Abstract
Objectives:
The Working Mind is a program designed to reduce stigmatizing attitudes toward mental illness, improve resilience, and promote mental health in the general workplace. Previous research has revealed positive program effects in a variety of workplace settings. This study advances previous work in implementing randomization and a control group to assess the intervention’s efficacy.
Methods:
The program was evaluated using a cluster-randomized design, with pretest, posttest, and a 3-month follow-up in 2 implementation groups across 4 sites.
Results:
The Working Mind program was effective at decreasing mental health stigma and increasing self-reported resilience and coping skills at the pre–post assessment in both delivery groups. The program’s effects were maintained to the time of 3-month follow-up. Qualitative data provided further evidence that participants benefited from the program.
Conclusions:
This study represents an advancement over past research and provides further support for efficacy of the Working Mind program. Directions for future research, including replication using rigorous methodological procedures and examination of program effects over longer follow-up intervals, are discussed.
Keywords: stigma, mental health, randomization, evaluation
Abstract
Objectifs:
L’Esprit au travail est un programme conçu pour réduire les attitudes stigmatisantes à l’endroit de la maladie mentale, améliorer la résilience et promouvoir la santé mentale en milieu de travail général. La recherche précédente a révélé des effets positifs du programme dans divers milieux de travail. La présente étude ajoute aux travaux antérieurs en mettant en œuvre la randomisation et un groupe témoin afin d’évaluer l’efficacité de l’intervention.
Méthode:
Le programme a été évalué à l’aide d’une méthode randomisée en grappes, avec un suivi avant, après et à 3 mois dans 2 groupes de mise en œuvre répartis dans 4 sites.
Résultats:
Le programme l’Esprit au travail a été efficace pour réduire la stigmatisation de la santé mentale et accroître la résilience et les capacités d’adaptation auto-déclarées lors de l’évaluation avant et après des deux groupes de mise en œuvre. Les effets du programme se maintenaient au moment du suivi de 3 mois. Les données qualitatives ont fourni plus de données probantes indiquant que les participants bénéficiaient du programme.
Conclusions:
Cette étude représente un progrès par rapport à la recherche précédente, et apporte plus d’appui à l’efficacité du programme l’Esprit au travail. Les orientations de la future recherche, notamment une réplication utilisant des procédures méthodologiques rigoureuses et l’examen des effets du programme sur des intervalles de suivi plus longs sont discutés.
Mental health issues in the workplace have become a dominant occupational health concern in Canada.1 Poor mental health is associated with diminished productivity and higher absence rates,2 suboptimal work performance and difficulties with work confidence and work goals,3 and low job satisfaction.4,5 In reciprocal fashion, work-related stress factors, including job insecurity, job demands, organizational changes, workplace conflict, and low social support, are detrimental to mental and physical health.6 Mental health problems increase health-care utilization, presenteeism, and absenteeism and reduce health-related quality of life.7,8
It has been estimated that more than 70% of young people and adults who experience mental health issues receive no treatment.9 This treatment gap is affected by: (a) lack of knowledge about signs and symptoms of mental illnesses, (b) lack of knowledge about treatment options; (c) prejudicial attitudes toward people experiencing mental illness; and (d) systemic discrimination against people with mental problems, including limited public service and expensive private alternatives.10 The combination of these circumstances affects reluctance to seek treatment, delays in seeking appropriate care, and discontinuation of service.
Distinctive features of mental health stigma in the work context have been described.11 Stigma enables exclusionary workplace practices, such as lack of career advancement, marginalization from full work integration, inequity in workplace policies, reduced responsibilities, and decreased participation in social activities at work. Stigma also predicts a reduced likelihood of hiring and a cycle of precarious job positions and unemployment.
