Abstract
As students do not qualify as essential health care workers, medical education faced severe disruptions during the COVID-19 pandemic including initial suspension of all in-person lectures and on-site rotations. Our Pathology Department was among the first at Northwestern to offer a completely virtual rotation with the goals of: (1) providing a comprehensive introduction to the practice of anatomic and clinical pathology, (2) emphasizing uninterrupted and continued excellence in education, and (3) minimizing exposure risk during the pandemic. The innovative 2-week curriculum incorporated diverse teaching modalities including live and recorded lectures; live and recorded video demonstrations; interactive small group discussions; interactive virtual sign-outs; and written and multimedia assignments, quizzes, and projects. The virtual elective ran from March to July 2020 with 52 total participating medical students. On post-rotation evaluations, students rated the pathology virtual elective 4.7/5.0 compared to other virtual rotations and 4.0/5.0 compared to all rotations (including in-person and virtual). Furthermore, continual improvements were made to the established framework based on rotation feedback such that curriculum content was more abundant and more favorably rated by the last cohort when compared to the first. Finally, although students identified interest in over 10 different medical specialties, all participants expressed increased interest in choosing pathology as a specialty and better understanding of pathology’s role in patient care. We hope our detailed description of creating and evaluating a completely virtual elective rotation serves as a model for other departments to improve pathology education and visibility.
Keywords: COVID-19, curriculum, education, pathology, student, virtual, remote, rotation
Introduction
The COVID-19 pandemic has posed the greatest challenge to the public health infrastructure in the United States in over a century. Health policy strategies aimed at managing the pandemic have focused on minimizing exposure risk. Many academic medical centers have limited the numbers of nonessential health care workers in clinical care spaces, and the long-term impact of such efforts on trainee education remains unknown. Specifically for medical students, the transition to long-distance learning followed abrupt cessation of all in-person lectures and on-site clerkships early in the course of the pandemic.
At the Northwestern University Feinberg School of Medicine (NUFSOM), the administration responded rapidly to the advice of the Association of American Medical Colleges to remove medical students from clinical settings on March 17, 2020.1 The need for online opportunities for training was further emphasized several days later when the state of Illinois issued a Stay at Home order on March 21, 2020. In contrast to resident trainees, most medical students are not deemed essential health care workers,2, 3 and for approximately 3 months, all students at any level of training were removed from direct, on-site patient care. Third- and fourth-year medical students engaged in entirely virtual clinical experiences from March 17, 2020, to June 3, 2020 (Figure 1 ).
Figure 1.
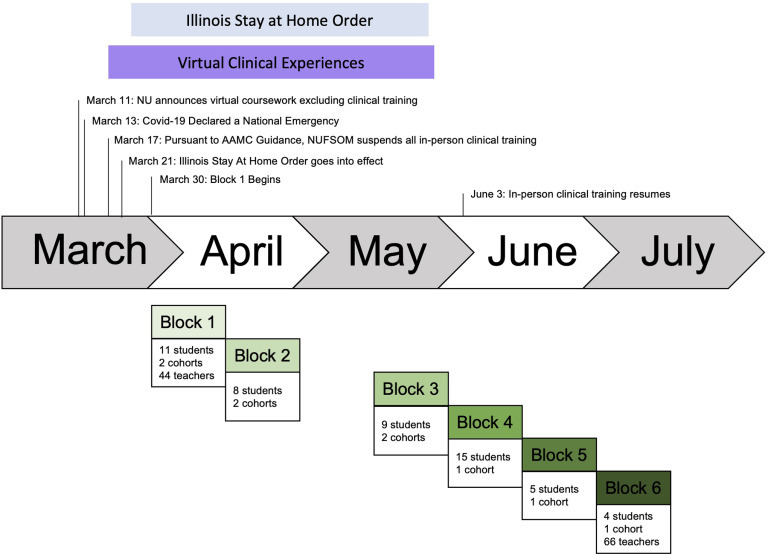
Timeline of Virtual Pathology Elective at Northwestern University Feinberg School of Medicine (NUFSOM). Each block of the virtual elective consisted of 2 weeks of content, 1 each dedicated to AP and CP. A total of 52 medical students participated in the elective from March to July 2020. No students participated in the virtual elective from April 27 to May 8 (between blocks 2 and 3) due to a mandatory break placed on all virtual rotations by NUFSOM. Students progressed as 1 single cohort or divided into 2 cohorts that alternated AP and CP weeks. Total teachers include attending and resident physicians, clinical fellows, medical students, and administrative staff contributing to the elective. During June 2020, students had the option of returning to in-person clinical clerkships or continuing virtual learning opportunities. AAMC indicates American Association of Medical Colleges; AP, anatomic pathology; CP, clinical pathology; NU, Northwestern University.
