outcomes given the increased volume of patients,1 concerns substantiated by previous research.2,3
In this article we report on the centralization “case study” in Calgary and focus on the closure of one hospital and the resultant amalgamation of coronary revascularization procedures from 2 facilities to a single facility. Our specific objectives were to determine, for coronary artery bypass grafting (CABG) and percutaneous transluminal coronary angioplasty (PTCA), if there was an association between the hospital closure and the number of discharges per month, burden of comorbidity, length of hospital stay and in-hospital mortality, by comparing periods before and after the hospital closure. We also compared population rates for myocardial infarction, CABG and PTCA before and after the closure.
Methods
We used CRHA administrative hospital discharge data from July 1994 to March 1998, a period of 21 months preceding and 24 months following the official March 1996 closure of the hospital. CABG cases were identified by screening all hospital discharge records for ICD-9-CM4 procedure codes representing CABG surgery (36.10–36.19); this included patients undergoing combined CABG and valve procedures. PTCA cases were identified by screening for procedure codes 36.01–36.03, 36.05, 36.06 and 36.09.
The number of discharges per month for CABG and PTCA was obtained. We determined a summary estimate for the number of discharges per month before the closure by calculating the mean number of discharges per month for the 21 months preceding the closure. The mean number of discharges per month after the closure was determined in the same manner.
We calculated age- and sex-standardized population rates for CABG and PTCA in the year before and the year after the closure, using a direct method of standardization, with the 1996 CRHA population as a standard. For the years 1995 and 1997 the Alberta Health Registry was used to determine the CRHA population at the mid-point of the fiscal year (Sept. 30) as the denominator for the rates. These adjusted rates enable comparison of rates in one year relative to another, after the effects of changes in population structure have been removed.
We measured burden of comorbidity for CABG and PTCA patients using the comorbidity index of Charlson and associates.5 Deyo and collaborators6 have since identified corresponding ICD-9-CM codes to define these conditions, which enables use of the comorbidity index with administrative databases.6 The comorbidity index allowed us to identify the 17 variables mapped by Deyo and collaborators (e.g., myocardial infarction, diabetes mellitus and chronic pulmonary disease). We considered a condition to be present only when the “diagnosis type” indicator (in the hospital administrative data) was consistent with diagnoses that were present before CABG or PTCA.
Hospital resource use was assessed according to length of stay (LOS) in hospital. We determined summary estimates for LOS before and after the hospital closure by calculating the mean LOS for the 2 periods.
Mortality is a frequently used measure of quality of hospital care.7 For patients undergoing CABG, we calculated the crude and risk-adjusted in-hospital mortality before and after the closure. For patients undergoing PTCA we used a combined outcome of in-hospital mortality or CABG, or both, because CABG after PTCA is also an indicator of a poor outcome.
We compared the clinical characteristics of patients before and after the closure using the χ2 test. The characteristics evaluated included the sociodemographic variables age and sex, the 17 variables defined from the comorbidity index, other severity-of-illness variables identified from the ICD-9-CM diagnosis codes8 (unstable angina, hypertension, prior CABG, prior PTCA, ventricular aneurysm, and combined CABG and valve procedure) and the admission status (urgent v. elective, defined dichotomously from the “admission type” field in the hospital administrative data). We compared continuous measures before and after the closure using Student's t-test. The independent association between hospital closure and mean LOS was evaluated with the use of multiple linear regression analysis to control for other predictors of LOS such as increasing age and comorbidity; the dependent variable was LOS measured in days, and the unit of analysis was individual CABG or PTCA cases. Logistic regression analysis was used to develop a risk-adjustment model for the calculation of risk-adjusted death rates among CABG patients, as previously described.8 We used the risk-adjustment model to calculate the predicted probability of in-hospital death for each patient who underwent CABG before or after the hospital closure. We then calculated the average of these predicted probabilities of death during the 2 study periods to yield an expected death rate (E). The observed death rate (O) was then divided by E to generate an O/E ratio for each study period. To calculate the risk-adjusted death rates, we then multiplied the period-specific O/E ratios by the overall death rate for the entire 45-month study period. Similar analyses were undertaken for each patient who underwent PTCA, except in this instance the outcome was death or CABG, or both.
