Abstract
Purpose:
To assess the magnitude of benefit to early treatment initiation, enabled by newborn screening or prenatal diagnosis, in patients with cross-reactive immunological material (CRIM)-negative infantile Pompe disease (IPD), treated with enzyme replacement therapy (ERT) and prophylactic immune tolerance induction (ITI) with rituximab, methotrexate, and IVIG.
Methods:
A total of 41 CRIM-negative IPD patients were evaluated. Amongst patients who were treated with ERT+ITI (n=30), those who were invasive ventilator-free at baseline and had ≥6 months of follow-up were stratified based on age at treatment initiation: 1) early (≤4 weeks), 2) intermediate (>4 and ≤15 weeks), and 3) late (>15 weeks). A historical cohort of 11 CRIM-negative patients with IPD treated with ERT monotherapy served as an additional comparator group.
Results:
Twenty patients were included; five, seven, and eight in early, intermediate, and late treatment groups, respectively. Genotypes were similar across the three groups. Early-treated patients showed significant improvements in left ventricular mass index, motor and pulmonary outcomes, as well as biomarkers creatine kinase and urinary glucose tetrasaccharide, compared to those treated later.
Conclusion:
Our preliminary data suggest that early treatment with ERT+ITI can transform the long-term CRIM-negative IPD phenotype, which represents the most severe end of the Pompe disease spectrum.
INTRODUCTION
Pompe disease (OMIM #232300, glycogen storage disease II) is an autosomal recessive disorder caused by pathogenic variants in the GAA gene, resulting in a deficiency of enzyme acid α-glucosidase (GAA) and accumulation of lysosomal glycogen in cardiac, skeletal, and smooth muscles1. Classic infantile Pompe disease (IPD) is characterized by progressive muscle weakness, hypertrophic cardiomyopathy, and eventually respiratory insufficiency, leading to death due to cardiac and/or respiratory failure prior to one year of age2,3. The advent of enzyme replacement therapy (ERT) with recombinant human acid α-glucosidase (rhGAA, alglucosidase alfa) drastically transformed the natural history of the disease, allowing prolonged survival and improving cardiac and motor outcomes4–6. However, patient outcomes on ERT vary due to factors such as cross-reactive immunological material (CRIM) status5,7–9, the development of anti-rhGAA immunoglobulin G (IgG) antibodies5,10–12, age at ERT initiation6,13–15, dose of ERT16–18, as well as severe cardiac involvement, invasive ventilation, and failure to thrive at baseline19.
CRIM-negative IPD patients have two null variants in the GAA gene that result in a complete inability to produce native enzyme7. These patients respond poorly to ERT due to the development of high and sustained anti-rhGAA IgG antibody titers (HSAT; defined as ≥51,200 at or beyond 6 months on ERT) or sustained intermediate titers (SIT; defined as ≥12,800 and <51,200)10,12. CRIM-positive IPD patients produce some amount of endogenous GAA and are therefore typically expected to produce low anti-rhGAA IgG antibody titers (LT; defined as ≤6,400), and exhibit a better response to ERT9,19. While a subset of CRIM-positive IPD patients also develop HSAT leading to poor clinical outcomes20, it is well-recognized that CRIM-negative status is associated with significant immunological challenges, earlier symptom onset, a more aggressive disease course, and poorer survival7,19.
In order to prevent and/or mitigate the detrimental effects of anti-rhGAA IgG antibodies, several approaches to immune modulation, both prophylactic and therapeutic, have been attempted in patients with IPD21. A short, five-week course of immune tolerance induction (ITI) with rituximab, methotrexate, and intravenous immunoglobulin (IVIG) in the ERT-naïve setting has been shown to induce immune tolerance to ERT in the largest cohort of patients with IPD, leading to significantly improved overall survival and reduced cardiomyopathy, and is now considered the optimal approach for the treatment of CRIM-negative IPD22–25.
Initiation of ERT at an early age can also improve treatment outcomes by intervening in the early stages of the disease, prior to extensive involvement and loss of tissue function. Amongst IPD patients diagnosed via newborn screening (NBS) in Taiwan, of whom all were CRIM-positive, early treatment with ERT within the first month of life led to improved long-term clinical outcomes including independent walking and ventilator-free survival26. The extent of these benefits in CRIM-positive patients has been shown to increase with even earlier initiation of ERT (within the first few days of life)15. Additionally, increasing evidence suggests that the administration of ERT doses higher than the standard 20 mg/kg every other week (EOW) can improve long-term clinical outcomes in patients with IPD16,18,27.
While prophylactic ITI and early ERT initiation are beneficial, the extent of these benefits is not well-characterized in CRIM-negative IPD, the most severe Pompe disease phenotype. The purpose of this study was to assess the benefit of early ERT+ITI treatment in CRIM-negative patients with IPD.
PATIENTS AND METHODS
Patients and Inclusion Criteria
A retrospective chart review of an international pediatric Pompe cohort was conducted. Patients were selected based on the following inclusion criteria: (a) confirmed diagnosis of CRIM-negative IPD4, 28; (b) prophylactic ITI with rituximab, methotrexate, and IVIG as previously published22,23; (c) ERT at a cumulative dose of 20–40 mg/kg weekly or EOW; (d) not invasively ventilated at baseline; and (e) ≥6 months of follow-up data available. Invasively ventilated patients were excluded to eliminate potential selection bias due to disproportionately higher risk of ventilator-dependence and/or death at follow-up. Eligible patients were stratified based on age at ERT+ITI: 1) early treatment group (ETG, ≤4 weeks), 2) intermediate treatment group (ITG, >4 and ≤15 weeks), and 3) late treatment group (LTG, >15 weeks). A previously reported cohort of CRIM-negative IPD patients treated with ERT monotherapy and not invasively ventilated at baseline served as an additional comparator group7.
Data Collection and Analysis
Clinical data including GAA pathogenic variants, age and doses of ERT+ITI treatment, overall and invasive ventilator-free survival, left ventricular mass index (LVMI), feeding status, motor status, creatine kinase (CK), urinary glucose tetrasaccharide (Glc4), and anti-rhGAA IgG antibodies were extracted from medical records provided by each patient’s principal care provider. CRIM status, anti-rhGAA IgG antibody titers, and urinary Glc4 were determined as previously described, 4,22,28,29. The upper limit of normal urinary Glc4 was determined to be the 95th percentile of age-matched controls (20 mmol/mol creatinine, 0–6 months; 14 mmol/mol creatinine, 6–12 months; 8.3 mmol/mol creatinine, 1–3 years; 3.0 mmol/mol creatinine, >3 years)30. LVMI was measured using 2D, M-mode, and/or Doppler echocardiography. Data collection was completed on December 1st, 2019 or when at least six months of follow-up were available.
Lifelong average dose of ERT was calculated using a previously published method, averaging the product between the proportion of time the patient spent on each dose, and a multiplier relative to the standard labeled dose (e.g. both 20 mg/kg W and 40 mg/kg EOW are assigned a multiplier of 2, as they are twice the standard dose of 20 mg/kg EOW)31. In addition to Kaplan-Meier analysis of invasive ventilator-free survival outcomes, pulmonary outcomes were described in terms of the type of ventilation required, and the three groups were compared in terms of the likelihood of requiring either invasive or non-invasive ventilation by the time of final assessment. Comparisons of LVMI measurements were made at baseline and final assessment, and longitudinal LVMI was assessed for time to normalization. Feeding status was described in terms of oral feeding or use of any feeding support such as nasogastric tube (NG-tube) or gastrostomy tube (G-tube). Motor status was described as either ambulatory or non-ambulatory, and/or whether age-appropriate developmental milestones were achieved. The likelihood of achieving independent ambulation and the likelihood of oral feeding by the time of final assessment were compared across the three groups. CK and urinary Glc4 values were compared at baseline and six months on ERT and observed for differences in longitudinal trends beyond six months. Longitudinal anti-rhGAA IgG antibody titers were assessed for peak titers; patients were classified as being immune tolerant (LT or seronegative), SIT, or HSAT.
