Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic brought remarkable disruption to the ways in which healthcare was delivered. This study aimed to examine changes in pediatric healthcare utilization in Hunan Province, China, during the COVID-19 pandemic.
Methods
An electronic survey was conducted among 142 hospitals in Hunan Province, China. Using data from January 1 to April 30, 2019 as a reference, the changes in the number of visits for different types of pediatric healthcare between January 1 and April 30, 2020 were calculated. Changes in the number of admissions for infections and injuries were also evaluated.
Results
The total number of pediatric healthcare presentations decreased by 53.3% in the first four months of 2020. The most remarkable reductions were observed in the utilization of emergency room (ranging from –45.7% to –94.9% among three hospital levels) and observation room (–55.8% to –77.7%); neonatal inpatient care experienced the smallest decreases (–21.2% to –25.5%). Approximately 85% of the total reduction in the number of pediatric inpatient admissions was attributable to the reduction in admissions for infections. A 13.3% increase in the number of admissions for injuries was observed among third-level hospitals.
Conclusions
The utilization of all types of pediatric healthcare services in Hunan Province declined markedly after the outbreak of COVID-19. The reasons, consequences, and responses to these changes should be addressed in future studies and actions.
Keywords: Coronavirus disease 2019 (COVID-19), hospital levels, infection, pediatric healthcare, service utilization
Introduction
The coronavirus disease 2019 (COVID-19) pandemic brought remarkable disruption to the ways in which healthcare was delivered. Increasing evidence from around the world has shown that the number of patients presenting to hospitals decreased dramatically after the outbreak of COVID-19 or after lockdowns due to COVID-19 (1-5).
It is widely accepted that the reduction in patients presenting to hospitals could be partly due to the reduced incidence of infectious diseases that resulted from measures aimed at mitigating and controlling the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (6-9). However, concerns that patients may avoid going to the hospital due to fear of infection with SARS-CoV-2 have grown (4,5). Similar situations were also encountered during the 2003 SARS epidemic (10). A delay in seeking healthcare could lead to adverse outcomes and increased mortality. This can be especially significant for pediatric patients, for whom delay in treatment could have long-term adverse impacts. Furthermore, healthcare-seeking behavior and the disease spectrum among pediatric patients differ from those of adult patients. Therefore, for the healthcare system to evaluate the impact of COVID-19 on pediatric healthcare and develop response plans, investigations focusing on changes in pediatric healthcare utilization after the COVID-19 pandemic outbreak are needed. Efforts around the world have been made to evaluate such changes (4,9,11-18). Many studies have reported decreases in the utilization of pediatric emergency services (4,11-17). For example, during Italy’s national lockdown for COVID-19, substantial decreases (73–88%) in pediatric emergency department (Em) visits were observed during March 1–27, 2020 (4). In a hospital in Ireland, pediatric Em attendance decreased by 51.45% for March and April 2020 compared with 2019 (15). In a single-center study in Germany, a 63.8% drop in pediatric Em healthcare utilization was observed in the four weeks after lockdown (12). Other studies also reported decreases in the utilization of pediatric intensive care units (PICUs) (18) and hospitalization services (9,11). Drops in the number of patients with infections and increases in the number of injuries were also observed (7-9,19). However, few studies have investigated the utilization of pediatric healthcare service across all hospital levels and covering all types of healthcare services. Studies with such designs, which must usually be conducted on a regional level, could provide a better overview of the impact of the COVID-19 pandemic on pediatric healthcare utilization. The present study examined changes in pediatric healthcare utilization in Hunan Province, China, during the COVID-19 pandemic.
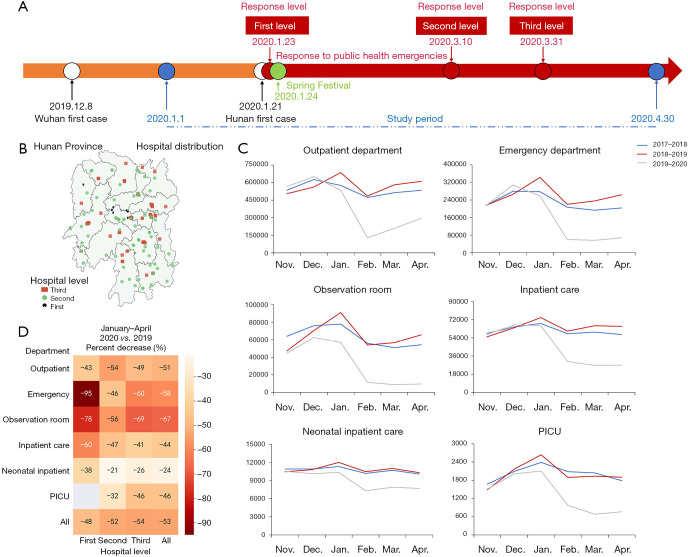
Hunan Province is adjacent to Hubei province, where the first case of COVID-19 was reported at the end of December, 2019 (Figure 1A). The population of Hunan Province was estimated at 69.18 million in 2019. By April 30, 2020, Hunan Province had reported 1019 COVID-19 cases. The platform serving the Hunan Pediatric Medical Quality Control Center and the Hunan Association of Pediatricians allowed us to conduct an electronic survey on the utilization of pediatric healthcare services among first-, second-, and third-level hospitals in Hunan Province. This study had three objectives: (I) to quantify changes in the utilization of different types of pediatric healthcare, including outpatient (Op) visits, Em presentations, observation room (Ob) admissions, and inpatient care (Ip) admissions, by calculating the percent change relative to 2019; (II) to evaluate these changes among different hospital levels; and (III) to estimate changes in the number of inpatient admissions for infections and injuries. Our findings will provide a reference for pediatric healthcare providers to evaluate the impact of COVID-19 on pediatric healthcare utilization and develop subsequent research programs and response plans. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tp-20-465).
