Abstract
Aim
We investigated the optimum time and number of observations for assessing women in the Day Assessment Unit.
Methods
A single centre prospective observational study was undertaken. Women referred for blood pressure assessment in the Day Assessment Unit were recruited.
Results
The blood pressure of women who subsequently developed preeclampsia was noted to change differently over the time of observation compared to women with other hypertensive disorders, most notably in the first and third hour (p = 0.042), although the averages at each hour did not differ between these two groups.
Conclusions
Mean blood pressure measured over four hours did not significantly differ compared to blood pressure measured over one hour. Women who subsequently developed preeclampsia had a different pattern of blood pressure change whilst in the Day Assessment Unit.
Keywords: Pre-eclampsia, gestational hypertension, blood pressure assessment
Introduction
According to World Health Organization (WHO), preeclampsia remains one of the leading preventable causes of maternal mortality.1 Preeclampsia affects as many as 10 million women, and 76,000 women die from preeclampsia and related disorders worldwide per year.2
Preeclampsia is one of the most common reasons for admission to hospital during pregnancy.3 It is a significant economic and social burden on the health care system and also for the woman.4,5
Day care assessment units offer an alternative to inpatient evaluation. Compared to inpatient stay, Day Assessment Units (DAUs) are cost effective for assessing hypertension and an acceptable modality for women.6,7 Women with hypertensive disorders of pregnancy (HDP) may require several visits to DAU. Four-hour visits are time consuming for women and also add to staffing costs.
Although, there are clear-cut definitions regarding blood pressure (BP) and criteria that would constitute preeclampsia, the literature regarding the optimal frequency of blood measurements in women being assessed in DAU is limited. PreCog guidelines8 recommend measuring BP 10 min apart. However, due to the limited literature, different hospitals have different protocols as to what constitutes effective assessment.9 Shennan et al. assessed BP measurements every 15 min versus a single reading at 90 min with an automated machine and found that mean systolic blood pressure (SBP) dropped over 90 min compared with the first reading; however, the same effect was not noted for the diastolic blood pressure (DBP). The mean of all single readings were similar for both the SBP and DBP, over a period of 90 min.10
This study was carried out to test the hypothesis that BP assessment after the first hour does not significantly differ to the BP after four hours of assessment.
Materials and methods
This study was a prospective observational study undertaken in a tertiary metropolitan hospital accounting for approximately 13,000 deliveries annually (Liverpool Hospital, New South Wales).
The DAU of Liverpool Hospital is staffed by senior midwives who are responsible for the initial assessment of women referred for the evaluation of their BP. Referrers include general practitioners, obstetric consultants or registrars and renal physicians. Hypertension was defined according to SOMANZ criteria (11) as a SBP greater than or equal to 140 mmHg and/or diastolic BP greater than or equal to 90 mmHg.11 Women referred to DAU had been found to be hypertensive (BP reading greater than or equal to 140/90 mmHg). This may have been as a one-off in clinic or with a general practitioner. Potentially, it was a sustained elevation elsewhere and women were sent for further assessment, e.g. white coat hypertension or preeclampsia. No woman who had normal BP was referred to the DAU for an assessment.
Pregnant women over the age of 18, not in labour, diagnosed with hypertension (classified or unclassified) who were referred to DAU for assessment of their BP were recruited after providing informed consent. A formal diagnosis of hypertension need not have been made at the time of inclusion to the study. Only a woman’s first DAU assessment was included for analysis. Women were excluded if they were unable to give consent, under the age of 18, had a karyotypically/morphologically abnormal fetus or already had been diagnosed with preeclampsia. Women were referred to DAU only after 20 weeks of gestation. This study was approved by the SWSLHD Research and Ethics Committee.
After arriving in the DAU and resting for 10 min, women had their BP assessed every 15 min for the first hour and half hourly thereafter for a total assessment of four hours. The BP was averaged at one hour, two hours, three hours and four hours for the purpose of analysis. Women had routine blood and urine tests performed as per routine DAU assessment. The blood tests included electrolytes, urea, creatinine, full blood count, liver function tests and uric acid, and a spot urine was assessed for the protein: creatinine ratio and culture if indicated.
