Abstract
Objectives
To examine the extent to which the racial and ethnic composition of nursing homes (NHs) and their communities affects the likelihood of COVID-19 cases and death in NHs, and whether and how the relationship between NH characteristics and COVID-19 cases and death varies with the racial and ethnic composition of the community in which an NH is located.
Methods and Design
Centers for Medicare & Medicare Services Nursing Home COVID-19 data were linked with other NH- or community-level data (eg, Certification and Survey Provider Enhanced Reporting, Minimum Data Set, Nursing Home Compare, and the American Community Survey). Setting and Participants: NHs with more than 30 occupied beds (N=13,123) with weekly reported NH COVID-19 records between the weeks of June 7, 2020, and August 23, 2020. Measurements and model: Weekly indicators of any new COVID-19 cases and any new deaths (outcome variables) were regressed on the percentage of black and Hispanic residents in an NH, stratified by the percentage of blacks and Hispanics in the community in which the NH was located. A set of linear probability models with NH random effects and robust standard errors were estimated, accounting for other covariates.
Results
The racial and ethnic composition of NHs and their communities were both associated with the likelihood of having COVID-19 cases and death in NHs. The racial and ethnic composition of the community played an independent role in the likelihood of COVID-19 cases and death in NHs, even after accounting for the COVID-19 infection rate in the community (ie, daily cases per 1000 people in the county). Moreover, the racial and ethnic composition of a community modified the relationship between NH characteristics (eg, staffing) and the likelihoods of COVID-19 cases and death.
Conclusions and Implications
To curb the COVID-19 outbreaks in NHs and protect vulnerable populations, efforts may be especially needed in communities with a higher concentration of racial and ethnic minorities. Efforts may also be needed to reduce structural racism and address social risk factors to improve quality of care and population health in communities of color.
Keywords: COVID-19, nursing home, racial and ethnic differences
Nursing home (NH) residents have been disproportionally affected by the COVID-19 pandemic.1, 2, 3 Racial and ethnic minority NH residents may even have exacerbated risks of COVID-19 infection and death. There have been longstanding concerns that racial and ethnic minority NH residents experience lower quality of care than their white counterparts.4, 5, 6 Indeed, recent studies have suggested that NHs with a higher proportion of racial and ethnic minorities had higher rates of COVID-19 infection and related death.7, 8, 9, 10, 11, 12 However, current studies on NH COVID-19 outbreaks offer mixed findings on the relationship between NH characteristics, such as NH staffing and its overall quality rating, and COVID-19 outbreaks.9 , 10 , 13, 14, 15 For example, some studies found that more registered nurse (RN) hours per resident day12 and lower star rating16 were related to higher likelihood of COVID-19 cases, whereas other studies found a negative relationship between RN hours and COVID-19 cases,14 and no consistent relationship between NH star rating and COVID infection.17 The inconsistency is partly due to the different populations and study periods in these studies. In addition, some studies used the early NH COVID-19 data reported by the Centers for Medicare & Medicaid Services (CMS),7 which may be less accurate as NHs may have needed time to become familiar with the reporting process.18 Thus, more evidence is needed.
In addition to the relationship between NH racial and ethnic composition and COVID-19 outbreaks, communities where an NH is located were found to also contribute to the outbreak of COVID-19 in NHs.15 Although it has been suggested that communities with a higher proportion of racial and ethnic minorities have a higher rate of COVID-19 infection,19 and community transmission is related to COVID-19 outbreak in NHs,20 it is unknown whether and how community characteristics, other than COVID-19 infection rate, affect COVID-19 outbreak in NHs and how the racial and ethnic composition of the community impacts the relationship of NH factors with COVID-19 outbreaks in NHs. For example, communities with a higher percentage of racial and ethnic minorities are more likely to be economically deprived.21 NHs in these communities may not have adequate infection control, supplies, or protocols and may be less prepared for the pandemic. In addition, NHs in high-minority communities may have amplified risks of outbreak of COVID-19 as their staffing, especially direct care workers, and delivery personnel may be more likely to be exposed to COVID-19.
Therefore, the main objectives of this study were to examine the extent to which racial and ethnic composition of NHs and their communities were associated with the likelihood of COVID-19 cases and death in NHs, and whether and how the relationship between NH characteristics and COVID-19 cases and death varied with the racial and ethnic composition of their community.
Methods
Data
CMS Nursing Home COVID-19 data include information on weekly new COVID-19 cases and death in all Medicare- and/or Medicaid-certified NHs in the United States.22 We downloaded the data on October 5, 2020, and linked it with other NH-level data, including 2019 Certification and Survey Provider Enhanced Reporting (CASPER) data, the CMS Nursing Home Compare 2020 May data (which provided information for the year prior to May 2020,23 downloaded on June 16, 2020), and 2018 Minimum Data Set. Several publicly available community-level data, including county-level COVID-19 infection data,24 the Area Health Resource File, LTC FocUS data,25 and the American Community Survey data,26 were obtained and linked.
