Abstract
Background
Chronic cough has many diverse causes, including common and uncommon causes. There are few comprehensive reports on rare causes of chronic cough. The purpose of this study is to determine the etiological distribution, clinical features, and diagnostic value of special examinations in patients with rare causes of chronic cough.
Methods
A retrospective analysis of patients with chronic cough who underwent medical history taking, full examination, and etiological treatment over a 13-year period was conducted. Causes of chronic cough with a prevalence of less than 3% were defined as rare causes.
Results
A total of 1,554 patients were enrolled, and 39 causes of chronic cough were identified. Among them, 1,055 cases were due to common causes, whereas 235 cases were due to rare causes; the causes involved 7 bodily systems. The top five rare causes were protracted bacterial bronchitis, somatic cough syndrome, diffuse panbronchiolitis, obstructive sleep apnea syndrome (OSAS), and interstitial lung disease, accounting for 67.2% of all rare causes. Among 235 patients with rare causes, causes in 90 (38.3%) patients were detected by chest high-resolution computed tomography (HRCT), in 44 (18.7%) patients by bronchoscopy/nasopharyngoscopy, and in 21 (8.9%) patients by pulmonary spirometry and diffusing capacity testing.
Conclusions
Among the 31 rare causes of chronic cough in this cohort, the top five were protracted bacterial bronchitis, somatic cough syndrome, diffuse panbronchiolitis, OSAS, and interstitial lung disease. Special examinations, such as chest HRCT and bronchoscopy, should be considered after excluding common causes of chronic cough.
Keywords: Chronic cough, rare cause, spectrum, special examination
Introduction
Chronic cough is a common complaint of patients in respiratory clinics, and the global prevalence is approximately 9.6% (1). There are many different conditions related to chronic cough. The most common causes of chronic cough include cough variant asthma (CVA), eosinophilic bronchitis (EB), upper-airway cough syndrome (UACS), and gastroesophageal reflux cough (GERC), accounting for 51% to 92% of cases of chronic cough (2-7). A few rare conditions, such as obstructive sleep apnea syndrome (OSAS), idiopathic pulmonary fibrosis, and relapsing polychondritis, have also been reported (8-10). Although rare causes account for a low proportion of chronic cough cases, a wide variety of conditions involving systems other than the respiratory system can be involved. Patients with uncommon causes often receive a misdiagnosis and inappropriate treatment for a long time, leading to great impairment in quality of life and a substantial economic burden. There are few systematic reports on the distribution of rare causes of chronic cough. In addition, the diagnosis of rare causes depends on special examinations, such as high-resolution computed tomography (HRCT), nasopharyngoscopy, or bronchoscopy. However, the usefulness of special examinations in diagnosing rare causes of chronic cough has rarely been reported in previous studies (11-13). Hence, we summarize the etiology, clinical features of and diagnostic methods applied to patients with chronic cough due to rare causes who visited our hospital from 2006 to 2018, aiming to highlight rare diagnoses in chronic cough patients.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-2671).
Method
Subjects and diagnostic protocol
This was a retrospective study. Data were extracted from the medical records of consecutive chronic cough patients who underwent full examinations and treatment who received outpatient care at the First Affiliated Hospital of Guangzhou Medical University from 2006 to 2018. A standard form was used to record demographics, clinical features, laboratory results, primary diagnosis, response to therapy, follow-up, and final diagnosis for chronic cough patients. The inclusion criteria for patients with chronic cough were as follows: (I) chronic cough lasting more than 8 weeks as the sole or predominant symptom; (II) no abnormalities on plain chest film; (III) no acute upper-airway infection in the past 4 weeks; (IV) age older than 16 years old; (V) cause of cough determined by the diagnostic protocol and management of chronic cough as referred to in our previous report (14).
