Abstract
Purpose
SP-102 is a novel epidural steroid injection (ESI) formulation of 10 mg dexamethasone sodium phosphate in a viscous gel solution. Repeat dosing of ESIs is possible if required for pain relief, but with consideration of hypothalamic–pituitary–adrenal (HPA) axis suppression from prolonged systemic exposure. This phase I/II study investigated the effect of initial and repeat SP-102 injections on HPA suppression and analgesia.
Methods
Subjects with lumbosacral radiculopathy received an initial epidural SP-102 injection (T1) on day 1, followed by a repeat injection (T2) on ≥28 days later. To determine HPA suppression, area under the effect curve over 28 days and maximum change from baseline were calculated for cortisol, glucose levels, and white blood cell (WBC) count. Equivalent effect on HPA suppression of T1 relative to T2 was determined if the 90% CIs for ratios of these measures were within 80%–125%. The effect of repeat injections on leg and back pain was also assessed.
Results
Based on the responder analysis, all subjects had achieved a cortisol response by day 3 after initial injection and by day 2 after repeat injection. The repeat injection had similar effects on glucose levels and WBC count to the initial injection. Pain scores decreased after each injection and remained low for the 28-day follow-up, with some evidence of improved analgesic effect of the second dose compared with the first. There were no serious adverse events or discontinuations due to adverse events.
Conclusion
The lack of cumulative effect and rapid resolution of HPA suppression following repeated SP-102 dosing suggests that consideration of HPA pharmacodynamics is not clinically relevant when making decisions regarding repeat dosing. SP-102 ESIs provided prolonged pain relief, with preliminary evidence of greater efficacy after repeat injection. A phase III trial is ongoing.
Clinical Trial Identifier
ClinicalTrials.gov: NCT03613662.
Keywords: epidural steroid injections, lubosacral radicuar pain, sciatica, neuropathic pain
Introduction
Lumbosacral radicular pain (also known as sciatica) has an estimated lifetime incidence of 13%–40% and annual incidence of 1%–5%.1–3 Epidural steroid injections (ESIs) are commonly used for lumbosacral radicular pain when more conservative treatments, including analgesic or nonsteroidal anti-inflammatory drugs, muscle relaxants, and physical therapy, have been ineffective.2,4,5 ESI use has been associated with positive outcomes for patients in prospective randomized trials and retrospective studies, including reduced leg and back pain and avoidance of surgery.6,7
In 2014 the US Food and Drug Administration (FDA) issued a requirement that all injectable glucocorticoid product labels carry a warning, due to reports of serious and sometimes fatal neurological events with epidural administration.8 All recorded events that resulted in permanent disability or death were associated with injection of particulates containing (suspension) steroid formulations. In contrast, use of soluble glucocorticoids, such as dexamethasone, has been associated with fewer adverse reactions9,10 resulting in their recommendation as first-choice steroid for ESIs by an expert panel.11 However, studies on dexamethasone ESIs have suggested that their analgesic effect has a shorter duration than particulate steroids.12,13 Given the safety concerns with particulate-containing ESIs, there is a clear need to extend the duration of the analgesic effect of dexamethasone.
SP-102 is a novel formulation of dexamethasone consisting of dexamethasone sodium phosphate equivalent to 10 mg dexamethasone in 2 mL injectable viscous gel designed to prolong residence at the site of injection. Data from a phase I pharmacokinetic and pharmacodynamic (PD) bridging study indicate that this has been achieved, with epidural injections of SP-102 resulting in lower maximum plasma concentration and longer time to maximum plasma concentration of dexamethasone than intravenous administration of standard dexamethasone sodium phosphate solution (manuscript in preparation).
In clinical practice, it is common to administer repeat ESIs.14 However, prolonged systemic absorption of corticosteroids and associated suppression of the hypothalamic–pituitary–adrenal (HPA) axis can result in susceptibility to infection, Cushing syndrome, hyperglycemia, and loss of bone density.15 The duration of HPA suppression of any extended-release steroid formulation, such as SP-102, needs to be considered. Therefore, the primary objective of this study was to characterize the repeat-dose PDs of epidural SP-102 with respect to HPA suppression in subjects with lumbosacral radiculopathy. Secondary objectives of the study were to determine the safety profile and assess the analgesic effects of single and repeat-dose epidural SP-102.