In the ERT monotherapy comparator group, overall and invasive ventilator-free survival, anti-rhGAA IgG antibodies, and LVMI were evaluated as available. To determine the outcomes of ERT+ITI, ETG, ITG, and LTG were combined and compared to the ERT monotherapy group.
Statistics
Data were described using n (%) and median (minimum-maximum) as appropriate. The Kaplan-Meier method was used to analyze overall and ventilator-free survival data with the log-rank test to generate 2-tailed P-values. Comparisons of continuous variables were conducted using the Wilcoxon/Kruskal-Wallis rank-sum test32. Chi-square tests of independence were used to determine the significance of categorical factors. Statistical analyses were conducted in JMP® Pro version 1533.
RESULTS
Patient demographics and treatment details (Table 1)
Table 1.
Patient demographics and treatment details
| Patient ID | Median age in weeks at ERT initiation (range) |
ERT Dose at Initiation (mg/kg)a | ERT Dose at Final Assessment (mg/kg)a | Lifelong Average Dose | Alive or deceased at final assessment | Median age in months at final assessment (range) | Race/Ethnicity | GAA Pathogenic Variants | |
|---|---|---|---|---|---|---|---|---|---|
| Allele 1 | Allele 2 | ||||||||
| Early Treatment Group (n=5) | |||||||||
| E1 | 2.1 (0.3–3.4) |
20 EOW | 40 EOW | 1.38 | Alive | 28.3 (9.3–51.8) |
Hispanic | c.2560C>T | c.2560C>T |
| E2 | 40 EOW | 40 EOW | 2.00 | Alive | Caucasian/African American | c.525delT | c.2560C>T | ||
| E3 | 20 EOW | 40 EOW | 1.57 | Alive | Caucasian | c.1051delG | c.1579delA | ||
| E4 | 20 EOW | 40 EOW | 1.04 | Alive | Caucasian | c.525delT | c.525delT | ||
| E5 | 20 EOW | 40 W | 1.75 | Alive | Caucasian, Hispanic | c.1827C>G | c.2662G>T | ||
| Intermediate Treatment Group (n=7) | |||||||||
| I1 | 7.6 (4.4–13.3) |
20 EOW | 40 EOW | 1.32 | Alive | 83.4 (21.4–113.3) |
Caucasian, Hispanic | c.525delT | c.1694_1697delTCTC |
| I2 | 20 EOW | 40 EOW | 1.38 | Alive | Caucasian/African American | c.525delT | c.2560C>T | ||
| I3 | 20 EOW | 40 W | 2.29 | Alive | African American/Hispanic | c.2560C>T | c.2560C>T | ||
| I4 | 20 EOW | 40 W | 2.98 | Alive | African American | c.1754+2T>A | c.1822C>T | ||
| I5 | 20 EOW | 40 EOW | 1.39 | Alive | Caucasian | c.236_246del | c.236_246del | ||
| I6 | 20 EOW | 40 W | 1.17 | Alive | Hispanic | c.2608C>T | c.2608C>T | ||
| I7 | 20 EOW | 30 W | 2.05 | Alive | Caucasian | c.258dupC | c.2227C>T | ||
| Late Treatment Group (n=8) | |||||||||
| L1 | 17.9 (15.4–28.3) |
20 EOW | N/A | N/A | Deceased | 49.7 (15.0–135.5) |
Caucasian | c.1548G>A | c.525delT |
| L2 | 40 EOW | 40 W | 3.93 | Alive | Caucasian/Native American/African American | c.2560C>T | c.525delT | ||
| L3 | 20 EOW | 40 EOW | 1.25 | Alive | Caucasian | c.340_341insT | c.340_341insT | ||
| L4 | 20 EOW | 20 EOW | 1.00 | Deceased | African American | c.2560C>T | c.2560C>T | ||
| L5 | 20 EOW | 40 EOW | 1.86 | Alive | Caucasian, Hispanic | c.1195–18_2190–20del | c.1195–18_2190–20del | ||
| L6 | 20 EOW | 20 EOW | 1.00 | Alive | African American | c.546+2T>C | c.546+2T>C | ||
| L7 | 20 EOW | 20 EOW | 1.00 | Alive | Caucasian/African American | c1548G>A | c2560C>T | ||
| L8 | 20 EOW | 20 EOW | 1.00 | Alive | Caucasian/Asian | c.2237G>A | c.437delT | ||
For consistency, ERT doses of 20 mg/kg weekly were considered the same as those who received 40 mg/kg every other week.
GAA: gene encoding enzyme acid alpha-glucosidase; F: Female; M: Male; EOW: every other week; W: weekly; ERT, enzyme replacement therapy; N/A: not available.
In the international pediatric Pompe cohort, 30 CRIM-negative IPD patients received ERT+ITI with rituximab, methotrexate, and IVIG. No other immunomodulatory regimens were administered in the ERT-naïve setting. Ten patients were excluded due to invasive ventilation at baseline (n=8) or insufficient follow-up (n=2), leaving 20 patients for inclusion and analysis. These patients were further stratified into the ETG (n=5), ITG (n=7), and LTG (n=8). The historical ERT monotherapy cohort consisted of 11 CRIM-negative patients.
Median age at ERT initiation was 2.1 weeks (0.3–3.4 weeks), 7.6 weeks (4.4–13.3 weeks), and 17.9 weeks (15.4–28.3 weeks) in the ETG, ITG, and LTG, respectively. Three ETG patients were diagnosed via NBS and the two remaining were diagnosed prenatally. Two ITG patients were diagnosed via NBS and the remaining five were diagnosed by clinical symptomology. All LTG patients were diagnosed by clinical symptomatology. In the ERT monotherapy group, median age at ERT initiation was 13.0 weeks (1.1–30.4 weeks).
Of all GAA variants (n=40) in the accumulated cohort of patients treated with ERT+ITI, 25.0% (n=10) were the common African American GAA variant c.2560C>T, which accounted for 3/10 (30.0%), 3/14 (21.4%), and 4/16 (25.0%) of variants in the ETG, ITG, and LTG, respectively34. Genotypes were similar in the ERT monotherapy group7.
All patients were initiated on the standard cumulative ERT dose of 20 mg/kg EOW except for patients E2 and L2, who began ERT at 40 mg/kg EOW (Table 1). None of the other patients (n=18) transitioned to a higher dose of ERT within the first six months (Figure S1A). The median lifelong average dosage of ERT was 1.57 (1.04–2.01), 1.39 (1.17–2.98), and 1.00 (1.00–3.93) in the ETG, ITG, and LTG respectively, with no significant difference between groups. There was no significant difference in age or time on ERT at dose escalation across the three groups (Figure S1B).
Overall and invasive ventilator-free survival
All five ETG patients (100%) and all seven ITG patients (100%) were alive at median ages of 28.3 months (9.3–51.8 months) and 83.4 months (21.4–113.3 months), respectively. 6/8 LTG patients (75.0%) were alive at a median age of 49.6 months (28.1–135.5 months). Patients L1 and L4 were deceased at 56.9 months and 15.0 months respectively; in both cases, the cause of death was respiratory failure due to disease progression. No statistical difference (p=0.135) in overall survival was found between ETG, ITG, and LTG (Figure 1A). Patients treated with ERT+ITI exhibited significantly prolonged overall survival than those treated with ERT monotherapy (P<0.0001), who were all deceased at a median age of 28.8 months (18.0–50.2 months) (Figure 1C).