Mental health strategies are needed in the workplace to promote mental health, prevent mental illness where possible, provide access to the appropriate services, reduce stigma, assist employees who are struggling, and generally foster a supportive workplace culture.12 Workplace mental health can also be supported by various policies, including the National Standard for Psychological Health and Safety in the Workplace created by the Mental Health Commission of Canada,13 and comparable standards in other countries.14–17
Several critical components exist for effective workplace-based disability prevention programs, these aspects include access to treatment and navigation through the disability management system.18 A review of workplace anti-stigma prevention programs unfortunately revealed that many programs purporting to reduce stigma and promote mental health in the workplace do not evaluate their intervention effects, use program acceptability as an outcome index, or do not publish their results as they are proprietary.19
The Mental Health Commission of Canada has undertaken an anti-stigma initiative called Opening Minds (OM) to assess and reduce stigmatizing attitudes, beliefs, and behavioral intentions of Canadians toward people with a mental illness.20 OM has targeted various audiences, including health-care providers, youth, the workforce, and media.21 For example, the Road to Mental Readiness (R2MR) for First Responders program was adapted from a program developed by the Canadian Department of National Defence and then applied to multiple first responder groups.22,23 The Working Mind is an adaptation of the R2MR program for the general workplace. The program attempts to reduce stigma toward persons with mental health illnesses, ameliorate awareness of various signs of mental health using the Mental Health Continuum Model, improve coping and resiliency skills (RS), educate about policies and practices to promote mental health in the workplace, and assist employees to seek support when needed.12 A key element of the program is contact-based education, where individuals who experienced a mental health illness and have recovered or are in recovery tell their stories.
The Working Mind program has been evaluated in many workplaces across Canada.12 Evaluation results reveal modest reductions in stigma and increased coping skills that generally last through 3-month follow-up evaluations.12 Unfortunately, because employers typically adopt and then simply implement the program, it has been difficult to conduct more sophisticated study designs, such as including randomization. The current article represents a cluster-randomization trial of the program delivered in a large provincial employer within Canada in both an immediate and delayed format. It was predicted that the program would demonstrate by stigma reduction and resiliency improvement outcomes, consistent with previous research. It was further predicted that these results would only be evidenced once the program was delivered, but not while the delayed implementation group was waiting.
Methods
Study Design and Participants
The study used a cluster-randomized trial design and was implemented in the Nova Scotia Health Authority (NSHA), with the support of the Mental Health Commission of Canada. Participants were recruited through the Occupational Health, Safety & Wellness branch of the NSHA in geographically distinct sites of the province, through requests sent to managers in various programs of the NSHA. A total of 4 sites asked for participation in the study, including 2 office sites and 2 sites comprised of kitchen and maintenance staff.
Procedures
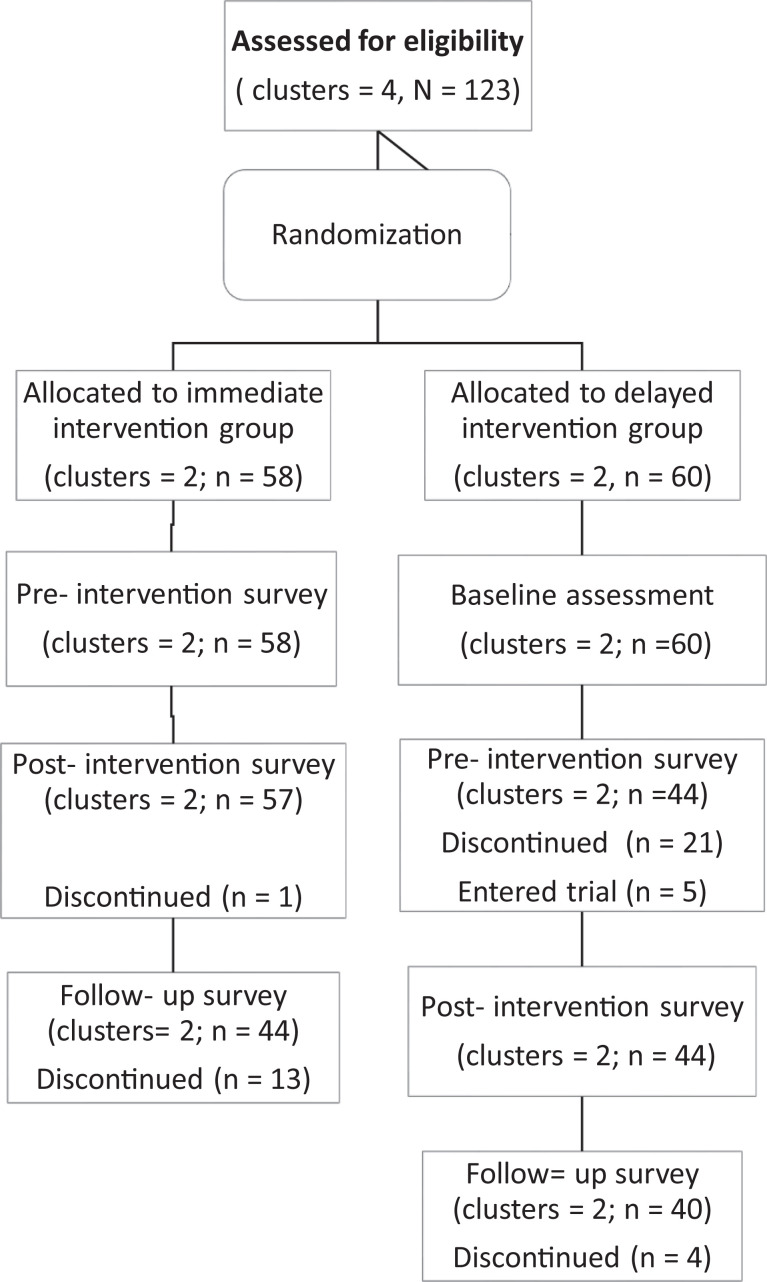