Methods
Ethics and Registration
This phase I/II study was submitted to ClinicalTrials.gov as NCT03613662 on July 9, 2018. The study was approved by the Copernicus Group Institutional Review Board, and patients were informed of the purpose of the trial and provided written consent. This trial was conducted according to the ethical principles stated in the Declaration of Helsinki. Patient enrollment commenced on July 13, 2018, with the last subject last visit completed on March 15, 2019.
SP-102 is an investigational drug that has received fast-track designation from the FDA. SP-102 is not currently FDA-approved for any indication.
Subject Eligibility
All subjects had a diagnosis of lumbosacral radicular pain at the screening visit, defined as pain radiating unilaterally or bilaterally into the leg(s). Average screening and baseline numeric pain-rating scale (NPRS) pain scores over the previous 24 hours were required to be between 4 and 9 in the affected leg(s). Subjects had to meet appropriate clinical criteria for lumbar ESI as per the discretion of the investigator.
Eligible subjects were aged 18–70 years. Effective birth control if relevant was required, and subjects with diabetes, abnormalities of the cortisol system, cancer, or other significant medical complications were excluded. If subjects were taking oral, nonopioid analgesics for indications other than radicular pain, they needed to remain on stable doses from the screening visit through to the end of the study. They could be on no more than 30 mg morphine equivalent for no more than 2 days per week in the 30 days prior to the screening visit and needed to discontinue all opioids prior to the screening visit.
Study Design and Interventions
The study took place at a pain clinic in Boise, ID, USA. All subjects received a fluoroscopically guided transforaminal or interlaminar epidural injection of SP-102 at baseline (initial injection, treatment 1 [T1]). The injection was placed in only one location for all patients, and there was no dose splitting. Subjects who experienced radicular pain after 4 weeks (defined as average NPRS pain score in affected limb of 4–9 in the previous 24 hours) were eligible to receive a second epidural injection of SP-102 (repeat injection, treatment 2 [T2]). If the subject was not eligible for T2 or chose to withdraw from further participation in the study, the subject was scheduled for an end-of-study visit.
Objectives
The primary objective of this study was to characterize repeat-dose PDs of SP-102 administered by epidural injection with respect to HPA suppression, using plasma-cortisol levels, white blood cell (WBC) count, and blood glucose as biomarkers.
Secondary objectives were to determine the safety profile and assess the analgesic effects of single -and repeat-dose SP-102.
Assessments
HPA suppression was assessed by monitoring changes in plasma-cortisol levels, WBC count, and blood glucose before and after T1 and T2 from blood samples obtained from subjects. Before blood was drawn, subjects were required to fast for at least 10 hours, except for the sample taken at the screening visit. Predose morning values before each treatment were determined to be the baseline values.
Factors other than steroid ESIs can have an effect on cortisol, glucose, and WBC levels.16–19 For this reason, subjects were confined to a controlled environment for 12 hours overnight before blood was drawn for lab samples. Subjects were also screened for signs or symptoms of infectious disease and other factors that could have an impact on lab results.
All subjects were monitored for adverse events (AEs), which were coded according to MedDRA terms. Treatment-emergent AEs (TEAEs) were defined as AEs that had an onset or preexisting AEs that worsened on or after the initial injection and within 30 days of the last study treatment. Safety assessments included laboratory values, physical examination with a focus on neurological findings, and electrocardiography.
Analgesic effects were assessed using the NPRS (current, worse, and average pain) of the lower back and leg and the Brief Pain Inventory — short form (BPI-SF). The only rescue analgesic allowed during this study was up to 3 g acetaminophen daily, and all rescue-medication use was recorded.
PD, safety, and analgesia assessments were collected at screening, predose, daily for 4 days postdose (during which time subjects were housed overnight in a restricted environment), and at three outpatient follow-up visits on days 8, 15, and 28 after each injection.
Statistical Analysis
All statistical analyses were performed using SAS 9.4. Descriptive statistics were used for all measurements. No formal statistical power calculations were performed for this study.
