Subgaleal hemorrhage is a rare but potentially lethal condition found in newborns.1 It is caused by rupture of the emissary veins, which are connections between the dural sinuses and the scalp veins. Blood accumulates between the epicranial aponeurosis of the scalp and the periosteum. This potential space extends forward to the orbital margins, backward to the nuchal ridge and laterally to the temporal fascia. In term babies, this subaponeurotic space may hold as much as 260 mL of blood.2 Subgaleal hemorrhage can therefore lead to severe hypovolemia, and up to one-quarter of babies who require neonatal intensive care for this condition die.1 The prevalence at birth of moderate-to-severe subgaleal hemorrhages is approximately 1.5 per 10 000 births. Despite yearly reports from the Obstetrical Care Review Committee for the Office of the Chief Coroner for Ontario, many health care workers have limited knowledge of subgaleal hemorrhage. This article describes a typical case of subgaleal hemorrhage in a newborn who was 1 of 4 patients admitted to the Children's Hospital of Eastern Ontario, in Ottawa, with this condition from Jan. 1, 1996, to Sept. 30, 1999, and reviews the key elements of identification and treatment.
A 3891-g female was born at 41 weeks' gestation to a primigravid mother. Labour was spontaneous and the presentation was occiput posterior. After rotation of the head, vacuum extraction was attempted 3 or 4 times. A tight nuchal cord was cut approximately 50 seconds prior to delivery. There was mild shoulder dystocia. Apgar scores were 3, 4 and 7 at 1, 5 and 10 minutes respectively. The cord blood pH was 7.26, with a base deficit of 7.2 mmol/L. The baby required bag and mask ventilation for a short time. The baby was initially described as flaccid and “shocked” looking. She was sent to the nursery for observation with oxygen as required. When the baby was 1.5 hours of age, the transport team from the regional children's hospital was called because the baby was paler and unresponsive. Fluid boluses were suggested but not given because of lack of intravenous access. On their arrival, the transport team noted severe swelling of the baby's scalp. A hematocrit done when the baby was 3.5 hours of age was 0.34 compared with an umbilical cord blood hematocrit of 0.49. The baby received 50 mL/kg boluses of crystalloid and blood products, as well as glucose, sodium bicarbonate and dopamine. Despite full neonatal intensive care, the baby continued to deteriorate with severe encephalopathy, profound hypotension, renal failure and disseminated intravascular coagulation. She died at approximately 18 hours of age. Postmortem examination confirmed a massive subgaleal hemorrhage, with several diastatic fractures and anoxic-ischemic changes within the brain.
This baby died of hypovolemic shock caused by massive subgaleal hemorrhage with a secondary acute encephalopathy. Could the course of her illness have been modified if her condition had been recognized earlier? Both the US Food and Drug Administration and Health Canada have issued warnings about the use of vacuum extraction.3,4 To quote the Health Canada alert, “All Health Care Professionals responsible for the post-natal care of infants whose delivery involved the use of Vacuum Assisted Delivery Devices …must monitor the infant for signs of subgaleal haemorrhage.”4 The baby described here had the vacuum applied 3 or 4 times, which should have increased staff vigilance for subgaleal hemorrhage. In addition, the baby's pallor and shocked appearance at birth, despite there being no biochemical evidence of fetal asphyxia, should have increased concern. Unfortunately, subgaleal hemorrhage was not diagnosed early, and the baby could not be saved despite massive volume resuscitation.
