In recent years, e-cigarette use (or “vaping”) has emerged as a smoking alternative. Vaporizers can contain ingredients ranging from solvents and flavoring to drugs such as nicotine and cannabinoids. In Canada, addition of nicotine to e-cigarettes was approved in 2018, and the addition of cannabis oils became legally regulated in 2019. However, both nicotine and cannabis vaping products were widely available before these dates.
Vaping has generally been viewed as a harm-reduction strategy due to the well-known adverse effects of smoking combustible tobacco. E-cigarettes are widely used for smoking cessation and relapse prevention. In this letter, we report the emergence of an additional phenomenon: vaping as a de novo substance use pattern.
The data sources for this study included the 2017 Canadian Tobacco, Alcohol and Drugs Survey (CTADS, n = 8,614)2 and the 2019 Canadian Tobacco and Nicotine Survey (CTNS, n = 16,349).3 The CTADS used an invitation letter to contact sampled households. The letter provided information for accessing an online questionnaire. This was followed by telephone contact if there was no response. The CTNS collected data either by online questionnaire or by computer-assisted telephone interview. Both surveys targeted noninstitutionalized adults (age > 15) living in the 10 provinces. Each data set includes a set of 500 replicate weights developed by Statistics Canada using a bootstrap procedure. This allows investigators to conduct analyses that account for methodological features of the surveys and to adjust for nonresponse.
Each survey asked participants whether they had used e-cigarettes in the past 30 days. In 2017, 2.9% (95% CI, 2.3 to 3.5) reported past 30 day use, whereas the 2019 estimate was 4.7% (95% CI, 4.2 to 5.3). While direct comparisons cannot be made, the data suggest an increase in use and help to quantify the extent of change, previously described as an “explosion.”1 Both surveys described an expected pattern of use. E-cigarette users were more likely to be male and were younger than nonusers. Also, e-cigarette users more often reported binge drinking, cannabis use, and use of other drugs. A detailed descriptive analysis of CTNS findings is available from Statistics Canada.4
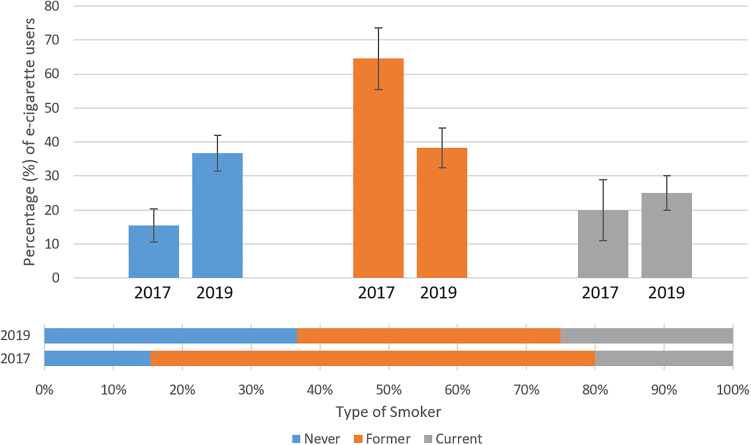
A sizable proportion of e-cigarette users in both surveys reported being current smokers or former smokers, consistent with harm-reduction or smoking cessation goals. For example, in 2017, 64.5% (95% CI, 55. 5 to 73.6) of e-cigarette users reported current smoking, compared to 13.5% (95% CI, 12.1 to 15.0) of nonusers. In 2017, 15.5% of e-cigarette users reported that they had never smoked, suggesting a de novo pattern of substance use. By 2019, this proportion had more than doubled to 36.7%. The percentage of e-cigarette users who were current, former, or never-smokers is depicted in Figure 1. The observed changes suggest that e-cigarette use can no longer be regarded exclusively as a smoking cessation or harm-reduction strategy. Rather, in 2019, e-cigarette users were equally as likely to be never smokers or current smokers, whereas a smaller proportion consists of former smokers.
Figure 1.