Creating a permanent online curriculum typically requires a substantial investment in time, planning, coordination, and the use of new technologies and resources, some unique to remote teaching. These commitments were not feasible for NUFSOM during its early emergency response to the pandemic, particularly to accommodate each clinical rotation. In order to provide continued education in compliance with government guidelines, many individual departments mobilized to generate online content for virtual learning.
The Pathology Department at NUFSOM adapted an emergency remote teaching (ERT) model in the design of our online curriculum and was among the first departments within the institution to offer a completely virtual elective rotation. While online education offers many opportunities for improved learning and flexibility,4, 5, 6, 7 the suddenness of the transition necessitated an adaptable curriculum that could produce reliable outcomes under times of duress, thereby highlighting the distinction between ERT and traditional online learning.8 In the much-shortened time frame for content creation, our goal was to create a general framework that allowed for iterative improvements based on participant feedback while still incorporating familiar elements of traditional online and in-person learning curricula. We provided active online instruction with a high instructor–student ratio and varying formats for active engagement between learners and instructors. Active instructional opportunities were supported by volunteers from within our Pathology Department.
Emergency remote teaching differs from traditional online learning in that it is designed as a temporary measure to address an abrupt disruption in traditional learning.4 Therefore, our approach did not intend to upend traditional models of undergraduate medical education as some propose,9, 10 but rather to maintain the pipeline of physicians by providing quality education and continued access to resident and physician mentors during the ongoing COVID-19 pandemic.
Materials and Methods
Curriculum Design and Course Objectives
The curriculum was developed under the leadership of 2 attendings, 2 residents, 2 medical students, and the pathology residency program coordinator. With social distancing restrictions, our vision was to model the schedule on how a medical student might spend their time during an in-person pathology rotation. The primary objective was to provide medical students (MS3 and MS4) a comprehensive introduction to the practice of anatomic pathology (AP) and clinical pathology (CP), emphasizing uninterrupted and continued excellence in education, while keeping in compliance with minimizing exposure risk during a public health crisis. By completing the Virtual Pathology Elective, medical students were expected to fulfill the following specific course objectives: (1) describe the scope of practice and daily work flow of resident and attending pathologists; (2) demonstrate how knowledge gained during previous medical school courses applies to daily pathology practice; (3) bridge the gap between pathology and patient-facing specialties and emphasize mutually beneficial best practices; (4) describe the basic tools, skills, and practice of autopsy, surgical pathology, and cytopathology; and (5) describe the basic tools, skills, and practice within transfusion medicine, hemostasis and coagulation, chemistry, hematopathology, microbiology, and diagnostic molecular biology.
Medical students were expected to dedicate between 15 and 25 hours per week to rotation-specific activities including all self-study, live sessions, and assignments. With the exception of live interactions with pathology attendings and residents, the curriculum was designed to be independently navigable with the majority of content available in an asynchronous format.
Content Creation and Delivery Platform
The Virtual Pathology Elective curriculum was hosted in Box (Box Tools, Version 4.13.0), a secure cloud-based file-sharing and collaboration environment. All faculty, staff, and students could be given free access with their Northwestern institutional account. Individual folders for each rotation day contained the majority of learning materials and assignments. Textbook reading assignments were available online via the Galter Health Sciences Library and Learning Center. A number of freely available, case-based online modules and resources were assigned to supplement both the AP and CP curricula. These modules were provided courtesy of the Pathology Education Instructional Resource from the University of Alabama at Birmingham,11 Cytopathology Unknowns Conference from Johns Hopkins University,12 Emory Pathology e-learning Portal from Emory University,13 and the American College of Radiology.14
Software used for communication and materials creation included Acrobat (Adobe, Version 20.013.20064), PowerPoint (Microsoft Office Professional Plus 2019/2016 Products, Version 16.43), Word (Microsoft Office Professional Plus 2019/2016 Products, Version 16.41), and Outlook (Microsoft Office Professional Plus 2019/2016 Products, Version 16.43). Multimedia demonstrations were recorded on personal cellular devices and computers and edited with Splice Video Editor & Maker (Bending Spoons Apps IVS, Version 4.2.5) and QuickTime (Apple, Inc, Version 10.5). All published curriculum materials were edited for removal of Protected Health Information and vetted for Health Insurance Portability and Accountability Act compliance.
Communication Platform
Zoom (Zoom Video Communications, Inc, Version 5.0.2) with Northwestern institutional access served as the main virtual platform for live lectures, small group discussions, and group presentations. Teams (Microsoft, Version 1.00.300362) was used for live sessions that involved sensitive patient information including sign-outs and live-streams of intraoperative (frozen section) consultations.