For blood-cortisol and glucose levels and WBC counts, the area under the effect curve over 28 days (AUEC28) was defined using observed values, in line with an addendum made to the statistical analysis plan after database lock. Maximum change from baseline (Emax) in cortisol, WBC count, and glucose levels was calculated as the maximum increase or decrease in observed values from T1 day 0 and T2 days 0–28, following the initial (T1) and repeat (T2) epidural injections, respectively. An analysis to determine subjects with a cortisol response and the time point of this response was performed. Responders were defined as subjects whose cortisol levels returned to baseline after injection, with this being defined as cortisol levels returning to <10 nmol/L below baseline or any value including and above baseline. If a subject returned to their baseline values, they were considered a responder for the remainder of the visits.
PD parameters were analyzed using a mixed-model ANOVA with a fixed effect for treatment and a random effect for subject after logarithmic transformation. Estimates and two-sided 90% CIs for geometric means and ratios of geometric means were calculated using antilogarithm transformation of least-squares estimates. An a priori lack of effect of repeat injection on PDs would be determined if the 90% CIs for the ratio of T2 to T1 for both AUEC28 and Emax were completely contained within the range of 80%–125%. Pain assessment closest to and prior to dosing in each treatment period was used as baseline for each treatment period.
Results
Subject Characteristics and Disposition
A total of 27 subjects were recruited, of whom eight were excluded for not meeting the eligibility criteria. Nineteen subjects were enrolled between July 25 and November 7, 2018 and underwent an initial injection of SP-102. The last recorded study visit was on January 15, 2019. Fifteen subjects underwent repeat injections at a median of 42(IQR 42–49) days after the initial injection. Four subjects did not have pain scores high enough to justify repeat injection of SP-102. All subjects completed the study, and no major deviations from the protocol were reported.
The median age of study participants was 60 (IQR 46–65) years, 63% (12 of 19) were female, and all were Caucasian, except for three subjects (15.8%) who had Hispanic/Latino ethnicity (Table 1). Median body-mass index was 32 (IQR 25–35).
Table 1.
Subjects’ baseline characteristics
| n=19 | ||
|---|---|---|
| Age (years), median (IQR) | 60 (46–65) | |
| Sex | Male, n (%) | 7 (36.8) |
| Female, n (%) | 12 (63.2) | |
| BMI (kg/m2), median (IQR) | 32.1 (25.1–35.1) | |
| Straight-leg raise (L5–S1), n (%) | Pain down affected extremity | 7 (36.8) |
| Paresthesia down affected extremity | 0 | |
| Femoral stretch test (L3–L4), n (%) | Pain down affected extremity | 7 (36.8) |
| Paresthesia down affected extremity | 3 (15.8) | |
Abbreviation: BMI, body-mass index.
Pharmacodynamics
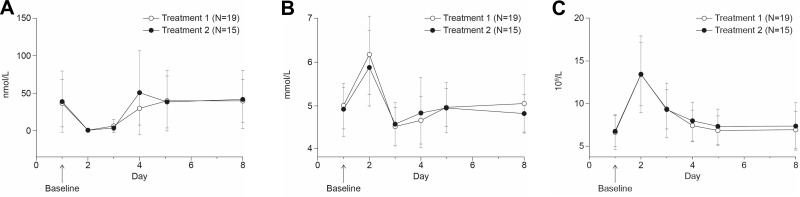
Mean plasma cortisol levels dropped during the 24 hours immediately after T1 (n=19) and T2 (n=15), injections but increased after day 3 (Figure 1A). The AUEC28 ratio (comparison of T2 versus T1) for cortisol levels was 116% (90% CI 88%–154%). The upper end of the CI range was outside the boundary that would indicate equivalence of the cortisol response between T1 and T2. However, a paired t-test revealed no significant difference between AUEC28 values for the two treatments (p=0.091). Cortisol levels were also examined for 8 days after each injection. The AUEC8 ratio was 100% (90% CI 73%–138%), with a paired t-test indicating that there was no significant difference in AUEC28 values between the two treatments at this time point (p=0.59). The Emax ratio for cortisol was 97% (90% CI 73%–128%). Results of cortisol-responder analysis, in which responders were defined as subjects whose cortisol levels returned to <10 nmol/L below baseline or any value including and above baseline, showed that all subjects had their cortisol return to baseline levels by day 3 of the initial injection and by day 2 of the repeat injection.
Figure 1.
Pharmacodynamic assessments of single and repeat doses of SP-102. Pharmacodynamic assessments through 8 days after initial (T1) and repeat (T2) epidural injections. Mean cortisol levels over time (A), mean blood-glucose levels over time (B), mean WBC count over time (C). Error bars denote SD.
