Abstract
Study Design:
A retrospective cohort study.
Objective:
The world was unprecedentedly struck by the new coronavirus in December 2019. Consequently, lockdown measures were imposed by many governments. Health-care services were reserved for emergencies and malignancies. Nevertheless, many patients who urgently needed these services did not present. This study estimates the impact of COVID-19 and lockdown measures on the patients’ flow in the outpatient clinic (OPC) and the operations for laryngeal and/or oropharyngeal neoplasms.
Methods:
This study is a retrospective cohort study performed in otolaryngology department of a tertiary care hospital which is a major referral center. All patients who attended the OPC and all operations performed for laryngeal and/or oropharyngeal neoplasms were counted from February 1, 2020 to May 31, 2020 and compared with the previous year as a reference.
Results:
In 2020, the number of patients attending the otolaryngology OPC and the laryngeal and/or oropharyngeal surgeries showed a major drop, especially after imposing the lockdown measures. The total number of these operations in April and May 2019 dropped by 79% for the same period in 2020.
Conclusion:
An estimate of 79% of patients, who had been presenting for laryngeal and/or oropharyngeal neoplasms, did not show up due to indirect COVID-19 effect.
Keywords: impact of COVID, COVID and cancer, lockdown and cancer, impact of lockdown
Introduction
By the end of December 2019, the world was unprecedentedly struck by coronavirus SARS-2 which was diagnosed in China. On January 30, 2020, the World Health Organization (WHO) announced a Public Health Emergency and later the virus was named COVID-19. On March 11, 2020, the disease was declared as a pandemic.1
Consequently, lockdown measures were imposed by many governments including closing shops, travel restrictions, canceling events, and social distancing became crucial. Health-care services were directed toward emergencies. Yet, some drawbacks arose which were indirectly related to COVID-19 such as slowing of research process and canceling of conferences.2 In some places, cancer patients faced major curbs for getting the health service or the chemotherapy.3
It is worth mentioning that head and neck cancers are common and has a higher mortality rate in the developing countries.4 This study highlighted the indirect impact of COVID-19 on patients with laryngeal and/or oropharyngeal neoplasms.
Patients and Methods
This study is a retrospective cohort study performed in Ear, Nose and Throat (ENT) Department of a tertiary care hospital which provides tertiary care for a city, with almost 21 million population, in addition to referrals from other cities of the country. Institutional approval was obtained.
Based on the WHO announcement of COVID-19 as a Public Health Emergency of International Concern (PHEIC) on the 30th January 2020, all patients who attended the ENT outpatient clinic (OPC), from the 1st of February 2020 to the 31st of May 2020, were counted from the OPC’s documents. All operations performed for laryngeal and/or oropharyngeal neoplasms, whether diagnostic or therapeutic, were counted and retrieved from the operative theater’s documents for the same period.
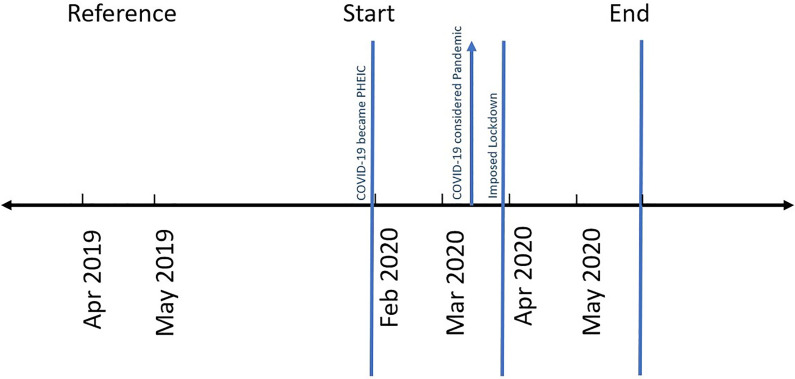
After the WHO declaration of COVID-19 as a pandemic in the middle of March 2020 and starting of lockdown measures in the country by its end, the change in the number of patients attending the OPC and those involved in the surgeries was noted for 2 months after. Moreover, comparison between the surgeries for laryngeal and/or oropharyngeal neoplasms was done between April–May 2020 and April–May 2019 as a reference for the same period in the previous year to rule out any seasonal variations (Figure 1).
Figure 1.