Figure 1.
Changes in pediatric healthcare utilization in Hunan Province, China, during the COVID-19 pandemic. (A) Timeline of key events during the COVID-19 pandemic in Hunan Province. (B) Distribution of 142 study sites in Hunan Province. (C) Number of pediatric patients presenting to study sites from November to April from 2017 to 2020, organized by service type. (D) Reduction rate in the number of pediatric patients during the COVID-19 pandemic, by health service type and hospital level. January to April 2020 vs. January to April 2019. PICU, pediatric intensive care unit; COVID-19, coronavirus disease 2019.
Methods
Study design
This was a cross-sectional study using historical data for comparisons. An electronic survey was conducted among 142 hospitals participating in the Hunan Pediatric Medical Quality Control Center and the Hunan Association of Pediatricians networks in Hunan Province, including 9 first-level, 74 second-level, and 59 third-level hospitals (Figure 1B). Data were extracted from electronic medical records for each hospital. Information was collected on the number of presentations seeking pediatric healthcare (patients aged 0–18 years) in these hospitals from November to April each year from 2017 to 2020. Inpatients’ primary diagnoses were collected from 46 hospitals. In the analysis evaluating the percentage changes in healthcare utilization after the outbreak of COVID-19, the study period was January 1 to April 30, 2020, and the comparison period was January 1 to April 30, 2019.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Medical Ethics Committee of the Hunan Children’s Hospital (HCHLL-2020-81). Written informed consent was waived by the Medical Ethics Committee of the Hunan Children’s Hospital.
Measures
To evaluate the utilization of pediatric healthcare, the number of recorded visits for the following types of healthcare were investigated: Op, Em, Ob, and Ip. The number of admissions to neonatal Ip and the PICU were also collected separately.
To evaluate changes in the utilization of different healthcare types, the odds of the following visit types were calculated: Op/Em, (Op + Em)/Ob, and (Op + Em)/Ip. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to compare the odds in 2020 with those in 2019 and to evaluate the statistical significance of the changes.
Evidence showed that the outbreak of COVID-19 had an impact across the pediatric disease spectrum, especially on infectious diseases and injures (7-9,19). Therefore, we categorized inpatients’ primary diagnoses into four categories, including respiratory infection, other infections, injury, and other diseases, and investigated the percent changes and proportion changes after the outbreak. A consensus meeting was held to discuss classifications where there was disagreement. If the disagreement persisted after this discussion, a fourth clinician with a senior title made the final decision.
Important time points
Figure 1A shows the timeline with key events. It should be noted that the utilization of healthcare services was expected to decrease during the Spring Festival Holidays (lasting at least 7 days), which are usually at the end of January or the beginning of February.
Statistical analysis
The percentage changes during the study period in 2020 relative to 2019 for the total numbers of Op visits, Em presentations, Ob admissions, and Ip admissions were calculated. Poisson regression was used to calculate the type III P values to evaluate the interactions between the hospital level and the overall change. Type III P values <0.05 indicated that changes were disproportionate among different hospital levels. ORs for indicated visit types were calculated as the ratios of the odds of hospital visit types of interest during the study period in 2020 (Jan. 1 to Apr. 30) to the same odds during the comparison period in 2019. The 95%CI of the OR was calculated using the following formula (20):
| [1] |
| [2] |
where a and b are the number of presentations needed to calculate the odds in 2019, and c and d are the number of each presentation type in 2020 [e.g., for the odds of (Op + Ed)/Ob, a = (Op + Ed)2019, and b = Ob2019, c = (Op + Ed)2020, and d = Ob2020]. To evaluate changes in the number of certain disease types among inpatients, rate ratios (RRs) were calculated by dividing the number of patients with the diagnosis of interest during the study period in 2020 by that number in 2019, assuming that the total number of children in Hunan Province was stable during 2019 and 2020. The 95% CI of the RR was calculated using the following formula (20):
| [3] |
where a is the number of admissions categorized as the disease of interest during the study period in 2020, and c is that number during the comparison period in 2019. Changes in ratios were considered statistically significant if the 95% CI of the OR or RR excluded 1.0. Chi-square tests were used to compare changes in disease proportions between 2020 and 2019. All tests of hypotheses were two tailed and the type 1 error rate was fixed at 5%. Missing data were not imputed. Statistical analyses were performed using SAS 9.3 (SAS Institute, Inc., Cary, NC, USA). The PROC GENMOD procedure was applied for the Poisson regression.