Mean blood glucose rose slightly during the 24 hours postinjection for T1 and T2, before dropping below baseline, then increasing to pretreatment levels by day 5 and remaining stable during the follow-up (Figure 1B). There were no significant differences between T1 and T2: the AUEC28 ratio for glucose levels was 101% (90% CI 96%–106%). The Emax ratio for blood glucose was 61% (90% CI 26%–143%), which was outside the prespecified range.
Mean WBC count followed a return to baseline pattern similar to both cortisol and glucose levels (Figure 1C). The AUEC28 ratio for WBC values was 103% (90% CI 93%–114%), while the Emax ratio was 103% (90% CI 83%–127%).
Safety and Tolerability
All AEs reported during the study period were TEAEs, except for one AE of pertussis that occurred 32 days after T1 in one subject. The most common TEAE was headache (seven of 19, 36.8%), which was considered at least possibly related to the study drug in all cases. Other AEs experienced by more than one subject over the course of both treatments were dyspepsia (two of 19, 10.5%), nasopharyngitis (two of 19, 10.5%), and tooth abscess (two of 19, 10.5%). Five events of infection were experienced by four subjects after the first dose (nasopharyngitis [n=2], tooth abscess [n=2], and respiratory tract infection [n=1]; Table 2). After the second dose, one infection-related AE of tooth abscess and one AE of bronchitis were recorded. None of the infections were considered to be related to the ESI. Overall, AEs were predominantly mild in nature, and there were no serious AEs or discontinuations due to the study drug (Table 2). Two moderate AEs of abdominal pain (one of 19, 5.3%) and headache (one of 19, 5.3%) were considered at least possibly related to the study drug.
Table 2.
AEs in subject after single and repeat doses of SP-102
| Initial (T1), n=19 | Repeat (T2), n=15 | ||||
|---|---|---|---|---|---|
| Subjects, n (%) | Events, n | Subjects, n (%) | Events, n | ||
| AEs, all severity | 13 (68.4) | 21 | 8 (53.3) | 10 | |
| TEAEs | 12 (63.2) | 20 | 8 (53.3) | 10 | |
| Mild | Total | 10 (52.6) | 15 | 6 (40) | 7 |
| Headache | 4 (21.1) | 4 | 3 (20) | 3 | |
| Nasopharyngitis | 2 (10.5) | 2 | |||
| Tooth abscess | 2 (10.5) | 2 | |||
| Body aches | 1 (5.3) | 1 | |||
| Dyspepsia | 1 (5.3) | 1 | 1 (6.7) | 1 | |
| GERD | 1 (5.3) | 1 | |||
| Increased glucose | 1 (5.3) | 1 | |||
| Increased WBCs | 1 (5.3) | 1 | |||
| Migraine | 1 (5.3) | 1 | |||
| Neck pain | 1 (5.3) | 1 | |||
| Night sweats | 1 (5.3) | 1 | |||
| Respiratory tract infection | 1 (5.3) | 1 | |||
| Abdominal discomfort | 1 (6.7) | 1 | |||
| Back pain | 1 (6.7) | 1 | |||
| Bronchitis | 1 (6.7) | 1 | |||
| Food poisoning | 1 (6.7) | 1 | |||
| Moderate | Total | 2 (10.5) | 3 | 2 (13.3) | 2 |
| Headache | 1 (5.3) | 1 | |||
| Abdominal pain | 1 (5.3) | 1 | 1 (6.7) | 1 | |
| Tooth abscess | 1 (6.7) | 1 | |||
| Back pain | 1 (5.3) | 1 | |||
| Severe | 0 | 0 | 0 | 0 | |
| TEAEs related to study drug | 10 (52.6) | 13 | 5 (33.3) | 5 | |
| Mild | 8 (42.1) | 11 | 5 (33.3) | 5 | |
| Moderate | 2 (10.5) | 2 | 0 | 0 | |
| Severe | 0 | 0 | 0 | 0 | |
| SAEs (any type) | 0 | 0 | 0 | 0 | |
| Deaths | 0 | 0 | 0 | 0 | |
Abbreviations: AEs, adverse events; GERD, gastroesophageal reflux disease; TEAEs, treatment-emergent AEs; SAE, serious AEs; WBCs, white blood cells.