Grading and Evaluations
The Virtual Pathology Elective was graded based on a “Credit”/“No-Credit” system, unchanged from how an in-person 2-week Pathology Elective was graded prepandemic. Other virtual electives offered at this time were also graded on a “Credit”/“No-Credit” system. At NUFSOM, traditional-track medical students are allowed two 2-week “Credit”/“No-Credit” elective rotations as part of their total 20 required weeks of elective rotations. NUFSOM placed a limit on the amount of virtual learning which could be used to satisfy core clerkship requirements and allowed students to begin multiple clerkships virtually with the expectation that they would return for in-person learning once available. A limited number of fourth-year students were allowed to complete more required clerkships under the virtual learning format in order to satisfy graduation requirements. In addition to participation in virtual electives such as the Virtual Pathology Elective, third- and fourth-year students were also able to engage in scholarly research requirements or take personal flex time.
For the Virtual Pathology Elective, students were evaluated based on attendance, participation in live sessions, completion of assignments, and completion of a group presentation. A 25-question multiple choice quiz to assess students’ understanding of important concepts in pathology was administered pre-rotation; the same quiz was administered post-rotation
After the elective, students were also required to fill out evaluations for the rotation and for faculty, residents, and other instructors. The rotation evaluation was hosted and responses collected on Microsoft Forms.15 The evaluation asked for students’ opinions on both overall and specific aspects of the curriculum and students’ perceptions about pathology.
Statistical Analyses
The data analyses and visualizations were conducted using Excel (Microsoft Office Professional Plus 2019/2016 Products, Version 16.43) and the R programming language, specifically packages: tidyverse, readxl, janitor, lubridate, ggthemes, and RColorBrewer.16 Calculations included simple summary statistics (mean, median, range) as well as Student t test.
Results
The Virtual Pathology Elective ran for a total of six 2-week blocks from March 30, 2020, until July 03, 2020, with a break during the April 17, 2020, to May 08, 2020, block due to a mandatory break placed on all virtual rotations by NUFSOM. This long-distance learning option was offered to all medical students who had completed phase 1a and 1b of the NUFSOM curriculum. The number of different completely virtual electives offered varied during this time, with 7 to 10 available per block. The Virtual Pathology Elective was among the first-available completely virtual electives along with: Medical Humanities—Epidemics in US History, Medical Humanities—Uncertainty in Medicine, Medical Humanities—Medical Improv & Telemedicine, Medical Students as Educators, Virtual Radiology, and Virtual COVID-19.
A total of 52 medical students completed the entire 2-week rotation. Rotators were mostly third-year (34/52, 65%) and fourth-year (17/52, 33%) students, with 1 rare second-year student (2%) enrolled in block 3. The majority of participants (35/52, 67%) had enrolled in at least one other virtual elective prior to their participation in the Virtual Pathology Elective.
The 2-week curriculum allocated equal time to AP and CP and covered a wide range of topics within autopsy, surgical pathology, cytopathology, transfusion medicine, hemostasis and coagulation, microbiology, chemistry, hematopathology, and diagnostic molecular biology. At the beginning of each block, all rotators started the course together to receive a brief introduction to pathology as a field and career, learn how to navigate Box and the virtual elective materials, and also meet the Virtual Pathology Elective Team. The students in blocks 1 to 3 were further subdivided into 2 groups, with 1 group starting on an AP week and the other on a CP week; the 2 groups then switched for the remaining week in the block. Beginning in block 4, all students were combined into 1 group and completed the entire course together. Near the end of each block, all rotators gathered virtually for final group presentations to share interesting topics and how they will apply what they have learned in their future practice. This final meeting also allowed for in-person rotation feedback from the students and was well attended by pathology residents, faculty, and department leadership (Figure 2 ).
Figure 2.
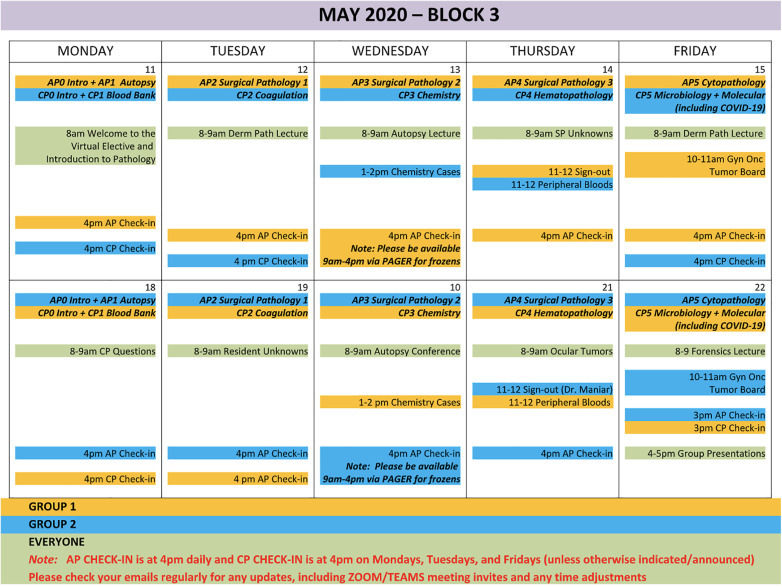
Sample Virtual Pathology Elective rotation calendar (block 3). The 2-week curriculum covered a wide range of topics in both anatomic pathology (autopsy, surgical pathology, cytopathology) and clinical pathology (transfusion medicine, hemostasis and coagulation, microbiology, chemistry, hematopathology, and diagnostic molecular biology). Students in blocks 1 to 3 were further subdivided into 2 groups, while students in blocks 4 to 6 completed the rotation as 1 group.