Sample
We included weekly reported COVID-19 records that passed the CMS “quality check” (which ensure the data quality) for NHs with more than 30 occupied beds. Per CMS's suggestion,18 we excluded the first 3 weeks of data because initial reporting may not have been accurate. Because NHs could correct previously reported data18 and we expected that NHs were more likely to correct recently reported data, we also excluded the last 3 weeks of data to minimize the concern of potential data inaccuracy. In total, we included 12 weeks of data (between the week of June 7 and the week of August 23) for 13,123 NHs in the United States.
Variables
Two outcome variables were determined based on the CMS COVID-19 data: whether an NH had any new COVID-19 cases in a week and whether an NH had any COVID-19–related deaths in a week. Key independent variables included the racial and ethnic composition of an NH, defined as the percentage of residents who were either black or Hispanic in an NH, based on 2018 Minimum Data Set, and the racial and ethnic composition of the community in which the NH was located, based on the American Community Survey data. We categorized NHs into 3 mutually exclusive groups based on the percent of racial and ethnic minorities: NHs with low (0 to <2.63%), moderate (2.63% to <16.26%), or high (≥16.26%) percent minorities, with each accounting for approximately 33% of all NHs. We categorized the community as having either high or low minority prevalence based on the percentage of blacks or Hispanics at the 5-digit zip code level, with a cutoff point of 18.5% of Hispanics or 13.4% of blacks (which are the population averages in the United States based on Census Bureau data).27
We identified a set of NH- and community-level factors possibly related to the likelihood of COVID-19 infection in NHs, based on the literature.7 , 9, 10, 11, 12, 13, 14, 15, 16, 17 NH characteristics included a 5-star overall rating, ownership (profit and chain affiliation), hospital affiliation status, staffing level [RN hours per resident per day and certified nursing assistant (CNA) hours per resident per day], number of occupied beds, percentages of Medicare and Medicare residents, and the presence of any nurse practitioner or physical assistant in the facility. Community level factors included number of weekly new COVID-19 cases per 1000 people in the county, median household income in the county, the percentage of population aged ≥65 years (zip code level), the percentage of population with high school or higher education (county level), and whether the NH was located in a rural county.
Statistical Analyses
We estimated a set of linear probability models with NH random effects and robust standard errors (clustered at county level) to examine the probabilities of any COVID-19 infection and COVID-19 deaths. As trends in the probabilities of COVID-19 cases and death may not be linear over time, we used spline regressions to estimate the trends in the likelihood of COVID-19 cases and death in an NH and allowed the trends in the probability of COVID-19 cases and death to vary across high-, moderate-, and low-minority NHs. We then stratified the analyses by high- vs low-minority communities to examine whether and how the relationship between NH characteristic and the probabilities of COVID-19 cases and COVID-19 death varied across these communities. To facilitate the interpretation, we calculated the adjusted weekly probabilities of COVID-19 cases and death for each of the 3 NH groups in high- vs low-minority communities.
Results
Table 1 compares characteristics of NHs, by 3 groups of NHs and by communities. As shown in the table, the rate of COVID-19 cases, death, and characteristics of NHs varied across 3 types of NHs and between communities. For example, the unadjusted rate of any COVID-19 cases in low-, moderate- and high-minority NHs were 5.5%, 11.1%, and 14.8% in low-minority communities, and 10.6%, 14.5%, and 20.4% in high-minority communities. Table 2 presents the findings from the regression analyses, stratified by racial and ethnic composition of the community. NHs with a high proportion of minorities (ie, blacks and Hispanics) had 5.0 to 7.2 percentage points higher (P < .05) likelihood of COVID-19 cases and 2.6 to 6.4 percentage points higher death than NHs with low proportion of minorities at baseline.
Table 1.