Results
Overall changes in pediatric healthcare visit numbers
Figure 1C shows the number of pediatric healthcare visits at the study sites between November and April in the three recent years. Compared with the two years before the COVID-19 pandemic, the number of visits started to decline in January 2020 for all healthcare service types, and the declining trend has attenuated or rebounded since March 2020.
Changes according to healthcare service type and hospital level
Table 1 shows the changes in the number of pediatric patients from January to April after the pandemic began. Overall, the total number of healthcare presentations among our 142 study sites decreased by 53.3% compared with the same period in 2019. The percentage change in the total number of healthcare visits among the first-, second-, and third-level hospitals were –48.1%, –52.4%, –53.7%, respectively. Declines in the number of visits were observed for all visit types and at all hospital levels. Type III P values for the interaction between year and hospital level revealed significantly disproportionate decreases at all three hospital levels.
Table 1. Changes in the number of pediatric patients during the COVID-19 pandemic, by visit type and hospital level.
| Visit type | Hospital level | No. of site | January–April | Percent change (%) | P† | |
|---|---|---|---|---|---|---|
| 2019 (comparison) | 2020 (COVID-19) | |||||
| Outpatient department | First-level | 9 | 16,212 | 9,201 | −43.3 | <0.0001 |
| Second-level | 73 | 778,703 | 355,049 | −54.4 | ||
| Third-level | 58 | 1,567,360 | 803,976 | −48.7 | ||
| All | 140 | 2,362,275 | 1,168,226 | −50.6 | ||
| Emergency department | First-level | 1 | 296 | 15 | −94.9 | <0.0001 |
| Second-level | 35 | 143,946 | 78,209 | −45.7 | ||
| Third-level | 45 | 917,042 | 363,348 | −60.4 | ||
| All | 81 | 1,061,284 | 441,572 | −58.4 | ||
| Observation room | First-level | 1 | 112 | 25 | −77.7 | <0.0001 |
| Second-level | 22 | 26,827 | 11,871 | −55.8 | ||
| Third-level | 40 | 240,051 | 75,190 | −68.7 | ||
| All | 63 | 266,990 | 87,086 | −67.4 | ||
| Inpatient care | First-level | 8 | 5,210 | 2,089 | −59.9 | <0.0001 |
| Second-level | 69 | 114,463 | 61,202 | −46.5 | ||
| Third-level | 59 | 146,243 | 86,927 | −40.6 | ||
| All | 136 | 265,916 | 150,218 | −43.5 | ||
| Neonatal inpatient care | First-level | 1 | 139 | 86 | −38.1 | <0.0001 |
| Second-level | 60 | 16,948 | 13,353 | −21.2 | ||
| Third-level | 55 | 26,705 | 19,814 | −25.8 | ||
| All | 116 | 43,792 | 33,253 | −24.1 | ||
| PICU | First-level | 0 | ||||
| Second-level | 6 | 300 | 205 | −31.7 | 0.0087 | |
| Third-level | 28 | 8,060 | 4,312 | −46.5 | ||
| All | 34 | 8,360 | 4,517 | −46.0 | ||
| All types | First-level | 9 | 21,830 | 11,330 | −48.1 | <0.0001 |
| Second-level | 74 | 1,063,939 | 506,331 | −52.4 | ||
| Third-level | 59 | 2,870,696 | 1,329,441 | −53.7 | ||
| All | 142 | 3,956,465 | 1,847,102 | −53.3 | ||
†, type III P values for the interaction between the overall change among all hospitals and change in each hospital levels. A type III P values <0.05 indicated that changes were disproportionate among different hospital levels. PICU, pediatric intensive care unit; COVID-19, coronavirus disease 2019.
As shown in the heat map (Figure 1D), the most remarkable reductions (percentage decrease) were observed in utilization of the Em (–45.7% to –94.9%) and Ob (–55.8% to –77.7%); neonatal inpatient care experienced the smallest decreases (–21.2% to –25.5%). Among the three hospital levels, the first-level hospitals had the sharpest percentage decreases in utilization of the Em, Ob, Ip, and neonatal inpatient care.