A typical day started with virtual attendance at the pathology residents’ morning didactics conference, which was already held over Zoom or Microsoft Teams. Rotators would then refer to their schedule, confirm their rotation day (eg, CP3, AP2,…etc) and find the corresponding Box folder. This folder contained all the learning resources a student would need to independently navigate their curriculum for the day including a “Start Here” PowerPoint, with audio voice-over, which described the general learning objectives, an outline of the learning materials (and how to find them), and descriptions of assignments and deliverables. Learning materials within the Box folders were numbered and labeled for easy navigation (Figure 3 ).
Figure 3.

Navigating the Virtual Pathology Elective curriculum materials in Box. After attending morning conference with the pathology residents, medical students would refer to the rotation calendar, confirm their rotation day (eg, AP2, CP3,…etc) and find the corresponding Box folder. Each rotation day folder contained everything a student would need to independently navigate the curriculum. The “Start Here” PowerPoint described the general learning objectives, outlined the learning materials (and how to find them), and described any assignments. Learning materials within the Box folders were numbered and labeled for easy navigation.
The provided self-guided learning materials included recorded PowerPoint lectures, recorded video demonstrations, assigned textbook readings, and online learning modules/cases. Most days included at least 1 interactive virtual session including additional live lectures, live sign-outs, small group discussions, multidisciplinary tumor boards, and live streams of intraoperative (frozen section) consultations. Students reinforced their learning by completing a variety of assignments including multiple choice questions, recorded multimedia (including “grossing” a household item such as a piece of fruit), short answer questions (both with specific correct answers and also discussion style), and group presentations. Students uploaded completed assignments to their individual, designated Box folders, which also helped to track their progress throughout the rotation.
The general framework and delivery for the Virtual Pathology Elective remained consistent from block 1 through block 6. Based on student feedback in post-rotation evaluations, continual changes and additions were made to specific curriculum materials. Although the majority of rotators in block 1 felt that there was the right amount of material by learning modality, every category had a number of rotators who either wanted more or wanted less of a particular course material. In particular, many students wanted more instances of live lectures and live sign-outs. By block 6, all rotators felt that there was the right amount in 10 of 14 types of learning modalities used in the curriculum. In 3 of the 4 categories which did not achieve unanimous approval from students (residents’ morning didactics, live lectures, and small group discussion), increased percentages of rotators thought they were assigned the appropriate amount by block 6. For one category (multimedia assignments), a lower proportion of students felt there was the correct amount by block 6 (Figure 4 ). Detailed descriptions of the block 1 and block 6 curriculums and participants are included for comparison in the Supplementary Appendix.
Figure 4.
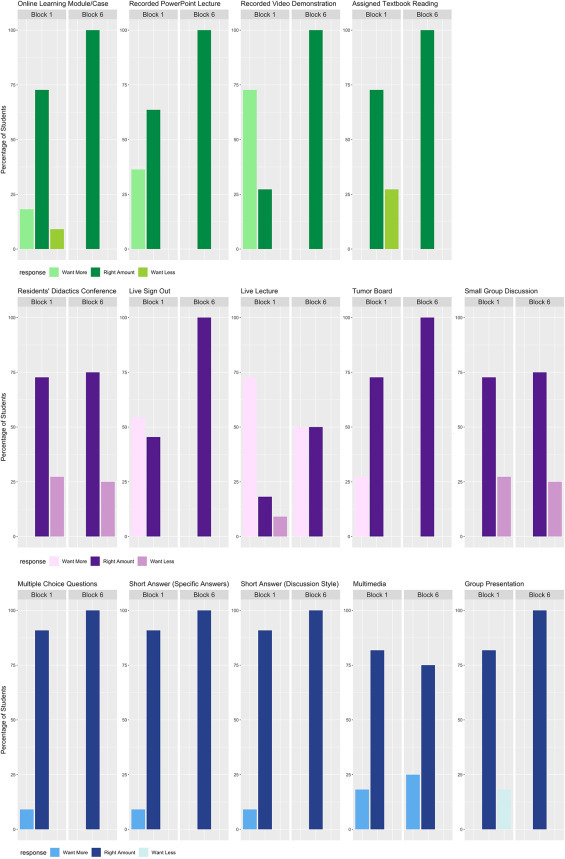
Comparing students’ perceptions of passive (green), live (purple), and assignment (blue) learning modalities. The majority of rotators in block 1 already felt that there was the right amount of each type of learning modality, but each category still had a number of rotators who either wanted more or wanted less of a particular delivery method. Changes and additions were continually made to the Virtual Pathology Elective curriculum based on students’ feedback. By block 6, all rotators felt that there were the right amounts of 10 of 14 types of learning modalities. Even in categories which did not achieve unanimous approval from students (residents’ morning didactics, live lectures, and small group discussion), satisfaction scores showed increased proportions of rotators who thought they were assigned the appropriate amount.