Figure 1. Kaplan-Meier survival analysis of CRIM-negative IPD patients treated with ERT monotherapy compared to those treated ERT+ITI (combined and by individual groups).
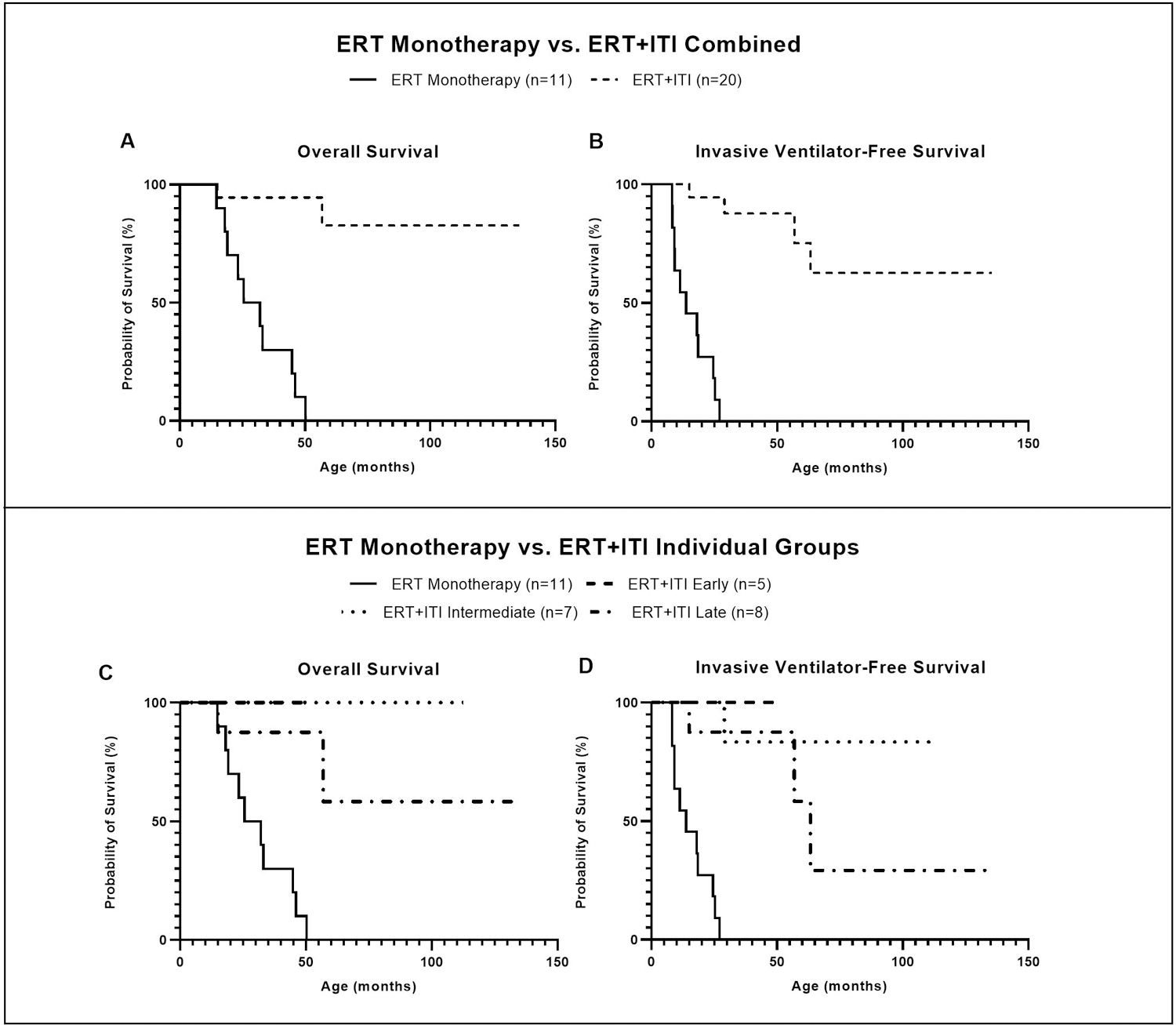
A & B) Comparison of overall and invasive ventilator-free survival in all patients treated with ERT+ITI (n=20) versus those treated with ERT monotherapy (n=11). Both overall and invasive ventilator-free survival were significantly prolonged in patients treated with ERT+ITI (p<0.0001). C & D) Comparison of overall and invasive ventilator-free survival in early (n=5), intermediate (n=7), and late (n=8) treatment groups, and the ERT monotherapy group (n=11).
As defined by the inclusion criteria, none of the patients were invasively ventilated at baseline (Table 2). All five ETG patients (100%) remained invasive ventilator-free throughout the course of ERT, and none required non-invasive ventilation such as BiPAP or CPAP. 6/7 ITG patients (85.7%) and 6/8 LTG patients (75.0%) remained invasive ventilator-free. Patients I4, L4, and L6 became invasive ventilator-dependent at age 29.0 months, 15.0 months, and 63.3 months, respectively. Additionally, three ITG patients (I1, I3, I7) and two LTG patients (L5, L8) required either BiPAP, CPAP, or cough assist vest. There was no significant difference in invasive ventilator-free survival between groups (p=0.158) (Figure 1B). However, compared to the ETG, use of either invasive or non-invasive ventilation was significantly more likely in both the ITG (p=0.034) and the LTG (p=0.044). Invasive ventilator-free survival was significantly improved in patients treated with ERT+ITI, compared to the ERT monotherapy group (P<0.0001), who were all deceased and/or ventilator-dependent at a median age of 13.8 months (8.2–27.1 months) (Figure 1D).
Table 2.