Sites were randomly assigned by the first author, without knowledge of location or workforce positions, to an immediate or delayed implementation group. By chance, the 2 clusters of office workers were allocated to the immediate intervention group, whereas the other staff clusters were allocated to the delayed intervention group. The immediate implementation group consisted of 58 participants, who engaged in the program immediately after completing the presurvey. They also completed the assessment measures at 2 other time points, immediately after the program’s completion, and at a 3-month follow-up period. The delayed implementation group consisted of 60 participants, who received the program after a 3-month delay. Their outcomes were assessed at the baseline (i.e., the same time point when the immediate group completed the presurvey), just before the program (at a 3-month delay in comparison to the immediate group), immediately at the program’s conclusion, and at a 3-month follow-up period. Figure 1 presents the CONSORT diagram of participant flow.
Figure 1.
CONSORT flow diagram. Note. The immediate intervention group participated in the study for a total of 3 months, including the pre- and postintervention surveys, plus a 3-month follow-up assessment; the delayed intervention group participated in the study for a total of 6 months, as they waited for 3 months after the baseline assessment until they took part in the intervention and then underwent the same assessment as the immediate intervention group.
Outcome Measures
Stigma
Stigma was measured using the Opening Minds Scale for Workplace Attitudes (OMS-WA).21 The OMS-WA is a 22-item self-report questionnaire developed to assess attitudes, stereotypes, and behavioral intentions toward people experiencing mental health issues.12,23 Good internal consistency (i.e., α > .7) of this measure was reported in previous studies.21,24
Resiliency skills
RS were examined by a 5-item scale, specifically designed for the R2MR for First Responders program.12,23 This scale reflects participants’ perceptions of their skill level and ability to recover from adverse or traumatic event.
Mental health coping scale
The Mental Health Coping Scale12 consisted of 5 items which explored participants’ perceived understanding of mental health in the workplace, their intentions toward seeking help, and their willingness to support a colleague in regard to mental health in the workplace.
Open-ended questions
At the 3-month follow-up period, participants were asked if they had used any of what they had learned in The Working Mind program at work or at home (yes/no response), and if yes, to provide more details in their responses. Open-ended responses were analyzed for themes.
Training and ethics approval
Training of the trainers was provided by the Mental Health Commission of Canada (MHCC), but the actual trainers were from the employer. Ethics approval for the project was obtained form the University of Calgary Conjoint Faculties Research Ethics Board (REB# 14-1620).
Results
The data for this study were collected by paper and pencil completion of all measures, except for the follow-up data for the immediate delivery group, as these data were obtained through email completion of the questionnaires. Data were collected and sent from the site where the questionnaires were completed to the University of Calgary, where the data were entered into a computer file. All surveys were collected with identifying information but the employer was not provided this information. Data were checked for errors and omissions. If data points were missing within a given scale (n = 14), the scale score was prorated based on the available item responses. No estimation was made of other missing data, and the Last Observation Carried Forward methodology was not employed, as this method can bias study results in longitudinal data sets.25 Descriptive statistics and preliminary analyses of the internal reliabilities of the scales were conducted with SPSS Version 25.26 All other statistics were conducted with R.27
Descriptive Statistics
Descriptive statistics for the demographic variables are presented in Table 1. Descriptive statistics for each dependent measure at each time point are presented in Table 2.