The diagnostic workflow was established to identify the causes of chronic cough in 2003 (14) and later slightly modified according to the cough guidelines (15,16). Briefly, detailed medical history, physical examination, chest radiograph, spirometry, assessment of bronchial hyperresponsiveness, and induced sputum test were conducted in all the patients at entry. 24-h esophageal pH-multichannel impedance monitoring were selected in some patients who was suspected for GERC or failed to initial treatment. Diagnosis of CVA was determined if the patient presented bronchial hyperresponsiveness and responded to anti-asthmatic treatment. EB was diagnosed with normal pulmonary function, a lack of airway hyperresponsiveness, sputum eosinophil count ≥2.5% and response to corticosteroids. GERC was confirmed if 24 h esophageal pH value monitoring showed a DeMeester score of ≥12.7 and symptom association probability of ≥80%, and cough resolved after anti-reflux treatment. UACS was diagnosed based on history, symptoms and signs of rhinitis/sinusitis, and cough improved after specific therapy directed to UACS. To explore uncommon causes, Multidisciplinary consultation and special investigations were conducted, including bronchoscopy, chest HRCT, sinus CT, nasopharyngoscopy, polysomnography, and pulmonary diffusing capacity testing etc. If the above investigations failed to indicate the causes of cough, or if the cough persisted after treatment directed to all potential causes, unexplained cough (UC) was considered. A description of the diagnosis of chronic cough is provided in Table S1.
Causes of chronic cough with rates of less than 3% were defined as rare causes in this study. This retrospective study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (No. 201778) and individual consent for this retrospective analysis was waived.
Statistical analysis
Data are expressed as means ± standard deviations (SDs), medians (interquartile ranges, IQRs) or numbers (percentages). Statistical comparisons between groups were performed with one-way analysis of variance (ANOVA) for normally distributed data, Kruskal-Wallis tests for skewed data, and chi-square tests for proportions, with appropriate post hoc tests for multiple comparisons (adjusted with the Bonferroni method). Missing data were not imputed. A P value <0.05 (two-sided) was considered significant. Statistical analysis was performed using SPSS 25.0.
Results
Spectrum of the causes of chronic cough
A total of 1,554 chronic cough patients were enrolled from 2006 to 2018; 807 (51.9%) patients were female. The average age of the patients was 43.3±14.1 years, and the cough duration was 24 (10.0–84.0) months. The spectrum and frequency of chronic cough are shown in Figure 1. 1,055 (58.8%) cases were due to common causes, 330 (18.4%) cases were due to other common causes, 235 (13.1%) cases were due to rare causes,and the remaining 173 cases (9.6%) were due to UC. The common causes included EB (18.3%), CVA (16.3%), GERC (13.2%), and UACS (11.1%). Other common causes consisted of chronic bronchitis (6.1%), bronchiectasis (4.5%), atopic cough (4.4%) and postinfectious cough (3.5%).
Figure 1.
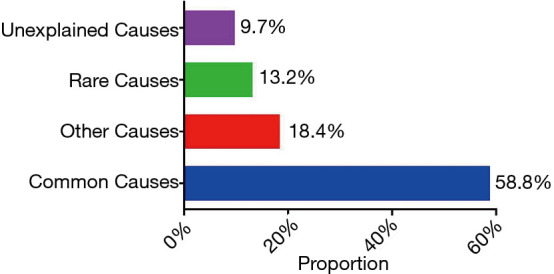
The spectrum and frequency of chronic cough.
The rare causes of chronic cough are shown in Table 1. According to the anatomic location, we classified the rare causes into four groups: upper-airway diseases (28 cases, 1.6%), lower-airway diseases (102 cases, 5.7%), lung diseases (27 cases, 1.5%) and other system diseases (78 cases, 4.4%). The other system diseases involved the neuropsychological system, cardiovascular system, endocrine system, hematological system and skeletal musculature system. The top five-rare causes were protracted bacterial bronchitis (44 cases, 2.5%), somatic cough syndrome (previously referred to as psychogenic cough) (37 cases, 2.1%), diffuse panbronchiolitis (31 cases, 1.7%), obstructive sleep apnea syndrome (23 cases, 1.3%), and interstitial lung disease (23 cases, 1.3%), which accounted for 67.2% of all rare causes (Figure 2).