Clinical outcomes in CN IPD patients treated with ERT+ITI
| Patient ID | LVMI (g/m2) | Ventilation Status | Motor Status | Feeding Status | ||||
|---|---|---|---|---|---|---|---|---|
| Base-line | Follow-up (weeks on ERT) | Baseline | Follow-up (weeks on ERT) | Baseline | Follow-up (weeks on ERT) | Baseline | Follow-up (weeks on ERT) | |
| Early Treatment Group (n=4) | ||||||||
| E1 | 65.4 | 58.8 (48)a | CPAP for a week | No support (221) | Head lag, central hypotonia | Ambulating independently (221) | Oral | Oral (221) |
| E2 | 55.5 | 46.4 (35) | No support | No support (27) | Age appropriate gross motor skill developmentc | Meeting developmental milestones (27) | Oral | Oral (27) |
| E3 | 158.0 | 46.0 (47) | No support | No support (156) | AIMS percentile rank <5%, delayed milestonesd | Active with walking, running and jumping. 25th percentile on Peabody locomotion test (88) | Oral | Oral (156) |
| E4 | 173.3 | 41.4 (26) | Oxygen | No support (33) | AIMS percentile rank 11%–25% | N/A | Oral | Oral (33) |
| E5 | NAb | 63.0 (163) | No support | No support (162) | NA | Ambulatory, normal developmental milestones (162) | Oral | Oral (162) |
| Intermediate Treatment Group (n=7) | ||||||||
| I1 | 180.4 | 80.4 (23) | No support | Overnight BiPAP (59) | Hypotonia | Generalized hypotonia, unable to bear weight. AIMS Score <1 percentile rank for age (50) | NG Tube | G Tube (59) |
| I2 | 156.2 | 60.2 (141) | No support | No support (101) | Mild hypotonia | Ambulatory, meeting normal developmental milestones (101) | Oral | Oral (101) |
| I3 | 140.6 | 53.8 (252) | No support | CPAP with nasal mask (199) | Motor status and milestones appropriate for her age | Ambulatory (224) | Oral | Oral (213) |
| I4 | 84.0 | 53.5 (217) | No support | Invasively ventilated (204) | Hypotonia | Not ambulatory. Can raise hands to mouth, holds head up, sits with and without support (211) | Oral | Oral (204) |
| I5 | 277.0 | 80.0 (334) | Oxygen | No support (76) | Severe hypotonia, floppy baby, no head or neck control | Ambulates independently (76) | NG Tube | Oral (76) |
| I6 | 160.3 | 57.8 (437) | Oxygen | No support (450) | Head lag, severe hypotonia, motor delay | Ambulates unassisted, wheelchair as needed mostly for transportation (450) | NG Tube | Oral (450) |
| I7 | 156.7 | 53.8 (208) | No support | Vest/cough assist (273) | Hypotonia | Ambulatory (273) | Oral | Oral (273) |
| Late Treatment Group (n=8) | ||||||||
| L1 | 440.0 | 257.0 (63) | Transient ventilation for 3 days | No support (67) | Hypotonia | Not ambulatory. Prop-sit independently, sits briefly without hand support, rolls from supine to side lying, bears weight through lower extremities in supported standing (80) | Oral | Oral (80) |
| L2 | 433.1 | 67.6 (169) | No support | No support (169) | Normal symmetric bulk, appeared to have normal tone | Not ambulatory (169) | Oral | Primarily G tube with some oral intake (169) |
| L3 | NA | NA | No support | No support (378) | Hypotonia | Ambulatory (378) | Oral | Oral (378) |
| L4 | 220.0 | 83.0 (39) | No support | Invasively ventilated (46) | Unable to independently hold head or sit unsupported | Not able to independently hold head or sit unsupported (46) | NG Tube | GJ Tube (46) |
| L5 | 448.9 | 62.7 (185) | Requires nasal O2 | Recommended CPAP at night, severe OSA (195) | Delayed motor milestones | Ambulatory (195) | Oral and NG Tube | Oral, used G tube for first 2 years on ERT (195) |
| L6 | 445.8 | 68.0 (274) | Oxygen and BiPAP at night | Invasively ventilated (271) | Head lag, antigravity movements arms> legs | Not ambulatory. Can move arms against gravity (286) | NG tube | G Tube (271) |
| L7 | 211.9 | 192.5 (26) | No support | No support (136) | Mild hypotonia, delayed head control at 3 months but rolling | Ambulatory. Walks, runs, jumps, feeds self, plays with siblings, dresses self, walks up stairs (136) | NG tube | NG tube and oral (136) |
| L8 | 176.0 | 48.0 (105) | BiPAP | BiPAP (92) | Hypotonia | N/A | G tube | G Tube (92) |
LVMI: left ventricular mass index; CPAP: continuous positive airway pressure; BiPAP: bilevel positive airway pressure; N/A: not available; NG tube: nasogastric tube; G tube: gastrostomy tube; GJ tube: gastrostomy-jejunostomy tube; AIMS: Alberta Infantile Motor Scale; OSA: obstructive sleep apnea; ERT: enzyme replacement therapy
Echocardiographs have shown normal cardiac structure and function throughout 221 weeks of follow-up; LVMI calculations not available beyond 48 weeks on ERT
Baseline echocardiograph indicated moderate biventricular hypertrophy
Assessed at 19 days on ERT
Assessed at 3 weeks on ERT
Cardiac Function: LVMI
At a median age of 0.9 weeks (0.0–3.3 weeks), the ETG had a median baseline LVMI of 111.7 g/m2 (55.5–173.3 g/m2, n=4). At a median age of 8.9 weeks (4.0–13.0 weeks), the ITG had baseline LVMI of 158.5 g/m2 (140.6–180.4 g/m2, n=7). The LTG had a baseline median LVMI of 433.1 g/m2 (176–448.9 g/m2, n=7), measured at a median age of 18.6 weeks (14.1–25.3 weeks), which was significantly higher than both the ETG (p=0.011) and the ITG (p=0.011) (Figure 2A).
Figure 2. LVMI in CRIM-negative IPD patients treated with ERT+ITI at baseline and final assessment.
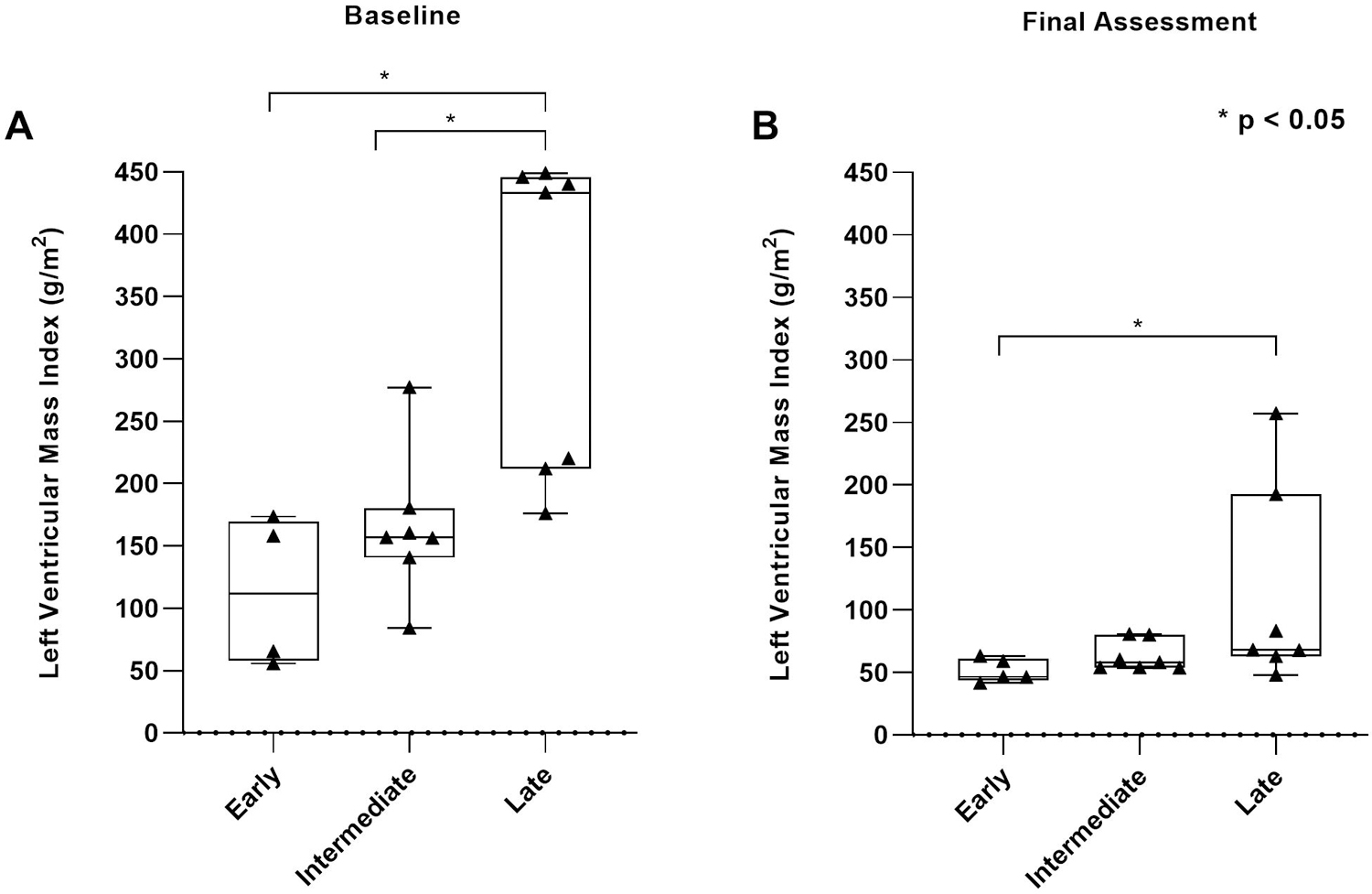
A) Comparison of LVMI (g/m2) in ETG (n=4), ITG (n=7), and LTG (n=7) at baseline; B) Comparison of LVMI (g/m2) in ETG (n=5), ITG (n=7), LTG (n=7) at final assessment. Upper limit of normal range is 64.0 g/m2.