Table 1.
Participant Demographic Characteristics by Group.
| Variables | Immediate group | Delayed group |
|---|---|---|
| (n = 58) | (n = 65) | |
| Mean (SD) | Mean (SD) | |
| Age | 43.75 (9.9) | 43.69 (10.65) |
| % (n) | % (n) | |
| Gender | ||
| Male | 3.45 (2) | 9.23 (6) |
| Female | 96.55 (56) | 90.77 (59) |
| Education | ||
| Less than high school | 0 (0) | 0 (0) |
| High school | 0 (0) | 32.31 (21) |
| Non-university certificate | 27.59 (16) | 30.77 (20) |
| Bachelor degree | 51.72 (30) | 29.23 (19) |
| Graduate degree | 20.69 (12) | 7.69 (5) |
| Marital status | ||
| Single | 7.01 (4) | 24.62 (16) |
| Married | 61.4 (35) | 55.38 (36) |
| Divorced or separated | 8.77 (5) | 3.08 (2) |
| Common law | 21.05 (12) | 16.92 (11) |
| Widowed | 1.75 (1) | 0 (0) |
Note. SD = standard deviation.
Table 2.
Descriptive Statistics for Dependent Measures From Baseline to 3-Month Follow-up.
| Time point | Immediate group (n = 44) | Delayed group (n = 40) |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Baseline | ||
| OMS-WA | 37.42 (9.29) | |
| Mental Health Coping Scale | 18.15 (3.2) | |
| Resiliency Scale | 16.15 (3.31) | |
| Preprogram | ||
| OMS-WA | 32.41 (6.28) | 39.16 (9.3) |
| Mental Health Coping Scale | 19.45 (2.23) | 18 (2.88) |
| Resiliency Scale | 16.78 (2.99) | 16.59 (2.95) |
| Postprogram | ||
| OMS- WA | 28.7 (6.41) | 34.7 (7.89) |
| Mental Health Coping Scale | 20.96 (1.91) | 19.84 (2.07) |
| Resiliency Scale | 17.93 (3.12) | 18.59 (3.13) |
| 3-Month follow-up | ||
| OMS-WA | 29.95 (6.13) | 34.15 (9.72) |
| Mental Health Coping Scale | 20.52 (2.44) | 19.35 (2.73) |
| Resiliency Scale | 18.05 (2.68) | 18.08 (2.89) |
Note. OMS-WA = Opening Minds Scale for Workplace Attitudes; SD = standard deviation.
Preliminary Analyses
Group differences in baseline characteristics (i.e., gender, education level, marital status) were investigated with chi-square analyses and analysis of variance, as appropriate. Independent sample t-tests were conducted on dependent variables (i.e., OMS-WA, mental health coping skills [MHCS], RS), using the data from presurvey. These analyses indicated that the immediate group and the delayed group were not statistically different in terms of gender, χ2(1) = 1.68, P = 0.19; marital status, χ2(4) = 9.06, P = 0.06; or age, F(1, 119) = .001, P = 0.98. However, there was a significant difference between groups in education level, χ2(3) = 26.48, P < 0.001, as the immediate group had a higher level of education than the delayed group.
Internal reliabilities of the scales were assessed by Cronbach αs, collapsed across all participants who provided data at each assessment point. The reliability of the OMS-WA was .89 across all time points (i.e., baseline, pretest, posttest, and follow-up). The Cronbach α coefficient for the Mental Health Coping Scale was moderate at .71 at baseline, .67 at pretest, .68 at posttest, and .71 at follow-up. Finally, the RS scale had a high level of internal consistency (.83 at baseline, .83 at pretest, .86 at posttest, and .81 at follow-up).