Hematological and biochemical abnormalities were infrequent and not thought to be clinically relevant, with one subject experiencing blood-glucose and WBC perturbations large enough to be recorded as mild AEs.
Analgesia
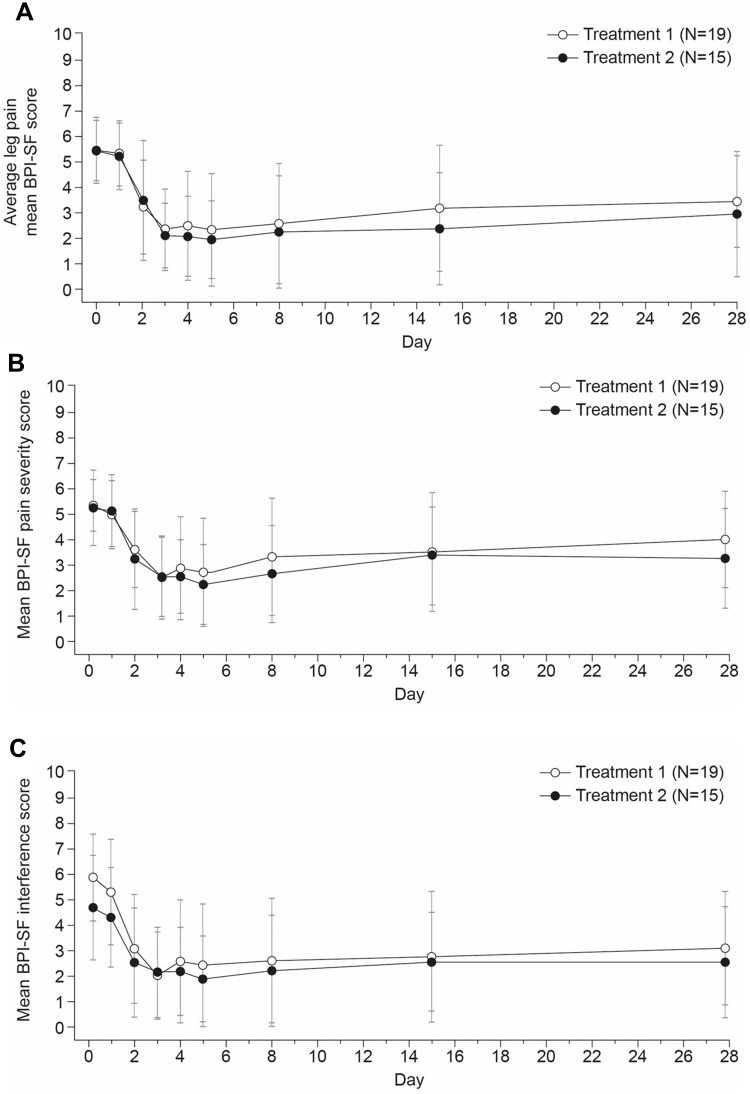
There was a decrease in NPRS value for average pain in the affected leg from a mean 5.4±1.3 at T1 baseline to 3.4±1.8 at day 28. For subjects that received a second injection of SP-102, NPRS values for average pain in the affected leg were mean 5.4±1.2 at T2 baseline and 2.9±2.5 at day 28 (see Figure 2A). In sum, 47% (nine of 19) of subjects had ≥50% reduction in average leg pain from T1 baseline after 28 days and 60% (nine of 15) ≥50% reduction of pain from T2 baseline after 28 days.
Figure 2.
Analgesic effects of single and repeat doses of SP-102. Analgesic assessments after initial (T1) and repeat (T2) epidural injections. Mean NPRS score for average leg pain (A), mean BPI-SF pain-severity score (B), mean BPI-SF pain-interference score (C). Error bars denote SD.
Abbreviations: NPRS, numeric pain-rating scale; BPI-SF, Brief Pain Inventory — short form.
The impact of SP-102 on low-back pain was less pronounced, with average scores for worst back pain of 6.4±1.7 at T1 baseline and 5.1±2.0 after 28 days. At T2 baseline, mean scores for worst back pain were 6.5±1.4 and had decreased to 4.0±2.4 by day 28. Four of (subjects (21%) reported a reduction in average back pain of ≥50% from baseline to 28 days after T1, which had increased to seven of 15 subjects (47%) by 28 days after T2 compared to T2 baseline.