In the ETG, median LVMI was 46.4 g/m2 (41.4–63.0 g/m2, n=5) at a median follow-up time of 47.0 weeks on ERT (26–163 weeks) (Table 2). The ITG and LTG had median LVMI of 57.8 g/m2 (53.5–80.4 g/m2, n=7) and 68.0 g/m2 (48.0–257.0 g/m2, n=7) at median follow-up times of 217 weeks (23–437 weeks) and 105 weeks (26–274 weeks), respectively. LVMI at final assessment was significantly higher in the LTG than in the ETG (p=0.023); there was no significant difference between ETG and ITG (Figure 2B). Although LVMI decreased in all patients, two ITG patients (I1, I5) and three LTG patients (L1, L4, L7) had LVMI above the normal range of 64.0 g/m2 at final assessment35. By 21 weeks on ERT, LVMI was normalized in all ETG patients; only one ITG patient (I4) and one LTG patient (L8) had normalized LVMI within this period.
Feeding Status
All five ETG patients (100%) remained on oral feeds from baseline throughout the course of ERT (Table 2). Four ITG patients (57.1%; I2, I3, I4, I7) were feeding orally throughout the study period. Patients I1, I5, and I6 required NG-tube feeds at baseline; at final assessment, patients I5 and I6 had transitioned to oral feeds, whereas patient I1 still required a G-tube. In the LTG, two patients (25.0%; L1 and L3) remained on oral feeds. Patient L2 fed orally at baseline, yet required G-tube at final assessment. Four patients (L4, L5, L6, L7) required NG-tube and one patient (L8) required G-tube at baseline; patient L5 was able to transition to oral feeds by final assessment, whereas patients L4, L6, L7, and L8 required either NG-tube, G-tube, or gastrostomy-jejunostomy tube (GJ-tube). Early-treated patients were significantly less likely to require enteral feeding support at final assessment than those in the LTG (p=0.009).
Motor Status
Follow-up motor status was available for 4/5 early-treated patients, of whom all (100%) were independently ambulatory or meeting age-appropriate developmental milestones. By comparison, 5/7 ITG patients (71.4%) were independently ambulatory. In the LTG, follow-up motor status was available for 7/8 patients, of whom only three (42.9%) were independently ambulatory at final assessment. In the ETG, independent ambulation was significantly more likely than in the LTG (p=0.028) and nearly significantly more likely than in the ITG (p=0.052).
Biomarkers: CK and Urinary Glc4
At baseline, median CK measurements were elevated at 826.5 U/L (738–1877 U/L) in the ETG (n=4), 619 U/L (338–846 U/L) in the ITG (n=6), and 907 U/L (773–1002 U/L) in the LTG (n=5), with no significant difference between groups. At six months on ERT, all five patients in the ETG achieved normalized CK (median 178.0 U/L, 87–258 U/L), relative to the upper limit of normal range (320 U/L; age 0 to 9 years). In contrast, median CK decreased but did not normalize in any ITG patients (551.5 U/L, 344–2071 U/L), with four patients exhibiting increasing trends. In the LTG, CK remained abnormally elevated (median 969.5 U/L, 665–2255 U/L). There was significant improvement in the ETG compared to both ITG (p=0.020) and LTG (p=0.020).
Baseline urinary Glc4 was significantly more elevated (p=0.037) in the LTG (n=6, median 48.4 mmol/mol creatinine; 40.2–59.7 mmol/mol creatinine) than in the ITG (n=5, median 28.7 mmol/mol creatinine, 22.8–39.6 mmol/mol creatinine), and substantially more elevated (p=0.052) than in the ETG (n=3, median 20.6 mmol/mol creatinine, 13.9–25.6 mmol/mol creatinine). At six months on ERT, urinary Glc4 was within normal range in all five ETG patients (median 5.9 mmol/mol creatinine, 3.1–9.1 mmol/mol creatinine) 30,36. This was significantly lower (p=0.014) than in the LTG (median 22.8 mmol/mol creatinine, 8.4–40.8 mmol/creatinine) and not significantly lower (p=0.074) than in the ITG (median 13.9 mmol/mol creatinine, 8.4–27.1 mmol/mol creatinine).
The ETG continued to exhibit improved and relatively stable longitudinal trends for CK and urinary Glc4 levels beyond the first six months, whereas the ITG and LTG showed persistent CK and Glc4 elevation and greater fluctuation over time, with a number of patients showing increasing trends in both parameters (Figure 3).
Figure 3. Longitudinal CK and Urinary Glc4 in CRIM-negative IPD patients treated with ERT+ITI.
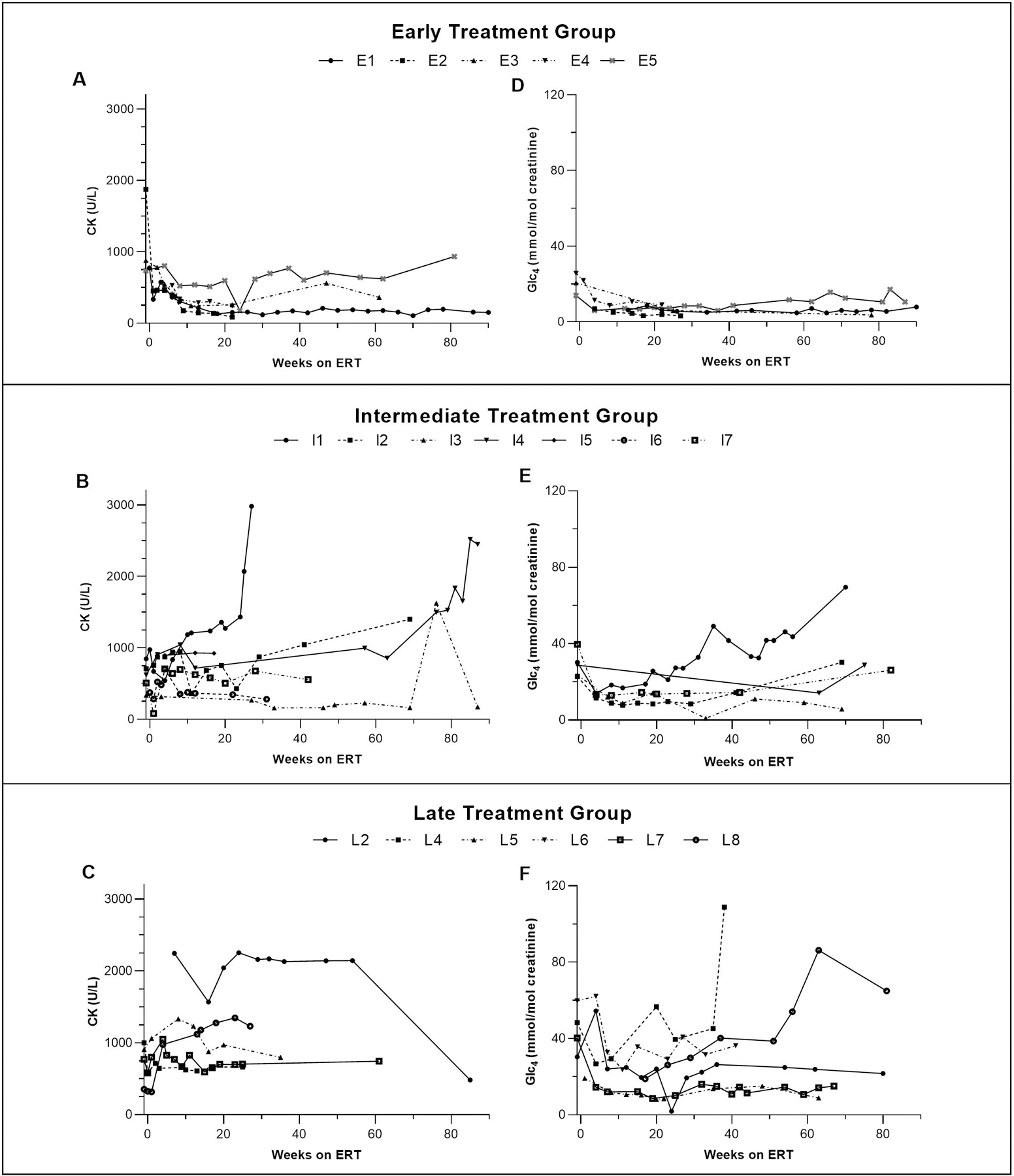
A-C: CK in early, intermediate, and late treatment groups, respectively. D-F: urinary Glc4 in early, intermediate, and late treatment groups, respectively. The early treatment group exhibited continued stable trends in both CK and urinary Glc4 at or near normal range (CK upper limit of normal: 320 U/L, age 0–9 years; Glc4 upper limit of normal: 20 mmol/mol creatinine, age 0–6 months; 14 mmol/mol creatinine, age 6–12 months; 8.3 mmol/mol creatinine, age 1–3 years; 3.0 mmol/mol creatinine, age >3 years). Persistent elevation of biomarkers was seen in both intermediate and late treatment groups with a number of patients exhibiting worsening trends over time. This pattern is consistent with previously reported findings in long-term survivors of IPD.