Results
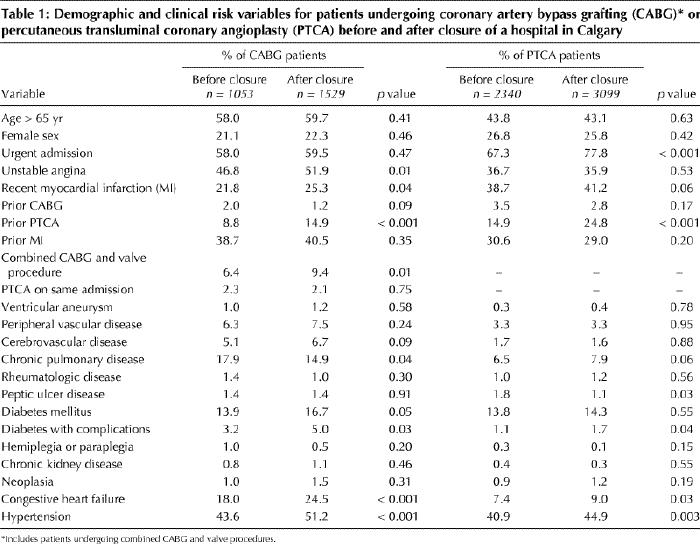
The prevalence of demographic and clinical risk variables before and after the hospital closure in the 2 patient groups are outlined in Table 1. The age and sex distribution of the patients were similar for these 2 study periods. Compared with the period before the closure, CABG patients after the closure were significantly more likely to be admitted with unstable angina or a recent myocardial infarction and to have had a prior PTCA; the PTCA patients after the closure were significantly more likely to be admitted urgently and to have had a prior PTCA.
Table 1
There was a significant increase in the mean number of discharges per month after the closure in the CABG group (from 50.8 to 63.7, p < 0.001) and in the PTCA group (from 111.4 to 129.1, p < 0.001).
The population rates (per 100 000) in the year following the closure, compared with the year before the closure, increased for CABG (51.6 in 1995 v. 67.3 in 1997) and for PTCA (129.8 in 1995 v. 143.6 in 1997) (Fig. 1). For comparison we included the rates for myocardial infarction for the same periods. Although there was a slight increase, the myocardial infarction rates were more stable, at 158.2 in 1995 and 164.3 in 1997.
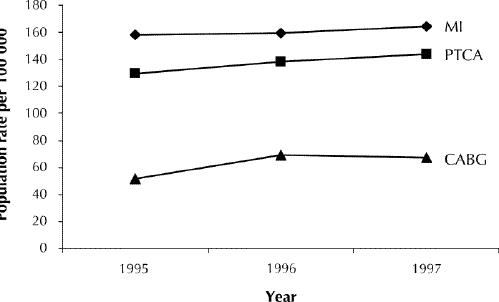
Fig. 1: Population rates (per 100 000) of myocardial infarction (MI), percutaneous transluminal coronary angioplasty (PTCA) and coronary artery bypass grafting (CABG) during the year before and the year after the closure of a Calgary hospital in March 1996.
The burden of comorbidity was slightly higher after than before the hospital closure in both the CABG and PTCA groups. For the CABG patients, the comorbidity index score was 1.3 before and 1.5 after the closure (p < 0.001). The corresponding scores for PTCA patients were 1.0 and 1.1 (p = 0.04).
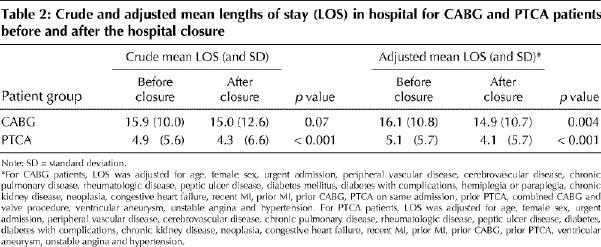
In terms of hospital resource use, the mean LOS in hospital, after adjustment for comorbidity, was significantly lower after than before the closure in the 2 patient groups (Table 2).
Table 2
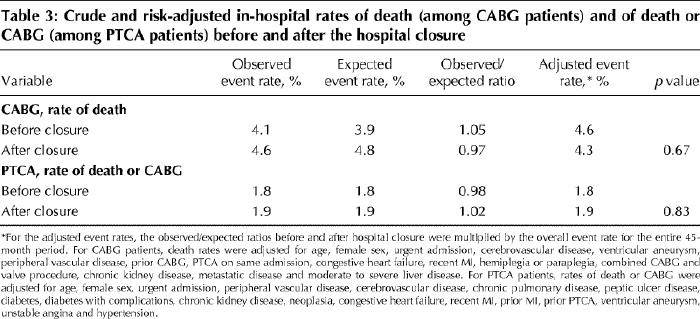
Rates of death (among the CABG patients) and rates of death or CABG (among the PTCA patients) are presented in Table 3. Among the CABG patients the crude death rates were 4.1% before and 4.6% after the closure. After adjustment for the generally higher severity of illness for patients after the closure, the death rate decreased, from 4.6% before to 4.3% after the closure (p = 0.67). The same trend was not seen, however, among the PTCA patients, who had almost identical crude and adjusted rates of death or CABG of 1.8% before and 1.9% after the closure. The increase after the closure in the expected death rate among the CABG patients (from 3.9% to 4.8%) and the expected rate of death or CABG among the PTCA patients (from 1.8% to 1.9%) suggests that patients selected for CABG and PTCA have become sicker since the hospital closure, and yet, for CABG, there was a trend toward more favourable adjusted short-term outcomes.