Analyses of Randomization and Clustering Effects
As noted above, a cluster-randomization procedure was strictly followed. It became apparent, however, that the randomization eventuated in the immediate delivery group to be comprised almost entirely of sites with administrative staff, whereas the delayed delivery group was comprised of mostly maintenance and kitchen staff. Also, as noted above, there were only 2 levels of clustering within each randomized group, which raised concerns about the ability to estimate clustering effects.28
Given the desire to test the effects of randomization and to evaluate the potential clustering effects, a 2 (group: immediate vs. delayed) by 2 (time point: time 1 vs. time 2) linear mixed model analysis with subject modeled as random effect and cluster modeled as fixed effect was conducted in R27 to examine changes in stigma, resiliency, and coping scores. Time 1 consisted of the baseline scores for the delayed group and pretest scores for the immediate group, whereas Time 2 consisted of the pretest scores for the delayed group and follow-up scores for the immediate group. These data were expected to demonstrate nonsignificant effects of clustering, but a significant interaction effect, revealing that the immediate intervention group demonstrated difference while the delayed intervention group revealed no changes during the waiting interval.
Stigma scores revealed a significant interaction effect, F(1/77) = 4.06, P = 0.047, and a significant group effect, F(1/76) = 25.70, P < 0.001. There were no significant main effects of time, F(1/77) = .92, P = 0.342, or cluster, F(1/76) = .04, P = 0.851. Follow-up pairwise comparison analyses revealed a significant Time 1 to Time 2 reduction in stigma for the immediate group, t(77) = 2.02, P = 0.031, but not the delayed group, t(77) = .72, P = 0.475.
Scores on RS revealed a significant time effect, F(1/74) = 5.68, P = 0.020. There were no significant main effects of group, F(1/74) = 2.26, P = 0.137, or cluster, F(1/74) = .03, P = 0.872. Although there was no significant interaction effect, F(1/74) = 1.23, P = 0.270, pairwise comparison analyses revealed the expected significant Time 1 to Time 2 improvement in RS for the immediate group, t(75) = 2.62, P = 0.011, but not the delayed group, t(77) = .85, P = 0.396.
Finally, scores on MHCS revealed a significant group effect, F(1/76) = 13.89, P < 0.001, and a significant time effect, F(1/77) = 6.55, P = 0.012. There was no significant main effect of cluster, F(1/76) = 2.38, P = 0.127. Although there were no significant interaction effect, F(1/77) = 1.38, P = 0.245, pairwise comparison analyses revealed a significant Time 1 to Time 2 improvement in MHCS for the immediate group, t(77) = 2.77, P = 0.007, but not the delayed group, t(77) = .94, P = 0.350.
Test of Primary Hypotheses
A 2 (groups: immediate vs. delayed) by 3 (time intervals: pretest, posttest, follow-up) linear mixed model analysis with subject modeled as random effect and cluster modeled as fixed effect was used to investigate program effects. A similar pattern of results was expected across stigma reduction (OMS-WA), improvement in MHCS, and improvement in RS, in that it program benefits were expected, which would maintain until the follow-up assessment period. Group differences were expected for stigma (see above), but no interactions were expected to emerge.
Changes in Stigma
Stigma scores on the OMS-WA revealed a significant time effect, F(2/154) = 16.33, P < 0.001 (see Figure 2). There was also a significant group effect, F(1/76) = 16.23, P < 0.001, but the interaction effect was not statistically significant, F(2/154) = 1.02, P = 0.362. Furthermore, the main effect of cluster was not statistically significant, F(1/76) = .02, P = 0.892. Based on hypotheses, pairwise comparison analyses revealed a significant pre- to postreduction in stigma for both the immediate, t(154) = 3.22, P = 0.004, and the delayed group, t(154) = 4.12, P < 0.001. Change from posttest to follow-up showed some increase for the immediate group, but this change was not statistically significant, t(154) = .85, P = 0.675. A similar pattern was observed in the delayed group, where the change was not significant, t(154) = .03, P = 0.999. Overall, stigma demonstrated a significant reduction from pre- to posttest, which was maintained to the time of the follow-up assessment.
Figure 2.
Stigma reduction over time (changes in total OMS-WA scale scores). OMS-WA = Opening Minds Scale for Workplace Attitudes.