Table 1. The spectrum and frequency of rare causes of chronic cough based on anatomy.
| Anatomy | Causes |
|---|---|
| Upper-airway (28, 1.6%) | OSAS (23, 9.79%), mucous cyst of salivary gland (1, 0.43%), laryngocarcinoma (1, 0.43%), VCD (2, 0.85%), laryngeal amyloidosis (1, 0.43%) |
| lower-airway (102, 5.7%) | PBB (44, 18.72%), DPB (31, 13.19%), FACC (4, 1.70%), bronchial tuberculosis (5, 2.13%), bronchial foreign body (2, 0.85%), broncholithiasis (1, 0.43%), BACC (1, 0.43%), Kartagener syndrome (1, 0.43%), relapsing polychondritis (8, 3.40%), sarcoidosis (1, 0.43%), postoperative cough (4, 1.70%) |
| Lung (27, 1.5%) | ILD (23, 9.79%), atypical pneumoconiosis (2, 0.85%), COP (2, 0.85%) |
| Other systems (78, 4.4%) | Somatic cough syndrome (37, 15.74%), hyperventilation syndrome (15, 6.38%), ACEI-induced cough (8, 3.40%), arrhythmia (5, 2.13%), HIVD (3, 1.28%), goiter (1, 0.43%), occupational cough (2, 0.85%), styloid process syndrome (1, 0.43%), HES (3,1.28%), catamenial cough (1, 0.43%), LCH (1,0.43%), cardiogenic cough (1,0.43%) |
Data are presented as (cases, percentage of total cases of chronic cough). OSAS, obstructive sleep apnea syndrome; VCD, vocal cord disfunction; PBB, protracted bacterial bronchitis; DPB, diffuse panbronchiolitis; FACC, fungus-associated cough; BACC, bronchial adenoid cystic carcinoma; ILD, interstitial lung disease; COP, cryptogenic organizing pneumonia; ACEI, angiotensin-converting enzyme inhibitor; HIVD, herniated cervical intervertebral disc; HES, hypereosinophilic syndrome; LCH, Langerhans cell histiocytosis.
Figure 2.
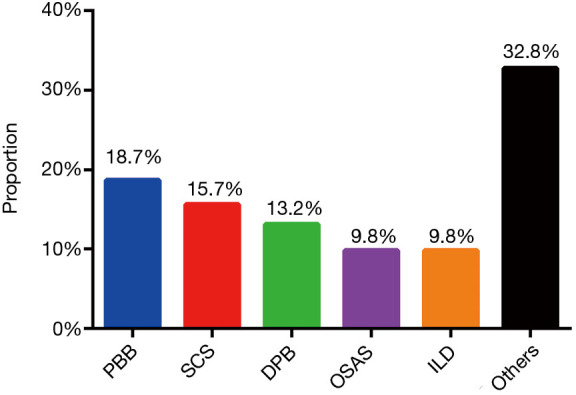
The spectrum and frequency of rare causes. PBB, protracted bacterial bronchitis; SCS, somatic cough syndrome; DPB, diffuse pan bronchiolitis; OSAS, obstructive sleep apnea syndrome; ILD, interstitial lung disease.