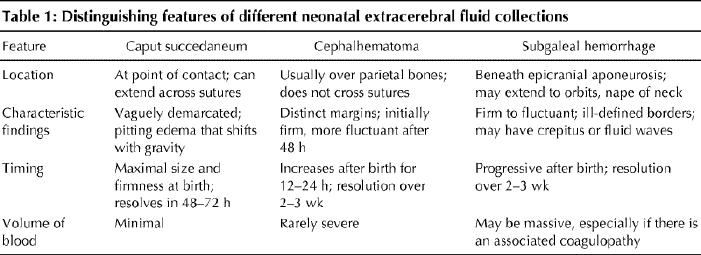
Subgaleal hemorrhage is most often associated with vacuum extraction and forceps delivery, but it may also occur spontaneously.5 Inappropriate placement of the vacuum extractor is a significant contributor to failed vacuum extraction and subgaleal hemorrhage.1,6 Optimizing the outcome for babies with subgaleal hemorrhage requires early diagnosis, careful monitoring and prompt treatment. Diagnosis is made by history-taking and physical examination. Monitoring includes a minimum of 8 hours' observation for all babies following difficult vacuum extractions or forceps deliveries, regardless of Apgar score or need for resuscitation.7 This observation should include at least hourly recording of vital signs. Examination of the head, including the circumference of the head and assessment of the location and characteristics of any swelling (Table 1), should be repeated hourly if concerns are present. Using these features to aid early recognition is an important key to intact survival. The presence of fluctuance early on, whether or not the swelling is progressive, is an important distinguishing feature of subgaleal hemorrhage. Because blood spreads through a large tissue plane in subgaleal hemorrhage, blood loss may be massive before hypovolemia becomes evident. When subgaleal hemorrhage is suspected, hemoglobin measurement should be performed as soon as possible and should be monitored every 4–8 hours, as should coagulation studies.8 Although it is not necessary to make the clinical diagnosis, optimal imaging for subgaleal hemorrhage is by CT or MRI.9,10 Radiographs of the skull can be done to identify accompanying fractures.8
Table 1
Other than appropriate resuscitation, intensive care management and the massive quantities of blood products that are often urgently required to maintain circulation in babies with subgaleal hemorrhage, there is no specific treatment. Pressure wrapping of the head has been advocated by some,6 but the large subaponeurotic space is difficult to wrap except with a cap that is attached under the chin; wrapping might be disadvantageous if cerebral edema were present. After stabilization, consideration should be given to investigating the possibility of a congenital coagulopathy. Bilirubin levels must also be carefully monitored.8
Early recognition, careful monitoring, prompt and aggressive administration of blood products to avoid hypovolemic shock, and treatment of any associated coagulopathy are the keys to improving outcome. Whenever assisted delivery devices have been used, the individuals who will be caring for the baby must be promptly notified so that the baby will be regularly examined and monitored. Increased awareness of subgaleal hemorrhage should lead to earlier identification, referral and treatment, with resultant improved outcomes.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. Deborah Davis, Division of Neonatology, Rm. 8231, Ottawa Hospital, General Campus, 501 Smyth Rd., Ottawa ON K1H 8L6; fax 613 737-8889; ddavis@ottawahospital.on.ca
References
- 1.Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health 1996;32:228-32. [DOI] [PubMed]
- 2.Eliachar E, Bret AJ, Bardiaux M, Tassy R, Pheulpin J, Schneider M. Hématome souscutané cranien du nouveau-né. Arch Fr Pediatr 1963;20:1105-11. [PubMed]
- 3.United States Food and Drug Administration. FDA public health advisory: need for CAUTION when using vacuum assisted delivery devices. Rockville (MD): FDA; 1998 May 21. Available: www.fda.gov/cdrh/fetal598.html (accessed 2001 April 10).
- 4.Health Protection Branch. The use of vacuum assisted delivery devices and fetal subgaleal haemorrhage. Medical device alert 110. Ottawa: Health Canada; 1999 February 23. Available: www.hc-sc.gc.ca/english/search.htm (accessed 2001 April 10). (Note: After reaching this page, enter the following phrases, “Medical Device Alert 110 AND vacuum assisted,” to access relevant information.)
- 5.Plauché WC. Subgaleal hematoma. A complication of instrumental delivery. JAMA 1980;244:1597-8. [PubMed]
- 6.Vacca A. Birth by vacuum extraction: neonatal outcome. J Paediatr Child Health 1996;32:204-6. [DOI] [PubMed]
- 7.Florentino-Pineda I, Ezhuthachan SG, Sineni LG, Kumar SP. Subgaleal hemorrhage in the newborn infant associated with silicone elastomer vacuum extractor. J Perinatol 1994;14:95-100. [PubMed]
- 8.Pape KE, Wigglesworth JS. Birth trauma. In haemorrhage, ischaemia and the perinatal brain. Clin Develop Med 1979;69/70:62-5.
- 9.King SJ, Boothroyd AE. Pictorial review. Cranial trauma following birth in term infants. Br J Radiol 1998;71:233-8. [DOI] [PubMed]
- 10.Ilagan NB, Weyhing BT, Liang KC, Womack SJ . Radiological case of the month. Neonatal subgaleal hemorrhage. Arch Pediatr Adolesc Med 1994;148:65-6. [DOI] [PubMed]