Table 2 compares the odds of different healthcare types from January to April in 2020 and 2019. The direction of changes differed among the three hospital levels for the odds of Op/Em and the odds of (Op + Em)/Ip. The odds of (Op + Em)/Ob were increased among all hospital levels.
Table 2. Comparison of the odds of visits according to different service types between January–April 2019 and January–April 2020.
| Odds for service types | Hospital level | Odds2019 | Odds2020 | OR (95% CI)† |
|---|---|---|---|---|
| Op/Em | First-level | 54.8 | 613.4 | 11.2 (6.66, 18.83) |
| Second-level | 5.4 | 4.5 | 0.84 (0.83, 0.85) | |
| Third-level | 1.7 | 2.2 | 1.30 (1.29, 1.30) | |
| All | 2.2 | 2.6 | 1.19 (1.18, 1.19) | |
| (Op + Em)/Ob | First-level | 147.4 | 368.6 | 2.50 (1.62, 3.86) |
| Second-level | 34.4 | 36.5 | 1.06 (1.04, 1.09) | |
| Third-level | 10.3 | 15.5 | 1.50 (1.49, 1.51) | |
| All | 12.8 | 18.5 | 1.44 (1.43, 1.45) | |
| (Op + Em)/Ip | First-level | 3.2 | 4.4 | 1.39 (1.32, 1.47) |
| Second-level | 8.1 | 7.1 | 0.88 (0.87, 0.89) | |
| Third-level | 17.0 | 13.4 | 0.79 (0.78, 0.8) | |
| All | 12.9 | 10.7 | 0.83 (0.83, 0.84) |
†, ORs were calculated as Odds2020/Odds2019 in 2019. Statistical significance of changes in ratios were determined if the 95% CI of the OR excluded 1.0. CI, confidence interval; Ip, inpatient care; Ob, observation room; Op, outpatient; Em, emergency department; OR, odds ratio.
Changes in the number of inpatients by disease categories
Table 3 shows the changes in the number of inpatients by disease category. Among all study sites, the number of inpatient admissions with respiratory infections and other infections declined by 58.2% and 44.3%, respectively, with significant decreases at all hospital levels. The reduction in the number of respiratory infections and other infections accounted for 71% and 11.8% of total reductions, respectively. Changes in the number of injuries were not significant in first- and second-level hospitals; a significant increase in the number of injury cases was observed in third-level hospitals (percent change: +13.3%, RR =1.13, 95% CI: 1.03, 1.24).
Table 3. Changes in the number of inpatients by disease categories during the COVID-19 pandemic.
| Hospital level | Primary diagnosis | January–April | Change | Proportion in total change (%) | % change | RR (95% CI)† | |
|---|---|---|---|---|---|---|---|
| 2019 (comparison) | 2020 (COVID-19) | ||||||
| First-level | Respiratory infection | 2,436 | 924 | −1,512 | 96.2 | −62.1 | 0.38 (0.35, 0.41) |
| Other infections | 132 | 67 | −65 | 4.1 | −49.2 | 0.51 (0.38, 0.68) | |
| Injury | 6 | 4 | −2 | 0.1 | −33.3 | 0.67 (0.19, 2.37) | |
| Other diseases | 22 | 29 | 7 | −0.4 | 31.8 | 1.32 (0.76, 2.30) | |
| Total | 2,596 | 1,024 | −1,572 | 100 | −60.6 | 0.39 (0.36, 0.42) | |
| Second-level | Respiratory infection | 27,709 | 11,378 | −16,331 | 80.7 | −58.9 | 0.41 (0.40, 0.42) |
| Other infections | 5,197 | 2,648 | −2,549 | 12.6 | −49.1 | 0.51 (0.49, 0.53) | |
| Injury | 191 | 165 | −26 | 0.1 | −13.6 | 0.86 (0.70, 1.06) | |
| Other diseases | 5,152 | 3,809 | −1,343 | 6.6 | −26.1 | 0.74 (0.71, 0.77) | |
| Total | 38,249 | 18,000 | −20,249 | 100 | −52.9 | 0.47 (0.46, 0.48) | |
| Third-level | Respiratory infection | 22,969 | 9,917 | −13,052 | 67.5 | −56.8 | 0.43 (0.42, 0.44) |
| Other infections | 5,605 | 3,381 | −2,224 | 11.5 | −39.7 | 0.60 (0.57, 0.63) | |
| Injury | 787 | 892 | 105 | −0.5 | 13.3 | 1.13 (1.03, 1.24) | |
| Other diseases | 16,497 | 12,334 | −4,163 | 21.5 | −25.2 | 0.75 (0.73, 0.77) | |
| Total | 45,858 | 26,524 | −19,334 | 100 | −42.2 | 0.58 (0.57, 0.59) | |
| All | Respiratory infection | 53,114 | 22,219 | −30,895 | 75.1 | −58.2 | 0.42 (0.41, 0.43) |
| Other infections | 10,934 | 6,096 | −4,838 | 11.8 | −44.3 | 0.56 (0.54, 0.58) | |
| Injury | 984 | 1,061 | 77 | −0.2 | 7.8 | 1.08 (0.99, 1.18) | |
| Other diseases | 21,671 | 16,172 | −5,499 | 13.4 | −25.4 | 0.75 (0.73, 0.77) | |
| Total | 86,703 | 45,548 | −41,155 | 100 | −47.5 | 0.53 (0.52,0.54) | |
†, statistical significance of changes in ratios were determined if the 95% CI of the RR excluded 1.0. CI, confidence interval; RR, rate ratio; COVID-19, coronavirus disease 2019.