The clinical characteristics of rare causes
The patient demographics and characteristics of chronic cough due to rare causes, common causes, other common causes, and unexplained causes are shown in Table S2. Of cases with rare causes, females accounted for 54.9%, the average age was 48.2±15.1 years, and the average cough duration was 24 (10 to 72) months. Regarding timing, cases with rare causes reported daytime cough, nighttime cough, morning cough, and cough before sleep, accounting for 89.3%, 37.9%, 52.7% and 66.2% respectively. Over one-third of cases with rare causes had laryngeal paresthesia, sneezing, nasal congestion, throat clearing, or chest tightness. The most common previous diagnoses of cases with rare causes were pharyngitis (39.0%) and chronic bronchitis (33.5%). Regarding previous treatment in patients with rare causes, antibiotics (80.3%) and antitussives (74.6%) were the most popular therapeutic agents. However, there were no significant difference in clinical characteristics to discriminate between cases with rare causes and cases with other causes of chronic cough.
Usefulness of special examinations in diagnosing rare causes of chronic cough
Some special examinations were performed to diagnose rare causes of chronic cough, including chest HRCT, sinus CT, pulmonary diffusing capacity testing, nasopharyngoscopy and bronchoscopy. The special examinations performed to diagnose rare causes of chronic cough are shown in Table 2. Among 235 cases with rare causes, the causes of 44 (18.7%) cases were detected by bronchoscopy or nasoscopy. Abnormality in pulmonary diffusing capacity was observed in 21 (8.9%) cases with rare causes, indicating the cause of chronic cough. There were 90 (38.3%) cases with rare causes whose causes were indicated by chest HRCT.
Table 2. Values of special examinations in diagnosing rare causes in the cohort.
| Examination | Rare causes (cases) | Total cases, (%) |
|---|---|---|
| Bronchoscopy/nasopharyngoscopy | Relapsing polychondritis (3 cases), Bronchial tuberculosis (5 cases), Bronchial foreign body (2 cases), Mucous cyst of salivary gland (1 case), Broncholithiasis (1 case), TACC (1 case), Pneumoconiosis (1 case), COP (2 cases), Laryngocarcinoma (1 case), VCD (2 cases), Laryngeal amyloidosis (1 case), PBB (6 cases), Sarcoidosis (1 case), DPB (7 cases), ILD (6 cases), HES (2 cases), LCH (1 case), BACC (1 case) | 44/235 (18.7%) |
| HRCT | DPB (31 cases), ILD (23 cases), Relapsing polychondritis (8 cases), COP (2 cases), PPB (9 cases), Bronchial tuberculosis (5 cases), Bronchial foreign body (2 cases), TACC (1 case), Broncholithiasis (1 case), LCH (1 case), Atypical pneumoconiosis (2 cases), Kartagener syndrome (1 case), HES (3 cases), BACC (1 case) | 90/235 (38.3%) |
| Sinus CT | DPB (31 cases), OSAS (1 case) | 32/235 (13.6%) |
| Pulmonary diffusing capacity | ILD (14 cases), DPB (3 cases), TACC (1 case), LCH (1 case), sarcoidosis (1 case), COP (1 case) | 21/235 (8.9%) |
OSAS, obstructive sleep apnea syndrome; VCD, vocal cord disfunction; PBB, protracted bacterial bronchitis; DPB, diffuse pan bronchiolitis; FACC, fungus-associated cough; BACC, bronchial adenoid cystic carcinoma; ILD, interstitial lung disease; COP, cryptogenic organizing pneumonia; ACEI, angiotensin-converting enzyme inhibitor; HES, hypereosinophilic syndrome; LCH, Langerhans cell histiocytosis.
Discussion
To the best of our knowledge, this was the first study to describe the distribution and clinical features of rare causes of chronic cough in a large sample population. A total of 31 rare causes were identified, and in some cases, special examinations were useful for diagnosing rare causes.
CVA, EB, UACS and GERC were the four most common causes of chronic cough, accounting for 58.8%, and the proportion of other common causes was 18.4%, similar to previous studies (3,4). The proportion of patients with rare causes in this study was 13.1%. The top 5 rare causes were protracted bacterial bronchitis, somatic cough syndrome, diffuse panbronchiolitis, OSAS and interstitial lung disease, accounting for 67.2% of cases in patients with rare causes. Regarding the anatomical locations of the rare causes, the proportion of lower-airway diseases was the highest, which may be related to the afferent nerves in the airway causing cough (17). Stimulation in the larynx, trachea, and bronchus may present as obvious cough, whereas cough is usually not the main symptom of small airway and alveolar wall damage.