Smoking status among individuals with past 30-day e-cigarette use, by survey year. Note. Error bars are 95% confidence intervals. Estimates reported in the vertical and horizontal bars are the same, depicted in different ways to provide a complementary visual impression of the mix of smoking types (horizontal) and associated precision (vertical).
The reasons for these trends cannot be fully clarified by survey data. However, the 2017 survey included items asking about reasons for use. Respondents could select more than 1 reason. The most common reason was “curiosity”: 65.7% (95% CI, 52.1 to 79.3), but a large proportion of respondents reported a belief that e-cigarettes were less harmful than conventional cigarettes, both to themselves (46.9%; 95%CI, 32.4 to 61.4) and others (45.5%; 95% CI, 33.0 to 62.1). The next most common reasons were that e-cigarettes were viewed as being “more acceptable to nontobacco users” (42.7%; 95% CI, 27.0 to 58.1) and that they contained “flavors I like” (40.8%; 95% CI, 25.0 to 56.5).
As the harms associated with e-cigarette use are not fully understood,1 the implications of these findings for population health are uncertain. As e-cigarette use emerges as a new pattern of substance use, the prevalence of e-cigarette-associated substance use disorders, either involving nicotine or cannabis, requires ascertainment. Research may also be required to determine whether conventional treatments for smoking cessation and cannabis use disorders are effective for cessation in this growing population and whether cessation of vaping leads to better mental health outcomes.5
Limitations of this study include methodological features of the CTADS and CTNS surveys and the differences between them. In addition to general cautions about the accuracy of self-reported responses and representativeness of the samples, methodological differences necessitate additional caution when interpreting differences between the 2 surveys. These surveys use different approaches to sampling, different modes of data collection, and there are differences in the wording of some questions. As such, the results are vulnerable to selection or measurement biases. These surveys provide high-level epidemiologic data and do not address questions such as the frequency or dosages of drug exposures or whether a substance use disorder is present. For example, past month use may in some cases represent experimentation rather than a more problematic pattern of use.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by Cuthbertson & Fischer Chair in Pediatric Mental Health and the University of Calgary.
ORCID iD: Scott B. Patten, MD, PhD  https://orcid.org/0000-0001-9871-4041
https://orcid.org/0000-0001-9871-4041
Kathryn Wiens, MSc, PhD Candidate  https://orcid.org/0000-0003-3451-6788
https://orcid.org/0000-0003-3451-6788
Aysha Lukmanji, BA&Sc  https://orcid.org/0000-0002-7033-2612
https://orcid.org/0000-0002-7033-2612
Rudra Dahal, BSc, Med  https://orcid.org/0000-0001-7911-0779
https://orcid.org/0000-0001-7911-0779
Andrew G. M. Bulloch, PhD  https://orcid.org/0000-0003-3305-7874
https://orcid.org/0000-0003-3305-7874
References
- 1. Cao DJ, Aldy K, Hsu S, et al. Review of health consequences of electronic cigarettes and the outbreak of electronic cigarette, or vaping, product use-associated lung injury. J Med Toxicol. 2020;16(3):295–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Statistics Canada. Canadian Tobacco, Alcohol and Drugs Survey (CTADS): summary of results for 2017 Ottawa: Statistics Canada; 2019. [updated 2019 Jan 4]. [accessed 2020 Jul 15]. https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2017-summary.html.
- 3. Statistics Canada. Canadian Tobacco and Nicotine Survey (CTNS). 2020. [updated 2020 Feb 14]. [accessed 2020 Jul 15]. https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&Id=1251796
- 4. Statistics Canada. Canadian Tobacco and Nicotine Survey (CTNS): summary of results for 2019. 2020. [updated 2020 Jul 8]. [accessed 2020 Jul 15].
- 5. Dahal R, Adhikari K, Patten SB. Smoking cessation and improvement in mental health outcomes: do people who quit smoking by switching to electronic cigarettes experience improvement in mental health? Can J Psychiatry. 2020;65(7):512–514. [DOI] [PMC free article] [PubMed] [Google Scholar]