To accommodate the necessary additions to the curriculum based on student feedback, the Virtual Pathology Elective recruited increased numbers of Pathology Department members to create learning materials or to lead live lectures and small group discussions (Figure 5 ).
Figure 5.
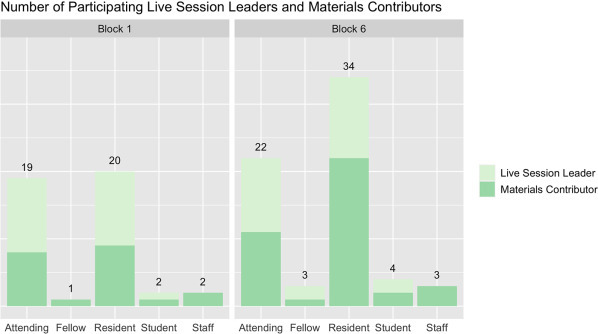
Increased Pathology Department engagement in the Virtual Elective and medical student education. To accommodate the necessary additions to the curriculum based on students’ rotation feedback, increased numbers of pathology attendings, fellows, residents, and staff participated by creating recorded learning materials and leading live lectures and small group discussions. Participants often contributed to both live sessions and recorded materials across multiple days of the curriculum.
All students who completed the 2-week curriculum received “Credit.” Pre- and post-rotation quiz scores did not officially count toward a grade; however, the average post-rotation quiz score was significantly higher than the average pre-rotation quiz score (86.4% vs 69.3%, P value < 2.2e-16; Figure 6 ).
Figure 6.
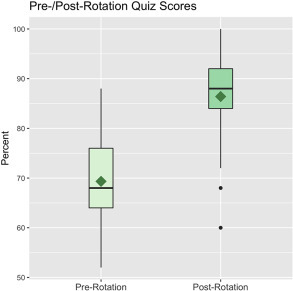
Comparing pre- and post-rotation quiz scores. All Virtual Pathology Elective students took a 25-question multiple choice quiz before and after the rotation to evaluate their knowledge of important pathology concepts. The average post-rotation quiz score was significantly higher than the average pre-rotation quiz score (86.4% vs 69.3%, P value < 2.2e-16).
Many students were undecided about which specialty to pursue (14/52, 27%), and the remaining students were interested in a wide variety of fields encompassing both medicine and surgery. One student listed pathology as their anticipated specialty. After completing the Virtual Pathology Elective, students were significantly more likely to choose pathology as their own specialty (9.6% vs 29.3%, P value < 1.7e-07) and even more likely to recommend pathology to their peers (23.6% vs 74.1%, P value < 2.2e-16; Figure 7 ).
Figure 7.
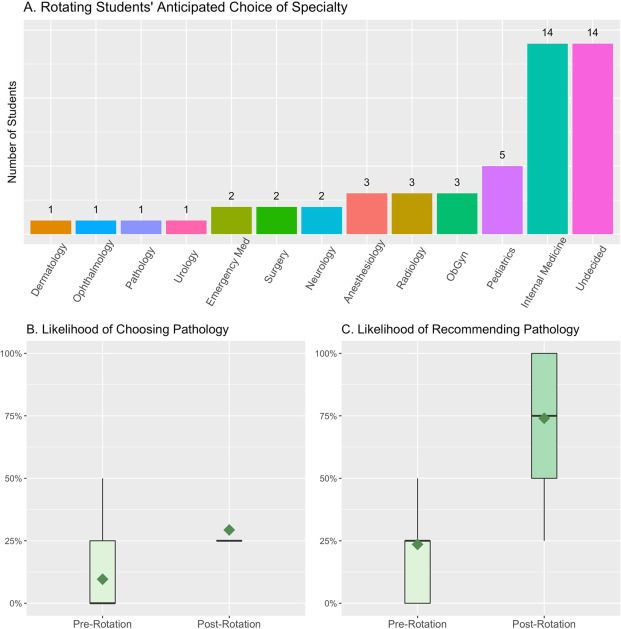
Medical students’ anticipated specialties and likelihood of choosing/recommending pathology. A, Many students were undecided about which specialty to pursue (14/52, 27%), and the remaining students were interested in a wide variety of fields encompassing both medicine and surgery. One student listed pathology as their anticipated specialty. B, After completing the Virtual Pathology Elective, students were significantly more likely to choose pathology as their own specialty (9.6% vs 29.3%, P value < 1.7e-07) and (C) even more likely to recommend pathology to their peers (23.6% vs 74.1%, P value < 2.2e-16).