Changes in RS
The analysis of the change in time on the RS scale showed a significant time effect, F(2/153) = 16.76, P < 0.001. However, neither the group effect, F(1/76) = .03, P = 0.875, nor the interaction effect, F(2/153) = .36, P = 0.698, was statistically significant. Furthermore, the main effect of cluster was not statistically significant, F(1/76) = .05, P = 0.825. Further examination of changes in time was performed. Follow-up pairwise comparison analysis revealed a significant pre- to posttest increase in RS for both the immediate group, t(153) = 3.6, P = 0.001, and the delayed group, t(153) = 4.27, P < 0.001. Some reduction in RS from posttest to follow-up was observed for both the immediate, t(153) = .52, P = 0.861, and the delayed group, t(153) = 1.46, P = 0.313, but this change was not statistically significant for either group. Overall, changes in RS were maintained from the posttest to the time of the follow-up test.
Changes in MHCS
Scores on MHCS revealed a significant time effect, F(2/154) = 13.94, P < 0.001, and a significant group effect, F(1/76) = 6.97, P = 0.01, but the interaction was not statistically significant, F(2/154) = .22, P = 0.800. Furthermore, the main effect of cluster was not statistically significant, F(1/76) = 1.44, P = 0.233. Further assessment of the time effect via pairwise comparison analyses revealed a significant pre- to posttest improvement in MHCS for the immediate group, t(154) = 3.35, P = 0.003, as well as for the delayed group, t(154) = 3.86, P < 0.001. Compared to the scores at posttest, follow-up scores reflected some decrease in the MHCS scores for both groups, but this change was not statistically significant for either the immediate, t(154) = .61, P = 0.816, or the delayed group, t(154) = 1.33, P = 0.380. The pattern demonstrated improvement in MHCS from pre- to posttest, which were sustained to the time of follow-up survey.
Additional Outcomes
At the follow-up assessment, participants were asked: “Have you used any of what you learned in the Working Mind Program at work or at home?” Fully 77.38% (n = 84) of participants indicated a positive response. The most common items included use of the Mental Health Continuum Model (18.37%) and to skills they learned in the program (16.33%). Providing empathy to another, being a support to another, having better understanding of mental health in the workplace, and introducing self-care activities to their lives were also commonly mentioned (12.24%, 12.24%, 10.2%, and 10.2%, respectively).
Program Effect Sizes
Program effect sizes were calculated, using the pretest and follow-up scores and with Cohen d 29 for comparison to other results.12 The effect size for stigma reduction, as indexed by the OMS-WA, was .49 in the immediate group, .52 in the delayed group, and .46 in the overall sample. The RS effect sizes were .49 and .66 in the immediate and delayed groups, respectively, and .57 in the entire sample. Finally, the effect size for the Mental Health Coping Scale was .58 in the immediate group and .62 in the delayed group, with an overall effect size of .58.
Discussion
In contrast to previous studies,12,23 this study included cluster randomization and a delayed control group in order to estimate the intervention’s efficacy. Sites were geographically distinct, and although the sites differed in some respects at baseline, the results revealed that the Working Mind program was effective at reducing stigmatizing attitudes toward mental illnesses and increasing perceived resiliency and coping skills. The delayed group did not change in terms of stigma, resilience, and MHCS while waiting for the program delivery. In addition, follow-up analyses demonstrated that the positive changes observed for stigma, resilience, and MHCS were retained over a 3-month interval.
Outcome effect sizes for both groups were moderate.26 This magnitude of effect is not unexpected, as it is unlikely that a 4-hour long intervention will produce changes with large effect sizes.30 The observed effect sizes of stigma reduction and resiliency improvement were somewhat larger than a previous meta-analysis, however, which reported an effect size of .38 for stigma reduction and .50 for resiliency improvement across 8 diverse workplace settings in Canada.12 Similarly, 6 different replications of the Understanding Stigma program found a mean effect size of .30 for stigma reduction.31
Study Strengths and Limitations
This study has several strengths, including the use of a control group, and validated outcome measures that enabled direct comparisons of effect sizes with previous research.12 The evaluation was conducted at a location removed from the actual workplace, which minimizes concerns about employee privacy and presentation biases. This study further benefited from quantitative measures and qualitative questions, the latter of which clearly demonstrated that a significant majority of participants utilized the program during the follow-up period.