Table 3
Interpretation
In this “case study” of hospital closure and centralization of coronary revascularization procedures, we found that an increased number of procedures were performed after the closure, on sicker patients, with shorter hospital stays. For CABG patients, we also found a statistically nonsignificant decrease in the rate of in-hospital deaths.
A limited amount of research has examined hospital closures, and what is available has tended to focus on the reasons for closure or the perceived impact on individuals, rather than the outcomes of the closure.2,3,9,10 Brownell and Roos11 recently reported on the Winnipeg experience of downsizing, with 22.6% of acute care beds closed between 1992 and 1995. Besides the Winnipeg experience, our study is one of the few reports available that has monitored the effects of downsizing on access and quality of care.
Despite public concern regarding access to health care services, we found a significant increase in the mean number of discharges per month after the hospital closure in both the CABG and PTCA groups. For CABG, this is consistent with national rates, which reflect a steady increase in the number of CABG procedures performed per year.12 This paradox of a reduction in the number of beds available and yet an increase in the mean number of discharges for CABG and PTCA may be explained in part by a decrease in LOS. Similar observations were made in Winnipeg after downsizing, with a decline in mean LOS for surgical, obstetric and medical patients.13
Centralization of cardiac revascularization procedures in Calgary has occurred without negative effects on quality of care, as measured by in-hospital rates of death. The PTCA patients experienced a slight, nonsignificant increase in the rate of death or CABG, which probably relates to the increased use of primary (i.e., immediate) PTCA in patients presenting with acute myocardial infarction. Meanwhile, the CABG patients in our study experienced a statistically nonsignificant, but nonetheless notable, decrease in the adjusted death rate. In the Winnipeg experience, Brownell and associates13 also found no significant increase in death rates within 30 days after discharge for 3 common conditions: acute myocardial infarction, hip fracture and cancer surgery.
The slight decline in adjusted death rates among the CABG patients after the hospital closure may be a result of the centralization of services and may be explained in part by the volume–outcome phenomenon. Lower death rates have been associated with higher volumes of procedures in studies of CABG14,15 and PTCA.16,17,18,19,20 The association between volume and outcome may be due to several factors, including improved technique from greater experience, selective referral to higher-volume centres and treatment of sicker patients at low-volume hospitals. More important, it may be the processes of care within these facilities that lead to optimal outcomes, rather than the volume per se, with volume acting merely as a surrogate for quality of care.
Several potential limitations should be considered in the interpretation of our results. First, we used administrative data as the source of information for risk adjustment; these data may lack the detail needed to assess severity that prospectively collected clinical data provide. The data source also lacked detail to account for changes in medical practice, including the use of stenting and antiplatelet agents for PTCA, which may influence LOS and clinical outcomes. Second, we lacked information on geographic equity of access, particularly given the relocation of revascularization services to a more peripherally located hospital in Calgary. Third, our data source limited our assessment of mortality to deaths that occurred in hospital only, reflecting short-term outcomes. In addition, we limited our assessment to one area of health care, often perceived as high profile and well funded; the influence of hospital closure and restructuring on other areas may have been different. We were unable to assess the impact of the hospital closure, and the observed decrease in LOS, on readmission rates and longer-term mortality. Brownell and Roos,11 however, reported no significant increase in readmission rates for 13 common conditions following downsizing in Winnipeg. Finally, although restructuring of health care services occurred throughout Alberta, we limited our study to the evaluation of cardiac services in an urban centre. Our results are not generalizable to the effects of hospital closures in rural areas.
Despite these limitations, our study provides useful and nationally relevant information. The experience of hospital closure and centralization of revascularization procedures in Calgary was one of success. We found that, for revascularization, the restructuring was associated with increased population rates of procedures, performed on sicker patients, with shorter stays in hospital, and, for CABG patients, a trend toward more favourable short-term outcomes. Similar restructuring measures are occurring both nationally21 and internationally.22 Our findings indicate that such controversial changes can occur without negatively influencing the delivery of health care services.
Footnotes
This article has been peer reviewed.