Comparison of Nursing Home Characteristics by Prevalence of Minorities in the Nursing Homes and in Their Communities
| Low-Minority Community |
High-Minority Community |
|||||
|---|---|---|---|---|---|---|
| Low-Minority NHs | Moderate-Minority NHs | High-Minority NHs | Low-Minority NHs | Moderate-Minority NHs | High-Minority NHs | |
| No. of NHs | 3921 | 2938 | 684 | 278 | 1497 | 3805 |
| % of weeks with COVID cases | 5.48 | 11.06 | 14.76 | 10.61 | 14.47 | 20.38 |
| % of weeks with COVID death cases | 2.40 | 5.33 | 7.23 | 4.99 | 7.08 | 10.22 |
| Average cases over the entire period (SD) | 0.05 (0.11) | 0.11 (0.16) | 0.15 (0.18) | 0.11 (0.18) | 0.15 (0.18) | 0.21 (0.20) |
| Average death cases over the entire period (SD) | 0.02 (0.08) | 0.05 (0.11) | 0.07 (0.13) | 0.05 (0.11) | 0.07 (0.13) | 0.10 (0.15) |
| Star rating | ||||||
| 1-star | 9.41 | 18.48 | 23.98 | 4.32 | 12.09 | 25.73 |
| 2-star | 16.45 | 20.76 | 25.15 | 12.95 | 18.44 | 24.76 |
| 3-star | 17.57 | 17.60 | 17.98 | 14.39 | 20.17 | 19.16 |
| 4-star | 24.56 | 22.53 | 17.11 | 27.70 | 22.98 | 16.82 |
| 5-star | 32.01 | 20.63 | 15.79 | 40.65 | 26.32 | 13.53 |
| Hospital affiliation status (yes) | 3.52 | 1.23 | 2.05 | 2.52 | 2.47 | 1.97 |
| CNA hours per resident per day (SD) | 2.37 (0.54) | 2.18 (0.49) | 2.16 (0.47) | 2.59 (0.66) | 2.33 (0.53) | 2.22 (0.47) |
| RN hours per resident per day (SD) | 0.81 (0.38) | 0.65 (0.32) | 0.61 (0.37) | 0.89 (0.49) | 0.64 (0.35) | 0.50 (0.29) |
| Occupancy rate (SD) | 75.86 (14.23) | 72.94 (17.99) | 71.70 (14.84) | 75.53 (13.36) | 71.92 (14.81) | 72.27 (15.69) |
| No. of occupied beds (SD) | 67.96 (34.03) | 82.42 (43.76) | 95.94 (57.71) | 69.50 (37.64) | 79.83 (41.10) | 91.56 (49.10) |
| For profit | 64.40 | 82.33 | 85.23 | 49.28 | 76.35 | 88.88 |
| Not for profit | 35.60 | 17.67 | 14.77 | 50.72 | 23.65 | 11.12 |
| Government owned | 7.65 | 4.59 | 2.19 | 5.40 | 6.08 | 4.36 |
| % Medicaid | ||||||
| Low | 31.57 | 19.43 | 14.91 | 50.36 | 27.72 | 11.54 |
| Moderate | 52.10 | 53.54 | 42.54 | 31.65 | 50.57 | 45.60 |
| High | 12.01 | 21.24 | 38.89 | 10.43 | 16.23 | 39.71 |
| Missing | 4.31 | 5.79 | 3.65 | 7.55 | 5.48 | 3.15 |
| % Medicare | ||||||
| Low | 23.90 | 19.88 | 29.39 | 21.22 | 15.43 | 25.44 |
| Moderate | 50.06 | 50.03 | 46.64 | 42.81 | 44.82 | 51.04 |
| High | 21.73 | 24.30 | 20.32 | 28.42 | 34.27 | 20.37 |
| Missing | 4.31 | 5.79 | 3.65 | 7.55 | 5.48 | 3.15 |
| Chain | 53.76 | 61.98 | 58.92 | 40.29 | 54.64 | 59.50 |
| Missing | 4.31 | 5.79 | 3.65 | 7.55 | 5.48 | 3.15 |
| NP/PA | 45.50 | 59.94 | 62.87 | 41.01 | 52.04 | 58.03 |
| Missing | 4.31 | 5.79 | 3.65 | 7.55 | 5.48 | 3.15 |
| Rural | 7.91 | 2.08 | 0.88 | 2.88 | 1.60 | 1.66 |
| Median household income in a county (SD) | 54,954.39 (13,041.42) | 59,415.13 (16,171.78) | 63,758.75 (17,381.03) | 57,950.48 (14,146.98) | 57,296.58 (14,831.69) | 54,522.22 (14,965.07) |
| Percentage of population aged ≥65 y (zip code level) (SD) | 19.91 (6.64) | 19.00 (6.91) | 18.24 (5.47) | 16.06 (4.72) | 15.83 (5.19) | 14.60 (4.52) |
| % population with at least high school education in a county (SD) | 89.56 (4.33) | 89.17 (4.03) | 88.13 (4.19) | 86.79 (4.82) | 86.32 (5.12) | 84.19 (5.97) |
| Weekly new COVID cases per 1000 people in a county (SD) | 0.59 (0.70) | 0.75 (0.74) | 0.85 (0.79) | 1.00 (1.00) | 1.08 (0.98) | 1.39 (1.58) |
NP/PA, nurse practitioner/physician assistant; SD, standard deviation.
Values are percentages unless otherwise noted.
Table 2.