Anti-rhGAA IgG Antibodies
All five ETG patients (100%) remained immune tolerant to ERT with a median follow-up duration of 31 weeks (28–174 weeks). 5/7 ITG patients (71.4%) remained immune tolerant to ERT with four (I1, I2, I5, I6) remaining seronegative and one (I3) maintaining LT. Patient I7 developed SIT, yet subsequently became immune tolerant without any further immune modulation; patient I4 developed HSAT. All LTG patients (100%) were immune tolerant to ERT with two (L1, L6) remaining seronegative, and six (L2, L3, L4, L5, L7, L8) maintaining LT. The number of immune tolerant patients did not differ significantly between groups, yet ETG patients were significantly more likely to remain seronegative than those in both the ITG (p=0.047) and LTG (p=0.003).
In contrast to CRIM-negative IPD patients treated with ERT monotherapy, of whom median peak titer was 204,800 (n=10, 25,600–1,638,400), patients treated with ERT+ITI had significantly lower median peak titer of 0 (n=20, 0–51,200) (p<0.0001) (Figure S2).
DISCUSSION
This study in the largest reported cohort of CRIM-negative IPD patients illustrates significant improvements in overall clinical outcomes in those who were treated with ERT+ITI within the first month of life, compared to those treated at a later age. All ETG patients were alive at final assessment without need of any respiratory assistive device or enteral feeding, had normal cardiac function, met age-appropriate developmental milestones, and were immune tolerant to ERT. This clinical picture represents a drastically transformed phenotype from what has historically been the expected clinical course for patients with CRIM-negative IPD, who were all either deceased or invasive ventilator-dependent by 27.1 months of age7.
The differences in clinical outcomes based on age at ERT+ITI initiation are likely attributed to more extensive involvement and increased disease burden at baseline in late-treated IPD patients. Histologic response may be improved with earlier treatment initiation, as lower glycogen content at baseline is associated with more sustained post-treatment glycogen clearance37. For example, significantly elevated baseline LVMI in the LTG coincided with significantly higher LVMI at final assessment and delayed normalization of median LVMI when compared to the ETG, likely due to the development of more severe cardiomyopathy prior to treatment initiation. Additionally, 66% (10/15) of patients in ITG and LTG required an assistive breathing device during the course of treatment. As the primary cause of death in IPD is cardiorespiratory failure3, early intervention with ERT+ITI is essential to halt the progression of cardiac involvement and ensure invasive ventilator-free survival.
A similar pattern is present upon comparison of feeding status. None of the patients in the ETG required feeding support throughout the study period, whereas in ITG and LTG patients, 53.3% (8/15) and 40.0% (6/15) required enteral feeding at baseline and at study end, respectively. This is consistent with previous reports suggesting that IPD patients who required non-oral feeding support under six months of age go on to require long-term non-oral feeding support38. Although ERT has been shown to improve dysphagia in certain individuals39, our findings suggest that early intervention prior to onset of severe muscle weakness may prevent the need for enteral feeding, hence improving the long-term prognosis and quality of life.
Longitudinal biomarker data in early-treated patients show a trend that is distinct from those treated at a later age. While abnormal elevation of baseline Glc4 and CK was seen in all three groups, early-treated patients showed normalization of these parameters within the first six months, with continued stability throughout the duration of follow-up. The trend of persistent elevation in biomarker levels observed in the ITG and LTG is consistent with what has been previously described in long-term survivors of IPD9. Because both Glc4 and CK offer a quantitative assessment of long-term muscle damage as a result of glycogen accumulation in Pompe disease36, the observed biomarker trend suggests that early treatment may alleviate some the clinical challenges that are currently seen in long-term IPD survivors.
Another factor that may have played a role in these clinical improvements is the dose of ERT administered. Long-term survivors of IPD initially respond well to ERT at the standard dose of 20 mg/kg EOW, yet may exhibit clinical plateau and subsequent decline noted at 20–24 months on ERT9,26. Increasing evidence in clinically diagnosed CRIM-positive IPD patients who were immune tolerant or had low antibody titers to ERT suggests that some of these complications can be addressed by increasing ERT doses up to 40 mg/kg weekly16,27. The benefits of higher ERT dose include improvement of muscle function, cardiac status, and ventilator-free survival, as well as a significant reduction in biomarkers, such as urinary Glc4, suggesting efficient tissue glycogen clearance16–18,27. Of note, a recent report has also demonstrated the importance of early initiation of higher ERT doses, prior to biomarker changes, which typically precede clinical deterioration31. Additionally, increased ERT doses have been safely tolerated with no significant changes to anti-rhGAA IgG antibody response16. In this study, those who received higher lifelong average ERT doses in the LTG remained invasive ventilator-free throughout the study period and had comparatively less severe disease burden than those receiving the standard dose. However, their outcomes were not as ideal as those in the ETG group, particularly in terms of cardiac, motor, and biomarker parameters. Our findings expand upon previous reports to suggest that the significant clinical benefits brought upon by early ERT+ITI initiation may be further enhanced by increasing the ERT dose in CRIM-negative IPD patients.
Compared to the historical ERT monotherapy cohort, who were initiated on ERT at a similar range of ages and were invasive ventilator-free at baseline, patients treated with ERT+ITI exhibit significantly prolonged survival, reduced cardiomyopathy, and significantly attenuated anti-rhGAA IgG antibody response. Additionally, despite being excluded from analysis, patients with less than six months of follow-up data (n=3), including one patient who was treated within the first month of age, were reviewed for survival and safety of ITI to eliminate selection bias; none were deceased or experienced adverse events related to ITI administration. We have reported the long-term ITI safety outcomes of 25 CRIM-negative and 9 CRIM-positive IPD individuals, including all patients in the present study, demonstrating normal CD19%, adequate immune humoral response post-rituximab, and absence of any serious sequelae or deaths related to ITI administration40.