Measurement of BP was recorded as per SOMANZ guidelines.11 BP was measured with the woman comfortable and her legs resting on a flat surface. The SBP was assessed as Korotkoff sound 1 and diastolic BP at Korotkoff sound 5. A larger cuff, covering 80% of the arm circumference was used when the upper arm circumference was greater than 33 cm. Demographic data were recorded (including race (self-reported), age and parity). Clinical data recorded included gestation at booking, booking SBP and DBP, booking weight, height, smoking status, pre-existing medical history, history of hypertension in previous pregnancies, presence of other antenatal complications, e.g. gestational diabetes. The outcome of the pregnancy was collected after delivery and the final hypertensive disease of pregnancy diagnosis was ascertained. Delivery details included the mode of delivery, gestational age, gender and weight of the baby.
Statistics
BP was analysed using SPSS v23.0 (USA). Analysis was undertaken using paired-wise comparisons with Bonferroni correction for multiple comparisons. Where differences between diagnostic groups were assessed, a general linear model (GLM) analysis of repeated measures was undertaken with post hoc testing between groups adjusted for multiple comparisons. Results were considered statistically significant if the p-value was less than 0.05. Data are expressed as the mean ± standard error of the mean (SEM). Allowing for a Type 1 error of 5% (two-sided t-test) and given 90% power, and a within group standard deviation of 9.5 mmHg (based on published data) and a difference between the two groups of 5 mmHg (chosen as this would be clinically significant difference), a total of 40 women were required.
Results
Forty women were recruited in the study carried out between November 2009 and April 2010. Of the 40 women recruited, most were Caucasian (n = 31, 78%), with an average body mass index of 28.7 ± 6.5 and age of 28.9 (±6.1) years. Primigravidas constituted 48% of women and 42% (n = 17) of women had a pre-existing hypertensive disorder diagnosed prior to attending the DAU (Table 1). Of the women referred to DAU, 77.5% went on to develop hypertensive disease of pregnancy. Of those women, 50% developed preeclampsia, 27.5% developed gestational hypertension. Among the women referred, 6.4% of the women had pre-existing hypertension and went on to develop superimposed hypertensive disease of pregnancy. If the women were monitored only for one hour, 62.5% would have a diagnosis of hypertensive disease of pregnancy.
Table 1.
Baseline demographics of the women included.
| Parameter | Result (n = 40) |
|---|---|
| Maternal age (yrs) | 28.9 ± 1.0 |
| BMI (kg/m2) | 28.7 ± 1.1 |
| Gestation (weeks) | 33.5 ± 0.6 |
| Parity | |
| Primigravid | 19 (48%) |
| Multigravid | 21 (52%) |
| Ethinicity | |
| Caucasian | 31 (77.5%) |
| Asian | 5 (12.5%) |
| Other | 4 (10%) |
| Smoking (cigarettess/day) | |
| 0 | 36 (90%) |
| 1–4 | 1 (2.5%) |
| >5 | 3 (7.5%) |
| Gestational diabetes | 5 (12.5%) |
| Hypertension in previous pregnancy | 9 (22.5%) |
| Pre-pregnancy hypertension | 17 (42%) |
| Comorbid medical disorders (e.g. renal disease, thyroid disease) | 5 (12.5%) |
Note: Data are number of woman (%) or mean ± standard error of the mean.
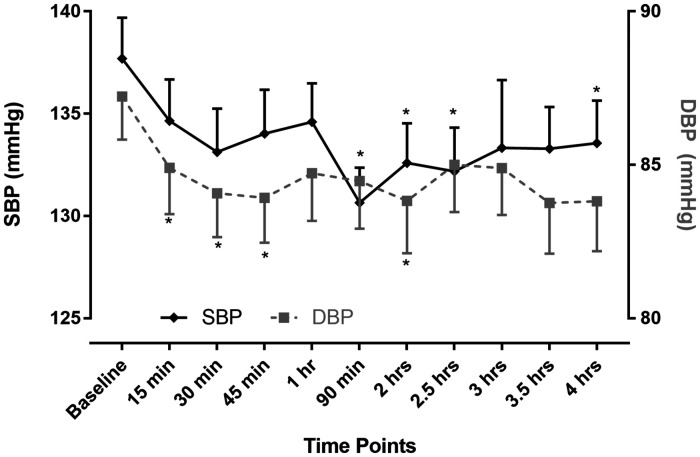
The SBP significantly changed over time (GLM; SBP p = 0.01). The DBP did not significantly change over time (GLM; DBP p = 0.23). The SBP was significantly lower only after 90 min of observations compared to baseline only. The DBP was only significantly lower compared to baseline within the first hour and was not different compared to baseline subsequently (Table 2, Figure 1).