Results of Regression Models on Weekly Indicators of Any COVID-19 Cases and Any COVID-19 Deaths in an NH, Stratified by Racial and Ethnic Composition of the Community in Which an NH Is Located (Low- vs High-Minority Communities)
| Probability of Any COVID-19 Cases in an NH |
Probability of Any COVID-19 Death in an NH |
|||
|---|---|---|---|---|
| Low-Minority Community | High-Minority Community | Low-Minority Community | High-Minority Community | |
| NH characteristics | ||||
| Low-minority NHs | Reference | |||
| Moderate-minority NHs | 0.057‡ (0.010) | −0.010 (0.026) | 0.026‡ (0.008) | 0.013 (0.018) |
| High-minority NHs | 0.072‡ (0.021) | 0.050† (0.026) | 0.064‡ (0.018) | 0.056‡ (0.018) |
| Star rating | ||||
| 1-star | Reference | |||
| 2-star | 0.008 (0.006) | 0.007 (0.008) | −0.001 (0.004) | 0.006 (0.006) |
| 3-star | 0.009 (0.006) | −0.000 (0.008) | −0.002 (0.004) | 0.001 (0.007) |
| 4-star | 0.012† (0.005) | −0.007 (0.008) | −0.002 (0.004) | −0.008 (0.006) |
| 5-star | 0.010∗ (0.005) | −0.004 (0.009) | −0.004 (0.004) | −0.008 (0.007) |
| Hospital affiliation status (yes) | −0.017‡ (0.007) | −0.014 (0.017) | −0.015‡ (0.004) | −0.008 (0.011) |
| CNA hours per resident per day | 0.005 (0.003) | 0.026‡ (0.005) | −0.000 (0.002) | 0.014‡ (0.004) |
| RN hours per resident per day | −0.009† (0.004) | −0.028‡ (0.009) | −0.001 (0.003) | −0.010 (0.007) |
| Occupancy rate | −0.001‡ (0.000) | −0.003‡ (0.000) | −0.002‡ (0.000) | −0.003‡ (0.000) |
| No. of occupied beds | 0.001‡ (0.000) | 0.001‡ (0.000) | 0.000‡ (0.000) | 0.000‡ (0.000) |
| For profit | Reference | |||
| Not for profit | 0.002 (0.004) | −0.016† (0.007) | 0.005∗ (0.003) | 0.004 (0.006) |
| Government owned | −0.005 (0.006) | −0.030† (0.013) | −0.004 (0.005) | −0.015 (0.010) |
| % Medicaid | ||||
| High (>76.04) | Reference | |||
| Low (≤48.94) | −0.001 (0.005) | −0.000 (0.009) | −0.006 (0.004) | 0.002 (0.007) |
| Moderate (>48.94 and ≤76.04) | 0.006 (0.005) | −0.002 (0.006) | 0.001 (0.003) | 0.005 (0.005) |
| Missing | −0.007 (0.009) | −0.008 (0.015) | −0.015† (0.006) | −0.002 (0.011) |
| % Medicare | ||||
| High (>17.31) | Reference | |||
| Low (≤6.06) | −0.014‡ (0.005) | −0.024‡ (0.008) | −0.004 (0.004) | −0.006 (0.006) |
| Moderate (>6.06 and ≤17.31) | −0.010† (0.004) | −0.001 (0.007) | −0.003 (0.003) | 0.005 (0.005) |
| Chain membership | 0.003 (0.003) | 0.020‡ (0.005) | −0.001 (0.002) | 0.013‡ (0.004) |
| Any NP/PA | 0.006∗ (0.003) | 0.014‡ (0.005) | 0.005† (0.002) | 0.009† (0.004) |
| Rural | −0.010† (0.005) | −0.027∗ (0.016) | −0.006∗ (0.003) | −0.002 (0.013) |
| Time trends and their interactions with NH racial and ethnic composition | ||||
| Week of 06/07–week of 06/21 | −0.006‡ (0.002) | −0.005 (0.010) | −0.008‡ (0.002) | 0.001 (0.007) |
| Week of 06/21–week of 07/05 | −0.002 (0.002) | 0.023† (0.010) | −0.002 (0.001) | −0.005 (0.008) |
| Week of 07/05–week of 07/12 | 0.002 (0.004) | −0.009 (0.019) | −0.007‡ (0.002) | 0.004 (0.013) |