Acknowledgements: Dr. Ghali is supported by a Population Health Investigator Award from the Alberta Heritage Foundation for Medical Research and holds a Government of Canada Research Chair in health services research. The project was funded by an operating grant from the Calgary Regional Health Authority (Ralph Coombs Health Research Fund).
Competing interests: None declared.
Reprint requests to: Dr. William A. Ghali, University of Alberta Health Sciences Centre, 3330 Hospital Dr. NW, Calgary AB T2N 4N1; fax (403) 283-6151; wghali@ucalgary.ca
References
- 1.Rutherford B. Health cuts too much. Calgary Herald 1995 Apr 23:A7.
- 2.Bindman AB, Keane D, Lurie N. A public hospital closes: impact on patients' access to care and health status. JAMA 1990;264:2899-904. [DOI] [PubMed]
- 3.Muus KJ, Ludtke RL, Gibbens B. Community perceptions of rural hospital closure. J Community Health 1995;20:65-73. [DOI] [PubMed]
- 4.The international classification of diseases, 9th revision, clinical modification. 4th ed. New York: McGraw-Hill; 1995.
- 5.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. [DOI] [PubMed]
- 6.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613-9. [DOI] [PubMed]
- 7.Hannan EL, Kilburn H Jr, Racz M, Shields E, Chassin MR. Improving the outcomes of coronary artery bypass surgery in New York State. JAMA 1994; 271:761-6. [PubMed]
- 8.Ghali WA, Quan H, Brant R. Coronary artery bypass grafting in Canada: national and provincial mortality trends, 1992–1995. CMAJ 1998;159(1):25-31. Abstract available: www.cma.ca/cmaj/vol-159/issue-1/0025.htm [PMC free article] [PubMed]
- 9.Hernandez SR, Kaluzny AD. Hospital closure: a review of current and proposed research. Health Serv Res 1983;18:419-35. [PMC free article] [PubMed]
- 10.James AM. Closing rural hospitals in Saskatchewan: On the road to wellness? Soc Sci Med 1999;49:1021-34. [DOI] [PubMed]
- 11.Brownell MD, Roos NP. Monitoring the Winnipeg hospital system: the update report 1993/1994. Winnipeg: Manitoba Centre for Health Policy and Evaluation; 1996.
- 12.Ghali WA, Quan H, Brant R. CABG in Canada [letter]. CMAJ 1999;161(8): 941. Available: www.cma.ca/cmaj/vol-161/issue-8/letters-8.htm#1 [PMC free article] [PubMed]
- 13.Brownell MD, Roos NP, Burchill C. Monitoring the impact of hospital downsizing on access to care and quality of care. Med Care 1999;37(6 Suppl):JS135-50. [DOI] [PubMed]
- 14.Hannan EL, O'Donnell JF, Kilburn H Jr, Hernard HR, Yazici A. Investigation of the relationship between volume and mortality for surgical procedures performed in New York State hospitals. JAMA 1989;262:503-10. [PubMed]
- 15.Peterson ED, DeLong ER, Jollis JG, Mulbaier LH, Mark DB. The effect of New York's bypass surgery provider profiling on access to care and patient outcomes in the elderly. J Am Coll Cardiol 1998;32:993-9. [DOI] [PubMed]
- 16.Canto JG, Every NR, Magid DJ, Rogers WJ, Malmgren JA, Frederick PD, et al. The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. N Engl J Med 2000;342:1573-80. [DOI] [PubMed]
- 17.Ritchie JL, Maynard C, Chapko MK, Every NR, Martin DC. Association between percutaneous transluminal coronary angioplasty volumes and outcomes in the Healthcare Costs and Utilization Project 1993–1994. Am J Cardiol 1999; 83:493-7. [DOI] [PubMed]
- 18.Hannan EL, Racz M, Ryan TJ, McCallister BD, Johnson LW, Arani DT, et al. Coronary angioplasty volume–outcome relationships for hospitals and cardiologists. JAMA 1997;277:892-8. [PubMed]
- 19.Jollis JG, Peterson ED, DeLong ER, Mark DB, Collins SR, Muhlbaier LH, et al. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med 1994;331:1625-9. [DOI] [PubMed]
- 20.Kimmel SE, Berlin JA, Laskey WK. The relationship between coronary angioplasty procedure volume and major complications. JAMA 1995;274:1137-42. [PubMed]
- 21.Anderson GM. Hospital restructuring and the epidemiology of hospital utilization: recent experience in Ontario. Med Care 1997;35(10 Suppl):OS93-101. [DOI] [PubMed]
- 22.Harrison AJ. Hospitals in England: impact of the 1990 National Health Service reforms. Med Care 1997;35(10 Suppl):OS50-61. [DOI] [PubMed]