In 2019, 61.26% of inpatients at the study sites had a primary diagnosis that could be categorized as respiratory infection, and in 2020, the proportion declined to 48.78% (Table 4). Significant changes in these proportions were observed at all hospital levels; the proportion of respiratory infections decreased, whereas the proportions of other disease categories increased.
Table 4. Changes in the distribution of diseases among pediatric inpatients during the COVID-19 pandemic (January–April 2020 vs. January–April 2019).
| Hospital level | Diagnosis | 2019 (comparison) | 2020 (COVID-19) | P | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| First-level | Respiratory infection | 2,436 | 93.84 | 924 | 90.23 | <0.0001 | |
| Other infections | 132 | 5.08 | 67 | 6.54 | |||
| Injury | 6 | 0.23 | 4 | 0.39 | |||
| Other diseases | 22 | 0.85 | 29 | 2.83 | |||
| Second-level | Respiratory infection | 27,709 | 72.44 | 11,378 | 63.21 | <0.0001 | |
| Other infections | 5,197 | 13.59 | 2,648 | 14.71 | |||
| Injury | 191 | 0.50 | 165 | 0.92 | |||
| Other diseases | 5,152 | 13.47 | 3,809 | 21.16 | |||
| Third-level | Respiratory infection | 22,969 | 50.09 | 9,917 | 37.39 | <0.0001 | |
| Other infections | 5,605 | 12.22 | 3,381 | 12.75 | |||
| Injury | 787 | 1.72 | 892 | 3.36 | |||
| Other diseases | 16,497 | 35.97 | 12,334 | 46.50 | |||
| All | Respiratory infection | 53,114 | 61.26 | 22,219 | 48.78 | <0.0001 | |
| Other infections | 10,934 | 12.61 | 6,096 | 13.38 | |||
| Injury | 984 | 1.13 | 1,061 | 2.33 | |||
| Other diseases | 21,671 | 24.99 | 16,172 | 35.51 | |||
Discussion
Among the different types of healthcare, the Ob showed the greatest reduction in utilization, followed by the Em. The utilization of neonatal inpatient care was least affected by COVID-19. Approximately 85% of the total reduction in the number of pediatric inpatients could be attributed to the reduction in infections, and 13.3% of the increase in the number of injuries was observed among the third-level hospitals.
Remarkable reductions in the utilization of pediatric healthcare services were observed among our study sites. The reduction could be partly due to restrictive measures such as lockdowns, social distancing, travel restrictions, and school closures, which likely reduced the spread of infectious diseases (6-9). However, the pandemic did not decrease the incidence of all diseases. Evidence has suggested that the observed reductions may be a result of changes in healthcare-seeking behavior after the outbreak of COVID-19 (4,10). By analyzing the pattern of change among different hospital levels and healthcare types, as well as changes in disease compositions, our study evaluated the impact of COVID-19 on the pediatric healthcare system. Our findings could have implications for the adaptation and optimization of pediatric healthcare delivery in the post-pandemic era (21,22), and can serve as a reference for the development of emergency response plans for epidemics.
The utilization of pediatric services in first-, second-, and third-level hospitals has been disproportionately affected by COVID-19. First-level hospitals experienced the greatest changes in volumes of Em, Ob, and Ip utilizations, suggesting that first-level hospitals are the most vulnerable during and after an epidemic. First-level hospitals are supposed to provide the most fundamental healthcare to the community. However, they suffer from constraints of limited medical resources; they are less prepared for an epidemic and find it difficult to adapt quickly to changes under such stress. As a consequence, people seeking healthcare are less likely to choose a first-level hospital during an epidemic. Our findings suggested that emphasis should be placed on strengthening the emergency response capacity of first-level hospitals, especially in remote areas where the community might have limited access to secondary and tertiary hospitals. The roles of the three hospital levels and transport plans should also be addressed as a part of any emergency response.