| Week of 07/12–week of 08/09 | 0.001 (0.001) | −0.003 (0.006) | 0.002‡ (0.001) | 0.007 (0.004) |
| Week of 08/09–week of 08/23 | −0.003 (0.002) | 0.012 (0.011) | −0.001 (0.002) | −0.013 (0.009) |
| Moderate-minority NH × week of 06/07-06/21 | −0.012‡ (0.004) | 0.005 (0.011) | −0.004 (0.003) | −0.009 (0.008) |
| High-minority NH × week of 06/07-06/21 | −0.005 (0.009) | −0.004 (0.011) | −0.009 (0.007) | −0.015† (0.008) |
| Moderate-minority NH × week of 06/21-07/05 | −0.003 (0.004) | −0.018 (0.012) | −0.005∗ (0.003) | 0.007 (0.008) |
| High-minority NH× week of 06/21-07/05 | −0.006 (0.008) | −0.014 (0.011) | −0.011∗ (0.006) | 0.002 (0.008) |
| Moderate-minority NH × week of 07/05-07/12 | 0.012∗ (0.007) | 0.044† (0.021) | 0.012‡ (0.005) | 0.006 (0.015) |
| High-minority NH × week of 07/05-07/12 | −0.004 (0.015) | 0.030 (0.020) | 0.005 (0.011) | 0.009 (0.014) |
| Moderate-minority NH × week of 07/12-08/09 | −0.000 (0.002) | 0.002 (0.007) | −0.001 (0.001) | −0.002 (0.005) |
| High-minority NHs × week of 07/12-08/09 | 0.000 (0.004) | 0.003 (0.006) | −0.004 (0.003) | −0.003 (0.004) |
| Moderate-minority NHs × week of 08/09-08/23 | −0.002 (0.004) | −0.026† (0.012) | 0.004 (0.003) | 0.007 (0.010) |
| High-minority NHs × week of 08/09-08/23 | −0.004 (0.008) | −0.034‡ (0.011) | −0.000 (0.005) | 0.004 (0.009) |
| Community characteristics | ||||
| Median household income (in $1000) | 0.0004‡ (0.0001) | 0.0002 (0.0002) | 0.0004‡ (0.0001) | 0.0002 (0.0001) |
| % population ≥65 y (zip code level) | 0.001‡ (0.000) | −0.000 (0.001) | 0.000† (0.000) | −0.001 (0.000) |
| % population with at least high school education in a county | −0.001† (0.000) | −0.001† (0.001) | −0.001‡ (0.000) | −0.001‡ (0.000) |
| Weekly new COVID cases per 1000 people in a county | 0.052‡ (0.003) | 0.040‡ (0.005) | 0.019‡ (0.002) | 0.018‡ (0.003) |
| Intercepts | 0.139‡ (0.042) | 0.292‡ (0.058) | 0.185‡ (0.029) | 0.332‡ (0.044) |
| No. of observations | 87034 | 64620 | 87034 | 64620 |
| No. of NHs | 7543 | 5580 | 7543 | 5580 |
NP/PA, nurse practitioner/physician assistant; SD, standard deviation.
Unless otherwise noted, values are point estimates with standard errors in parentheses.
P < .10.
P < .05.
P < .01.
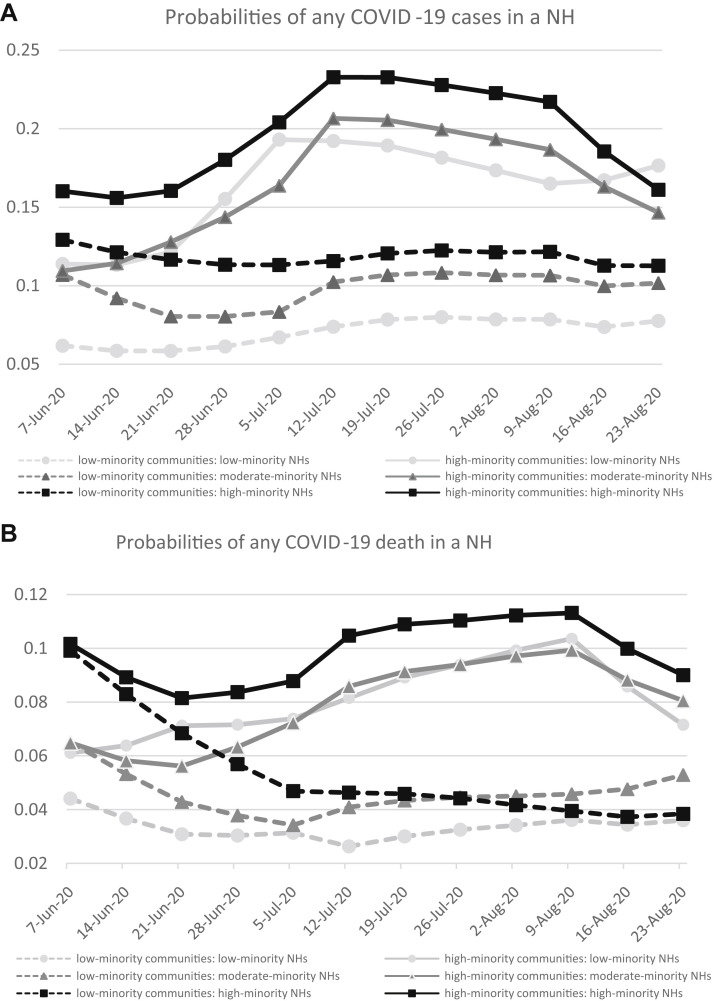
Figure 1 presents the trends in the predicted probabilities of any COVID-19 cases (panel A) and any COVID-19–related death (panel B), adjusting for NH and community characteristics. The variations in the probabilities of NH COVID-19 cases or death appeared to vary across the 3 groups of NHs as well as the 2 types of communities. For example, the differences in the predicted probability of having COVID-19 cases in high-minority NHs between high- vs low-minority community was about 12 percentage points during the week of July 12 (P < .01, statistical test not presented in the figure). On the other hand, the differences in such probabilities between high- vs low-minority NHs within each type of communities were about 4 percentage points during the same time period (P < .05).