Timeline of the study. PHEIC indicates Public Health Emergency of International Concern.
Statistical Methods
Data were coded and entered using the Statistical Package for the Social Sciences (SPSS) version 25. Data were summarized using frequencies (number of cases) and relative frequencies (percentages).
Results
Starting from February 2020 until the end of May 2020, 9472 patients visited the ENT OPC and 182 patients were subjected to laryngeal and/or oropharyngeal neoplasm surgeries.
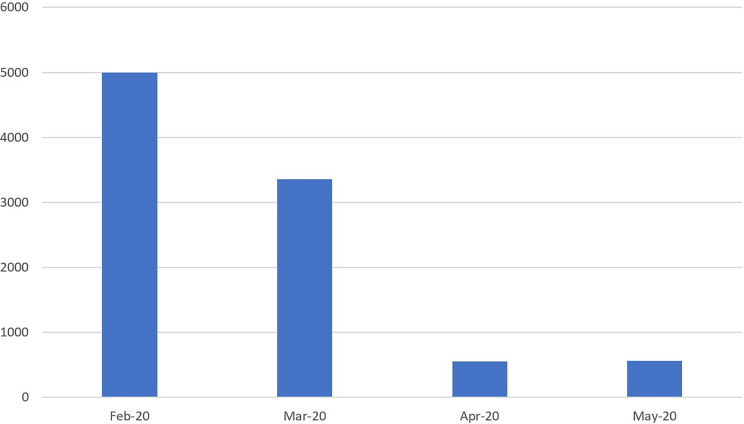
In 2020, the number of patients attending the ENT OPC in February was 4993 which dropped by 33% in March to 3357. Eighty-three percent plummet was observed in April where the numbers reached 556. A slight rise by 2% was detected in May to reach 566. The total reduction in the numbers was 4427 (89%) (Table 1 and Figure 2).
Table 1.
Count and Percentage Change of Patients Attending the ENT OPC and the Laryngeal and/or Oropharyngeal Operations During 2020.
| Month | Number of patients attending OPC (% change) | Number of performed operations (% change) |
|---|---|---|
| February | 4993 | 83 |
| March | 3357 (−33) | 72 (−13) |
| April | 556 (−83) | 17 (−76) |
| May | 566 (2) | 10 (−41) |
| Total | 9472 (−89) | 182 (−88) |
Abbreviations: ENT, Ear, Nose and Throat; OPC, outpatient clinic.
Figure 2.
Bar chart showing the count of patients attending the outpatient clinic.
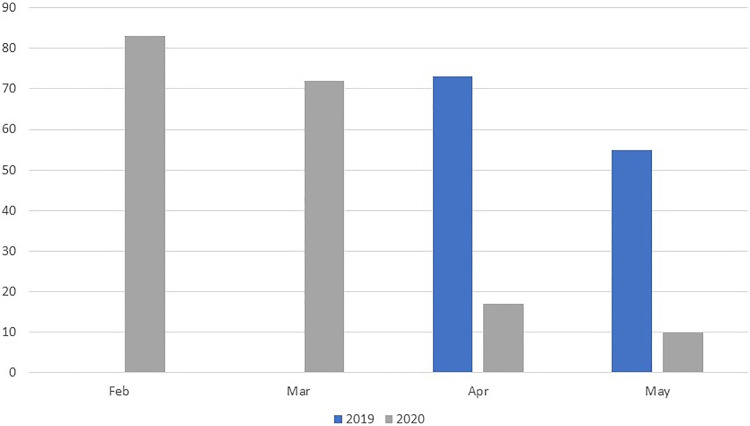
Regarding the number of laryngeal and/or oropharyngeal neoplasm surgeries performed in 2020, 83 operations’ count in February dropped to 72 in March with 13% reduction. Seventy-six percent plunge was noted in April when the numbers reached 17. Additional 41% drop in May led the numbers down to 10. The total reduction in the operations’ count was 73 (88%) (Table 1 and Figure 3).
Figure 3.
Bar chart showing the number of laryngeal and/or oropharyngeal neoplasm operations.
In 2019, the numbers of operations performed for laryngeal and/or oropharyngeal neoplasm surgeries were 73 and 55 for April and May, respectively. The details of the operations’ types were shown and used as a reference to the same months in 2020 (Table 2). The total number of laryngeal and/or oropharyngeal neoplasm operations in April and May 2019 was 128 which dropped by 79% to 27 for the same period in 2020.