AEUC28 T2:T1 ratios were <100% for average, current, and worst NPRS scores in the affected leg and lower back, with the lower end of the 90% CI range <50% in all cases in the leg (Table 3). This suggests that mean NPRS scores were lower in T2 for both leg and back pain.
Table 3.
Statistical analysis of PD and analgesic parameters
| AUEC28 ratio, % (90% CI) | Emax ratio, % (90% CI) | ||
|---|---|---|---|
| Plasma cortisol | 116 (88–154) | 97 (73–128) | |
| Blood glucose | 101 (96–106) | 61 (26–143) | |
| WBC count | 103 (93–114) | 103 (83–127) | |
| Leg NPRS | Average | 70 (47–105) | — |
| Current | 62 (42–93) | — | |
| Worst | 67 (46–99) | — | |
| Lower-back NPRS | Average | 74 (51–106) | — |
| Current | 78 (52–116) | — | |
| Worst | 75 (54–105) | — | |
Abbreviations: PD, pharmacodynamic; AUEC28, area under the effect curve over 28 days; Emax, maximum effect; NPRS, numeric pain-rating scale; WBC, white blood cell.
Mean BPI-SF pain-severity score was 5.3±1.0 at T1 baseline and had reduced by day 28, when it was 4.0±1.9 (Figure 2B). A similar trend was seen with T2, with mean scores of 5.2±1.5 at baseline and 3.3±1.9 at day 28. At 28 days after T1, four of 19 subjects (21%) reported a reduction in BPI-SF pain-severity score ≥50% compared to baseline. At the same point after T2, six of 15 subjects had achieved this level of improvement compared with T2 baseline (40%).
As with the severity score, mean BPI-SF pain-interference score reduced from 5.8±1.7 at T1 baseline and remained lower through to day 28 after the T1 injection — 3.1±2.2 (Figure 2C). At day 28, ten of 19 subjects (53%) had had a reduction in this score ≥50% compared to baseline. At T2 baseline, mean BPI-SF pain-interference score was 4.7±2.0, and at day 28 remained lower at 2.5±2.2, including six of 15 subjects (40%) who had had reductions ≥50% compared with T2 baseline.
Discussion
Results of PD parameters in this study indicated that there was no clinically relevant difference in HPA suppression between the initial and repeat injections of a viscous gel formulation of dexamethasone.
AUEC28 T2:T1 ratios were close to 1 for all PD parameters, with 90% CIs being contained within the prespecified 80%–125% range, denoting no effect for any but cortisol. However, an additional cortisol-responder analysis showed that for both treatments, all subjects had their cortisol return to baseline within 3 days of injection. In addition, observation of mean WBC count and blood glucose over the treatment period showed that they all returned to baseline levels within a week of injection. Previous clinical data on the effect of epidural dexamethasone on cortisol also showed normalization within the first week after administration,20 though some other trials have noted longer periods of perturbation that ultimately resolved within 3 weeks.17,21 It is possible that different dosing may account for this variability. A further consideration is that the phase I/II bridging study included the same measures of HPA suppression, and while that study was not designed to detect differences in these parameters, results suggested that epidural SP-102 administration had similar effects to intravenous injection of standard dexamethasone sodium phosphate solution. Taken together, available data thus indicate that SP-102 can be used as frequently for ESI as standard dexamethasone solutions currently in use, at least in terms of potential concerns regarding HPA suppression.
The finding that repeat doses of SP-102 had comparable PD effects is of importance, as repeated ESIs have been shown to provide cumulative benefit to patients with lumbar radiculopathy.14,22 The improved analgesic effect in the repeat dose in this study lends further support to this treatment approach, which is borne out in clinical practice: repeat doses are relatively common in the pain clinic. One analysis of a quality-assurance database of 6,582 transforaminal ESIs in 4,161 patients with unilateral lumbar radicular pain showed that nearly a quarter of patients received repeat injections.14 A prospective trial in a slightly younger patient population showed that just under half thepatients required at least one repeat injection.12
SP-102 appeared to be well tolerated by the study subjects over this treatment period, with no serious AEs reported and two moderate AEs considered possibly related to the study drug. It could be speculated that the prolonged residence at the site of injection might reduce the frequency of acute corticosteroid side effects, as systemic release of dexamethasone is delayed and not as concentrated as with intravenous or epidural injections of standard solution. However, as already discussed, investigation of the systemic effects of SP-102 in terms of HPA suppression does not appear to support this idea and suggests that cortisol-suppression time is a function of total exposure, rather than peak concentration.