This study found that protracted bacterial bronchitis accounted for the largest proportion of rare lower-airway causes of chronic cough. Protracted bacterial bronchitis is a common cause of chronic cough in children (18), but is rarely reported in adults (19,20). In 2003, Schaefer reported that cough was relieved after intravenous antibiotic treatment in 15 adult subjects with chronic productive cough and normal HRCT scans (19). Martin et al. reported adult protracted bacterial bronchitis with productive cough (20,21), suggesting that protracted bacterial bronchitis was also a cause of chronic cough in adults. In this study, protracted bacterial bronchitis produced a chronic productive cough or dry cough, which ruled out bronchiectasis, and patients had a good response after more than 2 weeks of antibiotic treatment. In addition, several rare lower-airway diseases were identified, including bronchial tuberculosis, bronchial foreign body, broncholithiasis, and relapsing polychondritis. Therefore, if common causes are excluded, lower- airway diseases should be considered first.
Cough is mediated by a complete neural reflex pathway, and any condition that affects this reflex pathway may cause cough. The afferent nerves associated with the cough reflex are not only distributed in the airway but also in other systems, e.g., the esophagus, sinuses, external auditory canal, pericardium, and others (17). Therefore, rare causes of chronic cough could involve many systems. This study found that the causes of chronic cough were related to the nervous system, endocrine system, cardiovascular system, skeletal system, etc. as well as psychology. It is generally considered that somatic cough syndrome is a common cause of cough in children aged 6 to 16 years (22,23). There are few reports on somatic cough syndrome in adults (24,25). However, the proportion of cases of somatic cough syndrome was second to protracted bacterial bronchitis in this study, indicating that adult somatic cough syndrome should be considered as a rare cause of chronic cough in adults. Many patients with somatic cough syndrome also have anxiety and depression, which might contribute to increased life pressure and work pressure induced by competitive economic transformation in China. There were a variety of other rare causes, such as hyperventilation syndrome, arrhythmia, goiter, styloid process syndrome, and hypereosinophilic syndrome. When diagnosing chronic refractory cough or “UC”, the above causes should be excluded carefully. Diffuse panbronchiolitis is an idiopathic inflammatory disease that was first reported in Japan in the 1960s, with over 50% of cases occurring in East Asia. It typically presents as chronic cough with copious purulent sputum and exertional dyspnea. More than 80% of patients have chronic paranasal sinusitis, their pulmonary function measurements show significant airflow limitation, and bilateral small nodular shadows are visible predominantly in the lower field of the lung on chest radiographs. In this study, we identified 31 diffuse panbronchiolitis patients who presented with chronic cough as the sole or predominate symptom who had normal respiratory function or mild airflow limitation, normal chest X-ray findings, and mild dilation of the bronchiolar passages and a “tree-in-bud” pattern on chest HRCT. Those patients experienced a significant improvement in cough after the use of long-term therapy with macrolide antibiotics.
Diagnosing rare causes of chronic cough is a challenge for clinicians. This study showed that many rare causes of chronic cough were misdiagnosed as chronic bronchitis or chronic pharyngitis, similar to our previous report in unselected patients with chronic cough. Approximately 80% of patients with chronic cough were diagnosed in our previous survey (26). Chronic bronchitis has a relatively high prevalence in epidemiological surveys of community populations (27,28). However, chronic bronchitis is not a common cause of cough addressed in respiratory specialist clinics, with a prevalence of only 1–7.0% according to previous surveys (2,4,7). The prevalence of chronic bronchitis was 6.1% in this study. There are no objective diagnostic criteria for chronic bronchitis, and the term “bronchitis” is often used as a common descriptor for a nonspecific and self-limited cough, which may explain why so many patients are misdiagnosed with chronic bronchitis (29). Chronic cough is often accompanied by pharyngeal paresthesia, including a scratchy throat, foreign body sensation in the pharynx, and paroxysmal irritation (30). Pharyngitis seems to be a good umbrella term for patients with chronic cough. Additionally, rare causes were frequently diagnosed as UC because there were no abnormal findings after routine examinations, and empirical treatment was unsuccessful. Therefore, the diagnosis of chronic bronchitis, chronic pharyngitis or UC should be made very carefully when common causes of chronic cough are ruled out.