A study limitation is that the cluster randomization yielded groups that were not equivalent at baseline. Cluster randomization works best when multiple groups are assigned to different conditions; it may have been superior in the current study to block groups on occupational categories first and then randomize to immediate versus delayed intervention. Further, the significant results that emerged were primarily in the context of the repeated assessments of participants over time and as a result of participation in The Working Mind program, which was a pattern of results that did benefit from randomization. A second study limitation was the moderate attrition at the presurvey time point in the delayed group and at the time of follow-up assessment in the immediate group. Some of this attrition may be due to participants who were not required to complete these evaluations. The follow-up attrition in the immediate group could also be due in part to the use of online questionnaires to collect the follow-up data. The use of different methods to collect some of the data (in person questionnaires vs. online) is a source of methodological variance in the data. Finally, the current study assessed the program effects at a 3-month follow-up period. Although this time interval matched previous research,12 future program evaluations should consider longer follow-up intervals.18
Summary and Directions for Future Research
The current study offers further evidence with for the efficacy of The Working Mind program to reduce workplace mental health stigma and increase resilience. The current results also reinforce previous outcomes with respect to the persistence of the program effects. These results add significantly to previous results about the benefits of the Working Mind program.12
The inclusion of more diverse workplace settings, other cultures, and target groups are potential targets for future study. Further, as this is the only randomized study of the Working Mind program, other randomized trials are recommended. If such trials employ cluster randomization, it would be ideal to have a large number of clusters to control for potential confounding variables. Another model of randomization would be to assign participants to either the current Working Mind program or an alternative intervention program to ascertain their relative benefits on program outcomes. Future work should utilize longer follow-up intervals and perhaps incentivize follow-up assessment participation. Future research could include other outcomes, such as disability claims or the use of mental health accommodations that may be affected indirectly by the intervention. Any program can also only represent a single tool in the range of possible workplace interventions.19 Further research of such programs in the context of larger organizational change11,32,33 will help to quantify their value for mental health promotion in the workplace.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The funds to support this project were provided by the Mental Health Commission of Canada in a grant awarded to the first author.
ORCID iDs: Keith S. Dobson  https://orcid.org/0000-0001-9542-0822
https://orcid.org/0000-0001-9542-0822
Veronika Markova  https://orcid.org/0000-0003-2357-9898
https://orcid.org/0000-0003-2357-9898
References
- 1. Dimoff JK, Kelloway EK. Bridging the gap: workplace mental health research in Canada. Can Psychol. 2013;54(4):203–212. [Google Scholar]
- 2. Bubonya M, Cobb-Clark DA, Wooden M. Mental health and productivity at work: does what you do matter? Labour Econ. 2017;46:150–165. [Google Scholar]
- 3. Honey A. The impact of mental illness on employment: consumers’ perspectives. Work. 2003;20(3):267–276. [PubMed] [Google Scholar]
- 4. Allan BA, Dexter C, Kinsey R, Parker S. Meaningful work and mental health: job satisfaction as a moderator. J Ment Health. 2016;27(1):38–44. [DOI] [PubMed] [Google Scholar]
- 5. Baba VV, Jamal M, Tourigny L. Work and mental health: a decade in Canadian research. Can Psychol. 1998;39(1-2):94–107. [Google Scholar]
- 6. Harvey SB, Modini M, Joyce S, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. 2017;74(4):301–310. [DOI] [PubMed] [Google Scholar]
- 7. Dewa CS, Chau N, Dermer S. Examining the comparative incidence and costs of physical and mental health-related disabilities in an employed population. Occup Environ Med. 2010;52(7):758–762. [DOI] [PubMed] [Google Scholar]