After completion of the Virtual Pathology Elective, students self-reported a significantly improved understanding of what pathologists do (2.4/5.0 vs 4.5/5.0, P value < 2.2e-17). Rotators also reported an increased likelihood of considering a pathologist in their future practice (2.4/5.0 vs 3.8/5.0, P value < 2.3e-17). Furthermore, students identified a significant increase in their confidence about what specific and useful questions to ask a pathologist (2.0/5.0 vs 4.3/5.0, P value < 2.2e-17; Figure 8 ).
Figure 8.
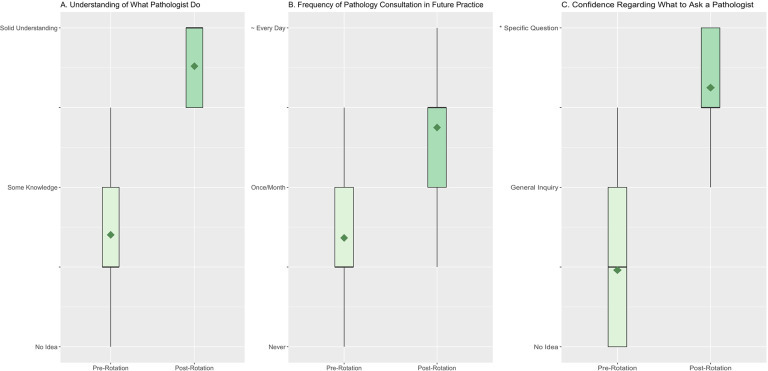
Improved understanding of pathology and how to best consult a pathologist. A, After completion of the Virtual Pathology Elective, students self-reported a significantly improved understanding of what pathologists do (2.4/5.0 vs 4.5/5.0, P value < 2.2e-17). B, Rotators also reported an increased likelihood of consulting a pathologist in their future practice (2.4/5.0 vs 3.8/5.0, P value < 2.3e-17). C, Furthermore, students identified a significant increase in their confidence about what specific and useful questions to ask a pathologist (2.0/5.0 vs 4.3/5.0, P value < 2.2e-17). *Specific question with actionable sequelae.
Overall, students rated the Virtual Pathology Elective 4.7/5.0 when compared to all virtual electives they had participated in (if any) and 4.0/5.0 when compared to all rotations/clerkships (including in-person) that they had ever participated in.
Discussion
The COVID-19 pandemic poses an unprecedented disruption to health care and medical education in our lifetime and has created an urgent need for ERT modalities. Many print and online pathology resources in the form of cases, videos, tutorials, and readings were already freely accessible even prior to this public health crisis.17, 18 However, our Virtual Pathology Elective is unique in that our novel curriculum organized existing content, created new educational materials, and included consistent interaction with faculty and residents to deliver a comprehensive rotation experience for all medical students, regardless of their specific interest in pathology.
The Virtual Pathology Elective was modeled after an in-person rotation, and this long-distance learning opportunity proved to be even more effective than a traditional rotation. One of the greatest benefits was our ability to reach more students than would be possible with a traditional clerkship. In the last 10 years, our Northwestern Department of Pathology hosted an average of 18 medical students per year, while the virtual rotation was able to accommodate more than 50 students in just 3 months. In just 2 weeks, students showed significant improvement in their knowledge of pathology as evidenced by increased postevaluation quiz scores. Furthermore, students began to appreciate pathology’s integral role in many aspects of patient care. With an improved understanding of the breadth of our specialty in diagnostic and laboratory medicine, virtual rotators could identify increased opportunities to consult a pathologist in their future practice. These results suggest that medical students completing the virtual elective will more effectively integrate pathologists in a variety of clinical scenarios and provide more comprehensive patient care.
As students began to appreciate the impact pathologists have on patient care, they also reported an increased likelihood of considering pathology as a career. This revelation is especially timely as novel recruitment techniques are needed to counter the anticipated shortage of trainees entering pathology residency programs. Current trends predict that the number of pathologists retiring will outpace the number of new trainees, resulting in a net deficit of approximately 5700 pathologists in the United States by 2030.19 Yet in the period from 2010 to 2019, applications for pathology residency decreased by 40%,20 despite high reports of job satisfaction among the pathology workforce.21 Because our Virtual Pathology Elective reached greater numbers of medical students and effectively highlighted the key role of pathology in a wide variety of patient scenarios, it is easy to see such a curriculum playing a vital role in student recruitment and long-term career planning.22
One of the greatest challenges during this time was evaluating the effectiveness of the numerous available learning modalities. To navigate this unchartered territory, we relied on the detailed feedback elicited by the post-rotation evaluation. Compared to a typical evaluation, this survey asked rather granular questions about every aspect of the curriculum, and students rated their perception of each learning modality. Students could additionally suggest by free-text the types of material they would like to see. One of the most popular aspects of the virtual rotation, the livestream of intraoperative (frozen section) consultations, was a direct suggestion from one of the earliest rotators. This valuable feedback allowed us to fine-tune our curriculum from block to block to continually deliver the best educational experience for the medical students.