History taking and physical examination are the first steps to establish a differential diagnosis; physicians should then select relevant testing, make a tentative diagnosis, and initiate empiric therapy. Although there were no reliable clinical characteristics, including cough timing, cough triggers and concomitant symptoms, to discriminate between patients with rare causes and patients with other causes of chronic cough, some clinical features were helpful in indicating a single etiology, e.g., ‘inspiratory wheezing’ indicates a central airway tumor or bronchial tuberculosis, ‘Velcro crackles’ indicate interstitial lung disease, and pain and numbness in the neck or arm indicate a herniated cervical intervertebral disc; moreover, arrhythmia might be the cause of cough. In the diagnostic procedure for chronic cough, chest HRCT is generally not the first option (31). Chest HRCT is more sensitive than chest X-ray, helping to identify rare causes in the airway and pulmonary parenchyma (31,32). Our study showed that chest HRCT resulted in high positive rates in the diagnosis of rare causes. Chest HRCT played an important role in diagnosing not only early interstitial lung disease but also established interstitial lung disease, bronchial foreign bodies, bronchial tuberculosis, broncholithiasis, relapsing polychondritis and other causes in this study. Bronchoscopy is recommended as a supplementary examination to diagnose rare causes (31), and its diagnostic value for common causes seems limited in unselected patients (12). Bronchoscopy not only confirmed a few airway-related causes but also contributed to observing indications of rare causes, such as cryptogenic organizing pneumonia, hypereosinophilic syndrome, Langerhans cell histiocytosis, etc., when combined with histopathology and chest HRCT. Therefore, we propose that HRCT and bronchoscopy should be considered if no abnormalities are observed in routine examinations and if patients do not respond to empirical treatment. A few specific examinations should be selected based on the patient's condition, e.g., PSG monitoring for patients with obesity or snoring and PET-CT for patients with suspected relapsing polychondritis.
There was limitation to the study. Since the prevalence of rare cause of chronic cough is low and its etiological diagnosis based more on special examinations, it is hard to conduct a prospective, multicenter survey on rare causes of chronic cough. This study might be limited by its retrospective nature as well as being derived from a single hospital. Nevertheless, our data provided the clues of the spectrum and usefulness of special examinations in rare cause of chronic cough.
Conclusions
In conclusion, rare causes of chronic cough accounted for 13.1% of all causes of chronic cough in this cohort. Thirty-one rare causes of chronic cough were identified and involved in many systems, including the respiratory system, nervous system, digestive system, cardiovascular system, endocrine system, hematological system, skeletal musculature system and others. Lower-airway diseases were the most common types of diseases in patients with rare causes. The top 5 rare causes of chronic cough were protracted bacterial bronchitis, somatic cough syndrome, diffuse panbronchiolitis, OSAS, and ILD, accounting for 67.2% of all cases with rare causes. No special clinical features indicating the diagnosis of chronic cough due to rare causes were identified. Special examinations such as HRCT and bronchoscopy play an important role in diagnosing rare causes and should be considered based on the patient’s condition after excluding common causes of chronic cough.
Supplementary
The article’s supplementary files as
Acknowledgments
The authors thank all the patients who participated in this study and all the doctors and nurses who helped to collect the data.