Table 2.
Mean SBP and DBP at all time points measured.
| Time of measurement | SBP ± SEM | DBP ± SEM | Compared to baseline, p-value |
|---|---|---|---|
| Baseline | 137.7 ± 2.0 | 87.2 ± 1.4 | |
| 15 min | 134.7 ± 2.0 | 84.9 ± 1.5* | 0.4/0.04 |
| 30 min | 133.1 ± 2.1 | 84.1 ± 1.4* | 0.1/0.016 |
| 45 min | 134.0 ± 2.2 | 83.9 ± 1.5* | 0.2/0.007 |
| 1 h | 134.6 ± 1.9 | 84.7 ± 1.5 | 0.3/0.4 |
| 90 min | 130.7 ± 1.7* | 84.5 ± 1.6 | <0.001/0.1 |
| 2 h | 132.6 ± 1.9* | 83.8 ± 1.7* | <0.001/0.002 |
| 2.5 h | 132.2 ± 2.1* | 85.0 ± 1.5 | 0.006/0.9 |
| 3 h | 133.3 ± 3.3 | 84.9 ± 1.5 | 0.9/0.9 |
| 3.5 h | 133.2 ± 2.0 | 83.7 ± 1.7 | 0.06/0.3 |
| 4 h | 133.6 ± 2.1* | 83.9 ± 1.6 | 0.04/0.1 |
SBP: systolic blood pressure; DBP: diastolic blood pressure; SEM: standard error of the mean.
*p < 0.05 compared to baseline measurement.
Figure 1.
Mean SBP and DBP ± SEM at each time point assessed in the Day Assessment Unit. SBP: systolic blood pressure; DBP: diastolic blood pressure. *p < 0.05 compared to baseline measurement.
When comparing the average BPs at 1, 2, 3 and 4 h, there was a significant change over time in the SBP and no difference in the DBP if the baseline BP was included in the calculations (GLM; SBP and DBP p = 0.038 and p = 0.7). If the baseline BP was excluded, there was no difference in SBP or DBP averages over time (GLM; SBP and DBP p = 0.2 and p = 0.7).
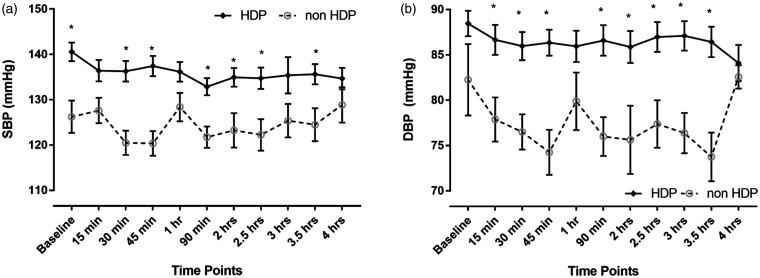
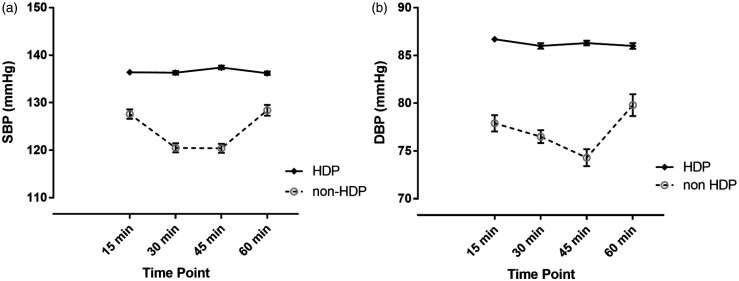
It is expected that the average BPs of women in subsequently different diagnostic groups is different. For example, women who subsequently develop a new diagnosis of a hypertensive disorder of pregnancy (preeclampsia or gestational hypertension) have a higher BP during the DAU assessment compared to those not subsequently diagnosed with a new HDP (GLM; SBP p = 0.005 and DBP p = 0.007, respectively) (Figure 2(a) and (b)) However, the SBP (p = 0.01) but not the DBP (p = 0.11) of women who subsequently developed HDP behaved differently over the first hour observation period compared to women who did not develop HDP. The women who did not develop a HDP had a drop in BP during the first hour that was not seen in women who would develop an HDP (Figure 3).