The greatest percentage change among different service types was observed in admissions for Ob services (overall percentage change=–67.4%). The volume of Ob admissions may have been most affected by the pandemic because both physicians and patients/guardians tended to avoid unnecessary hospital stays. A drop of 58.4% in pediatric Em attendance was observed in our study. Similar reductions were observed in many places around the world, ranging from a 30.4% drop in hospitals in Greater Manchester to an 88% decrease in regions of Italy (4,14-17). Although evidence has shown that the reduction in Em presentations was caused by a combination of factors, including a reduction in the incidence of respiratory diseases, reduction in injuries from outdoor activities, parents’ hesitancy to visit the hospital during the pandemic, and/or evaluating a condition as non-emergent (4,11-15,18). A great concern with regard to the decrease in pediatric Em visits was that patients who needed to receive Em healthcare did not visit the hospital, resulting in delayed treatment and adverse health outcomes (4,11-15,18). In addition to differences in the disease spectrum, one large difference between adult and pediatric Em attendance is that the decision regarding pediatric attendance is usually made by the child’s parents or guardians. Therefore, guardians’ appropriate evaluation of their children’s medical conditions is essential for their subsequent healthcare-seeking behavior. To avoid delayed hospital visits, health services should develop response plans such as delivering education programs for parents to reduce healthcare avoidance or providing pre-hospital phone-call evaluation services to give advice on hospital attendance.
The odds of (Op + Em)/Ip decreased at all hospital levels. As the absolute number of Op, Em, and Ip admissions were all decreased, the disproportionate change suggests that patients who did not need inpatient care were less likely to present to hospitals. This finding is in accordance with other reports, which found that the majority of reductions in pediatric visits were related to mild conditions or non-severe illnesses (4,12). For those with mild conditions or non-severe illnesses, parents may have found other ways of accessing treatment without going to the hospital (23,24). For example, online consultations were provided by many hospitals in Hunan Province as an emergency response. Globally, considerable effort has been made to promote telemedicine during the COVID-19 pandemic (25,26); however, the efficacy of these supplementary healthcare services should be further investigated. Subsequent monitoring of the ratios of different healthcare types is also needed, as this could provide valuable information for the allocation of medical resources within hospitals.
As expected, the number of admissions with infections, especially respiratory infections, markedly decreased at our study sites after the outbreak. Our findings were in accordance with those from a single-center study in Hangzhou City, China, which showed that most decreases in pediatric Op visits after the outbreak of COVID-19 were for infectious diseases such as respiratory syncytial virus infection, influenza, infectious diarrhea, rotavirus enteritis, and hand-foot-mouth disease (19). Studies outside China also reported declines in the number of pediatric respiratory infection-related hospitalizations (7-9). Zhang et al. built a transmission model and found that the social distancing implemented in China during the outbreak was sufficient to control COVID-19 (6). Therefore, the incidence of other infectious diseases that can be transmitted through daily contacts was likely also controlled during the COVID-19-related social distancing period. Nevertheless, it is impossible to determine how many reductions were due to decreased incidence and how many were due to changes in healthcare-seeking behavior. Like hospitals around the world that had made quick responses to the changes (27,28), hospitals in Hunan Province were divided, from the main entrance and throughout the hospital, into an infectious channel and non-infectious channel. This adaptation was intended to control in-hospital transmission and reduce the impact on healthcare-seeking for patients with non-infectious diseases. However, patients with infectious diseases might avoid going to the hospital because of fear. Strategies are needed to address this fear among patients with infectious diseases other than COVID-19.
In our study, the number of inpatients admitted for injuries increased among third-level hospitals. Increases in the number of Op visits for injuries were reported in a single-center study in Hangzhou, China (19). However, decreases in the number of injuries have also been reported (15). In a single center in Ireland, Em attendance for injury and poisoning between March and April 2020 decreased by 44.7% compared with 2019 (15). Although the number of injuries may have decreased because of reduced outdoor activities, there were concerns that measures being taken to control the spread of COVID-19 could put children at risk of child neglect and abuse (29). Therefore, an increased number of injuries may have been caused by safeguarding failure, parental burnout, and child maltreatment during the COVID-19 pandemic (30). The reasons for the unchanged or even increased number of injury cases in our study warrants further investigation, as such information could be used to guide the development of preventive intervention plans for similar events in the future, such as city lockdowns or school closures.
In addition to the allocation of medical resources for responding to a pandemic, hospital systems’ response plans for a pandemic should also include the efficient delivery of public information, adaptations to changes in healthcare-seeking behavior, and adaptations to the restriction of community services. In any situation, circumstances such as patients who waited until they collapsed before seeking healthcare should be avoided. Guardians may face difficult choices when a child requires healthcare during an epidemic. On the one hand, children are thought to be vulnerable to contacting infectious disease, so guardians are reluctant to take them to the hospital during an epidemic (4); on the other hand, a delay in treatment can be life-threatening or can have life-long adverse effects on a child’s health. In addition, restrictions on community services and transportation links during an epidemic could disrupt the routine healthcare-seeking behavior. Therefore, delivery of immediate and adequate information to guide guardians whose child might require healthcare services is essential to the efficient delivery of those services (31).