Table 2.
Types of the Operations Performed, in April and May, in 2019 and 2020.
| 2019 | 2020 | |||
|---|---|---|---|---|
| Operation | April | May | April | May |
| Laryngectomy (total and partial) | 15 | 7 | 3 | 1 |
| Direct laryngoscopy (diagnostic and therapeutic) | 45 | 34 | 1 | 5 |
| Tracheostomy | 8 | 12 | 12 | 3 |
| Laser | 3 | 0 | 1 | 0 |
| Oropharyngeal | 2 | 2 | 0 | 1 |
| Total number | 73 | 55 | 17 | 10 |
| 128 | 27 | |||
Discussion
Coronaviruses are known to cause respiratory tract infections. Several outbreaks were encountered in the past which menaced the public health such as Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). Recently, COVID-19 has been discovered by the end of December 2019. The method of person-to-person transmission could be through droplet such as coughing and sneezing or contact.5 Public gatherings were a potential way of spread. Thus, social distancing was advised by many governments.6 Moreover, lockdown measures were imposed by many countries. For instance, lockdown measures in Wuhan included travel restrictions, home quarantine, stopping public events and gatherings, closing of schools and universities. Many European countries followed similar measures later.7
In the authors’ country, partial lockdown was imposed by the government on the 24th of March 2020 which included night curfew, shorter shops’ operating times as well as total closure of restaurants, coffee shops, schools, universities, and governmental offices. The health services were only reserved for emergency and neoplastic cases with deferral of all other elective services.
The authors’ hospital used to provide services for vast number of cases. The ENT OPC, which was the main doorway for operations, received 4993 cases in February 2020 which dropped by 33% in March. Although the lockdown measures did not discourage patients who had emergency or neoplasms from seeking medical advice, numbers plummeted in April by 83% to reach 556 cases. It was understandable that elective cases deferred from presentation. However, it was incomprehensible why the patients’ count, who had laryngeal/oropharyngeal neoplasms, decreased which was subsequently detected by the reduction of the number of the diagnostic/therapeutic operations performed for them.
In this study, the authors measured the magnitude of the crisis on laryngeal/oropharyngeal neoplasm surgeries because the authors’ hospital is a major referral center, which frequently manages these cases. Thus, adequate operations’ count was obtained.
The operations’ count for laryngeal and/or oropharyngeal neoplasm surgeries was 83 and showed gradual drop by 13% in March. Yet, 76% plunge was noted in April where surgeries reached 17. The overall drop from the start of February to the end of May was 88% where only 10 cases received surgical care. The major drop of surgeries in April and May were compared to the same period of the previous year to rule out any seasonal variations and to propose what the numbers would have been if conditions had been normal. This comparison elucidated 79% drop of surgical care in this period, from 128 cases in 2019 to 27 cases in 2020.
Measures were taken by the hospital to protect its health-care staff at this period to mitigate the risk of infection, with subsequent self-isolation and understaffing. As ENT surgeries could be a potential cause of aerosol production, personal protective equipment (PPE) was provided and were used by the health-care workers, according to WHO recommendations8 such as eye protection, N95 respirators, surgical gowns, and gloves. Moreover, careful preoperative history taking about COVID symptoms was obtained and nasopharyngeal swabs and CT chest were performed for all ENT cases before surgery.
The Royal College of Surgeons of England’s (RCS) president, Professor Derek Alderson comment on the waiting time statistics released by NHS England on June 11 was “Elective operations cover not only essential orthopaedic work—giving relief to people in need of new hips, knees and other joints—but life-saving treatment for cancer, heart problems, and neurological disorders.”9
In accordance with the study’s results, Dore3 described a similar situation in India where COVID-19 has indirectly affected the provision of health-care services. She mentioned that patients needing dialysis could not transfer to the health-care facility as well as those needing chemotherapy and antenatal care. Surgeries were postponed due to understaffing and fear of contracting infection as in Asian Cancer Institute. She also added that there was no official recording for the lockdown-related deaths. Some of these factors could also be attributed for the under-presentation of the patients to the authors’ hospital such as travel restrictions and curfew hours which could discourage patients referred from distant areas. However, there was no surgical postponement due to understaffing in The ENT Department. In addition to the previous potential curbs, people could have misunderstood the governmental “Stay Home” message or had fears of contracting the disease in the hospitals’ venue. Future studies could unveil more details about the observations found in this initial study.