Figure 2.
The HDP (preeclampsia and gestational hypertension) and non-HDP mean (a) SBP and (b) DBP ± SEM at each time point assessed in the Day Assessment Unit. SBP: systolic blood pressure; DBP: diastolic blood pressure; HDP: hypertensive disorders of pregnancy. *p < 0.05 comparing HDP and non-HDP measurement at the time point indicated.
Figure 3.
The HDP (preeclampsia and gestational hypertension) and non-HDP mean (a) SBP and (b) DBP ± SEM during the first hour excluding baseline measurements. SBP: systolic blood pressure; DBP: diastolic blood pressure; min: minutes; HDP: hypertensive disorders of pregnancy.
Discussion
DAU is a well-established model of antenatal care, increasingly being used to reduce inpatient stay and costs associated with the same.7,9 The results of our study show that mean BP over one hour does not significantly differ to the BP over 4 h of assessment. Women who are referred to DAU also prefer this to an inpatient stay due to closer monitoring and attention that they receive in day care units.7
Assessing women for hypertension is one of the major reasons for a woman to be referred to DAU. The current definitions for hypertensive disorders in pregnancy are based on clinical readings and in recent times, there is considerable debate on using the conventional clinic derived BP to diagnose hypertensive disorders in pregnancy.12,13 Home BP monitoring offers an attractive option, especially in assessment of women with white coat hypertension. However, the limited availability of calibrated and validated machines limits the use of self-measurement of BP at home.14,15
Although there are a number of studies evaluating the importance and suitability of DAU for assessing BP, there is limited evidence regarding the optimum time for monitoring of the BP.6,7,9,16 A satisfaction survey by Dunlop et al. found that waiting in DAU for long periods (test results and review by medical officer) was viewed negatively by the women. Organising child care and visits to the hospital during peak hours was considered cumbersome.
Given that DAU’s function as a screening point, it is particularly important that evidence-based medicine is practised to optimise the use of DAU. BPs averaged at the end of each hour do not differ significantly when the initial BP was excluded. While averaging the BP, the first reading taken at DAU was invariably high for all group of women (HDP and non-HDP), consistent with other studies.10,17 Hence, we recommend discarding the initial value when the BP is being assessed. Our study demonstrates that waiting four hours for BP assessment is not required, but that pattern of change of the BP in the first hour may be important as well as the averages and the raw readings at each time point.
One of the limitations of our study was the relatively small number of cases. However, the findings of our study are significant in adding to the cost effectiveness, clinical and psychosocial effects of care in a DAU.
Conclusion
Women who are currently observed for four hours in the DAU could have this time period reduced as the BPs do not change substantially over time. However, the pattern of change may indicate a greater risk of preeclampsia later in the pregnancy. Given our small study population, we recommend the study to be carried out in multiple centres with diverse population to ensure generalizability.
Acknowledgements
This study was presented as a poster in PSANZ Conference, Canberra – 2017. We would like to thank the DAU midwives and patients for their help in the research.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: The ethics committee of the South Western Sydney Local Health District approved this study.
Guarantor: VK.