The limitations of this study include its small sample and relatively short duration, which are a result of its primary objective as an early phase I/II PD study and not unusual for this trial type. The small number of subjects meant that the Emax values calculated in this study were unable to give sufficient information for the intended analysis, given the variability between subjects: although the CIs tended to be outside the prespecified 80%–125% at both ends, ratios were close to 1 for all PD parameters except blood glucose, which was extremely variable. A larger sample would likely reduce the width of the CIs.
The pain data shown here are of interest for further study, indicating a prolonged analgesic effect of up to a month after a single injection, with AEUC28 ratios providing evidence of further improvement after a second injection for those who did not have an adequate initial response. The findings of this phase I/II study will be investigated further in an ongoing phase III, randomized, double-blind, placebo-controlled study (NCT03372161), which is designed to investigate the safety profile and efficacy of initial and single repeat injections of SP-102 in an anticipated 400 subjects.23
In conclusion, further research is needed, but results of this study show that a repeat dose of SP-102 has the same systemic effect on HPA suppression as the initial dose, with no evidence of cumulative/prolonged alterations in plasma cortisol, WBC count, or blood-glucose levels. Furthermore, there appeared to be a trend toward an additional analgesic effect with the second injection. These phase I/II results suggest that a repeat dose of SP-102 epidural injection could be used when clinically indicated to provide prolonged pain relief for lumbosacral radiculopathy, findings that are being further explored in an ongoing phase III clinical trial.
Acknowledgments
The authors thank Mark J Jaros PhD of Summit Analytical, Denver, CO, USA for providing statistical support for the study. The authors also thank Kalpana Patel, Scilex Pharmaceuticals Inc, and Elena Aruzumanyan for editorial support. Editorial and medical writing support was provided by Christine Elsner, Abigail Killen-Devine, and Kyle Lambe of Synergy Medical Communications, UK and funded by Scilex Pharmaceuticals, USA, in accordance with Good Publication Practice guidelines (http://www.ismpp.org/gpp3).24
Funding Statement
This study was supported by Scilex Pharmaceuticals Inc (formerly Semnur Pharmaceuticals Inc).
Data Sharing Statement
The authors certify that this manuscript reports original clinical trial data. Individual participant data that underlie the results reported in this article after deidentification (text, tables, and figures) are available, including the study protocol. Data requests should be submitted in the form of a research proposal to medical_affairs@scilexpharma.com for up to 36 months after the publication date.
Disclosure
CA reports employment with Scilex Pharmaceuticals Inc during the study and outside the submitted work. ES reports receiving consultancy fees from Scilex Pharmaceuticals Inc during the study. DL reports employment with Scilex Pharmaceuticals Inc during the study and outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318(5):291–300. doi: 10.1056/NEJM198802043180506 [DOI] [PubMed] [Google Scholar]
- 2.Frymoyer JW. Lumbar disk disease: epidemiology. Instr Course Lect. 1992;41:217–223. [PubMed] [Google Scholar]
- 3.Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007;99(4):461–473. doi: 10.1093/bja/aem238 [DOI] [PubMed] [Google Scholar]
- 4.Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007;334(7607):1313–1317. doi: 10.1136/bmj.39223.428495.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valat J-P, Genevay S, Marty M, et al. Sciatica. Best Pract Res Clin Rheumatol. 2010;24(2):241–252. doi: 10.1016/j.berh.2009.11.005 [DOI] [PubMed] [Google Scholar]
- 6.Cohen SP, Bicket MC, Jamison D, et al. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013;38(3):175–200. doi: 10.1097/AAP.0b013e31828ea086 [DOI] [PubMed] [Google Scholar]