A gratifying, though perhaps not completely surprising, finding was that medical students truly preferred live lectures, live sign-outs, and more direct communication with attendings and residents. These interactive teaching experiences were invaluable opportunities for questions and for gaining a deeper understanding of complex subject matter. Of the passive learning modalities, presentations created and recorded by Pathology Department members were very well received. Residents, fellows, and attendings showed great enthusiasm for creating educational content covering a wide variety of topics including: how to approach a surgical pathology slide, how to approach a cytopathology slide, thyroid fine-needle aspiration, and normal histology and pathology of numerous subspecialties (breast pathology, neuropathology, gastrointestinal pathology, gynecologic pathology, dermatopathology, genitourinary pathology). These home-grown lectures were more specifically geared to the medical students’ needs and allowed rotators to learn at their own pace while giving many pathology trainees and attendings the opportunity to get involved in medical student education. Creation of recorded lectures did require significant initial investment, but completed materials were easily reused and recycled, even for junior resident education. These department-made resources proved a sustainable option, optimizing education while minimizing overall time commitment and scheduling considerations for faculty and residents.
Areas for improvement we identified included the need for a more robust CP curriculum. During this initial 3-month run, there was more engagement by both attendings and residents to create AP-specific material. Possible reasons for this include resident preference and comfort teaching topics within AP in addition to the increased burden of clinical duties for pathologists overseeing the clinical laboratories during the pandemic. Increased engagement on the CP side, with continued enthusiasm on the AP side, would allow for future curated “tracks” for students interested in particular specialties. For example, a medical student who intends to specialize in obstetrics and gynecology could participate in a targeted pathology elective focusing on topics in perinatal autopsy, gynecologic histology and pathology, and PAP smear cytology during their AP week while focusing on laboratory assays for prenatal care, hemolytic disease of the fetus and newborn, fetal hemoglobin analysis, molecular testing for molar pregnancies, and cytogenetic screening during their CP week.
In conclusion, we hope our ERT experience and findings can serve as a framework for other institutions considering a remote learning option. The Virtual Pathology Elective earned high ratings from students, who showed increased knowledge of pathology, better understanding of its role in patient care, and greater interest in pursuing pathology as a career. Although this curriculum was created to address an emergent situation during a public health crisis, many aspects of our framework and approach could be sustained beyond this critical period to provide increasing numbers of medical students with excellent pathology education and a foundation for better patient care.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article was competitively selected by Academic Pathology’s Editors, from among abstracts submitted in response to a Special Call for COVID-19 Papers, to receive an article processing fee waiver sponsored by the Association of Pathology Chairs.
ORCID iD
Daniel Selgrade  https://orcid.org/0000-0001-5599-6659
https://orcid.org/0000-0001-5599-6659
Supplementary Material
Supplemental material for this article is available online.
Acknowledgments
The authors thank all the participating faculty, residents, fellows, and staff members in the Northwestern Department of Pathology who created valuable learning materials and enthusiastically led interactive sessions with our medical students.
Supplementary Material
Supplemental Material, sj-pdf-1-apc-10.1177_23742895211010275 - Virtual Pathology Elective Provides Uninterrupted Medical Education and Impactful Pathology Education During the COVID-19 Pandemic
Supplemental Material, sj-pdf-1-apc-10.1177_23742895211010275 for Virtual Pathology Elective Provides Uninterrupted Medical Education and Impactful Pathology Education During the COVID-19 Pandemic by Lucy Fu, Michael Swete, Daniel Selgrade, Clarence W. Chan, Raven Rodriguez, Kristy Wolniak and Luis Z. Blanco in Academic Pathology
References
- 1.Important guidance for medical students on clinical rotations during the coronavirus (COVID-19) outbreak. Press Release. Association of American Medical Colleges. https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak Published March 17, 2020.