Both the child’s guardians and healthcare system need time to adjust to the changes that follow by a pandemic like COVID-19. An evaluation of response efficacy is essential for the development of future emergency response plans. As we saw from the impact of the SARS epidemic on the utilization of healthcare services (10,32), changes in patterns of pediatric healthcare utilization after the outbreak of COVID-19 promise to be much longer lasting than the period covered in this study. At our study sites, patient volumes started to decrease in January 2020; increases in patient volumes were observed in April and the volumes are expected to continue increasing. However, until the COVID-19 pandemic ends, accompanied by a return to routine epidemic prevention and control practices in China, the observed changes in pediatric healthcare utilization are expected to last, especially for Ob and Em services. Whether the pandemic will change the social behavior of seeking healthcare in the long-term is not yet know. Answering this question will be important for health organizations’ adaptation to these changes and for planning strategies to deliver high-quality care to those who need it.
The strengths of this study included it was a multicenter study conducted at a provincial level; it covered all pediatric healthcare types and included all three hospital levels; it investigated changes by visit types and disease categories; and it calculated both percent change and relative ratios for the changes among different service types. Therefore, this study provides a representative reference for future studies and for hospital systems that are facing or will be facing similar challenges. This study has several limitations. First, the study sites were not selected by stratified sampling, so we could not estimate the number of changes on the provincial level using weighting methods. Second, this was a hospital-based study, therefore we were unable to evaluate how many pediatric patients needed healthcare but did not seek care. Third, we could not estimate how many patients had received delayed treatment. Fourth, the disease categories of respiratory infection diseases, other infections, and injuries were identified from the primary diagnosis included in the medical records; misclassification is possible, although we speculate that any such misclassification was non-differential and should therefore have limited impact on our estimation of percentage changes after the COVID-19 pandemic (33).
Conclusions
To summarize, the utilization of all types of pediatric healthcare in Hunan Province declined by over 50% within the first 4 months after the outbreak of COVID-19, and disproportionate changes were observed among different hospital levels and service types. Among pediatric inpatients, the number of respiratory infections was reduced at all hospital levels, whereas the number of injuries was increased in third-level hospitals. The reasons, consequences, and responses to these changes should be addressed in future studies.
Supplementary
The article’s supplementary files as
Acknowledgments
We thank the members from the Hunan Pediatric Medical Quality Control Center and the Hunan Association of Pediatricians networks for their participation in the survey. English in the manuscript was proofread by Textcheck (http://www.textcheck.com).
Funding: This work was funded by the Hunan Provincial Science and Technology Department Project (No. 2018SK2135, 2020SK1014-3), the Hunan Provincial Key Laboratory of Emergency Medicine for Children (No. 2018TP1028), and the Hunan Provincial Key Laboratory of Metabolomics in Critical Care Medicine (No. 2017TP1034). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Medical Ethics Committee of the Hunan Children’s Hospital (HCHLL-2020-81). Written informed consent was waived by the Medical Ethics Committee of the Hunan Children’s Hospital.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tp-20-465
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tp-20-465
Peer Review File: Available at http://dx.doi.org/10.21037/tp-20-465
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp-20-465). The authors have no conflicts of interest to declare.
References
- 1.Thornton J. Covid-19: A&E visits in England fall by 25% in week after lockdown. BMJ 2020;369:m1401. 10.1136/bmj.m1401 [DOI] [PubMed] [Google Scholar]
- 2.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol 2020;75:2871-2. 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tam CF, Cheung KS, Lam S, et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes 2020;13:e006631. 10.1161/CIRCOUTCOMES.120.006631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lazzerini M, Barbi E, Apicella A, et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020;4:e10-1. 10.1016/S2352-4642(20)30108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosenbaum L. The Untold Toll - The Pandemic's Effects on Patients without Covid-19. N Engl J Med 2020;382:2368-71. 10.1056/NEJMms2009984 [DOI] [PubMed] [Google Scholar]