COVID-19’s mortality rate is 0.66–7.8,10 whereas the mortality rate of head and neck cancer is 1.5% of all cancer deaths.11 Therefore, the mortality rate of COVID-19 could be indirectly increased by the under-presenting patients who did not seek medical advice in this period. Likewise, in this study, 79% reduction of surgical operations for patients having cancer or cancer-suspected lesions was noted. These patients may be currently suffering without seeking medical advice or may defer their presentation, leading to delay in diagnosis and management. Consequently, they may present later with advanced stages and unfavorable prognosis which could indirectly add to the COVID-19’s mortality rate.
Considering this study’s results and as a preparation for a potential second wave of the disease, the authors recommend clear special messages and advertisements targeting cancer-suspected and cancer patients to continue seeking medical advice. This may reverse any misunderstanding of the general concept of “Stay Home.” Furthermore, exemption from travel restrictions for these patients as well as proper supply and maintenance of adequate PPE supply is advised to protect the health-care staff, thus, preventing understaffing.
Due to the recent onset of COVID-19, the study’s duration was short. Future studies could be longer, multicenter, and may compare the advanced-stage cancer with previous figures. Detailed analysis of the reasons behind the under-presentation would be an interesting point of future research.
Conclusion
An estimate of 79% of patients, who had been presenting for laryngeal and/or oropharyngeal neoplasms, did not show up due to indirect COVID-19 effect.
Acknowledgement
The authors acknowledge Professor Usama Abd Alnaseer, Head of ENT Department, Cairo University, for his support to complete this study.
Footnotes
Ethical Approval: This study was approved by the ENT Ethical Committee, Faculty of Medicine, Cairo University.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mohamed Abd Elmottaleb Sabaa, MD  https://orcid.org/0000-0002-9491-6161
https://orcid.org/0000-0002-9491-6161
References
- 1. Rawaf S, Yamamoto HQ, Rawaf D. Unlocking towns and cities: COVID-19 exit strategy. East Mediterr Health J. 2020;26(5):499–502. doi:10.26719/emhj.20.028 [DOI] [PubMed] [Google Scholar]
- 2. Nassisi M, Audo I, Zeitz C, et al. Impact of the COVID-19 lockdown on basic science research in ophthalmology: the experience of a highly specialized research facility in France. Eye (Lond). 2020;34(7):1187–1188. doi:10.1038/s41433-020-0944-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dore B. Covid-19: collateral damage of lockdown in India. BMJ. 2020;369:m1711. doi:10.1136/bmj.m1711 [DOI] [PubMed] [Google Scholar]
- 4. Gupta B, Johnson N, Kumar N. Global epidemiology of head and neck cancers: a continuing challenge. Oncology. 2016;91(1):13–23. doi:10.1159/000446117 [DOI] [PubMed] [Google Scholar]
- 5. Rothan HA, Byrareddy SN. . The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi:10.1016/j.jaut.2020.102433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Quadri S. COVID-19 and religious congregations: implications for spread of novel pathogens. Int J Infect Diseas. 2020;96:219–221. doi:10.1016/j.ijid.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lau H, Khosrawipour V, Kocbach P, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020;27(3):1–7. doi:10.1093/jtm/taaa037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization. Rational Use of Personal Protective Equipment (PPE) for Coronavirus Disease (COVID-19): Interim Guidance. World Health Organization; 2020. [Google Scholar]
- 9. The Royal College of Surgeons of England. Patient numbers plummet as COVID “hollows out” NHS. Published 2020. Accessed June 18, 2020. http://www.rcseng.ac.uk/news-and-events/media-centre/press-releases/patient-numbers-plummet/
- 10. Mahase E. Covid-19: death rate is 0.66% and increases with age, study estimates. BMJ. 2020;369:m1327. doi:10.1136/bmj.m1327 [DOI] [PubMed] [Google Scholar]
- 11. Chow L. Head and neck cancer. N Engl J Med. 2020;382:60–72. doi:10.1056/NEJMra1715715 [DOI] [PubMed] [Google Scholar]