Our data suggest that the first few weeks after birth may be a critical period in newborns with CRIM-negative IPD, during which clinical symptoms may not yet be fully apparent, but timely treatment initiation can result in drastically improved clinical outcomes. The long-term prognosis of Taiwanese CRIM-positive IPD patients diagnosed via NBS and treated within the first 34 days of life has shown significantly improved overall and invasive ventilator-free survival compared to both clinically diagnosed patients and untreated patients, with all patients ambulating independently26. Although early intervention is also expected to yield significant clinical benefits in the CRIM-negative IPD population, who have significant immunological challenges and represent the most severe end of the Pompe disease spectrum, the extent and nature of these benefits has not been well-characterized. Our study expands upon previous findings to provide insight into an emerging, early-treated CRIM-negative phenotype with distinct characteristics, highlighting the importance of NBS and early treatment initiation in CRIM-negative IPD. One limitation of the study is the relatively young age and small sample size of the ETG. Although clinical plateau and/or deterioration may occur in long-term survivors of IPD, even those treated at an early age41, our current findings in the ETG show a promising prognosis. Nevertheless, further longitudinal follow-up with a larger cohort is needed in order to better characterize this early-treated CRIM-negative IPD phenotype. We suggest that an ideal approach is early treatment with ERT+ITI, combined with an increased ERT dose. Furthermore, every effort should be made to shorten the delay between diagnosis and treatment initiation, even in an NBS setting, to ensure that these particularly vulnerable infants are offered the best opportunity for an optimal clinical course.
Supplementary Material
ACKNOWLEDGEMENTS
This research was supported in part by a grant from Sanofi Genzyme and in part by Lysosomal Disease Network (LDN). LDN (2U54NS065768–06) is a part of the NCATS Rare Diseases Clinical Research Network (RDCRN). RDCRN is an initiative of the Office of Rare Diseases Research (ORDR), NCATS, funded through a collaboration between the NCATS, the NINDS, and the NIDDK. We thank Dr. Christina Grant, Dr. Lori-Anne Schillaci, Ms. Lorien King, Ms. Kathleen Crosby, Ms. Bethany Bland, Ms. Alissa Jorgenson, Ms. Alicia Turner, Ms. Kristin Isdell, Ms. Allison Walsh, Ms. Leanne Hagen, Ms. Lisa Berry, and all the other providers and clinical staff who helped in the acquisition of clinical data.
Footnotes
ETHICS DECLARATION
Nineteen patients were enrolled in a study approved by the Duke University Health System Institutional Review Board (IRB) (Pro00001562; LDN6709 Site 206; https://clinicaltrials.gov NCT01665326). One patient (L3) was enrolled after approval from the IRB or ethics committee approval at Soroka University Medical Center. Patients were included in the study after provision of written informed consent by their parent(s) or legal guardian(s). All patient data were de-identified.
CONFLICT OF INTEREST
Cindy Li, Katherine Dempsey, Vikas Bhambhani, and William J. Craigen have no conflicts of interest to declare.
Ankit K. Desai has received research support from Sanofi Genzyme and Lysosomal Disease Network (LDN).
Punita Gupta has received consulting fees and honoraria from Sanofi Genzyme, Amicus Therapeutics and Takeda Shire.
Robert J. Hopkin consults with Amicus Therapeutics, AVROBIO, Chiesi, Protalix BioTherapeutics, Sangamo, Sanofi-Genzyme and Takeda-Shire, and has been an investigator in clinical trials sponsored by Amicus Therapeutics, Protalix BioTherapeutics, Sanofi-Genzyme, and Takeda-Shire. He is on the speakers bureau for Alexion, Amicus Therapeutics, Sanofi-Genzyme. These activities have been monitored and found to be in compliance with the conflict of interest policies at Cincinnati Children’s Hospital Medical Center.
Pranoot Tanpaiboon is employed by Quest Diagnostics.
Can Ficicioglu has served as an advisor or consultant for Biomarin Pharmaceutical, Sanofi Genzyme, Swedish Orphan Biovitrum, Recordati, Orphan Technologies, Takeda Shire, Cycle Pharmaceuticals, Horizon Therapeutics, Alexion Pharmaceuticals, and Synlogic Therapeutics. Can Ficicioglu has received research grants for clinical research from Vtesse, Takeda Shire, Sangamo Therapeutics, Orphan Technologies, and Sanofi Genzyme.
Priya S. Kishnani has received research/grant support from Sanofi Genzyme, Valerion Therapeutics, and Amicus Therapeutics. Priya S. Kishnani has received consulting fees and honoraria from Sanofi Genzyme, Amicus Therapeutics, Vertex Pharmaceuticals and Asklepios Biopharmaceutical, Inc. (AskBio). PSK is a member of the Pompe and Gaucher Disease Registry Advisory Board for Sanofi Genzyme, Amicus Therapeutics, and Baebies. Priya S. Kishnani has equity in Asklepios Biopharmaceutical, Inc. (AskBio), which is developing gene therapy for Pompe disease.
DATA AVAILABILITY
All data is available within the manuscript and supplemental materials.
REFERENCES
- 1.Hirschhorn R, Reuser A. Glycogen storage disease type II; acid alpha-glucosidase (acid maltase) deficiency. The Metabolic and Molecular Bases of Inherited Disease 8th edition. Edited by: Scriver CR, Beaudet AL, Sly WS, Valle D. 2001. In: McGraw-Hill, New York. [Google Scholar]
- 2.van den Hout HM, Hop W, van Diggelen OP, et al. The natural course of infantile Pompe’s disease: 20 original cases compared with 133 cases from the literature. Pediatrics. 2003;112(2):332–340. [DOI] [PubMed] [Google Scholar]
- 3.Kishnani PS, Hwu W-L, Mandel H, Nicolino M, Yong F, Corzo D. A retrospective, multinational, multicenter study on the natural history of infantile-onset Pompe disease. The Journal of Pediatrics. 2006;148(5):671–676.e672. [DOI] [PubMed] [Google Scholar]
- 4.Kishnani PS, Nicolino M, Voit T, et al. Chinese hamster ovary cell-derived recombinant human acid alpha-glucosidase in infantile-onset Pompe disease. The Journal of pediatrics. 2006;149(1):89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amalfitano A, Bengur AR, Morse RP, et al. Recombinant human acid alpha-glucosidase enzyme therapy for infantile glycogen storage disease type II: results of a phase I/II clinical trial. Genet Med. 2001;3(2):132–138. [DOI] [PubMed] [Google Scholar]
- 6.Nicolino M, Byrne B, Wraith JE, et al. Clinical outcomes after long-term treatment with alglucosidase alfa in infants and children with advanced Pompe disease. Genet Med. 2009;11(3):210–219. [DOI] [PubMed] [Google Scholar]