Fig. 1.
Weekly predicted probability of any (A) COVID-19 case and (B) COVID-19 death in an NH, adjusting for facility and community characteristics. Predicted probabilities are presented for high- (squares), moderate- (triangles), and low-minority (circles) NHs located in high-minority (solid line) vs low-minority (dashed line) communities.
The trends in the adjusted probabilities in COVID-19 cases or death highlight the role of racial and ethnic composition of the community; for example, although high-minority NHs in low-minority communities had an overall decreasing trend in the likelihood of COVID-19 deaths over these weeks, high-minority NHs in high-minority communities saw an increasing trend in COVID-19 deaths for most of the weeks (Figure 1B).
Lastly, the relationship between NH characteristics and the probability of COVID-19 cases or death varied with the racial and ethnic composition of the community (Table 2). For example, although an hour increase in RN hours per resident per day was associated with 2.8 percentage points reduction in the probability of COVID-19 cases in NHs located in high-minority communities (P < .01), such relationship was smaller in low-minority communities (0.9 percentage points, P < .01). We also observed that a higher CNA staffing level was associated with a higher probability of COVID-19 cases (coefficient = 0.026, P < .01) or death (coefficient = 0.014, P < .01) in NHs located in high-minority communities, but there was no statistically significant relationship between CNA and the likelihood of COVID cases or death in low-minority communities. In addition, we found that a higher star rating of NHs was associated with a higher likelihood of COVID-19 cases in NHs located in low-minority communities but not in NHs located in high-minority communities.
Discussion
This study examined the relationship between racial and ethnic composition of an NH and its community and the probabilities of COVID-19 cases and death in NHs. We found that racial and ethnic composition of the community also had an impact on the likelihood of COVID-19 cases or death in an NH, additional to the racial and ethnic composition of an NH, and importantly, that the community racial and ethnic composition modified the relationship between NH characteristics and COVID-19 cases and death.
Although recent studies indicated that NH COVID-19 outbreaks were related to where the NH was located with respect to the area's prevalence of COVID-19,10 , 20 , 28 our study suggested the independent role of racial and ethnic composition of the community in the outbreak of COVID-19 in NHs, after accounting for the COVID-19 infection rate in the county and other covariates. Moreover, the variation in the likelihood of NH COVID-19 cases and death between high- vs low-minority communities appeared to be large. These findings may be related to the different NH characteristics between communities, as well as community behavioral factors. For example, NHs located in poor communities are more likely to be resource deprived6 and thus may face even greater challenges in dealing with the pandemic. In addition, it has been reported that composition of race and ethnicity of a community was associated with individual socioeconomic status, living condition, health belief, health behavior, and health status.29, 30, 31 These community behavioral characteristics may have directly or indirectly contributed to the COVID-19 infection in the community and consequently may have affected the likelihood of COVID-19 infection in NHs.
Furthermore, we found the relationship between NH characteristic and the likelihood of COVID-19 cases or death also varied by the racial and ethnic composition of a community. For example, the relationship between higher RN staffing and lower likelihood of any NH COVID-19 cases was stronger in high-minority communities than in low-minority communities. A high level of RN staffing was found to be generally related to better care quality in NHs.32 , 33 NHs with higher RN staffing may have been better prepared to implement and manage the procedures of infection control in NHs. The relationship between RN staffing and COVID-19 infection rates therefore may be particularly important for NHs located in high-minority communities, which are generally more likely to be socioeconomically deprived.21
On the other hand, we found that higher CNA staffing was associated with a higher probability of COVID-19 infection and death in NHs located in high-minority communities but was not associated with COVID-19 cases or death in low-minority communities. The majority of NH staff are CNAs,34 with about half blacks or Hispanic.35 Several reasons may contribute to this observed relationship. First, it is possible that CNAs are likely to be from the communities where NHs are located. Communities with a higher percentage of racial and ethnic minorities are more likely to be economically deprived and have higher COVID-19 rates, and thus may amplify the risks of cross-infections between CNAs and staff members. Or alternatively, as many CNAs live in poverty,35 they are likely to use public transportations to work, which increase their exposure to COVID-19 outbreaks in high-minority communities.36 , 37 Lastly, as NHs in high-minority communities are more likely to be resource deprived, they may have less capacity for implementing necessary infection control protocols and have a higher risk of cross-infection between residents and their direct care works.
There are some limitations to this study. First, although this study examined the probabilities of COVID-19 cases and deaths across NHs and communities with different racial and ethnic composition, we were unable to determine the underlying reasons that led to such variations. Second, this was a facility-level analysis, and we were unable to account for individual resident characteristics, which may also be related to the likelihood of COVID-19 infection or death. Third, NH staffing is likely to change with the COVID-19 outbreak in NHs. We were only able to account for staffing level prior to the pandemic and were not able to capture the effects of time-varying staffing level during the pandemic. On the other hand, staff-level changes may also be the consequence of COVID-19 outbreak in NHS, and staffing level prior to the pandemic addresses the potential impact of NHs’ preparedness for handling emergency situations, in particular the pandemic.