Contributorship: VK and AM were involved in data analysis and researched the literature. AM, BH and AH conceived the study. AM was involved in protocol development and gaining ethical approval. GL was involved in patient recruitment. VK wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
ORCID iD: Vidhu Krishnan https://orcid.org/0000-0001-7044-2654
References
- 1.WHO. WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia, www.who.int/reproductivehealth/publications/maternal_perinatal_health/9789241548335/en/ (accessed 3 October 2019). [PubMed]
- 2.Kuklina EV, Ayala C, Callaghan WM. Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol 2009; 113: 1299–1306. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg K, Sara T. Screening and surveillance of pregnancy hypertension—an economic approach to the use of daycare. Baillieres Clin Obstet Gynaecol 1990; 4: 89–107. [DOI] [PubMed] [Google Scholar]
- 4.Osungbade KO, Ige OK. Public health perspectives of preeclampsia in developing countries: implication for health system strengthening. J Pregnancy 2011; 2011: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Institute for Health and Care excellence. Hypertension in pregnancy: diagnosis and management. NICE guideline (NG133), www.nice.org.uk/guidance/ng133 (accessed 3 October 2019). [PubMed]
- 6.Dowswell T, Middleton P, Weeks A. Antenatal day care units versus hospital admission for women with complicated pregnancy. Cochrane Database Syst Rev 2009; 4: Cd001803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dunlop LUmstad M, McGrath G, , et al. Cost-effectiveness and patient satisfaction with pregnancy day care for hypertensive disorders of pregnancy. Aust N Z J Obstet Gynaecol 2003; 43: 207–212. [DOI] [PubMed] [Google Scholar]
- 8.Milne FRedman C, Walker J, , et al. Assessing the onset of pre-eclampsia in the hospital day unit: summary of the pre-eclampsia guideline (PRECOG II). BMJ 2009; 339: b3129. [DOI] [PubMed] [Google Scholar]
- 9.Saleh MM, Selinger M. Evaluation of the role of day assessment unit in the management of pregnancy induced hypertension. J Obstet Gynaecol 2005; 25: 651–655. [DOI] [PubMed] [Google Scholar]
- 10.Wilton A, Greef AD, Shennan A. Rapid assessment of blood pressure in the obstetric day unit using Microlife MaM technology. Hypertens Pregnancy 2007; 26: 31–37. [DOI] [PubMed] [Google Scholar]
- 11.Lowe SABowyer L, Lust K, , et al. The SOMANZ Guidelines for the Management of Hypertensive Disorders of Pregnancy 2014. Aust N Z J Obstet Gynaecol 2015; 55: 11–16. [DOI] [PubMed] [Google Scholar]
- 12.Shennan AH, Halligan AW. Measuring blood pressure in normal and hypertensive pregnancy. Baillieres Best Pract Res Clin Obstet Gynaecol 1999; 13: 1–26. [DOI] [PubMed] [Google Scholar]
- 13.Bergel E, Carroli G, Althabe F. Ambulatory versus conventional methods for monitoring blood pressure during pregnancy. Cochrane Database Syst Rev 2002; 2: Cd001231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bardak STurgutalp K, Ozcan T, , et al. How do we measure blood pressure at home? Blood Pressure 2015; 24: 174–177. [DOI] [PubMed] [Google Scholar]
- 15.Persu AFagrd R, De Cort P, , et al. The good use of home blood pressure monitoring. Consensus document. J de Pharmacie de Belgique 2009; ▪: 33–36. [PubMed] [Google Scholar]
- 16.Turnbull DAWilkinson c, Gerard K, , et al. Clinical, psychosocial, and economic effects of antenatal day care for three medical complications of pregnancy: a randomised controlled trial of 395 women. Lancet 2004; 363: 1104–1109. [DOI] [PubMed] [Google Scholar]
- 17.Magee LAVon Dadelszen P, Singer J, , et al. The CHIPS randomized controlled trial (control of hypertension in pregnancy study): is severe hypertension just an elevated blood pressure? Hypertension 2016; 68: 1153–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Magee LAPelsa, Helewa M, , et al. The hypertensive disorders of pregnancy (29.3). Best Pract Res Clin Obstet Gynaecol 2015; 29: 643–657. [DOI] [PubMed] [Google Scholar]
- 19.Penny JAShennan AH, Halligan AW, , et al. Blood pressure measurement in severe pre-eclampsia. Lancet 1997; 349: 1518. [DOI] [PubMed] [Google Scholar]
- 20.Harlow FH, Brown MA. The diversity of diagnoses of preeclampsia. Hypertens Pregnancy 2001; 20: 57–67. [DOI] [PubMed] [Google Scholar]
- 21.Cnossen JSVollebregt KC, De Vrieze N, , et al. Accuracy of mean arterial pressure and blood pressure measurements in predicting pre-eclampsia: systematic review and meta-analysis. BMJ 2008; 336: 1117–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halligan AWShennan AH, Lambert Paul, , et al. Automated blood pressure measurement as a predictor of proteinuric pre-eclampsia. BJOG 1997; 104: 559–562. [DOI] [PubMed] [Google Scholar]
- 23.Gupta MShennan AH, Taylor DJ, , et al. Accuracy of oscillometric blood pressure monitoring in pregnancy and pre-eclampsia. BJOG 1997; 104: 350–355. [DOI] [PubMed] [Google Scholar]
- 24.Rezk M, Gamal A, Emara M. Maternal and fetal outcome in de novo preeclampsia in comparison to superimposed preeclampsia: a two-year observational study. Hypertens Pregnancy 2015; 34: 137–144. [DOI] [PubMed] [Google Scholar]