- 7.MacVicar J, King W, Landers MH, et al. The effectiveness of lumbar transforaminal injection of steroids: a comprehensive review with systematic analysis of the published data. Pain Med. 2013;14(1):14–28. doi: 10.1111/j.1526-4637.2012.01508.x [DOI] [PubMed] [Google Scholar]
- 8.FDA drug safety communication. FDA requires label changes to warn of rare but serious neurologic problems after epidural corticosteroid injections for pain. 2014
- 9.Pountos I, Panteli M, Walters G, et al. Safety of epidural corticosteroid injections. Drugs R D. 2016;16(1):19–34. doi: 10.1007/s40268-015-0119-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Racoosin JA, Seymour SM, Cascio L, et al. Serious neurologic events after epidural glucocorticoid injection — the FDA’s risk assessment. N Engl J Med. 2015;373(24):2299–2301. doi: 10.1056/NEJMp1511754 [DOI] [PubMed] [Google Scholar]
- 11.Rathmell JP, Benzon HT, Dreyfuss P, et al. Safeguards to prevent neurologic complications after epidural steroid injections: consensus opinions from a multidisciplinary working group and national organizations. Anesthesiology. 2015;122(5):974–984. doi: 10.1097/ALN.0000000000000614 [DOI] [PubMed] [Google Scholar]
- 12.Kennedy DJ, Plastaras C, Casey E, et al. Comparative effectiveness of lumbar transforaminal epidural steroid injections with particulate versus nonparticulate corticosteroids for lumbar radicular pain due to intervertebral disc herniation: a prospective, randomized, double-blind trial. Pain Med. 2014;15(4):548–555. doi: 10.1111/pme.12325 [DOI] [PubMed] [Google Scholar]
- 13.Kim D, Brown J. Efficacy and safety of lumbar epidural dexamethasone versus methylprednisolone in the treatment of lumbar radiculopathy: a comparison of soluble versus particulate steroids. Clin J Pain. 2011;27(6):518–522. doi: 10.1097/AJP.0b013e31820c53e0 [DOI] [PubMed] [Google Scholar]
- 14.Murthy NS, Geske JR, Shelerud RA, et al. The effectiveness of repeat lumbar transforaminal epidural steroid injections. Pain Med. 2014;15(10):1686–1694. doi: 10.1111/pme.12497 [DOI] [PubMed] [Google Scholar]
- 15.Stout A, Friedly J, Standaert CJ. Systemic absorption and side effects of locally injected glucocorticoids. PM R. 2019;11:409–419. doi: 10.1002/pmrj.12042 [DOI] [PubMed] [Google Scholar]
- 16.Duan W, Shen X, Lei J, et al. Hyperglycemia, a neglected factor during cancer progression. Biomed Res Int. 2014;2014:461917. doi: 10.1155/2014/461917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedly JL, Comstock BA, Heagerty PJ, et al. Systemic effects of epidural steroid injections for spinal stenosis. Pain. 2018;159(5):876–883. doi: 10.1097/j.pain.0000000000001158 [DOI] [PubMed] [Google Scholar]
- 18.Ing VW. The etiology and management of leukopenia. Can Fam Physician. 1984;30:1835–1839. [PMC free article] [PubMed] [Google Scholar]
- 19.Vila G, Jørgensen JOL, Luger A, et al. Insulin resistance in patients with acromegaly. Front Endocrinol. 2019;10:509. doi: 10.3389/fendo.2019.00509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chutatape A, Menon M, Fook-Chong SMC, et al. Metabolic and endocrinal effects of epidural glucocorticoid injections. Singapore Med J. 2019;60(3):140–144. doi: 10.11622/smedj.2018140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maillefert JF, Aho S, Huguenin MC, et al. Systemic effects of epidural dexamethasone injections.. Rev Rhum. 1995;62(6):429–432. [PubMed] [Google Scholar]
- 22.Lee JH, Lee SH. Can repeat injection provide clinical benefit in patients with cervical disc herniation and stenosis when the first epidural injection results only in partial response? Medicine. 2016;95:e4131. doi: 10.1097/MD.0000000000004131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.ClinicalTrials.gov [Internet]. Bethesda(MD): National Library of Medicine (US). 2000 Feb 29. Identifier NCT03372161, Corticosteroid Lumbar Epidural Analgesia for Radiculopathy; 2017 Dec 13 [cited 2020 April 21]; [about 4 screens].Available from: https://clinicaltrials.gov/ct2/show/NCT03372161. Accessed April21, 2020.
- 24.Battisti WP, Wager E, Baltzer L, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med. 2015;163(6):461–464. doi: 10.7326/M15-0288 [DOI] [PubMed] [Google Scholar]