Conclusions and Implications
In conclusion, although racial and ethnic minority NH residents have experienced exacerbated risks of COVID-19 infection and death, this study showed that the racial and ethnic composition of the community in which the NH was located appeared to have a large impact on NH COVID-19 outbreak. Furthermore, the racial and ethnic composition of the community modified the relationship of some NH characteristics with management of COVID-19 outbreaks.
There has long been a great concern that structural racism and social factors are intertwined with the unequal health care and health outcomes among people of color.38 Poor living condition, barriers in access to care, and limited access to education in these communities may contribute to the higher COVID-19 infection rates in the community. This study shows that these same factors may subsequently affect the most vulnerable NH populations. Although CMS has implemented several policies to control COVID-19 outbreak in NHs, and vaccinations have been massively provided, additional efforts may be needed to reduce structural racism and address social risk factors to improve quality of care and population health in communities of color.
Footnotes
This study was supported by grants from the National Institute on Aging (NIA; RF1AG063811 & R01AG052451). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the National Institutes of Health or NIA.
The authors declare no conflicts of interest.
References
- 1.Abbasi J. “Abandoned” nursing homes continue to face critical supply and staff shortages as COVID-19 toll has mounted. JAMA. 2020;324:123–125. doi: 10.1001/jama.2020.10419. [DOI] [PubMed] [Google Scholar]
- 2.Kaiser Family Foundation Key questions about nursing home regulation and oversight in the wake of COVID-19. https://www.kff.org/coronavirus-covid-19/issue-brief/key-questions-about-nursing-home-regulation-and-oversight-in-the-wake-of-covid-19/ Available at: Published 2020. Accessed April 12, 2021.
- 3.New York Times . 2021. Nearly one-third of U.S. coronavirus deaths are linked to nursing homes.https://www.nytimes.com/interactive/2020/us/coronavirus-nursing-homes.html Available at: [Google Scholar]
- 4.Cai S., Mukamel D.B., Temkin-Greener H. Pressure ulcer prevalence among black and white nursing home residents in New York State: Evidence of racial disparity? Med Care. 2010;48:233–239. doi: 10.1097/MLR.0b013e3181ca2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cai S., Feng Z., Fennell M.L., Mor V. Despite small improvement, black nursing home residents remain less likely than whites to receive flu vaccine. Health Aff (Millwood) 2011;30:1939–1946. doi: 10.1377/hlthaff.2011.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mor V., Zinn J., Angelelli J. Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82:227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y., Cen X., Cai X., Temkin-Greener H. Racial and ethnic disparities in COVID-19 infections and deaths across U.S. nursing homes. J Am Geriatr Soc. 2020 doi: 10.1111/jgs.16847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.New York Times The striking racial divide in how COVID-19 has hit nursing homes. https://www.nytimes.com/article/coronavirus-nursing-homes-racial-disparity.html Available at: Published September 10, 2020. Accessed April 12, 2021.
- 9.Konetzka R.T. Caring for seniors amid the COVID-19 crisis. https://www.aging.senate.gov/imo/media/doc/SCA_Konetzka_05_21_20.pdf Available at: Published 2020. Accessed April 12, 2021.
- 10.Abrams H.R., Loomer L., Gandhi A., Grabowski D.C. Characteristics of U.S. nursing homes with COVID-19 cases. J Am Geriatr Soc. 2020;68:1653–1656. doi: 10.1111/jgs.16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorges R.J., Konetzka R.T. Factors associated with racial differences in deaths among nursing home residents with COVID-19 infection in the US. JAMA Netw Open. 2021;4:e2037431. doi: 10.1001/jamanetworkopen.2020.37431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorges R.J., Konetzka R.T. Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. J Am Geriatr Soc. 2020;68:2462–2466. doi: 10.1111/jgs.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Figueroa J.F., Wadhera R.K., Papanicolas I. Association of nursing home ratings on health inspections, quality of care, and nurse staffing with COVID-19 cases. JAMA. 2020;324:1103–1105. doi: 10.1001/jama.2020.14709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Y., Temkin-Greener H., Shan G., Cai X. COVID-19 infections and deaths among Connecticut nursing home residents: Facility correlates. J Am Geriatr Soc. 2020;68:1899–1906. doi: 10.1111/jgs.16689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ochieng N., Chidambaram P., Garfield R., Neuman T. Factors associated with COVID-19 cases and deaths in long-term care facilities: Findings from a literature review. https://www.kff.org/coronavirus-covid-19/issue-brief/factors-associated-with-covid-19-cases-and-deaths-in-long-term-care-facilities-findings-from-a-literature-review/ Available at: Published 2021. Accessed April 12, 2021.