Funding: This study was supported by Key-Area Research and Development Program of Guangdong Province (2019B020227006); Guangzhou Municipal Science and Technology Key Project (2002Z2-E0091); Incubative Project for Innovation Team of GMU (2017-159); and Clinical Research Foundation of GMU (2017-160). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective study was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (No. 201778). Since this study was a review of patients for whom we had clinical responsibility, consent to participate was not sought.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-2671
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-2671
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2671). Dr. KL serves as an editorial board member of Journal of Thoracic Disease. Dr. NZ serves as the Editor-in-Chief of Journal of Thoracic Disease. The authors have no other conflicts of interest to declare.
References
- 1.Song WJ, Chang YS, Faruqi S, et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 2015;45:1479-81. 10.1183/09031936.00218714 [DOI] [PubMed] [Google Scholar]
- 2.Lai K, Chen R, Lin J, et al. A Prospective, Multicenter Survey on Causes of Chronic Cough in China. Chest 2013;143:613-20. 10.1378/chest.12-0441 [DOI] [PubMed] [Google Scholar]
- 3.Lai K, Pan J, Chen R, et al. Epidemiology of cough in relation to China. Cough 2013;9:18. 10.1186/1745-9974-9-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung KF, Pavord ID. Prevalence, pathogenesis, and causes of chronic cough. Lancet 2008;371:1364-74. 10.1016/S0140-6736(08)60595-4 [DOI] [PubMed] [Google Scholar]
- 5.Fujimura M, Abo M, Ogawa H, et al. Importance of atopic cough, cough variant asthma and sinobronchial syndrome as causes of chronic cough in the Hokuriku area of Japan. Respirology 2005;10:201-7. 10.1111/j.1440-1843.2005.00686.x [DOI] [PubMed] [Google Scholar]
- 6.Brightling CE, Ward R, Goh KL, et al. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med 1999;160:406-10. 10.1164/ajrccm.160.2.9810100 [DOI] [PubMed] [Google Scholar]
- 7.Smyrnios NA, Irwin RS, Curley FJ. Chronic cough with a history of excessive sputum production. The spectrum and frequency of causes, key components of the diagnostic evaluation, and outcome of specific therapy. Chest 1995;108:991-7. 10.1378/chest.108.4.991 [DOI] [PubMed] [Google Scholar]
- 8.Smith JA, Woodcock A. Chronic Cough. N Engl J Med 2016;375:1544-51. 10.1056/NEJMcp1414215 [DOI] [PubMed] [Google Scholar]
- 9.Birring SS, Ing AJ, Chan K, et al. Obstructive sleep apnoea: a cause of chronic cough. Cough 2007;3:7. 10.1186/1745-9974-3-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ernst A, Rafeq S, Boiselle P, et al. Relapsing Polychondritis and Airway Involvement. Chest 2009;135:1024-30. 10.1378/chest.08-1180 [DOI] [PubMed] [Google Scholar]
- 11.Sen RP, Walsh TE. Fiberoptic bronchoscopy for refractory cough. Chest 1991;99:33. 10.1378/chest.99.1.33 [DOI] [PubMed] [Google Scholar]
- 12.Barnes TW, Afessa B, Swanson KL, et al. The Clinical Utility of Flexible Bronchoscopy in the Evaluation of Chronic Cough. Chest 2004;126:268-72. 10.1016/S0012-3692(15)32922-6 [DOI] [PubMed] [Google Scholar]
- 13.Volpe J, Storto ML, Lee K, et al. High-resolution CT of the lung: determination of the usefulness of CT scans obtained with the patient prone based on plain radiographic findings. AJR Am J Roentgenol 1997;169:369-74. 10.2214/ajr.169.2.9242737 [DOI] [PubMed] [Google Scholar]
- 14.Lai KF, Chen RC, Liu CL, et al. Etiology and a diagnostic protocol for patients with chronic cough. Zhonghua Jie He He Hu Xi Za Zhi 2006;29:96-9. [PubMed] [Google Scholar]