- 8. Lim KL, Jacobs P, Ohinmaa A, Schopflocher D, Dewa CS. A new population-based measure of the economic burden on mental illness in Canada. Chronic Dis Can. 2008;28(3):92–98. [PubMed] [Google Scholar]
- 9. Thornicroft G. Most people with mental illness are not treated. Lancet. 2007;370:807–808. [DOI] [PubMed] [Google Scholar]
- 10. Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help seeking, and public health programs. Am J Public Health. 2013;103(5):777–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Krupa T, Kirsh B, Cockburn L, Gewurtz R. Understanding the stigma of mental illness in employment. Work. 2009;33(4):413–425. [DOI] [PubMed] [Google Scholar]
- 12. Dobson KS, Szeto A, Knaak S. The working mind: a meta-analysis of a workplace mental health and stigma reduction program. Can J Psychiatry. 2019;64(1):39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Canadian Standards Association. National Standard of Canada for Psychological Health and Safety in the Workplace. Ottawa, Ontario: Canadian Standards Association; 2013. [Google Scholar]
- 14. Government of New Zealand. Health and Safety at Work. Wellington (NZ): Government of New Zealand; 2015. [Google Scholar]
- 15. Government of the United Kingdom. Equity Act. London, Queen’s Printer (England): Government of the United Kingdom; 2010. [Google Scholar]
- 16. Government of the United States. Americans with Disabilities Act. Washington (DC): Government of the United States; 2001. [Google Scholar]
- 17. Australian Government. Disability Discrimination Act; 1992. Canberra (Australia): Australian Government. [Google Scholar]
- 18. Pomaki G, Franche R, Murray E, Noushin K, Thomas ML. Workplace-based work disability prevention interventions for workers with common mental health conditions: a review of the literature. J Occup Rehabil. 2012;22(2):182–195. [DOI] [PubMed] [Google Scholar]
- 19. Szeto ACH, Dobson KS. Reducing the stigma of mental disorders at work: a review of current workplace anti-stigma intervention programs. App Prev Psychol. 2010;14:41–56. [Google Scholar]
- 20. Mental Health Commission of Canada. The Opening Minds Initiative; 2019. [Google Scholar]
- 21. Szeto ACH, Luong D, Dobson KS. Does labelling matter? An examination of attitudes and perceptions of labels for mental disorders. Soc Psychiatry Psychiatr Epidemiol. 2013;48(4):659–671. [DOI] [PubMed] [Google Scholar]
- 22. Szeto ACH, Adair M. Paramedicine and The R2MR—road to mental readiness. Can Paramedicine. 2016;39(1):18–21. [Google Scholar]
- 23. Szeto ACH, Dobson KS, Knaak S. The road to mental readiness for first responders: a meta-analysis of program outcomes. Can J Psychiatry. 2019;64(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Szeto ACH, O’Neill T, Dobson KS. The association between personality and individual differences and stigma toward people with mental disorders. Am J Psychiatr Rehabil. 2015;18(4):303–332. [Google Scholar]
- 25. Lane P. Handling drop-out in longitudinal clinical trials: a comparison of the LOCF and MMRM approaches. Pharm Stat. 2008;7(2):93–106. [DOI] [PubMed] [Google Scholar]
- 26. IBM Corp. IBM SPSS Statistics, Version 25.0. Released 2017. Armonk, New York: IBM Corp; 2017. [Google Scholar]
- 27. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 28. Gelman A, Hill J. Data Analysis using Regression and Multilevel/Hierarchical Models. Cambridge, Massachuesetts: Cambridge University Press; 2006. [Google Scholar]
- 29. Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159. [DOI] [PubMed] [Google Scholar]
- 30. Sagherian MJ, Huedo-Medina TB, Pellowski JA, Lisa AE, Blair TJ. Single-session behavioral interventions for sexual risk reduction: a meta-analysis. Ann Behav Med. 2016;50(6):920–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Knaak S, Szeto ACH, Kassam A, et al. Understanding stigma: a pooled analysis of a national program aimed at healthcare providers to reduce stigma towards patients with a mental illness. J Ment Health Addict Nurs. 2017;1(1):e19–e29. [Google Scholar]
- 32. Knaak S, Luong D, McLean R, Andrew S, Keith SD. Implementation, uptake, and cultural change: Results of a key informant study of a workplace mental health training in police organizations in Canada. Can J Psychiatry. 2019;64(6 Suppl):30S–38S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Janssens H, Clays E, De Clercq B, et al. Association between psychosocial characteristics of work and presenteeism: a cross-sectional study. Int J Occup Med Environ Health. 2016;29(2):331–344. [DOI] [PubMed] [Google Scholar]