- 2.Nassar AH, Zern NK, McIntyre LK, et al. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemic: the University of Washington experience. JAMA Surg. 2020;155:624–627. doi: 10.1001/jamasurg.2020.1219. [DOI] [PubMed] [Google Scholar]
- 3.Monroig-Bosque PDC, Hsu JW, Lin MS, et al. Pathology trainee redeployment and education during the COVID-19 pandemic: an institutional experience. Acad Pathol. 2020;7 doi: 10.1177/2374289520953548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monday LM, Gaynier A, Berschback M, et al. Outcomes of an online virtual boot camp to prepare fourth-year medical students for a successful transition to internship. Cureus. 2020;12 doi: 10.7759/cureus.8558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chao TN, Frost AS, Brody RM, et al. Creation of an interactive virtual surgical rotation for undergraduate medical education during the COVID-19 pandemic. J Surg Educ. 2021;78:346–350. doi: 10.1016/j.jsurg.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeong L, Smith Z, Longino A, Merel SE, McDonough K. Virtual peer teaching during the COVID-19 pandemic. Med Sci Educ. 2020:1–2. doi: 10.1007/s40670-020-01065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wendt S, Abdullah Z, Barrett S, et al. A virtual COVID-19 ophthalmology rotation. Surv Ophthalmol. 2021;66:354–361. doi: 10.1016/j.survophthal.2020.10.001. Epub 2020 Oct 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hodges C, Moore S, Lockee B, Trust T. The difference between emergency remote teaching and online learning. https://er.educause.edu/articles/2020/3/the-difference-between-emergency-remote-teaching-and-online-learning Published November 11, 2020.
- 9.Emanuel EJ. The inevitable reimagining of medical education. JAMA. 2020;323:1127–1128. doi: 10.1001/jama.2020.1227. [DOI] [PubMed] [Google Scholar]
- 10.Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323:2131–2132. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 11.Pathology Education Instructional Resource (PEIR) Division of Genomic Diagnostics & Bioinformatics in the Department of Pathology at the University of Alabama Birmingham. https://peir.path.uab.edu/wiki/Main_Page Published February 11, 2020.
- 12.Johns Hopkins University Unknowns Conference. http://apps.pathology.jhu.edu/cyto/ Published August 8, 2018.
- 13.Emory University Emory Pathology e-learning Portal. 2018. http://www.path.emory.edu/EPeP/
- 14.American College of Radiology Pathology Teaches. 2021. https://cortex.acr.org/Presenters/CaseScript/CaseView?Info=2LDWjJJ+HH6XS/0bVBeL6pasBHvpyjRvtI79N0Ecf7c=
- 15.Northwestern Department of Pathology Northwestern Virtual Pathology Elective Evaluation (END) https://forms.office.com/Pages/ResponsePage.aspx?id=YdN2fXeCCEekd2ToNmzRvNRcWxwJtWtFjb3SdCmKhPFURDg0VTZHVkVMM1k3WFlKUFBOVkZXNTRQSC4u Published March 30, 2020.
- 16.R Core Team . Foundation for Statistical Computing; 2020. R: A Language and Environment for Statistical Computing.http://www.R-project.org/ [Google Scholar]
- 17.Mukhopadhyay S, Booth AL, Calkins SM, et al. Leveraging technology for remote learning in the Era of COVID-19 and social distancing. Arch Pathol Lab Med. 2020;144:1027–1036. doi: 10.5858/arpa.2020-0201-ED. [DOI] [PubMed] [Google Scholar]
- 18.Balakrishnan R, Singh K, Harigopal M, Fineberg S. A Novel “Google Classroom”-Based pathology education tool for trainees during the COVID-19 pandemic: impactful learning while social distancing. Arch Pathol Lab Med. 2020;144:1445b–1447. doi: 10.5858/arpa.2020-0476-LE. [DOI] [PubMed] [Google Scholar]
- 19.Robboy SJ, Weintraub S, Horvath AE, et al. Pathologist workforce in the United States: I. Development of a predictive model to examine factors influencing supply. Arch Pathol Lab Med. 2013;137:1723–1732. doi: 10.5858/arpa.2013-0200-OA. [DOI] [PubMed] [Google Scholar]
- 20.Jajosky RP, Banks M, Jajosky AN. Concerns about the pathology job market dominate a popular online pathology forum and likely deterred American medical students from pursuing pathology residency. Heliyon. 2019;5 doi: 10.1016/j.heliyon.2019.e02400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia E, Kundu I, Kelly M, Soles R, Mulder L, Talmon GA. The American Society for Clinical Pathology’s job satisfaction, well-being, and burnout survey of pathologists. Am J Clin Pathol. 2020;153:435–448. doi: 10.1093/ajcp/aqaa010. [DOI] [PubMed] [Google Scholar]
- 22.Gross DJ, Black-Schaffer WS, Hoffman RD, et al. The State of the job market for pathologists: evidence from the college of American pathologists practice leader survey. Arch Pathol Lab Med. 2020;144:420–426. doi: 10.5858/arpa.2019-0356-CP. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-apc-10.1177_23742895211010275 - Virtual Pathology Elective Provides Uninterrupted Medical Education and Impactful Pathology Education During the COVID-19 Pandemic
Supplemental Material, sj-pdf-1-apc-10.1177_23742895211010275 for Virtual Pathology Elective Provides Uninterrupted Medical Education and Impactful Pathology Education During the COVID-19 Pandemic by Lucy Fu, Michael Swete, Daniel Selgrade, Clarence W. Chan, Raven Rodriguez, Kristy Wolniak and Luis Z. Blanco in Academic Pathology