- 6.Zhang J, Litvinova M, Liang Y, et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 2020;368:1481-6. 10.1126/science.abb8001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nascimento MS, Baggio DM, Fascina LP, et al. Impact of social isolation due to COVID-19 on the seasonality of pediatric respiratory diseases. PLoS One 2020;15:e0243694. 10.1371/journal.pone.0243694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuitunen I, Artama M, Mäkelä L, et al. Effect of Social Distancing Due to the COVID-19 Pandemic on the Incidence of Viral Respiratory Tract Infections in Children in Finland During Early 2020. Pediatr Infect Dis J 2020;39:e423-7. 10.1097/INF.0000000000002845 [DOI] [PubMed] [Google Scholar]
- 9.Gavish R, Krause I, Goldberg L, et al. A Drop in Number of Hospitalizations Among Children with Bacterial Infections During the COVID-19 Pandemic. Pediatr Infect Dis J 2021;40:e39-41. 10.1097/INF.0000000000002963 [DOI] [PubMed] [Google Scholar]
- 10.Chang HJ, Huang N, Lee CH, et al. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health 2004;94:562-4. 10.2105/AJPH.94.4.562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chong SL, Soo JSL, Allen JC, Jr, et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr 2020;20:562. 10.1186/s12887-020-02469-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dopfer C, Wetzke M, Zychlinsky Scharff A, et al. COVID-19 related reduction in pediatric emergency healthcare utilization - a concerning trend. BMC Pediatr 2020;20:427. 10.1186/s12887-020-02303-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davico C, Marcotulli D, Lux C, et al. Where have the children with epilepsy gone? An observational study of seizure-related accesses to emergency department at the time of COVID-19. Seizure 2020;83:38-40. 10.1016/j.seizure.2020.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chaiyachati BH, Agawu A, Zorc JJ, et al. Trends in Pediatric Emergency Department Utilization after Institution of Coronavirus Disease-19 Mandatory Social Distancing. J Pediatr 2020;226:274-277.e1. 10.1016/j.jpeds.2020.07.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dann L, Fitzsimons J, Gorman KM, et al. Disappearing act: COVID-19 and paediatric emergency department attendances. Arch Dis Child 2020;105:810-1. 10.1136/archdischild-2020-319654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roland D, Harwood R, Bishop N, et al. Children's emergency presentations during the COVID-19 pandemic. Lancet Child Adolesc Health 2020;4:e32-3. 10.1016/S2352-4642(20)30206-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Isba R, Edge R, Jenner R, et al. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child 2020;105:704. 10.1136/archdischild-2020-319385 [DOI] [PubMed] [Google Scholar]
- 18.Sperotto F, Wolfler A, Biban P, et al. Unplanned and medical admissions to pediatric intensive care units significantly decreased during COVID-19 outbreak in Northern Italy. Eur J Pediatr 2021;180:643-8. 10.1007/s00431-020-03832-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li H, Yu G, Duan H, et al. Changes in Children's Healthcare Visits During Coronavirus Disease-2019 Pandemic in Hangzhou, China. J Pediatr 2020;224:146-9. 10.1016/j.jpeds.2020.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. Lippincott Williams & Wilkins, 2008. [Google Scholar]
- 21.Sokol DK. Virulent epidemics and scope of healthcare workers' duty of care. Emerg Infect Dis 2006;12:1238-41. 10.3201/eid1208.060360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Voo TC, Capps B. Influenza pandemic and the duties of healthcare professionals. Singapore Med J 2010;51:275-81. [PubMed] [Google Scholar]
- 23.Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med 2020;382:1679-81. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 24.Valentino LA, Skinner MW, Pipe SW. The role of telemedicine in the delivery of health care in the COVID-19 pandemic. Haemophilia 2020;26:e230-1. 10.1111/hae.14044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc 2020;27:1132-5. 10.1093/jamia/ocaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wijesooriya NR, Mishra V, Brand PLP, et al. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev 2020;35:38-42. 10.1016/j.prrv.2020.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 2020;395:1678-80. 10.1016/S0140-6736(20)31067-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan RMR, Ong GY, Chong SL, et al. Dynamic adaptation to COVID-19 in a Singapore paediatric emergency department. Emerg Med J 2020;37:252-4. [DOI] [PubMed] [Google Scholar]
- 29.Green P. Risks to children and young people during covid-19 pandemic. BMJ 2020;369:m1669. 10.1136/bmj.m1669 [DOI] [PubMed] [Google Scholar]
- 30.Griffith AK. Parental Burnout and Child Maltreatment During the COVID-19 Pandemic. J Fam Violence 2020. [Epub ahead of print]. doi: . 10.1007/s10896-020-00172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lynn RM, Avis JL, Lenton S, et al. Delayed access to care and late presentations in children during the COVID-19 pandemic: a snapshot survey of 4075 paediatricians in the UK and Ireland. Arch Dis Child 2021;106:e8. 10.1136/archdischild-2020-319848 [DOI] [PubMed] [Google Scholar]
- 32.Huang YT, Lee YC, Hsiao CJ. Hospitalization for ambulatory-care-sensitive conditions in Taiwan following the SARS outbreak: a population-based interrupted time series study. J Formos Med Assoc 2009;108:386-94. 10.1016/S0929-6646(09)60082-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Whitcomb BW, Naimi AI. Things Don't Always Go as Expected: The Example of Nondifferential Misclassification of Exposure-Bias and Error. Am J Epidemiol 2020;189:365-8. 10.1093/aje/kwaa020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as