- 15.Asthma Workgroup of Chinese Society of Respiratory Diseases (CSRD), Chinese Medical Association . Guidelines for Diagnosis and Management of Cough(draft). Chin J Tube Resp Dise 2005;28:738-44. [Google Scholar]
- 16.Irwin RS, Baumann MH, Bolser DC, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest 2006;129:1S-23S. 10.1378/chest.129.1_suppl.1S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Canning BJ, Chang AB, Bolser DC, et al. Anatomy and Neurophysiology of Cough. Chest 2014;146:1633-48. 10.1378/chest.14-1481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kantar A, Chang AB, Shields MD, et al. ERS statement on protracted bacterial bronchitis in children. Eur Respir J 2017;50:1602139. 10.1183/13993003.02139-2016 [DOI] [PubMed] [Google Scholar]
- 19.Schaefer OP, Irwin RS. Unsuspected bacterial suppurative disease of the airways presenting as chronic cough. Am J Med 2003;114:602-6. 10.1016/S0002-9343(03)00079-2 [DOI] [PubMed] [Google Scholar]
- 20.Martin MJ, Harrison TW. Causes of chronic productive cough: An approach to management. Respir Med 2015;109:1105-13. 10.1016/j.rmed.2015.05.020 [DOI] [PubMed] [Google Scholar]
- 21.Martin MJ, Lee H, Clayton C, et al. Idiopathic chronic productive cough and response to open-label macrolide therapy: An observational study. Respirology 2019;24:558-65. 10.1111/resp.13483 [DOI] [PubMed] [Google Scholar]
- 22.Holinger LD, Sanders AD. Chronic Cough in Infants and Children. Laryngoscope 1991;101:596-605. 10.1288/00005537-199106000-00005 [DOI] [PubMed] [Google Scholar]
- 23.Gedik AH, Cakir E, Torun E, et al. Evaluation of 563 children with chronic cough accompanied by a new clinical algorithm. Ital J Pediatr 2015;41:73. 10.1186/s13052-015-0180-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gay M, Blager F, Bartsch K, et al. Psychogenic habit cough: review and case reports. J Clin Psychiatry 1987;48:483-6. [PubMed] [Google Scholar]
- 25.Mastrovich JD, Greenberger PA. Psychogenic cough in adults: a report of two cases and review of the literature. Allergy Asthma Proc 2002;23:27-33. [PubMed] [Google Scholar]
- 26.Lai K, Li B, Wang F, et al. Survey on the diagnosis and management of the patients with chronic cough. Int J Respir 2011;31:645-47. [Google Scholar]
- 27.Cerveri I, Accordini S, Verlato G, et al. Variations in the prevalence across countries of chronic bronchitis and smoking habits in young adults. Eur Respir J 2001;18:85-92. 10.1183/09031936.01.00087101 [DOI] [PubMed] [Google Scholar]
- 28.Kim V, Criner GJ. Chronic Bronchitis and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 2013;187:228-37. 10.1164/rccm.201210-1843CI [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Braman SS. Chronic Cough Due to Chronic Bronchitis. Chest 2006;129:104S-15S. 10.1378/chest.129.1_suppl.104S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen RC, Lai KF, Xu DY, et al. Etiological Diagnosis of Chronic Cough with Pharyngitis-Like Manifestations. Chinese Journal of Respiratory and Critical Care Medicine 2010;9:462-4. [Google Scholar]
- 31.Morice AH, McGarvey L, Pavord I. Recommendations for the management of cough in adults. Thorax 2006;61:i1. 10.1136/thx.2006.065144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Truba O, Rybka A, Klimowicz K, et al. Is a normal chest radiograph sufficient to exclude pulmonary abnormalities potentially associated with chronic cough? Adv Respir Med 2018;86:113-20. 10.5603/ARM.2018.0018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