- 7.Kishnani PS, Goldenberg PC, DeArmey SL, et al. Cross-reactive immunologic material status affects treatment outcomes in Pompe disease infants. Mol Genet Metab. 2010;99(1):26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parini R, De Lorenzo P, Dardis A, et al. Long term clinical history of an Italian cohort of infantile onset Pompe disease treated with enzyme replacement therapy. Orphanet journal of rare diseases. 2018;13(1):32-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prater SN, Banugaria SG, DeArmey SM, et al. The emerging phenotype of long-term survivors with infantile Pompe disease. Genetics in medicine : official journal of the American College of Medical Genetics. 2012;14(9):800–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banugaria SG, Prater SN, Ng YK, et al. The impact of antibodies on clinical outcomes in diseases treated with therapeutic protein: lessons learned from infantile Pompe disease. Genet Med. 2011;13(8):729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Gelder CM, Hoogeveen-Westerveld M, Kroos MA, Plug I, van der Ploeg AT, Reuser AJJ. Enzyme therapy and immune response in relation to CRIM status: the Dutch experience in classic infantile Pompe disease. Journal of inherited metabolic disease. 2015;38(2):305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berrier KL, Kazi ZB, Prater SN, et al. CRIM-negative infantile Pompe disease: characterization of immune responses in patients treated with ERT monotherapy. Genet Med. 2015;17(11):912–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kishnani PS, Corzo D, Leslie ND, et al. Early treatment with alglucosidase alpha prolongs long-term survival of infants with Pompe disease. Pediatr Res. 2009;66(3):329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chien Y-H, Lee N-C, Chen C-A, et al. Long-Term Prognosis of Patients with Infantile-Onset Pompe Disease Diagnosed by Newborn Screening and Treated since Birth. The Journal of Pediatrics. 2015;166(4):985–991.e982. [DOI] [PubMed] [Google Scholar]
- 15.Yang CF, Yang CC, Liao HC, et al. Very Early Treatment for Infantile-Onset Pompe Disease Contributes to Better Outcomes. J Pediatr. 2016;169:174–180 e171. [DOI] [PubMed] [Google Scholar]
- 16.Khan AA, Case LE, Herbert M, et al. Higher dosing of alglucosidase alfa improves outcomes in children with Pompe disease: a clinical study and review of the literature. Genetics in Medicine. 2020. [DOI] [PMC free article] [PubMed]
- 17.Landis JL, Hyland H, Kindel SJ, Punnoose A, Geddes GC. Pompe disease treatment with twice a week high dose alglucoside alfa in a patient with severe dilated cardiomyopathy. Mol Genet Metab Rep. 2018;16:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Case LE, Bjartmar C, Morgan C, et al. Safety and efficacy of alternative alglucosidase alfa regimens in Pompe disease. Neuromuscular Disorders. 2015;25(4):321–332. [DOI] [PubMed] [Google Scholar]
- 19.Broomfield A, Fletcher J, Davison J, et al. Response of 33 UK patients with infantile-onset Pompe disease to enzyme replacement therapy. J Inherit Metab Dis. 2016;39(2):261–271. [DOI] [PubMed] [Google Scholar]
- 20.Desai AK, Kazi ZB, Kishnani PS. Cross-reactive immunologic material positive infantile Pompe disease: Characterization of immune responses in patient treated with enzyme replacement therapy. Molecular Genetics and Metabolism;117(2):S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Desai AK, Li C, Rosenberg AS, Kishnani PS. Immunological challenges and approaches to immunomodulation in Pompe disease: a literature review. Annals of Translational Medicine. 2019;7(13):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Banugaria SG, Prater SN, Patel TT, et al. Algorithm for the early diagnosis and treatment of patients with cross reactive immunologic material-negative classic infantile pompe disease: a step towards improving the efficacy of ERT. PLoS One. 2013;8(6):e67052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kazi ZB, Desai AK, Berrier KL, et al. Sustained immune tolerance induction in enzyme replacement therapy-treated CRIM-negative patients with infantile Pompe disease. JCI Insight. 2017;2(16). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mendelsohn NJ, Messinger YH, Rosenberg AS, Kishnani PS. Elimination of antibodies to recombinant enzyme in Pompe’s disease. N Engl J Med. 2009;360(2):194–195. [DOI] [PubMed] [Google Scholar]
- 25.Messinger YH, Mendelsohn NJ, Rhead W, et al. Successful immune tolerance induction to enzyme replacement therapy in CRIM-negative infantile Pompe disease. Genet Med. 2012;14(1):135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chien YH, Lee NC, Chen CA, et al. Long-term prognosis of patients with infantile-onset Pompe disease diagnosed by newborn screening and treated since birth. J Pediatr. 2015;166(4):985–991 e981–982. [DOI] [PubMed] [Google Scholar]
- 27.van Gelder CM, Poelman E, Plug I, et al. Effects of a higher dose of alglucosidase alfa on ventilator-free survival and motor outcome in classic infantile Pompe disease: an open-label single-center study. J Inherit Metab Dis. 2016;39(3):383–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bali DS, Goldstein JL, Rehder C, et al. Clinical Laboratory Experience of Blood CRIM Testing in Infantile Pompe Disease. Molecular genetics and metabolism reports. 2015;5:76–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Young SP, Stevens RD, An Y, Chen Y-T, Millington DS. Analysis of a glucose tetrasaccharide elevated in Pompe disease by stable isotope dilution–electrospray ionization tandem mass spectrometry. Analytical Biochemistry. 2003;316(2):175–180. [DOI] [PubMed] [Google Scholar]
- 30.Chien Y-H, Goldstein JL, Hwu W-L, et al. Baseline Urinary Glucose Tetrasaccharide Concentrations in Patients with Infantile- and Late-Onset Pompe Disease Identified by Newborn Screening. JIMD Rep. 2015;19:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chien YH, Tsai WH, Chang CL, et al. Earlier and higher dosing of alglucosidase alfa improve outcomes in patients with infantile-onset Pompe disease: Evidence from real-world experiences. Mol Genet Metab Rep. 2020;23:100591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kruskal WH, Wallis WA. Use of Ranks in One-Criterion Variance Analysis. Journal of the American Statistical Association. 1952;47(260):583–621. [Google Scholar]
- 33.JMP Pro® [computer program]. Version 151989–2019.
- 34.Adams EM, Becker JA, Griffith L, Segal A, Plotz PH, Raben N. Glycogenosis type II: a juvenile-specific mutation with an unusual splicing pattern and a shared mutation in African Americans. Human mutation. 1997;10(2):128–134. [DOI] [PubMed] [Google Scholar]
- 35.Vogel M, Staller W, Bühlmeyer K. Left ventricular myocardial mass determined by cross-sectional echocardiography in normal newborns, infants, and children. Pediatric Cardiology. 1991;12(3):143–149. [DOI] [PubMed] [Google Scholar]
- 36.Young SP, Piraud M, Goldstein JL, et al. Assessing disease severity in Pompe disease: the roles of a urinary glucose tetrasaccharide biomarker and imaging techniques. Am J Med Genet C Semin Med Genet. 2012;160C(1):50–58. [DOI] [PubMed] [Google Scholar]
- 37.Thurberg BL, Lynch Maloney C, Vaccaro C, et al. Characterization of pre- and post-treatment pathology after enzyme replacement therapy for pompe disease. Laboratory Investigation. 2006;86(12):1208–1220. [DOI] [PubMed] [Google Scholar]
- 38.Swift G, Cleary M, Grunewald S, Lozano S, Ryan M, Davison J. Swallow Prognosis and Follow-Up Protocol in Infantile Onset Pompe Disease. JIMD reports. 2017;33:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fecarotta S, Ascione S, Montefusco G, et al. Improvement of dysphagia in a child affected by Pompe disease treated with enzyme replacement therapy. Italian Journal of Pediatrics. 2013;39(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Desai AK, Baloh CH, Sleasman JW, Rosenberg AS, Kishnani PS. Benefits of Prophylactic Short-Course Immune Tolerance Induction in Patients With Infantile Pompe Disease: Demonstration of Long-Term Safety and Efficacy in an Expanded Cohort. Frontiers in Immunology. 2020;11:1727 (10.3389/fimmu.2020.01727). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peng SS-F, Hwu W-L, Lee N-C, Tsai F-J, Tsai W-H, Chien Y-H. Slow, progressive myopathy in neonatally treated patients with infantile-onset Pompe disease: a muscle magnetic resonance imaging study. Orphanet Journal of Rare Diseases. 2016;11(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data is available within the manuscript and supplemental materials.