- 16.Bui D.P., See I., Hesse E.M. Association between CMS quality ratings and COVID-19 outbreaks in nursing homes—West Virginia, March 17-June 11, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1300–1304. doi: 10.15585/mmwr.mm6937a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White E.M., Kosar C.M., Feifer R.A. Variation in SARS-CoV-2 prevalence in U.S. skilled nursing facilities. J Am Geriatr Soc. 2020;68:2167–2173. doi: 10.1111/jgs.16752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services COVID-19 nursing home data. https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/ Available at: [PubMed]
- 19.Figueroa J.F., Wadhera R.K., Lee D. Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood) 2020;39:1984–1992. doi: 10.1377/hlthaff.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chatterjee P., Kelly S., Qi M., Werner R.M. Characteristics and quality of US nursing homes reporting cases of coronavirus disease 2019 (COVID-19) JAMA Netw Open. 2020;3:e2016930. doi: 10.1001/jamanetworkopen.2020.16930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meade E. ASPE Research Brief: Overview of community characteristics in areas with concentrated poverty. https://aspe.hhs.gov/system/files/pdf/40651/rb_concentratedpoverty.pdf Available at: Published 2014. Accessed November 18, 2021.
- 22.Centers for Medicare & Medicaid Services COVID-19 nursing home dataset. https://data.cms.gov/Special-Programs-Initiatives-COVID-19-Nursing-Home/COVID-19-Nursing-Home-Dataset/s2uc-8wxp Available at: Published 2020. Accessed December 16, 2020. [PubMed]
- 23.Centers for Medicare & Medicaid Services Design for Nursing Home Compare Five-Star Quality Rating System: Technical users’ guide. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/downloads/usersguide.pdf Available at:
- 24.USAFACTS US coronavirus cases and deaths: Track COVID-19 data daily by state and county. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map Available at:
- 25.LtcFocus. http://ltcfocus.org Available at:
- 26.United States Census Bureau Understanding and using American Community Survey data. https://wwwcensusgov/content/dam/Census/library/publications/2018/acs/acs_general_handbook_2018pdf Available at:
- 27.United States Census Bureau. https://www.census.gov/quickfacts/fact/table/US/PST045219#qf-headnote-b Available at:
- 28.Grabowski D.C., Konetzka R.T., Mor V. We can’t protect nursing homes from COVID-19 without protecting everyone. June 25, 2020. https://www.washingtonpost.com/opinions/2020/06/25/we-cant-protect-nursing-homes-covid-19-without-protecting-everyone/ Available at:
- 29.House J.S., Lepkowski J.M., Kinney A.M. The social stratification of aging and health. J Health Soc Behav. 1994;35:213–234. [PubMed] [Google Scholar]
- 30.Robert S.A. Socioeconomic position and health: The independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 31.Lantz P.M., House J.S., Lepkowski J.M. Socioeconomic factors, health behaviors, and mortality: Results from a nationally representative prospective study of US adults. JAMA. 1998;279:1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 32.Harrington C., Zimmerman D., Karon S.L. Nursing home staffing and its relationship to deficiencies. J Gerontol B Psychol Sci Soc Sci. 2000;55:S278–S287. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- 33.Harrington C., Swan J.H. Nursing home staffing, turnover, and case mix. Med Care Res Rev. 2003;60:366–392. doi: 10.1177/1077558703254692. [DOI] [PubMed] [Google Scholar]
- 34.National Center for Health Statistics Long-term care providers and services users in the United States, 2015–2016. https://www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf Available at: Published 2019. Accessed November 18, 2021. [PubMed]
- 35.Kaiser Family Foundation COVID-19 and workers at risk: Examining the long-term care workforce. https://www.kff.org/medicaid/issue-brief/covid-19-and-workers-at-risk-examining-the-long-term-care-workforce/?utm_campaign=KFF-2020-Medicaid%26utm_source=hs_email%26utm_medium=email%26utm_content=86855544%26_hsenc=p2ANqtz-_lP7AwFxEYqlHmG5FM3pOFDsyr4pEhfDoldSbNFOF5tsTktGkIWQ2uExwLMu5pRSa12BxQyThwTWs5ieylTb7fYzFWnA%26_hsmi=86855544 Available at:
- 36.Parker K., Minkin R., Bennett J. Economic fallout from COVID-19 continues to hit lower-income Americans the hardest. https://www.pewresearch.org/social-trends/2020/09/24/economic-fallout-from-covid-19-continues-to-hit-lower-income-americans-the-hardest/ Available at: Published 2020. Accessed April 12, 2021.
- 37.Iceland J., Weinberg D., Steinmetz E. Racial and ethnic residential segregation in the United States: 1980-2000. https://www.census.gov/prod/2002pubs/censr-3.pdf Available at: Published 2002. Accessed April 12, 2021.
- 38.Egede L.E., Walker R.J. Structural racism, social risk factors, and COVID-19—A dangerous convergence for black Americans. N Engl J Med. 2020;383:e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]